Abstract
COVID-19 patients may require supplemental oxygen therapy at home after recovery from COVID-19. We report benefits of add on Ayurvedic intervention in a 75-year-old gentleman who was oxygen dependent post hospitalisation. He was earlier treated for COVID-19 related bilateral pneumonitis, Acute Respiratory Distress Syndrome and Acute Renal Failure. Patient reported breathing difficulty, generalized weakness, reduced appetite and severe constipation. The Pulse Oximetry readings with oxygen support fluctuated between 80 and 85 %, Blood Pressure was 150/100 mm Hg, LDH raised at 463 IU/L and HbA1c at 8.7%. The patient was administered micro-doses of Rasasindura sublingually every 10 min for one day followed by administration of Indukānta Ghṛita and Suvarṇamālinīvasanta Rasa. The oxygen saturation improved to 95 % in 12 hrs of initiating treatment, oxygen support was weaned off on the third day of starting the Ayurvedic treatment, three weeks earlier than prescribed at the time of discharge. The patient is ambulant and maintaining oxygen saturation between 95 and 98 %. This case report highlights the potential of Ayurvedic intervention to manage patients with persistent hypoxia in post hospitalization phase. Well-designed studies are warranted to confirm the benefits of integrating such interventions with standard of care in COVID-19.
Keywords: COVID 19, SARS-CoV-2, Hypoxia, Ayurveda, Integrative medicine, Case report
1. Introduction
In the beginning of May 2021, the COVID 19 pandemic escalated in India with single day infections touching the highest ever numbers recorded globally since the outbreak in late 2019. The health care system in India was unimaginably overwhelmed and inadequate medical care is one of the major contributing factors to mortality associated with COVID-19 [1]. Patients with dropping oxygen saturation levels and breathing distress were unable to get oxygen supplementation in time or beds with oxygen support in hospitals [2]. Exact numbers of deaths attributable to oxygen shortage are not yet available, but oxygen crisis has been the hallmark of the second wave of COVID-19 in India [3]. In severe COVID-19, Acute Respiratory Distress Syndrome (ARDS) with pneumonia presents as a medical emergency requiring intensive care in hospital settings [4]. In critical stages, the immediate cause of death in most of the cases is respiratory failure, which happens due to diffuse alveolar damage [5]. A sudden surge of positive cases can overburden the health care system and deny patients access to hospital beds and oxygen in critical stages of illnesses. Harnessing the resources in India's pluralistic health care system is one amongst the possible strategies to address unmet needs at the peak of the pandemic crisis. COVID-19 patients in India have been approaching Ayurveda physicians for medical care in badly affected cities like Mumbai when left without options to access mainstream health care facilities. Outcomes of such encounters have been published [6,7] and indicate the potential of Ayurvedic interventions in COVID-19 related hypoxia. We report the case of a hypertensive and insulin dependent diabetic COVID-19 patient who was prescribed supplemental oxygen for 30 days after discharge from the hospital. The patient was able to stop oxygen therapy on the third day of administration of Ayurvedic treatment. This case report highlights the relevance and scope of integrating Ayurvedic interventions with standard of care to address the major challenges and gaps in medical management of the second wave of COVID-19 in India.
2. Patient information
2.1. De-identified patient specific information
A 75-year-old man living in Mumbai, a retired government official by profession consulted his Ayurvedic general practitioner after undergoing hospitalized care for COVID-19 related Acute Respiratory Distress Syndrome (ARDS) with bilateral pneumonitis as well as Acute Renal Failure (ARF).
2.2. Primary concerns and symptoms of the patient
The patient mainly complained of persistent breathing distress requiring oxygen support five days after being discharged from hospital. He reported to be suffering from generalized weakness, severe constipation, and reduced appetite. The patient was mainly concerned about the poor oxygen saturation levels that did not improve even after standard of care interventions for COVID-19.
2.3. Medical, family, and psycho-social history including relevant genetic information
The patient is a hypertensive, insulin dependent diabetic in the last twenty-five years. His father was also diabetic. Genetic history is not contributory in this case. He did not report any addictions and leads a quiet life at home after retirement from public service.
