Abstract
Background
Coronavirus Disease 2019 (COVID-19) has infected more than 5 million and lost the lives of more than 300 thousand people globally. It is the first-ever deadly pandemic with a significant degree of fear, worry and concern in the population at large. Therefore, this Meta-Analysis aims to assess the global prevalence and determinants of mental health disorders.
Methods
A three-stage search strategy was conducted on PubMed/Medline, Science direct LILACS and PsycINFO databases. The Heterogeneity among the included studies was checked with forest plot, χ2 test, I2 test, and the p-values. Publication bias was checked with a funnel plot and the objective diagnostic test was conducted with Egger's correlation, Begg's regression tests, and Trim and fill method.
Results
The Meta-Analysis revealed that the pooled prevalence of anxiety and depression 33.59% (95% confidence interval (CI): 27.21 to 39.97, 30 studies, 88,543 participants) and 29.98% (95% confidence interval (CI): 25.32 to 34.64, 25 studies, 78,191 participants) respectively.
Conclusion
The review revealed that more than thirty percent of patients developed anxiety and depression during COVID-19 Pandemic. This presages the health care stakeholders to prevent and intervene in mental health disorders.
Registration
This review was registered in Prospero international prospective register of systematic reviews (CRD42020183146).
Keywords: Coronavirus, COVID-19, Anxiety, Depression, Global
Highlights
-
•
This Meta-analysis revealed that depression and anxiety were very high among the students
•The Meta-analysis revealed that the risk of depression was associated with occupation and comorbidity.
•The review also showed that anxiety was increased by eighty-eight percent in female as compared to males
•This study presages the health care stakeholders to prevent and manage long term implications of mental health disorders.
1. Introduction
Severe acute respiratory syndrome (SARS-CoV-2) belongs to a group of viruses that cause Coronavirus disease 2019 (COVID-19) which affects the respiratory, gastrointestinal, liver and central nervous system of humans, livestock, bats, mice and another wild animals [1,2]. The World Health Organization (WHO) officially declared the COVID-19 epidemic as a public health emergency of international concern as of January 30, 2020 [3,4]. COVID-19 has affected more than 213 countries and regions worldwide (a total of five million and above confirmed cases, and cumulative deaths reached 300 and above deaths) [5].
As the COVID-19 pandemic rapidly sweeps across the world, it is inducing a considerable degree of fear, worry and concern in the population at large and among certain groups in particular, such as older adults, care providers and people with underlying health conditions [6,7].
The COVID-19 poses challenges in all aspects of life including mental health for the entire human race [8,9]. During a pandemic, the number of people whose mental health is affected tends to be greater than the number of people affected by the infection [10].
The increasing mental health burden during the COVID-19 outbreak, there have been increasing calls for enhanced mental health support [3,[9], [10], [11], [12]]. Emotions can be amplified by pre-existing depressive and anxiety disorders, contributing to the increased rumination of contracting the disease, and this can profoundly remodel people's behaviour and social interaction with others. Internationally, stigma and blame targeted at communities affected by the outbreak by other countries due to a fear of infection impedes cross-national trade, fueling further unrest (3).
Novel coronavirus pandemic is associated with shorter and long term mental health problems ranging from minor to severe mental illnesses as depicted with studies conducted since the first coronavirus outbreak in 2002 in China. Studies showed that the psychological impact of the novel coronavirus pandemic is was very high [4,13,14].
A cross-sectional study conducted by Naser et al. in Jordan among the general population, health care providers and University students to assess the mental health status revealed that the prevalence of overall depression was 23.8% and among which 11.3% was observed among health care providers [15].
Another study conducted by Zhang et al. in China among medical health workers on mental health and psychosocial related with COVID-19 showed that the prevalence of insomnia, anxiety, depression and somatization was (38.4 vs. 30.5%), (13.0 vs. 8.5%) (12.2 vs. 9.5%), and (1.6vs. 0.4%) respectively as compared to non-healthcare providers [16]. The other finding of the study was conducted in China by Wang C et al. (53.8%) [17]. On the other hand, a study done in china Wuhan by Dai Y et al. was (39.1% vs 51.6%) [18].
A study conducted by Liu et al. in China among 4976 doctors and nurses to assess the impacts of COVID-19 on Mental health showed that the prevalence of psychological distress, anxious symptoms, and depressive symptoms were 15.9%, 16.0%, and 34.6% respectively [19]. However, another study conducted in Singapore by Benjamin et al. among 490 health care providers to investigate the psychological impacts of COVID-19 outbreak showed that the prevalence of anxiety was higher among nonmedical health care workers than medical personnel (20.7% versus 10.8% [20].
The clinical characteristics of psychological distress have not been well established across the populations affected by the COVID-19 pandemic, although a generally increased level of mental distress has been reported from both the general public and frontline personnel [21].
Several studies showed that female gender is identified for the development of depression, anxiety and other mental illness in patients with COVID-19 [15,16,20,22,23].
A study conducted in China revealed that the majority of respondents were in the age range of 21.4–30.8 years (53.1%) and married (76.4%) [17]. Also, a study conducted in China which was six to ten years 1960 (45%) [18].
A cross-sectional study conducted in China by Zhang et al. among medical health workers on mental health and psychosocial problems showed that living in rural areas, at risk of contact with COVID-19 patients were the most common risk factors for insomnia, anxiety, obsessive-compulsive symptoms, and depression (16).
