Abstract
Introduction and importance
The aim of this case report is to present a technical report for rehabilitation of patients with atrophic maxilla with the use of extra-long transnasal implants associated with unilateral zygomatic implants.
Case presentation
The indications, contraindications, planning and surgical procedure are described in order to give surgeons confidence in the management of this surgical approach to how to increase the range of rehabilitative options available to surgeons and patients.
Clinical discussion
Maxillary bone atrophy is a challenge demanding a high degree of experience of dental surgeons who trains themselves to rehabilitate these patients, whose treatment options range from bone grafts through to zygomatic implants. Extensive regions of atrophy require the use of 4 zygomatic implants which, in spite of offering predictability of the treatment, increase the surgical risk, require zygomatic bone with volume for anchoring 2 zygomatic implants. Generally, this bone density is reduced in elderly patients, making apical anchorage of the implants unfeasible.
Conclusion
The case report presented is a feasible alternative for replacing the placement of a second zygomatic implant, thereby diminishing the surgical risk, and making it possible for the technique to be more extensively used and performed by a larger number of surgeons.
Keywords: Transnasal implants, Zygomatic implants, Atrophic maxilla, Quad zygoma, Case report
Highlights
-
•
Present a case report with the use of extra-long transnasal implants.
-
•
Alternative for substituting the insertion of a second zygomatic implant.
-
•
Decrease the surgical risk.
1. Introduction
Rehabilitation of patients with atrophic maxilla is a challenging treatment. Among the various treatment options, therapy with the use of zygomatic implants has been shown to be an option with high success rates over the last 30 years, is well accepted by patients, and improves their quality of life and masticatory function [1].
Depending on the degree of maxillary bone atrophy, 2 zygomatic implants may be used in combination with a minimum of 2 conventional anterior implants [2], or only 4 zygomatic implants (Quad Zygoma) in cases of absence of bone volume in the anterior region of the maxilla [3]. In spite the technique being a predictable and well documented in the literature, in the above-mentioned cases, a higher degree of experience of the surgeon is demanded. Moreover, there is increased surgical risk due to the apex of the second zygomatic implant being anchored close to the orbit [[3], [4], [5]]. Indication of the placement of 4 zygomatic implants also has limitation when the infraorbital foramen is within the trajectory of the zygomatic implant, dimension of the zygomatic bone is insufficient for anchorage of 2 zygomatic implants, and there is accentuated facial concavity of the patient between the zygomatic bone, maxillary sinus and alveolar ridge (ZAGA 3 e 4), making it unfeasible to place a zygomatic implant, due to the risk of dehiscense of the tissue and exposure of the implant body [[6], [7], [8]].
As an alternative to the use of 4 zygomatic implants, there is a new treatment option, with the placement of extra-long transnasal implants associated with unilateral zygomatic implants [6].
The aim of the present article is to describe the indications, contraindications, planning and surgical procedure for the placement of extra-long transnasal implants associated with unilateral zygomatic implants.
This case report has been reported in line with the SCARE Criteria [9].
1.1. Surgical technique
1.1.1. Indications
Sufficient bone volume in the frontal process of the maxilla for the apical anchorage of extra-long implants (minimum of 3 mm) [6]; Minimum bone height of 4 mm between the ridge of maxilla and nasal cavity. Bone height lower than this could make it unfeasible to perform immediate loading [6]; Insufficient maxillary bone volume in the pre-maxilla for the placement of 2 conventional implants [6]; Insufficient zygomatic bone volume for the placement of 2 zygomatic implants [6]; Position of the infraorbital foramen in the trajectory of the second zygomatic implant [6]; Large concavity of the anterior wall of the maxilla, in which a large portion of the implant will not be in contact with the bone, and will be covered by soft tissue only, thus increasing the risk for exposure of the implant body [6].
1.1.2. Contraindications
Very wide nasal cavities with distally placed lateral limit must be avoided since the implant will not be touching on the distal bone wall, thereby making bone grafting unfeasible after implant placement, and it could interfere in respiratory function [6].