2.4. Past interventions and outcomes
Patient was operated for prostatomegaly seventeen years ago. He is on medications for diabetes and hypertension in the past 25 years. After testing positive for COVID-19, patient developed breathing distress on exertion, intermittent fever, cough with expectoration, loss of appetite, general weakness, and tachypnea. He had severe constipation requiring soap water enema for evacuation. He was admitted to a hospital on 01/04/2021 and was subsequently diagnosed with Acute Respiratory Distress Syndrome and bilateral pneumonitis as well as Acute Renal Failure. He was admitted to ICU and was on Non-Invasive Ventilation for two weeks. During the hospital stay, he was administered a course of antibiotics, steroids, blood thinner and pirfenidone to prevent lung fibrosis. Insulin, anti-diabetic, and anti-hypertensive medications were administered to manage existing co-morbidities along with multivitamin tablets, vitamin C and zinc. He was catheterized using a Foley's catheter and needed soap water enema to move his bowels. He was discharged from the hospital on 16/04/2021 in a hemodynamically and clinically stable condition but with persistent breathing difficulty and reportedly low oxygen saturation levels. Pulse oximetry reading at the time of discharge has not been documented in the discharge card. He was advised home oxygen therapy at home for 30 days along with other medications.
3. Main clinical findings
At the time of seeking Ayurvedic treatment, the oxygen saturation of the patient was fluctuating between 80 and 85 % and the patient was on continuous home oxygen therapy. The patient was slightly overweight with a BMI of 26.7 (Height 150 cms, Weight 60 kg) and moderately built. The blood pressure was 150/100 mm Hg. His lab test report from the previous week reported HbA1c value of 8.7. Patient had tachypnea and was bedridden. On interrogation, the patient revealed that he possibly contracted the virus when he visited a nearby marketplace. Ayurvedic clinical assessment indicated reduced Agni (digestive and metabolic functions), Bala (strength) and Ojas (vitality). However, the Sattva (mental strength) of the patient was good.
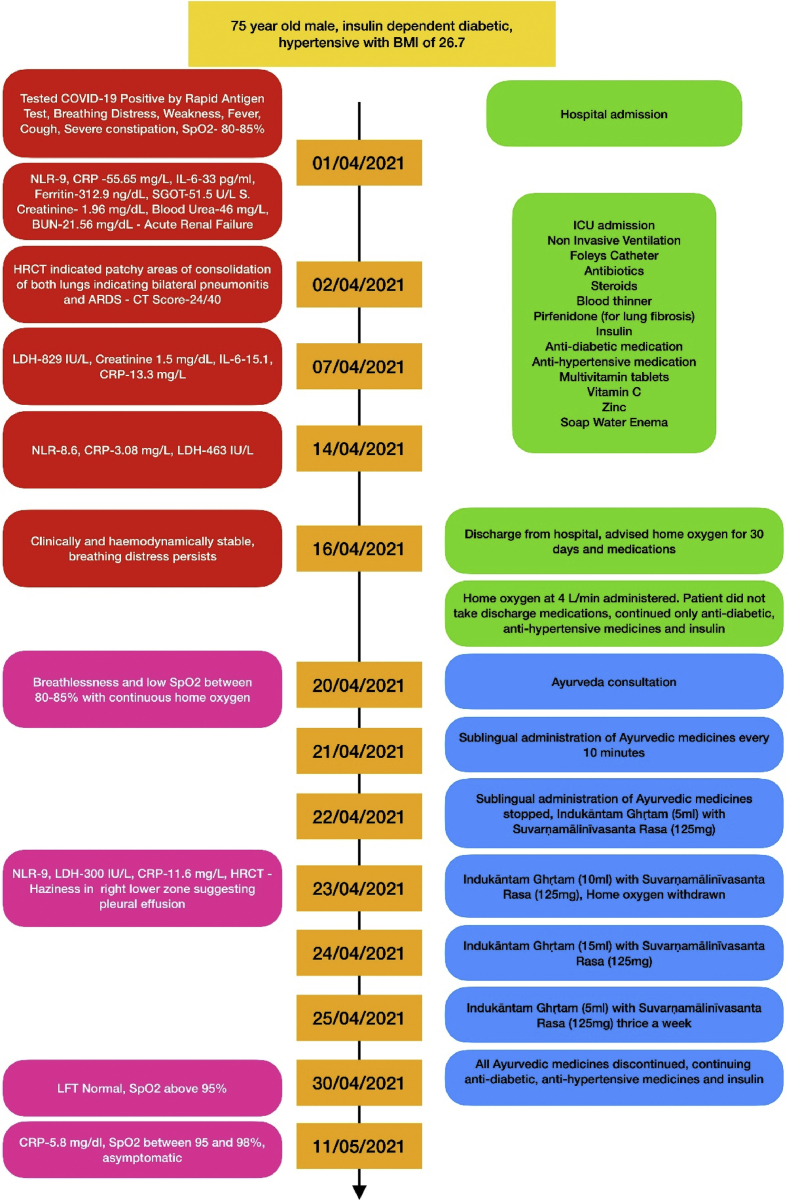
4. Timeline
Important information from the patient's treatment history has been organised in the form of a timeline. See Fig. 1.