Another study conducted in Singapore by Benjamin et al. on Psychological impacts of COVID-19 pandemic on health workers showed that mental health problems were associated with married and those with co-morbidities [20].
Another study conducted in Vietnam by Nguyen et al. among 3497 participants to identify the independent predictors of depression among COVID-19 patients revealed that depression was more likely in patients with older patients aged greater than 60 years, higher educational attainments, presence of morbidities, low social status and low physical activity [24].
A cross-sectional study conducted in Jordan by Naser et al. on the mental health status of the general population, health care workers and university students revealed that mental health problems were more likely in divorced participants among the general population and University Students with a history of chronic disease and those with high income (≥1500 JD) were at higher risk of developing anxiety [15].
Another study conducted in China by Ahmed on Epidemic of COVID-19 and associated Psychological Problems showed that young people aged 21–40 years; alcohol use and low mental well-being were more likely to develop mental health problems [[15], [16], [20], [22], [23]]. A study conducted in China by Kong et al. among Hospitalized Patients with COVID-19 to investigate the prevalence and factors associated with Depression and Anxiety showed that low social support, older age groups were more likely to develop anxiety and depression [22]. Today, evidence on prevalence and determinates of anxiety and depression among the general population is still in demand. Therefore, it is vital to conduct this Systematic Review and Meta-analysis is intended to provide evidence on prevalence and determinates of anxiety and depression among the general population globally.
2. Methods
2.1. Protocol and registration
The systematic review and meta-analysis was conducted based on the Preferred Reporting Items for Systematic and meta-analysis (PRISMA) protocols [25], and the Meta-analysis Of Observational Studies in Epidemiology (MOOSE) checklist [26]. This systematic review and meta-analysis were registered in Prospero international prospective register of systematic reviews (CRD42020183146).
2.2. Eligibility criteria
2.2.1. Types of studies
All cross-sectional studies assessing the prevalence of anxiety and depression among the general population without any language restriction from December 2019 up to April 2020 were incorporated.
2.2.2. Types of participants
The participants were all age groups of the population.
2.2.3. Outcomes of interest
The primary outcome of interest was the prevalence of anxiety and depression among the general population. Sociodemographic characteristics, social history, presence of comorbidities, history of pre-existing mental health disorders were determinants of preoperative anxiety.
2.2.4. Context
This systemic review and Meta-Analysis incorporated observational studies conducted globally and reporting the prevalence of anxiety and depression among the general population during COVID-19 pandemic.
2.2.5. Inclusion criteria
All observation (cross-sectional, case series, Cohort and case-control) studies assessing the prevalence and associated factors of anxiety and depression among the general population from December 2019 to April 2020 without language restriction which were published and unpublished articles conducted globally were included.
2.2.6. Exclusion criteria
Studies other than cross-sectional studies, studies that didn't report the prevalence of anxiety and depression, and cross-sectional studies scored less than fifty percent on quality assessment were excluded.
2.3. Search strategy
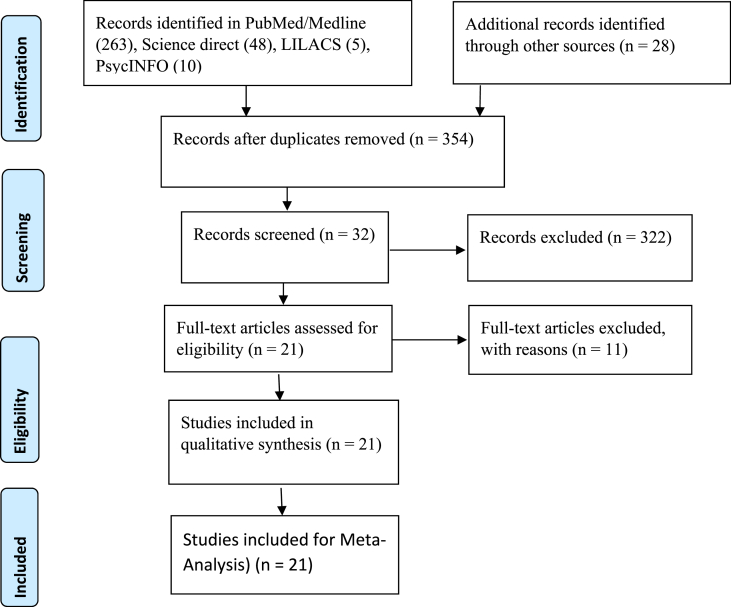
The search strategy was intended to explore all available published and unpublished studies on the prevalence of anxiety and depression among the general population globally. A three steps search strategy was employed in this review. An initial search on PubMed/Medline, Science direct LILACS and PsycINFO databases were carried out followed by an analysis of the text words contained in Title/Abstract and indexed terms. A second search was undertaken by combining free text words and indexed terms with Boolean operators. The third search was conducted with the reference lists of all identified reports and articles for additional studies. Finally, the additional and grey literature search was conducted on Google scholars up to ten pages. The result of the search strategy was presented with the Prism flow chart (Figure- 1).
2.4. Data extraction
The data from each individual study were extracted by SM and YA independently with Microsoft excel format and imported for analysis in R software version 3.6.1 and STATA version 16. Authors, publication year, mean age of participants, Country, events of anxiety, events of depression, sample size and events in each risk factor for factor analysis were extracted.