1.1.2.1. Planning
Patient, 63 years old, female, smoker, with total removable denture in the upper arch, who intends to undergo rehabilitation of the maxilla with implant-supported dental prosthesis. After analyzing the radiographic exams, the treatment options were presented to the patient, who opted for the placement of extra-long transnasal implants and zygomatic implants using the all-on-4 technique.
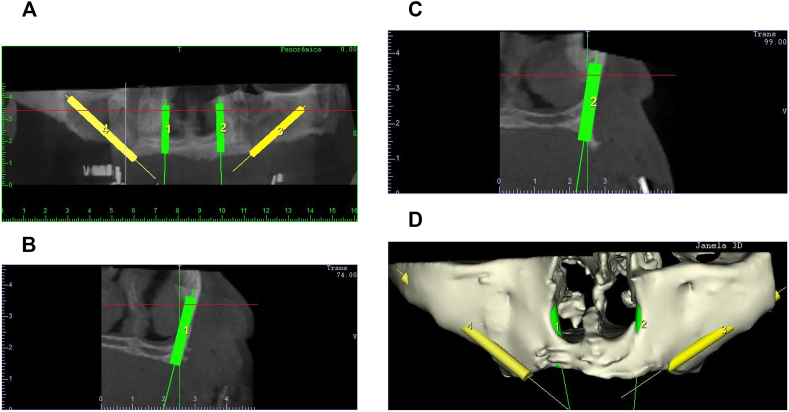
After clinical evaluation, a computed tomography study and surgical simulation in virtual planning software necessary (Fig. 1). During simulation, it is possible to verify the availability of frontal process of the maxilla and zygomatic bone, and perform virtual implant placement of the extra-long transnasal and zygomatic implants.
Fig. 1.
1A. Virtual surgical planning in software (Dentalslice® Bioparts) panoramic section. 1B Right transverse section, 1C Left transverse section, 1D 3D Reconstruction.
Virtual placement of the implants allows prediction of the diameter and length of all the implants, and enables better placement of each implant according to the zone of bone disposition [10]. Moreover, it is an important tool allied to anatomic knowledge of the face to observe the trajectory of implants and maintain a safe distance from the infraorbital foramen, orbit and lacrimal canal.
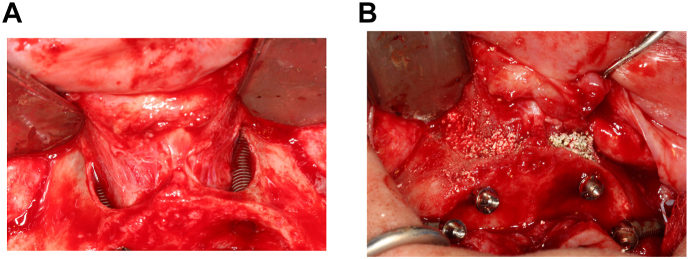
Once virtual planning has been made, and the surgeon is certain that there is bone available for all the implants to be inserted, impression of the stereolithographic model of the middle third of the face with the maxilla extended is recommended, in order to guarantee the execution of the technique in this model. Thus, it may be observed, in the most effective manner, if the case meets all the requisites that have previously been described (Fig. 2).
Fig. 2.
Surgical simulation on stereolithographic model (Prototype of middle third of face, with extended maxilla).
Considering the possibility of immediate loading, this is the time when all the reverse planning is done, such as molding, performing occlusal registering, testing the teeth and finally making the multifunctional surgical guide, which will be used in the trans surgical period and at the time of printing the implants for fabricating the screw-retained, implant-supported hybrid prosthesis, per the Branemark protocol.
1.2. Surgical procedure
The surgery should preferably be performed in hospital under general anesthetic, with nasal intubation [1]. Infiltrative anesthesia with vasoconstrictor must be administered to contain local bleeding and post-operative pain. The pre- and post-operative protocols are the same as those used for zygomatic implant placement surgery.