Fig. 1.
Timeline.
5. Diagnostic assessment
5.1. Diagnostic tests
Patient was tested antigen positive for COVID-19 on 01/04/2021. The HRCT scan on 02/04/2021 revealed patchy areas of consolidation in upper and lower lobes of both lungs, moderate involvement of both lungs (50–75 % involvement of parenchyma) and CT Score was 24/40. At the time of admission, NLR was 9, CRP - 55.65 mg/L, IL-6 – 33 pg/ml, Serum Creatinine - 1.96 mg/dL, SGOT – 51.5 U/L, Blood Urea – 46 mg/L and BUN – 21.56 mg/dL. During the hospital stay, LDH was found elevated at 829 IU/L (07/04/2021). D-Dimer and Ferritin were within normal limits. The laboratory values just before discharge from hospital (14/04/2021) were as follows - Hb - 10.7 g/dL, WBC - 6980 with NLR 8.6 (N-86, L-10), Platelet - 1.90 lakhs/cumm, CRP - 3.08 mg/L, LDH – 463 IU/L. HbA1c was 8.7 indicating poor control of diabetes See Table 2.
Table 2.
Results of relevant investigations.
| 01/04/21 | 02/04/21 | 04/04/21 | 05/04/21 | 07/04/21 | 11/04/21 | 14/04/21 | 20/04/21 | 23/04/21 | 30/04/21 | 11/05/21 | 14/06/21 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Hemoglobin (gm/dL) | 11.5 | 11.4 | 11.6 | 11.6 | 12.5 | 11.1 | 10.7 | 11.3 | ||||
| White Blood Cells (cells/mcL) | 9900 | 6980 | 12220 | 10750 | 10960 | 6980 | 10900 | 8790 | ||||
| Neutrophils (%) | 90 | 95 | 90 | 55 | 95 | 88 | 86 | 81 | 65 | |||
| Lymphocytes (%) | 10 | 3 | 10 | 40 | 3 | 10 | 10 | 9 | 26 | |||
| NLR | 9 | 31.7 | 9 | 1.38 | 31.7 | 8.8 | 8.6 | 9 | 2.5 | |||
| Interleukin 6 (pg/mL) | 33.8 | 15.1 | ||||||||||
| C Reactive Protein (mg/L) | 55.65 | 13.30 | 9.09 | 3.08 | 11.46 | 5.8 | ||||||
| Ferritin (ng/mL) | 312.9 | 288.9 | 312.5 | |||||||||
| HbA1c (%) | 8.7 | |||||||||||
| Serum Creatinine (mg/dL) | 1.96 | 2.03 | 1.58 | 1.5 | 1.08 | |||||||
| Blood Urea (mg/dL) | 46.2 | 21.20 | ||||||||||
| Blood Urea Nitrogen (mg/dL) | 21.56 | 9.91 | ||||||||||
| BUN/Creatinine ration | 9.18 | |||||||||||
| Lactate Dehydrogenase (U/L) | 829.2 | 547.5 | 463 | 300 | ||||||||
| SGOT (U/L) | 24.7 | 15 | ||||||||||
| SGPT (U/L) | 51.5 | 12 | ||||||||||
| SpO2 (%) | 80–85 | 80–85 | 95 | 95–98 | 95–98 | |||||||
| HRCT | 24/40 | |||||||||||
| Uric acid (mg/dl) | 5.19 | |||||||||||
| Calcium (mg/dl) | 9.25 | |||||||||||
| Phosphorus (mg/dl) | 3.11 |
Note: RBC, Platelets, Serum Electrolytes, D-Dimer, INR, Prothrombin as well Complete panel of Liver and Renal Function Tests were conducted during hospital stay. Only relevant lab results have been included in this table.
5.2. Diagnostic challenges
From the reports of the patient, it is not clear whether COVID-19 diagnosis was established by RT-PCR or Rapid Antigen Test (RAT). The headline of the report is RT-PCR but the result says Antigen Positive and CT Value is not mentioned. In the second wave of the pandemic in India, labs have been overwhelmed with increasing RT-PCR tests for confirming COVID-19 diagnosis. Positive RAT with clinical presentation of COVID-19 and supportive HRCT findings seems to be the basis of diagnosis. Other relevant laboratory tests such as inflammatory markers for COVID-19 were done to establish the diagnosis. However, a repeat Rapid Antigen or RT PCR was not done as it is not mandatory for hospital discharge or after 14 days of testing positive for COVID-19. Moreover, patients find it difficult to repeat these tests after recovery. Chest Xray was done a week after hospital discharge. Further HRCT assessment was deemed unnecessary considering the cost and risk of exposure to harmful radiation.