2.5. Assessment of methodological quality
Articles identified for retrieval were assessed by two independent Authors for methodological quality before inclusion in the review using a standardized critical appraisal Tool adapted from the Joanna Briggs Institute (Supplemental Table 1). The disagreements between the Authors appraising the articles were resolved through discussion. Articles with average scores greater than fifty percent were included for data extraction. The quality of this systematic review was evaluated with the Assessment of Multiple Systematic Reviews 2 (AMSTAR2) checklist [27].
2.6. Data analysis
The pooled prevalence of anxiety and depression were determined with a random effect model as there was substantial heterogeneity. The Heterogeneity among the included studies was checked with forest plot, χ2 test, I2 test, and the p-values. Substantial heterogeneity among the included studies was investigated with subgroup analysis and meta-regression. Sensitivity analysis was done to evaluate the influential studies and further analysis was made after removing the outliers.
Publication bias was checked with a funnel plot and the objective diagnostic test was conducted with Egger's correlation, Begg's regression tests, and Trim and fill method. Furthermore, moderator analysis was carried out to identify the independent predictors of the prevalence of preoperative anxiety among surgical patients.
3. Results
3.1. Description of included studies
A total of 354 articles were identified from different databases as described in the methodology section with the Prisma flow diagram (Fig. 1). Thirty-two articles were selected for evaluation after the successive screening. Twenty-one Articles with 72, 999 participants assessing the prevalence and determinants of anxiety and depression as a primary outcome among the general population were included (Table 1) and the rest were excluded with reasons [[28], [29], [30], [31], [32], [33], [34], [35], [36], [37], [38]].
Fig. 1.
Prisma flow chart.
Table 1.
Description of included studies.
| Author | Year | Sample | Country | Population | Quality score | Design |
|---|---|---|---|---|---|---|
| Ahmed et al.(23) | 2020 | 1074 | China | general population | 8 | online survey |
| Alenazi et al. [39] | 2020 | 4920 | Saudi | health workers | 4 | cross-sectional |
| Burhamah et al. [40] | 2020 | 4132 | Lebanon | General population | 6 | online survey |
| Chew et al. [41] | 2020 | 906 | Singapore | health workers | 7 | cross-sectional |
| Chi et al. [42] | 2020 | 2038 | China | Students | 4 | online survey |
| Cortes et al. [43] | 2020 | 1105 | Mexican | General population | 4 | online survey |
| Dai et al.(18) | 2020 | 4357 | China | general population | 6 | online survey |
| Ettman et al. [44] | 2020 | 1470 | USA | general population | 4 | online survey |
| Fu et at [45] | 2020 | 1242 | China | General population | 4 | online survey |
| González et al. [46] | 2020 | 3550 | Spain | health workers | 5 | online survey |
| Huang et al. [47] | 2020 | 7236 | China | general population | 7 | online survey |
| Kazmi et al. [48] | 2020 | 1000 | India | general population | 5 | online survey |
| Kong et al.(22) | 2020 | 144 | China | general population | 6 | cross-sectional |
| Lai et al. [49] | 2020 | 1257 | China | general population | 8 | cross-sectional |
| Li et al. [50] | 2020 | 398 | China | General population | 5 | online survey |
| Liang et al. [51] | 2020 | 864 | China | Women | 4 | cross-sectional |
| Liu et al. [52] | 2020 | 285 | China | Patients | 5 | cross-sectional |
| Liu et al. [53] | 2020 | 512 | China | medical workers | 5 | cross-sectional |
| Ma et al. [54] | 2020 | 770 | China | Patents | 5 | online survey |
| Mansourieh [55] | 2020 | 7173 | Iran | Family of health workers | 6 | online survey |
| Maroufizadeh et al. [56] | 2020 | 5328 | Iran | general population | 7 | cross-sectional |
| Naser et al.(15) | 2020 | 4126 | Jordan | health workers | 6 | cross-sectional |
| Nguyen et al. [24] | 2020 | 3942 | Vietnam | health workers | 6 | cross-sectional |
| Peng et al. [57] | 2020 | 2237 | China | General population | 5 | |
| Pisano et al. [58] | 2020 | 5989 | Italy | health workers | 6 | online survey |
| Que et al. [59] | 2020 | 2285 | China | health workers | 5 | |
| Rossi et al. [60] | 2020 | 18,147 | Italy | general population | 8 | online survey |
| Shevlin et al. [61] | 2020 | 2025 | United Kingdom | health workers | 6 | online survey |
| Sun et al. [62] | 2020 | 2091 | China | Patients | 7 | cross-sectional |
| Tadesse et al. [63] | 2020 | 408 | Ethiopia | Students | 8 | Cross-sectional |
| Wang et al. [17] | 2020 | 1738 | China | general population | 5 | cross-sectional |
| Ying et al. [64] | 2020 | 822 | China | general population | 8 | cross-sectional |
| Zhang et al. [65] | 2020 | 1563 | China | general population | 7 | online survey |
| Zhu et al. [19] | 2020 | 5062 | China | general population | 6 | online survey |
The included studies were published from January 29 to April 17, 2020, with sample size ranged from 144 to 18,147. The twenty-two included studies were conducted in CHINA (12 studies), India (1 study), Iran (one study), Italy (2 studies), Jordan (1 studies), Singapore (1 study), Spain (1 studies), United Kingdom (1 study) and Vietnam (1 study).
The majority of included studies were conducted on depression and anxiety (seventeen studies) while two studies were conducted to assess only post-traumatic stress syndrome and the other two were conducted with only anxiety.