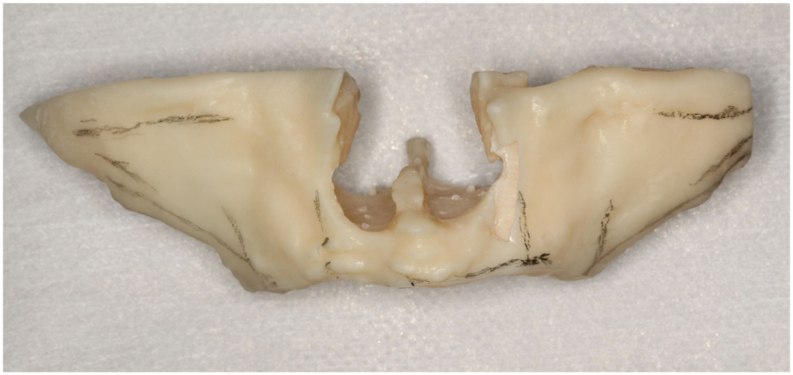
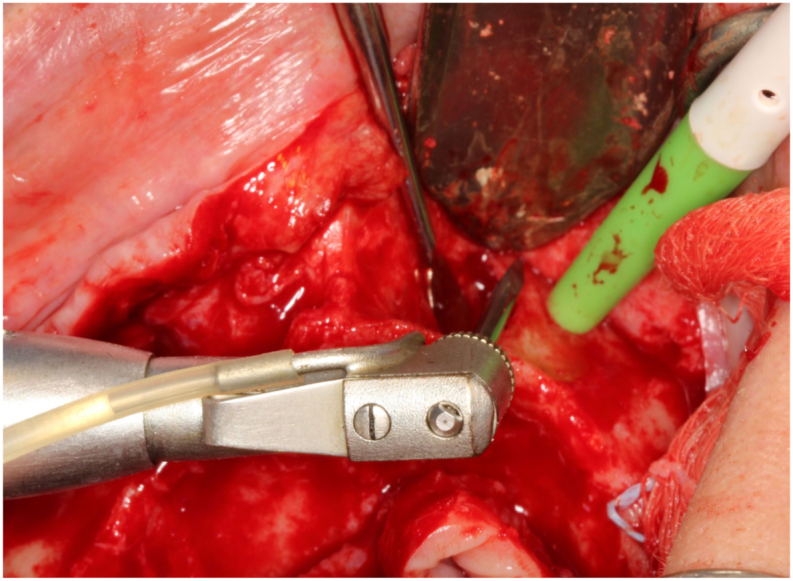
The procedure begins with incision in the midline. After this, a relaxant incision is made on the crest of the alveolar ridge in a slightly palatalized direction in the distal region of the first molars. Subsequently, the palatal and vestibular flap is detached, exposing the nasal cavity, infraorbital foramen and zygomatic bone. On detaching the flap, the lateral portion of the nasal cavity must be detached up to the height of the piriform aperture, exposing the nasal mucosa that is of a more purplish color than the gingival mucosa. With the aid of a Molt maxillary sinus lift detacher and curettes, the distal portion of the nasal mucosa must be detached, exposing the lateral wall and floor of the nasal cavity (Fig. 3). Rupture of the nasal mucosa is not common, because the membrane is thicker than the maxillary sinus. Should this occur, it must be sutured with absorbable thread.
Fig. 3.
Detachment of nasal membrane exposing the lateral wall and floor of the nasal cavity.
Osteotomy must begin with a conventional or palatine approach, as occurs in the other conventional implant placement techniques, using the surgical kit composed of extra-long burs (Helix Compact Surgical Kit GM® Long Neodent®), with perforation speed of 500–800 RPM, starting with the spear that must lightly touch the lateral wall of the nasal cavity, according to the planning in the software (Dentalslice® Bioparts) and must proceed in the direction of the frontal process of the maxilla (Fig. 4). After this, the 2.5 mm and 3.75 mm burs are used. Throughout the entire osteotomy up to insertion of the implant, the nasal membrane must remain withdrawn by means of maxillary sinus lift periosteal elevators or curettes. The implant diameter and thickness are previously selected during the virtual surgeries and those of the prototype, however, the exact size of fixation must be defined only after conclusion of cutting and probing the alveolus. The implant is inserted at a speed of 30 RPM maximum insertion torque of 60 N cm. Due to the small thickness of the frontal process of the maxilla, the recommendation is to use extra-long implants of up to 3.75 mm in diameter and lengths of 20, 22,5 and 25 mm (HelixGM® Long Implants Neodent®). After placement of the implant, the recommendation is to perform particulated bone grafting in the lateral portion and floor of the nasal cavity, to avoid nasal mucosa adherence to the implant threads, and the possibility of their exposure, which would increase the chance of infection, or difficulty in respiratory function (Fig. 5).