5.3. Diagnosis
5.3.1. Biomedical diagnosis
The diagnosis was COVID-19 based on antigen positivity with ARDS and bilateral pneumonitis (based on HRCT findings). On the basis of Renal Function Tests, which revealed slightly elevated creatinine, blood urea and blood urea nitrogen, he was diagnosed to be also suffering from Acute Renal Failure at the time of hospitalisation. Insulin dependent diabetes and hypertension were known co-morbidities.
5.3.2. Ayurvedic diagnosis
The clinical picture at the time of Ayurvedic assessment was that of a patient in the stage of transition to JĪrṇajvara (chronic fever). Retrospective analysis of the case history and course in the hospital pointed to a primary diagnosis of Sannipātajvara (Fever caused by derangement of all three dosas) showing dominance of Vāta and Kapha with association of Pitta [8] and residual effects in the Prāṇavahasrotas (The respiratory passages).
5.4. Prognostic outlook
The patient had recovered from the acute stage of ARDS and bilateral pneumonitis following hospitalized standard of care intervention for COVID-19. Inflammatory markers and creatinine were showing a normalizing trend. The patient was expected to recover gradually at home, though the possibility of long covid syndrome or further deterioration could not be ruled out. Co-morbidities with poor control of diabetes and hypertension as well as acute renal failure along with persistent breathing difficulties suggest challenges in recovery. At the time of discharge, the patient was expected to require at least one month of home oxygen therapy before further review.
6. Therapeutic interventions administered
6.1. Types of therapeutic intervention
6.1.1. Standard of care pharmacological interventions
Treatment administered in the hospital has been discussed in the section on past treatments. The patient was discharged from hospital with the following prescription. He was advised to taper and discontinue Omnacortil (20 mg for three days, 10 mg for three days and 5 mg for three days). Other medicines were Feropenen 200 mg 1-0-1 for 2days; Tab. Dobirex 150 mg - 1-0-1 and Tab. Perfinex 200 mg - 1-0-1 for 45 days; Tab. Janumet 50/500 - 1-0-1 for 15 days; Tab. Nexovas 10 mg - 1-0-0, Tab. Cobadex CZS - 0-1-0, Tab. Limsee 500 mg - 1-0-1 and Tab. Zinc 50 mg - 0-1-0 for 30 days; Inj. Lantus - 8 Units for 30 days; Levoflox 500 mg - 1-0-0 for 7 days and Cap. Uprise D3 60k once in a week for 4weeks. Except anti-diabetic and anti-hypertensive medications, patient did not take any of the above discharge medications prescribed to him.
6.1.2. Ayurvedic pharmacological interventions
Only internal medications were administered to the patient. Rasasindūra [9], Apāmārgakṣāra [10], Pippalīmūlacūrṇa [11] and Ṣaḍdharaṇacūrṇa [10] were administered sublingually with honey as adjuvant frequently [14](10 minutes) for a duration of 24 h. Indukāntaṃ Ghṛitaṃ [12] and Suvarṇamālinīvasanta Rasa [13] were administered internally. See Table 1 for details of Ayurvedic medicines administered.
Table 1.
Schedule of administration of Ayurvedic medications.
| Date | Rasasindūraṃ | Apāmārgakṣāraṃ | Pippalimūlacūrṇaṃ | Ṣaḍdharaṇacūrṇaṃ | Indukāntaṃ Ghṛitaṃ | Suvarṇamālinīvasanta Rasa |
|---|---|---|---|---|---|---|
| 21/04/2021 | 15 mg every 10 min on the first day, then every 1 h, 2 h and 3 h | 25 mg every 10 min on the first day, then every 1 h, 2 h and 3 h | 10 mg every 10 min on the first day, then every 1 h, 2 h and 3 h | 1 pinch | X | X |
| 22/04/2021 | X | X | X | X | 5 ml at 7:00 am | 125 mg at 7:00 am |
| 23/04/2021 | X | X | X | X | 10 ml at 7:00 am | 125 mg at 7:00 am |
| 24/04/2021 | X | X | X | X | 15 ml at 7:00 am | 125 mg at 7:00 am |
| 26/04/2021 | X | X | X | X | 5 ml at 7.00 am | 125 mg at 7:00 am |
| 28/04/2021 | X | X | X | X | 5 ml at 7.00 am | 125 mg at 7:00 am |
| 30/04/2021 | X | X | X | X | 5 ml at 7.00 am | 125 mg at 7:00 am |
6.1.3. Ayurvedic dietary regimen
Patient was advised to take rice, roti, dal, vegetables prepared with minimal oil or ghee and locally available fruits. He was told to avoid milk and milk products.