Twelve studies were conducted on the general population while six studies were conducted among health care workers and other four studies were conducted among patient, children and health care worker families.
The majority of included studies identified the possible risk factors of anxiety and depression among the population which includes but not limited to gender, age, marital status, educational level, and occupation.
4. Meta-analysis
This systematic review and Meta-Analysis was intended to provide evidence on anxiety, depression and its determents among the general population. Eighteen of the included studies reported the prevalence of anxiety and depression.
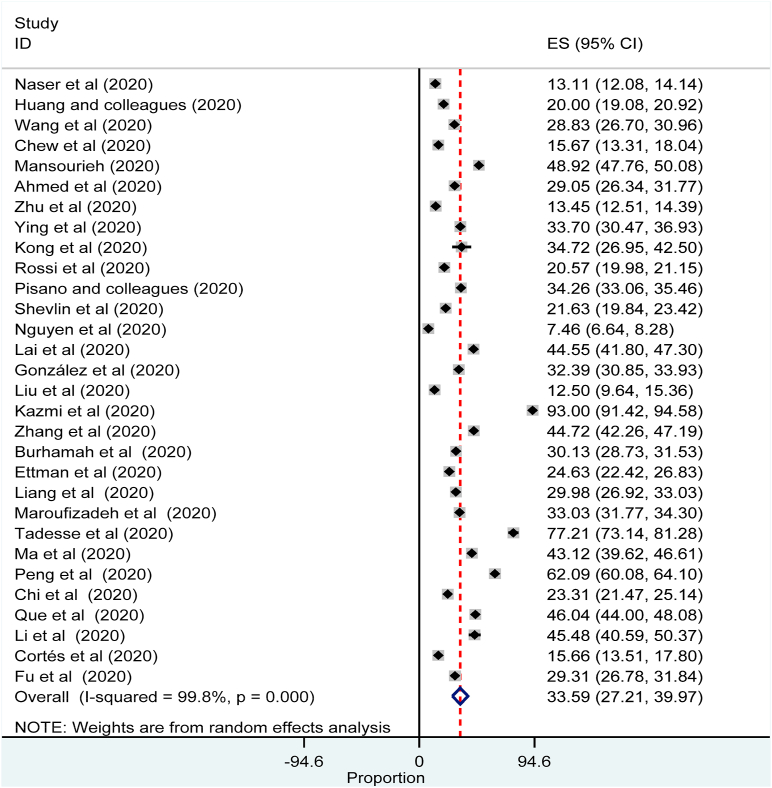
The pooled prevalence of depression during COVID-19 Pandemic was 33.59% (95% confidence interval (CI): 27.21 to 39.97, 30 studies, 88,543 participants (Fig. 2).
Fig. 2.
Forest plot for the prevalence of depression among the general population: The midpoint of each line illustrates the prevalence; the horizontal line indicates the confidence interval, and the diamond shows the pooled prevalence.
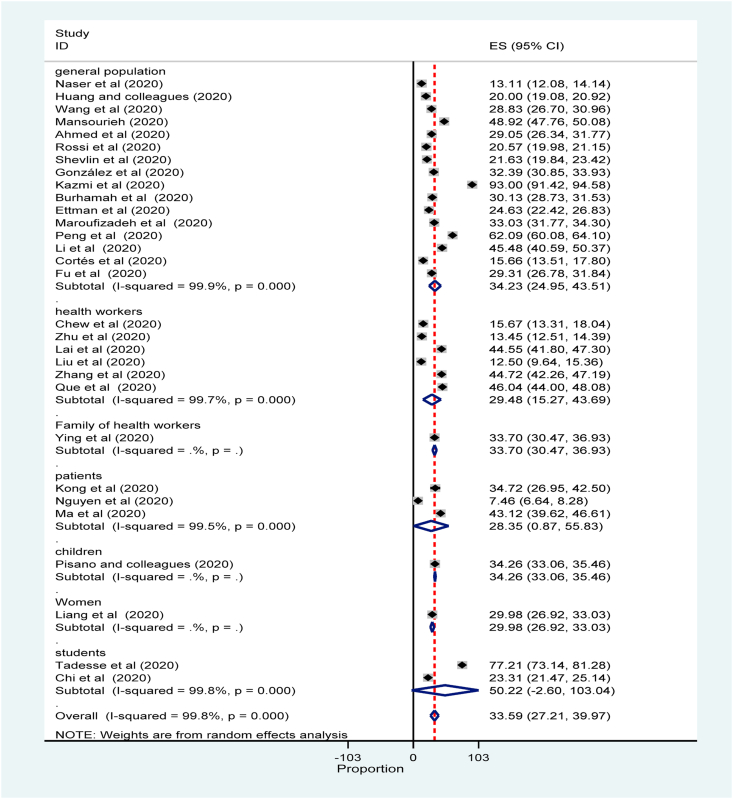
The subgroup Analysis by population revealed that prevalence of depression among the general population was 34.23% (95% confidence interval (CI): 24.95 to 43.51) while the prevalence of depression among students and children were 50.22% (95% confidence interval (CI): 2.6 to 103.04) and 34.26% (95% confidence interval (CI): 33.06 to 35.46) respectively (Fig. 3).
Fig. 3.
Forest plot for subgroup analysis of the prevalence of depression by population: The midpoint of each line illustrates the prevalence; the horizontal line indicates the confidence interval; the diamond shows the pooled prevalence.