Fig. 4.
Osteotomy performed with spear drill placed tangential the lateral wall of the nasal fossa, continuing up to frontal process of the maxilla.
Fig. 5.
5 A. Extra-long transnasal implant inserted (HelixGM® Long Implants Neodent®). 5B Bone graft performed with 80% Hydroxyapatite and 20% Tricalcium Betaphosphate Small (Blue Bone Regener®). (For interpretation of the references to color in this figure legend, the reader is referred to the Web version of this article.)
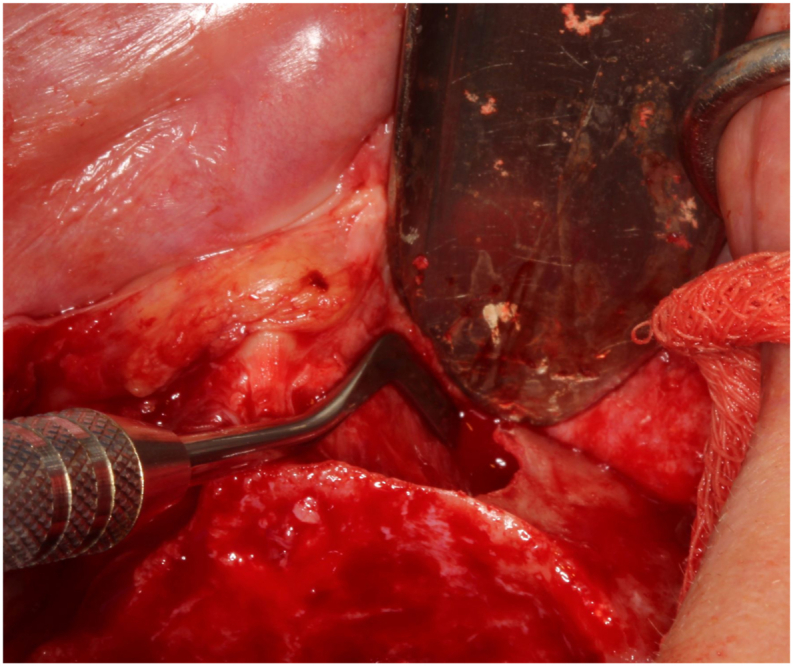
On conclusion of inserting the extra-long transnasal implants, osteotomy is performed for the placement of zygomatic implants. For zygomatic implants placed by the extra-maxillary technique (ZAGA 4), the recommendation is to cover the implant head with buccal fat pad from Bichat's Ball, or connective tissue from the palate to minimize dehiscense of the vestibular tissue, and consequently, exposure of the body and threads of the zygomatic implants [8] (Fig. 6). Immediate loading is performed when the majority of the implants have a minimum insertion torque of 30 N. cm [11], and consequently, the microunit abutments are inserted, transfer impressions are taken with the multifunctional surgical guide, and the screw-retained, implant-supported hybrid prosthesis with cast bar is delivered a few hours after surgery [12]. Final panoramic radiography must be performed to confirm the absence of gap and passiveness of the prosthesis (Fig. 7).
Fig. 6.