6.2. Duration of therapeutic intervention
Ayurvedic medicines were administered from 21/04/2021 until 30/04/2021. Table 1 summarises the details of administration of Ayurvedic medicines in this patient in the oxygen dependent phase.
From 22/04/2021 to 30/04/2021 the patient was advised to take Indukāntaṃ Ghṛitam with 1 tablet of Suvarṇmālinīvasanta Rasa. The dosage and strength of the medicines are mentioned in Table 1. Thereafter, he was advised to continue only the anti-diabetic and anti-hypertensive medications.
6.3. Changes in therapeutic intervention
After discharge from hospital, the patient had persistent breathing distress. He needed supplemental oxygen therapy at home and sought Ayurvedic treatment for relief. He was administered a combination of Rasasindūra, Apārmārgakṣāra and Pippalīmūlacūrṇa, as well as Ṣaḍdharaṇacūrṇa with the Ayurvedic clinical assessment of Vata involvement in the Amasaya (upper gastrointestinal tract) [14]. These medicines were administered at regular intervals of 10 min on the first day and then the frequency was reduced to once in an hour, once in 2 h and 3 h. When improvement of oxygen saturation levels were observed, it was inferred that clearance of the srotas (channels) and improvement of agni (digestive fire) had been achieved. Conservative administration of medicated ghee (śamanaghṛtapāna) in line with the principles of management of chronic fever (jīrṇajvaracikitsā) was initiated as three weeks had passed since the onset of the fever [14].
7. Follow-up and outcomes observed
Within 12 hours of sub-lingual administration of Ayurvedic medicines every 10 min, oxygen saturation levels of the patient improved from 80-85 % to 90–95 % (21/04/2021). After two days of administration of Indukāntaṃ Ghṛitam with Suvarṇmālinīvasanta Rasa, oxygen supplementation could be withdrawn completely and SpO2 levels were maintained above 95 % (23/04/2021).
After discontinuation of Ayurvedic medicines (30/04/2021), patient has been followed up for clinical evaluation. His oxygen saturation levels were stable between 95 and 98 %. Last SpO2 reading was taken on 11/05/2021. He did not complain of breathing distress. He continuned anti-diabetic and anti-hypertensive medications.
7.1. Clinician and patient-assessed outcomes
There are no specific clinician assessed outcomes to report other than what is discussed in the section on diagnostic assessment and rationale of treatment. There are no specific or relevant patient assessed outcomes to report in this case.
7.2. Important follow-up diagnostic test results
On 23/01/2021, the second day of starting Ayurvedic treatment CRP was high at 11.46 mg/dL, WBC was 10,900 with NLR of 9 (N-81, L-9 and LDH – 300 IU/L. Chest X ray revealed haziness in right lower zone obliterating right costophrenic angle suggesting pleural effusion. On 30/04/2021, Liver Function Test parameters were found to be within normal range. On 11/05/2021, CRP was normal at 5.8 mg/dL as well as WBC- 8790/cumm with NLR of 2.5 (N- 65, L- 26). Pulse oximetry readings were consistently above 95 % throughout the follow up period. As the patient had Acute Renal Failure during hospital stay and had been administered herbo-mineral preparations, we checked the renal function of the patient in the follow up period. All values were within normal limits. On 14/06/2021, Serum Creatinine was 1.08, Serum Urea was 21.20 and Blood Urea Nitrogen was 9.91 See Table 2.
7.3. Intervention adherence and tolerability
The patient could tolerate the administration of Ayurveda medications and had strictly adhered to the advised medications, diet, and lifestyle during the short course of Ayurvedic treatment.
7.4. Adverse and unanticipated events
The patient did not report any adverse or unanticipated events during or after administration of Ayurvedic treatment.