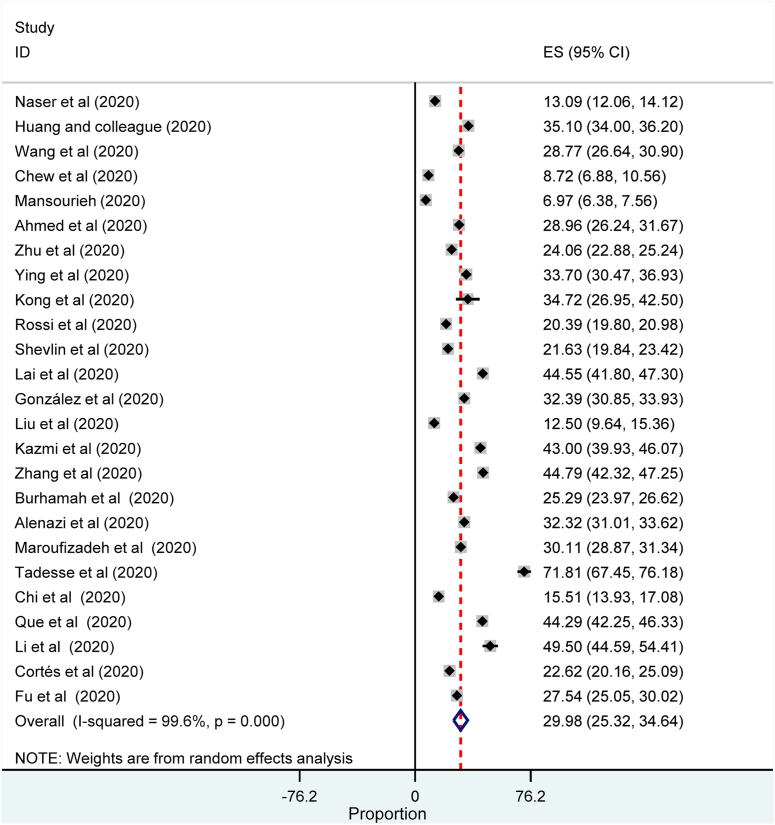
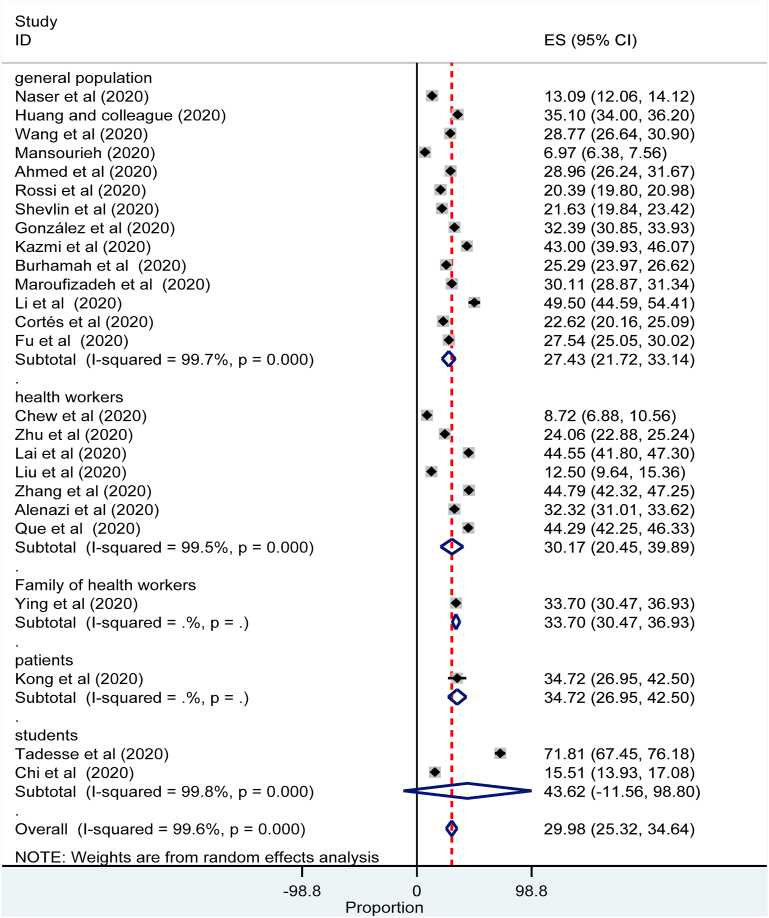
The Meta-Analysis revealed that the prevalence of anxiety during COVID-19 pandemic was 29.98% (95% confidence interval (CI): 25.32 to 34.64, 25 studies, 78,191 participants) (Fig. 4).
Fig. 4.
Forest plot for the prevalence of anxiety among the general population: The midpoint of each line illustrates the prevalence; the horizontal line indicates the confidence interval, and the diamond shows the pooled prevalence.
Subgroup analysis by population revealed that the prevalence of anxiety was the highest among students 43.62% ((95% confidence interval (CI): 11.56 to 98.80) followed by patients 34.72% (95% confidence interval (CI): 26.95 to 42.50) (Fig. 5).
Fig. 5.
Forest plot for subgroup analysis of the prevalence of anxiety by population: The midpoint of each line illustrates the prevalence; the horizontal line indicates the confidence interval; the diamond shows the pooled prevalence.