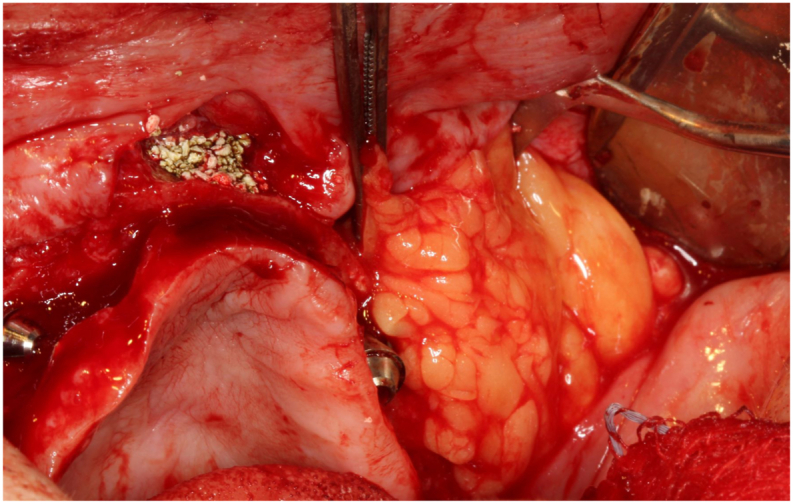
Zygomatic implant head coated with Bichat's Ball.
Fig. 7.
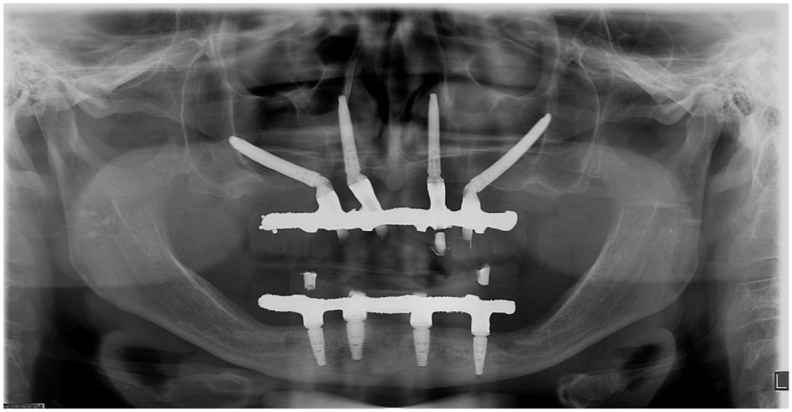
Final panoramic radiograph.
The main complications observed in the post-operative period of patients who received extra-long transnasal implants were transitory paresthesia of the ala of the nose, with the feeling of pins and needles, and tendency to improve in a mean time of 30 days after surgery, nasal oral fistula, this resulted from the excessive amount of biomaterial in the nasal cavity, which disappeared in a period of up to 90 days, and initial transitory difficulty with breathing in patients with deviated nasal septum. The patients showed good tolerance to the implants inserted in the nasal cavity and reported no discomfort or perception of these devices in this anatomic region. No rupture of the nasal membrane was observed or any change within the nasal cavity after insertion of the implants. Care is recommended when detaching the periosteum close to the infra-orbital nerve, placement of sufficient fine grained biomaterial around the transnasal implants to cover them, and placement of transnasal implants as tangentially as possible to the distal bone wall of the nasal cavity, in cases of patients with deviated nasal septum. If a fistula appears, a functional nasal endoscopic exam must be performed by an otorhinolaryngologist physician, to discard the possible occurrence of fenestration of the nasal mucosa and infection around the transnasal implants.
2. Discussion
According to the radiographic zones of bone availability, it will be possible to determine the number of implants to be placed in the maxilla with the type of implant and surgical techniques to be used [10]. When there is sufficient bone volume in zones 1 and 2, it will be possible to plan the placement of implants, which may be straight or inclined [2], with conventional and/or extra-long implants. These two zones allow a wide variation of implant trajectories, ranging from the use of the classical All on 4 [11] technique through to anchorage of implants on points M or V [13,14], by using the paranasal bones of the maxilla. Recently, the use of extra-long nasal implants was proposed, with a trajectory from the distal to mesial region, passing through the maxillary sinus, as an option for zygomatic implants [15].
In the absence of bone tissue in zones 1, 2 and 3 of the maxilla, the placement of 4 zygomatic implants is performed [10]. In spite of being a safe technique and well documented in the literature, it requires more experience of the surgeon, with increase in surgical risks [1,4,5]. An experienced surgeon perforated the orbital cavity in an attempt to place the second zygomatic implant, and reported only a hematoma in the orbit in the post-operative period [4]. There is surgical risk in every procedure, ranging from esthetic surgeries for facial corrections through to the placement of 4 zygomatic implants [5,16].