8. Discussion
8.1. Strengths and limitations of this case report
The data presented in this case report is restricted by the limitations of clinical practice. Due to the COVID-19 emergency, the patient was consulted remotely and elaborate physical examination was not possible. As discussed, it is not clear from available reports whether COVID-19 diagnosis was established by RT-PCR or Rapid Antigen Test. Only most relevant laboratory parameters were tested after initiation of Ayurvedic treatment, and the patient was not inclined to repeat the tests once he was weaned off oxygen support and improved clinically. Renal function tests were done at the time of hospital admission and creatinine was monitored in the first few days of hospital stay. These tests were not repeated later despite a diagnosis of Acute Renal Failure. It is a strength of this case report that the severity of the patient's condition requiring hospitalized care and oxygen supplementation in the post-hospitalization period have been well documented in the available medical records with relevant investigations and clinical assessment of treating physicians. It was five days since the patient had discontinued allopathic medications when Ayurvedic treatment was initiated. His oxygen saturation levels were poor (80–85 % with oxygen support), which improved within 12 h of administration of Ayurvedic treatment and oxygen support could be withdrawn subsequently on the third day. In the light of these observations, we can propose the hypothesis that Ayurvedic interventions have the potential to facilitate recovery in hypoxic COVID-19 patients and reduce oxygen dependency.
8.2. Discussion
COVID-19 patients can require oxygen support at home even after they are discharged from hospital. One study reported higher rates of readmission, multiorgan dysfunction and death in COVID-19 patients after hospital discharge compared to matched controls [15]. Due to increase in rate of hospitalization of COVID-19 patients, strategy for transitional care of patient from hospital to home has been proposed to reduce inpatient days in the hospital [16]. Ambulatory management of COVID-19 with home oxygen therapy has been associated with reduced mortality and readmission rates thirty days after discharge from hospital [17]. The COVID-HOT algorithm has been developed for providing safe and effective home oxygen therapy for COVID-19 patients [18]. A study on post-discharge health status of COVID-19 patients surveyed the participants at a median of 37 days after hospital discharge. It was found that 36.8 % required home oxygen and 13.5 % were still on oxygen support at the time of the survey [19]. In the present case, home oxygen was prescribed for 30 days after discharge, but oxygen support could be withdrawn on the third day after starting Ayurvedic treatment, which was the seventh day after discharge from the hospital. Mumbai become the epicenter of the second wave of the pandemic in India overburdening the health care system. Patients were being discharged after essential critical care at hospital for continued supportive care at home. The SpO2 levels of this patient was not found to be mentioned in the hospital discharge card. At the time of starting Ayurvedic treatment, it was far below the levels recommended for home care (80–85 %) even with oxygen supplementation. We could not determine if this was indicative of deterioration in his condition at home in the first five days after discharge. It is pertinent to note that the patient did not continue the discharge prescription except for anti-diabetic and anti-hypertensive medications.
8.3. The scientific rationale
We are reporting this case to present an important observation about the potential efficacy of Ayurvedic intervention in management of persistent hypoxia in COVID-19 patients. At the time of discharge, the patient was advised to continue medications and home oxygen support for thirty days before reporting again for further assessment. A quick recovery was not anticipated in this case. Five days after hospital discharge, the patient continued to have poor oxygen saturation levels below 90 % even with home oxygen therapy. The patient discontinued the discharge medications at the time of starting Ayurvedic treatment. The recovery observed within three days of administration of Ayurvedic treatment appears to be remarkable and needs to be investigated further for its potential in facilitating faster recovery from post-covid hypoxia.
The frequent administration of the combination of Rasasindūra, Apārmārgakṣāra, Pippalīmūlacūrṇa and Ṣaḍdharaṇacūrṇa was found to improve oxygen saturation levels within few hours. Frequent administration of medicines is indicated in management of respiratory distress. Sublingual administration enables the medicine to be absorbed quickly and spread through the prāṇavahasrotas (respiratory system) to exert its pharmacological action. It has been proposed that Ayurvedic metal nano particles could be repurposed as novel antiviral agents against SARS-CoV-2. Some commonly used Ayurvedic nano-metallic preparations could have anti-inflammatory and immunomodulatory activity [20]. Rasasindūra and Suvarṇamālinī Vasanta Rasa are both such nano-metallic herbo-mineral preparations administered to the patient. Of these, Rasasindūra was administered for its short-term effects and Suvarṇamālinī Vasanta Rasa for sustained effect. Apārmārgakṣāra is an alkaline substance obtained from the ashes of the plant Achyranthes aspera. It can remove the blockage of thick mucus, relieve congestion, and open the respiratory and circulatory channels. Pippalīmūlacūrṇa, the powder of the roots of Piper longum pacifies Vata and Kapha, which are involved in obstruction and fibrosis of lungs leading to breathing distress in COVID-19. Ṣaḍdharaṇacūrṇa is specifically indicated in the obstruction of Vāta in the gastroinstestinal tract, which is according to Ayurveda the trigger for respiratory pathologies. Indukāntaṃ Ghṛitaṃ is indicated for strengthening digestive fire (agni), opening the channels (srotas) and for strengthening the body (bṛṃhaṇa) after the acute stage of fever. One study reported its immunomodulatory property [21]. A word of caution must be put forth here regarding the use of Rasasindūra in higher doses. The recommended full dose of Rasasindūra is 125 mg (1 gunja or ratti) [22]. In an emergency situation, we have found that short term administration of Rasasindūra in higher doses is well tolerated by patients. After a maximum of five or six divided doses of 15 mg of Rasasindūra along with other medications mentioned above, it has been found that there is marked clinical improvement in patients and the frequency of the medicine can be reduced to once in one, two or 3 h and gradually withdrawn. It must be ensured that the dosage of Rasasindūra is reduced as soon as the patient shows signs of clinical improvement and must be discontinued if there is no response within the first 6 h of administration of the medicine. Medicines like Rasasindūra should only be administered under medical supervision and patients need to be warned against self-medication and prolonged use.