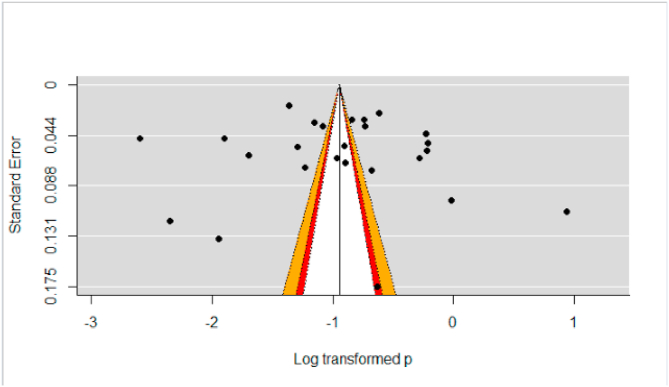
The funnel plot for evaluation of publication bias didn't show asymmetric funnel plot. Besides, the rank correlation and Egger's regression test didn't show a significant difference for small study effect of anxiety (p-value >0.05) (Fig. 6).
Fig. 6.
Funnel plot to assess publication bias. The vertical line indicates the effect size whereas the diagonal line indicates the precision of individual studies with a 95% confidence interval.
The funnel plot for evaluation of publication bias didn't show asymmetric funnel plot. Besides, the rank correlation and Egger's regression test didn't show a significant difference for small study effect of depression (p-value >0.05) (Supplemental Fig. 1).
4.1. Determinants of mental health Disorders(Anxiety and depression)
Literature mentioned different types of risk factors of anxiety and depression population despite the presence of inconclusive evidence on the major independent predictors of anxiety and depression. The most commonly mentioned risk factors of anxiety include gender, marital status, educational level and occupation. On the other hand, the most commonly mentioned risk factors of depression included marital status, occupation and comorbidity.
The systematic review and Meta-Analysis revealed that being female was the risk of anxiety was increased by eighty-eight percent as compared to counterpart males, OR = 1.12 (95% confidence interval (CI: 1.0 to 1.3, ten studies). The systematic review also showed that the risks of anxiety were associated with marital status, occupation and educational level with OR = 1.26 (95% confidence interval (CI): 1.0 to 1.8, four studies), OR = 1.1 (95% confidence interval (CI): 1.0 to 1.2, three studies), and OR = 1.1 (95% confidence interval (CI): 1.0 to 1.2, three studies) respectively (Supplemental Fig. 2).
The systematic review also showed that being married increased the risk of depression by eighty-two percent as compared to singles, OR = 1.18 (95% confidence interval (CI): 0.93 to 1.50, four studies). The systematic review and meta-analysis revealed that the risk of depression was associated with occupation and comorbidity OR = 1.16 (95% confidence interval (CI): 0.86 to 1.6, three studies) and OR = 1.84 (95% confidence interval (CI): 1.41 to 2.41, four studies) respectively (Supplemental Fig. 3).
5. Discussion
The mental health problems of the community during an outbreak crisis are a huge health care issue that necessitates prevention and early intervention [9,66,67].
This systematic review and Meta-Analysis revealed that the pooled prevalence of anxiety and depression were as high as 27% (95% confidence interval (CI): 21 to 33) and 32% (95% confidence interval (CI): 23 to 40) respectively which is in line with the majority of included studies (17, 19, 22, 23, 37, 46, 47, 58, 61, 64).
The prevalence of anxiety and depression in this systematic review and Meta-Analysis is higher than another systematic review and Meta-Analysis conducted among on health care worker during the COVID-19 pandemic, SARS and MERS outbreaks, 27% (95% confidence interval (CI): 14 to 40) and 26% (95% confidence interval (CI): 12 to 40) VS 14.8% (95% confidence interval (CI): 11.1 to 19) and 14.9% (95% confidence interval (CI): 12.1 to 18.2) respectively. This discrepancy might be explained by the inclusion of plenty of case reports and studies from previous coronavirus outbreaks from China and Arabian regions [68].
The subgroup analysis by population revealed that the prevalence of anxiety and depression were the highest among patients with COVID-19 followed by families’ of health care workers, health workers and the general population. However, the majority of included studies reported that mental health problems were more prevalent in health care workers [11,16,19,49] as compared to others (23, 46, 47, 61). This discrepancy might be due to the inclusion of the small number of studies assessing the prevalence of anxiety among patients with COVID-19 where in our case, there was only one study.
This Systematic Review identified the independent predictors of anxiety and depression among the population during the COVID-19 pandemic. Female gender, health care workers, married marital status and higher educational level were independent predictors of anxiety while ageing less than forty and comorbidity decrease the risk of developing anxiety. Also, marital status, health care workers, and comorbidity were independent predictors of depression while ageing less than forty and female gender reduction the risk of developing depression.
5.1. Quality of evidence
The systematic review and meta-analysis included plenty of studies with adequate sample size. The methodological quality of included studies was moderate to high quality as depicted with Joanna Briggs Institute assessment tool for meta-analysis of cross-sectional studies. However, substantial heterogeneity associated with dissimilarities of included studies of general populations, settings, location and anxiety and depression assessment tools which entail further observational and randomized controlled trials by controlling potential confounders.
5.2. Limitation of the study
The review incorporated plenty of studies with a large number of participants but the majority of studies included in this review didn't report risk determinants for factor analysis. The included studies were conducted in a different setting, and population which caused substantial heterogeneity. Besides, there were a limited number of studies in some countries and it would be difficult to provide conclusive evidence with results pooled from a fewer study.