With a view to diminishing the surgical risk in the placement of 4 zygomatic implants [5], the placement of extra-long transnasal implants must form part of the treatment plan of patients with atrophic maxillae, provided that there is sufficient bone volume for the apical locking of these implants in the frontal process of the maxilla, as described in the indications and surgical technique. The technique is also an option for cases in which the volume of zygomatic bone is insufficient for the placement of 2 zygomatic implants, making it difficult to achieve initial primary stability. This is more common in elderly patients who have low density zygomatic bone [6]. In the presence of bone volume in zone 2 of the maxilla, and absence in zone 1 [10], transnasal implants may be associated with conventional and/or posterior extra-long implants, thereby avoiding the placement of 4 zygomatic implants.
In patients with ZAGA 4 facial anatomy, where there is large concavity of the anterior wall of the maxilla, in which a large part of the zygomatic implant body remains without contact with the bone, and is covered by soft tissue only [7], the technique with use of extra-long transnasal implants allows greater predictability. This arises from the reduced risk of dehiscence of the vestibular tissue and exposure the threads of the zygomatic implant of which, the head will be localized in zone 1 of the maxilla [10]. Finite element studies have shown lower stress on the bone tissue, microunit screws and both zygomatic and conventional implants, when the zygomatic implants placed by the extra-maxillary technique were inserted in the region of the premolar, associated with anterior inclined implants, which in some way resembles the surgical technique presented [2]. We suggest that studies by the finite element method should be conducted, with the purpose of analyzing the stresses generated by extra-long transnasal implants in the adjacent bone tissues, and of the abutments and microunit screws. Moreover, the inclination, length, diameter and localization of extra-long transnasal implants, and their insertion techniques, should be compared with those of zygomatic implants.
Camargo et al. [6] recommended particulated bone grafting before insertion of the transnasal implants. The authors of this article, indicate bone grafting performed (with Small particles of synthetic Hydroxyapatite in the concentration of 80% and 20% Tricalcium Betaphosphate) only after insertion of the implants, for better visualization of their anchorage in the frontal process of the maxilla because otherwise, the trajectory of the implant may undergo change, giving a false impression of anchorage in the frontal process of the maxilla.
It was concluded that the technique of extra-long transnasal implants is a feasible alternative for substituting the insertion of a second zygomatic implant, thereby diminishing the surgical risk, and making it possible for the technique to be more extensively used and performed by a larger number of surgeons.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Sources of funding
None.
Ethical approval
None.
Patient consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contribution
Study design: Paulo H. T. Almeida. Data collection: Paulo H. T. Almeida. Data analysis: Paulo H. T. Almeida, Ayrton Arcazas Junior. Manuscript preparation: Paulo H. T. Almeida. Critical revision: Paulo H. T. Almeida, Sergio H. Cacciacane and Ayrton Arcazas Junior.
Research registration
None.
Guarantor
Paulo Henrique Teles de Almeida.