In the light of the known properties of the medicines administered to the patient and the results observed clinically, we presume that Ayurvedic interventions helped in reducing inflammation in the lung and clearance of fluids as well as in modulation of immunity. However, specific mechanism of action of such medicines in hypoxia needs to be studied systematically.
8.4. The primary “take-away” lessons of this case report
The outcomes of Ayurvedic intervention reported in this paper points to the potential of Ayurvedic intervention to facilitate faster recovery in COVID-19 patients who require home oxygen after hospital discharge. Further studies are needed to evaluate the benefits of integrating Ayurvedic care in the rehabilitation of patients recovering at home from residual clinical manifestations of severe COVID-19 infection.
Patient perspective
I was afflicted with COVID 19 one and a half months ago. On 1st April, I started getting discomfort and was admitted at a hospital. On 16th April, I was discharged from the hospital and I was advised to be on a dose of four liters oxygen/day for 30 days by the doctors. On 19th April, my oxygen saturation dropped, and I opted for Ayurveda treatment on 20th April. After 21st April, I started feeling better and by 23rd April, I could withdraw the support of oxygen. After that, my oxygen saturation was stable. By taking Ayurveda treatment, I could save a lot on my medical expenses and I could get rid of all the problems that were caused due to COVID.
Informed consent
Written informed consent has been obtained from the patient for publication of this case report and the full text of this manuscript has been shared with him. The document is made available to the editors for examination.
Author contributions
JJ, the first author is the treating physician who formulated the treatment protocol and was consulted by the patient for Ayurvedic care. JJ provided the summary of the diagnosis, treatment and observed outcomes and collected the informed consent from the patient for publication of this case report. SNS, SSK and PEN organized and analyzed the data in consultation with JJ and produced the first draft of the manuscript. They compiled relevant references from classical Ayurvedic texts. RP guided all the co-authors through every stage of preparation of the manuscript, provided scientific and technical inputs to develop the case report and redrafted the final version of the manuscript after several rounds of revision.
Funding sources
None.
Declaration of competing interest
None.
Footnotes
Peer review under responsibility of Transdisciplinary University, Bangalore.
References
- 1.Asrani P., Eapen M.S., Hassan M.I., Sohal S.S. Implications of the second wave of COVID-19 in India. Lancet Respir Med. 2021 Jun 30 doi: 10.1016/S2213-2600(21)00312-X. S2213-2600(21)00312-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Choudhary O.P., Priyanka, Singh I., Rodriguez-Morales A.J. Second wave of COVID-19 in India: dissection of the causes and lessons learnt. Trav Med Infect Dis. 2021 Jun 16;43:102126. doi: 10.1016/j.tmaid.2021.102126. Epub ahead of print. PMID: 34144178; PMCID: PMC8214078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Samarasekera U. India grapples with second wave of COVID-19. Lancet Microbe. 2021 Jun;2(6):e238. doi: 10.1016/S2666-5247(21)00123-3. Epub 2021 Jun 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kordzadeh-Kermani E., Khalili H., Karimzadeh I. Pathogenesis, clinical manifestations and complications of coronavirus disease 2019 (COVID-19) Future Microbiol. 2020 Sep;15:1287–1305. doi: 10.2217/fmb-2020-0110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Elezkurtaj S., Greuel S., Ihlow J., Michaelis E.G., Bischoff P., Kunze C.A., et al. Causes of death and comorbidities in hospitalized patients with COVID-19. Sci Rep. 2019;11:4263. doi: 10.1038/s41598-021-82862-5. 123AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Joshi J.A., Puthiyedath R. Outcomes of ayurvedic care in a COVID-19 patient with hypoxia - a case report. J Ayurveda Integr Med. 2020 Oct 13 doi: 10.1016/j.jaim.2020.10.006. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rastogi S. Ayurveda co-interventions have supported complete recovery in severe covid- 19 infection with a chest severity Score 18/25: a case report. J Ayurveda Integr Med. 2021 Mar 12 doi: 10.1016/j.jaim.2021.02.008. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Puthiyedath R., Kataria S., Payyappallimana U., Mangalath P., Nampoothiri V., Sharma P., et al. Ayurvedic clinical profile of COVID-19 - a preliminary report. J Ayurveda Integr Med. 2020 Jun 12 doi: 10.1016/j.jaim.2020.05.011. S0975-9476(20)30039-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Angadi Ravindra., editor. Rasatarangini of sadananda sharma. Chaukhabha Surbharati Prakashan; Varanasi: 2015. p. 98. [Chapter 6], Verse 207. [Google Scholar]
- 10.Trikamji Acaraya Yadavji. In: Ram Acarya Narayan., editor. Chaukhambha Sanskrit Sansthan; Varanasi: 2008. (Susrutasamhita of sushruta). [Sūtrasthāna, 11.11], [Cikitsāsthāna, 4.3-4] [Google Scholar]
- 11.Bhava Prakasha Nighantu. 9th ed. Motilal Banarsidas press; New Delhi: 1998. p. 14. Dwivedi Vishwanatha. [Google Scholar]
- 12.Krishnan Vaidyan K.V., Anekalilil S Gopala Pillai, Sahasrayoagam Alappuzha. Vidyarambham Publications; 2007. Ghrita prakarana; p. 322. [Google Scholar]
- 13.Acharya Bindu, Rasapaddhati Siddhiprada. 2nd ed. Chaukhambha Orientalia Varanasi; 2005. Hindi Commentary by Siddhinandana Mishra; p. 167. [Google Scholar]
- 14.Acharya J.T., editor. Carakasamhita of caraka. Chaukhamba Orientalia; Varanasi: 2011. [Cikitsāsthāna, 28.28], [Cikitsāsthāna, .3-165], [Cikitsāsthāna, .30-299-301] [Google Scholar]
- 15.Ayoubkhani D., Khunti K., Nafilyan V., Maddox T., Humberstone B., Diamond I., et al. Post-covid syndrome in individuals admitted to hospital with covid-19: retrospective cohort study. BMJ. 2021 Mar 31:372. doi: 10.1136/bmj.n693. n693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Borgen I., Romney M.C., Redwood N., Delgado B., Alea P., George B.H., et al. From hospital to home: an intensive transitional care management intervention for patients with COVID-19. Popul Health Manag. 2021 Feb;24(1):27–34. doi: 10.1089/pop.2020.0178. [DOI] [PubMed] [Google Scholar]
- 17.Banerjee J., Canamar C.P., Voyageur C., Tangpraphaphorn S., Lemus A., Coffey C., Jr., et al. Mortality and readmission rates among patients with COVID-19 after discharge from acute care setting with supplemental oxygen. JAMA Netw Open. 2021 Apr 1;4(4) doi: 10.1001/jamanetworkopen.2021.3990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sardesai I., Grover J., Garg M., Nanayakkara P.B., Di Somma S., Paladino L., et al. Short term home oxygen therapy for COVID-19 patients: the COVID-HOT algorithm. J Fam Med Prim Care. 2020 Jul 30;9(7):3209–3219. doi: 10.4103/jfmpc.jfmpc_1044_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Weerahandi H., Hochman K.A., Simon E., Blaum C., Chodosh J., Duan E., et al. Post-discharge health status and symptoms in patients with severe COVID-19. medRxiv. 2020 Aug 14 doi: 10.1101/2020.08.11.20172742. [Preprint] 2020.08.11.20172742 Update in: J Gen Intern Med. 2021 Jan 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sarkar P.K., Das Mukhopadhyay C. Ayurvedic metal nanoparticles could be novel antiviral agents against SARS-CoV-2. Int Nano Lett. 2021 Jan 6:1–7. doi: 10.1007/s40089-020-00323-9. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.George S.K., Rajesh R., Kumar S.S., Sulekha B., Balaram P. A polyherbal ayurvedic drug--Indukantha Ghritha as an adjuvant to cancer chemotherapy via immunomodulation. Immunobiology. 2008;213(8):641–649. doi: 10.1016/j.imbio.2008.02.004. Epub 2008 Apr 16. [DOI] [PubMed] [Google Scholar]
- 22.Sharma Sadananda, Angadi Ravindra., editors. Rasatarangini. 1st ed. Chaukamba Surbharati Prakashan; 2015. [6th Taranga verses 235-237] [Google Scholar]