5.3. Implication for practice
Evidence revealed that the global prevalence of anxiety and depression during COVID-19 is very high. If these acute mental health problems are left untreated early, there could be huge long term mental, social and economic impacts of the community.
This day, people who seek mental health care might not visit the health institutions due to fear of the deadly COVID-19 pandemic, lack of awareness about mental health problems, reduced delivery care system, poor perception of mental health care and inadequate mental health care. Therefore, mental health care advocacy to the community is required to prevent and intervene in mental health problems.
5.4. The implication for further research
The meta-analysis revealed that the prevalence of anxiety and depression were very high and the major independent predictors of anxiety and depression were outlined. However, the included studies were too heterogeneous and cross-sectional studies also don't show the temporal relationship between anxiety and depression and their determinants. Therefore, further observational and randomized controlled trials are in demand on COVID-19 by stratifying the possible independent predictors.
6. Conclusion
The global prevalence of anxiety and depression among the general population was very high which entails special attention. The Meta-Analysis revealed that the prevalence of anxiety and depression was the highest inpatient followed by the family of health workers while the lowest was seen in the general population followed by health workers.
The Meta-analysis revealed that gender, marital status, occupation and educational level were showed significant predictors of anxiety; but the independent variables age and comorbidity were not showed significant predictors of anxiety.
The systematic review and meta-analysis also showed that marital status, occupation and comorbidity were revealed significant predictors of depression; but the independent predictor's age and gender were not showed significantly associated predictors of depression.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and materials
Data and material can be available where appropriate.
Funding
No funding was obtained from any organization.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Authors' contributions
SA and YC conceived the idea design of the project. SA, YC, BB, SN, and BM were involved in searching strategy, data extraction, quality assessment, analysis, and manuscript preparation. All authors read and approved the manuscript.
Declaration of competing interest
The authors declare that there are no competing interests.
Acknowledgments
The authors would like to acknowledge Dilla University for technical support and encouragement to carry out the project.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.amsu.2021.102634.
Abbreviation
- OR
Odd Ration
- CI
Confidence Interval
- COVID-19
Coronaviruses Disease 19
- HCWs
Health Care Worker
- LILACS
LatinAmerican and the Caribbean on Health Sciences Literature
- MERS
the Middle East respiratory syndrome
- PsycINFO
Psychological Information Database
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- SARS
Severe Acute Respiratory Syndrome
- WHO
World Health Organization
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Xu J., Zhao S., Teng T., Abdalla A.E., Zhu W., Xie L. Systematic comparison of two animal-to-human transmitted human coronaviruses: SARS-CoV-2 and SARS-CoV. Viruses. 2020;12(2):244. doi: 10.3390/v12020244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Perico L., Benigni A., Remuzzi G. Should COVID-19 concern nephrologists? Why and to what extent? The emerging impasse of angiotensin blockade. Nephron. 2020;144(5):213–221. doi: 10.1159/000507305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ho C.S., Chee C.Y., Ho R.C. Mental health strategies to combat the psychological impact of COVID-19 beyond paranoia and panic. Ann. Acad. Med. Singapore. 2020;49(1):1–3. [PubMed] [Google Scholar]
- 4.Guo Y.-R., Cao Q.-D., Hong Z.-S., Tan Y.-Y., Chen S.-D., Jin H.-J. The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak–an update on the status. Military Medical Research. 2020;7(1):1–10. doi: 10.1186/s40779-020-00240-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Organization WH Coronavirus disease 2019 (COVID-19): situation report. 2020;70 [Google Scholar]
- 6.April KM. Class and race inequality, health, and COVID-19.
- 7.Faiq M., Kumar A., Singh H., Pareek V., Qadri R., Raza K., Kumari C., Narayan R., Kumar P., Kulandhasamy M., Pandey S. Preprints; 2020. COVID-19: a review on molecular basis, pathogenic mechanisms, therapeutic aspects and future projections. 2020040091. [DOI] [Google Scholar]
- 8.Jiloha R. COVID-19 and mental health. Epidemiology International (E-ISSN: 2455-7048) 2020;5(1):7–9. [Google Scholar]