Declaration of competing interest
None.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.amsu.2021.102635.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Almeida P.H., Salvoni A.D., França F.M. Evaluation of satisfaction of individuals rehabilitated with zygomatic implants as regards anesthetic and sedative procedure: a prospective cohort study. Ann Med Surg. (Lond) 2017;22:22–29. doi: 10.1016/j.amsu.2017.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Almeida P.H., Cacciacane S.H., França F.M. Stresses generated by two zygomatic implant placement techniques associated with conventional inclined anterior implants. Ann. Med. Surg. 2018;30:22–27. doi: 10.1016/j.amsu.2018.04.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Davo R., David L. Quad zygoma: technique and realities. Oral Maxillofac. Surg. Clin. 2019;31:285–297. doi: 10.1016/j.coms.2018.12.006. [DOI] [PubMed] [Google Scholar]
- 4.Davo R., Pons O., Rojas J., Carpio E. Immediate function of four zygomatic implants: a 1-year report of a prospective study. Eur. J. Oral Implant. 2010;3(4):323–334. [PubMed] [Google Scholar]
- 5.Campa O.V., Vrielincka L., Gemels B., Politis C. Intraorbital hemorrhage following a secondary intervention at integrated zygomatic implants: a case report. International Journal of Surgery Case Reports. 2018;43:21–24. doi: 10.1016/j.ijscr.2018.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Camargo V.B., Baptista D., Manfro R. Implante transnasal (Técnica Vanderlim) como opção ao segundo implante zigomático. Coppedê A. Soluções clínicas para reabilitações totais sobre implantes sem enxertos ósseos. 2019:198–214. São Paulo: Quintessence. [Google Scholar]
- 7.Aparicio C., Manresa C., Francisco K., Claros P., Alández J., González-Martin O., Albrektsson T. Zygomatic implant: indications, techniques and outcomes, and the zygomatic success code. Periodontology. 2000;66:41–58. doi: 10.1111/prd.12038. 2014. [DOI] [PubMed] [Google Scholar]
- 8.Aparicio C., Antonio S. Zygoma anatomy-guided approach “scarf graft” for prevention of soft tissue dehiscense around zygomatic implants: technical note. Int. J. Oral Maxillofac. Implants. 2020;35:e21–e26. doi: 10.11607/jomi.8065. [DOI] [PubMed] [Google Scholar]
- 9.Agha R.A., Franchi T., Sohrabi C., Mathew G., for the SCARE Group The SCARE 2020 guideline: updating consensus surgical case report (SCARE) guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 10.Bedrossian E., Sullivan R.M., Fortin Y., Maló P., Indresano T. Fixed-prosthetic implant restoration of the edentulous maxila: a systematic pretreatment evaluation method. J. Oral Maxillofac. Surg. 2008;66:112–122. doi: 10.1016/j.joms.2007.06.687. [DOI] [PubMed] [Google Scholar]
- 11.Maló P., Lopes A., Nobre M.A., Ferro A. Immediate function dental implants inserted with less than 30 n°cm of torque in full-arch maxillary rehabilitations using the all-on-4 concept: retrospective study. Int. J. Oral Maxillofac. Surg. 2018;47:1079–1085. doi: 10.1016/j.ijom.2018.04.008. [DOI] [PubMed] [Google Scholar]
- 12.Almeida P.H., Cacciacane S.H., Arcazas Junior A. Ten-Year follow-up of treatment with zygomatic implants and replacement of hybrid dental prosthesis by ceramic teeth: a case report. Ann Med Surg. (Lond) 2020;50:1–5. doi: 10.1016/j.amsu.2019.11.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jensen O.T., Adams M.W. The maxillary m-4: a technical and biomechanical note for all-on-4 management of severe maxillary atrophy–report of 3 cases. J. Oral Maxillofac. Surg. 2009;67(8):1739–1744. doi: 10.1016/j.joms.2009.03.067. [DOI] [PubMed] [Google Scholar]
- 14.Jensen O.T., Adams M.W., Smith E. Paranasal bone: the prime factor affecting the decision to use transsinus vs zygomatic implants for biomechanical support for immediate function in maxillary dental implant reconstruction. Int. J. Oral Maxillofac. Implants. 2014 Jan-Feb;29(1):e130–e138. doi: 10.11607/jomi.te52. [DOI] [PubMed] [Google Scholar]
- 15.Nicoli G., Piva S., Ferraris P., Nicoli F., Jensen O.T. Extra-long nasal wall– directed dental implants for maxillary complete arch immediate function: a pilot study. Oral Maxillofac. Surg. Clin. 2019;31:349–356. doi: 10.1016/j.coms.2019.01.004. [DOI] [PubMed] [Google Scholar]
- 16.Almeida P.H. Peer review report 3 on “in-hospital surgical treatment for haemorrhage after aesthetic mandibular osteotomy performed as an office-based day surgery”. Ann Med Surg. (Lond) 2017;13:284–285. doi: 10.1016/j.amsu.2017.10.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.