- 9.Holmes E.A., O'Connor R.C., Perry V.H., Tracey I., Wessely S., Arseneault L., Ballard C., Christensen H., Silver R.C., Everall I., Ford T. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. The Lancet Psychiatry. 2020 Jun 1;7(6):547–560. doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ornell F., Schuch J.B., Sordi A.O., Kessler F.H. "Pandemic fear" and COVID-19: mental health burden and strategies. Braz. J. Psychiatr. 2020 Jun;42(3):232–235. doi: 10.1590/1516-4446-2020-0008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Li W., Yang Y., Liu Z.-H., Zhao Y.-J., Zhang Q., Zhang L. Progression of mental health services during the COVID-19 outbreak in China. Int. J. Biol. Sci. 2020;16(10):1732. doi: 10.7150/ijbs.45120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yao H., Chen J.-H., Xu Y.-F. Patients with mental health disorders in the COVID-19 epidemic. The Lancet Psychiatry. 2020;7(4):e21. doi: 10.1016/S2215-0366(20)30090-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mak I.W.C., Chu C.M., Pan P.C., Yiu M.G.C., Chan V.L. Long-term psychiatric morbidities among SARS survivors. Gen. Hosp. Psychiatr. 2009;31(4):318–326. doi: 10.1016/j.genhosppsych.2009.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Maunder R.G., Lancee W.J., Balderson K.E., Bennett J.P., Borgundvaag B., Evans S. Long-term psychological and occupational effects of providing hospital healthcare during SARS outbreak. Emerg. Infect. Dis. 2006;12(12):1924. doi: 10.3201/eid1212.060584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Naser A.Y., Dahmash E.Z., Al-Rousan R., Alwafi H., Alrawashdeh H.M., Ghoul I., Abidine A., Bokhary M.A., AL-Hadithi H.T., Ali D., Abuthawabeh R. Mental health status of the general population, healthcare professionals, and university students during 2019 coronavirus disease outbreak in Jordan: across-sectional study. Brain Behav. 2020 Aug;10(8):e01730. doi: 10.1002/brb3.1730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhang W-r, Wang K., Yin L., Zhao W-f, Xue Q., Peng M. Mental health and psychosocial problems of medical health workers during the COVID-19 epidemic in China. Psychother. Psychosom. 2020:1–9. doi: 10.1159/000507639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Publ. Health. 2020;17(5):1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dai Y., Hu G., Xiong H., Qiu H., Yuan X. Psychological impact of the coronavirus disease 2019 (COVID-19) outbreak on healthcare workers in China. medRxiv. 2020 doi: 10.1101/2020.03.03.20030874. [DOI] [Google Scholar]
- 19.Zhu Z., Xu S., Wang H., Liu Z., Wu J., Li G. COVID-19 in Wuhan: sociodemographic characteristics and hospital support measures associated with the immediate psychological impact on healthcare workers. Eclinical Medicine. 2020;24:100443. doi: 10.1016/j.eclinm.2020.100443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Prasitlumkum N., Chokesuwattanaskul R., Thongprayoon C., Bathini T., Vallabhajosyula S., Cheungpasitporn W. Incidence of myocardial injury in COVID-19-infected patients: a systematic review and meta-analysis. Diseases. 2020;8(4):40. doi: 10.3390/diseases8040040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.RESPO P. 2020. C VID-19: tata institute OF social sciences. [Google Scholar]
- 22.Kong X., Zheng K., Tang M., Kong F., Zhou J., Diao L. Prevalence and factors associated with depression and anxiety of hospitalized patients with COVID-19. medRxiv. 2020 doi: 10.1101/2020.03.24.20043075. [DOI] [Google Scholar]
- 23.Ahmed M.Z., Ahmed O., Aibao Z., Hanbin S., Siyu L., Ahmad A. Epidemic of COVID-19 in China and associated psychological problems. Asian Journal of Psychiatry. 2020:102092. doi: 10.1016/j.ajp.2020.102092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nguyen H.C., Nguyen M.H., Do B.N., Tran C.Q., Nguyen T.T., Pham K.M. People with suspected COVID-19 symptoms were more likely depressed and had lower health-related quality of life: the potential benefit of health literacy. J. Clin. Med. 2020;9(4):965. doi: 10.3390/jcm9040965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Maraolo A.E. Una bussola per le revisioni sistematiche: la versione italiana della nuova edizione del PRISMA statement. BMJ. 2021;372 n71. [Google Scholar]
- 26.Stroup D.F., Berlin J.A., Morton S.C., Olkin I., Williamson G.D., Rennie D. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Jama. 2000;283(15):2008–2012. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- 27.Shea B.J., Reeves B.C., Wells G., Thuku M., Hamel C., Moran J. Amstar 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. Br. Med. J. 2017:358. doi: 10.1136/bmj.j4008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., Rubin G.J. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. The Lancet. 2020 Mar 14;395(10227):912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hamouche S. COVID-19 and employees' mental health: stressors, moderators and agenda for organizational actions. Emerald Open Research. 2020;2(15):15. [Google Scholar]
- 30.Ryalino C. Covid-19: what we know so far. Bali Journal of Anesthesiology. 2020;4(1):1. [Google Scholar]
- 31.Liebrenz M., Bhugra D., Buadze A., Schleifer R. Caring for persons in detention suffering with mental illness during the Covid-19 outbreak. Forensic science international Mind and law. 2020:1. doi: 10.1016/j.fsiml.2020.100013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nobles J., Martin F., Dawson S., Moran P., Savovic J. National Institute for Health Research, University of Bristol; Bristol, UK: 2020. The Potential Impact of COVID-19 on Mental Health Outcomes and the Implications for Service Solutions. [Google Scholar]
- 33.Shah K., Kamrai D., Mekala H., Mann B., Desai K., Patel R.S. Focus on mental health during the coronavirus (COVID-19) pandemic: applying learnings from the past outbreaks. Cureus. 2020;(3):12. doi: 10.7759/cureus.7405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sritharan J., Sritharan A. Emerging mental health issues from the novel coronavirus (COVID-19) pandemic. Journal of Health and Medical Sciences. 2020;(2):3. [Google Scholar]
- 35.Sultana A., Sharma R., Hossain M.M., Bhattacharya S., Purohit N. Burnout among healthcare providers during Covid-19: Challenges and evidencebased interventions. Indian J Med Ethics. July 4, 2020 doi: 10.20529/IJME.2020.73. Published online on. [DOI] [PubMed] [Google Scholar]
- 36.Thombs BD, Bonardi O, Rice DB, Boruff JT, Azar M, He C, et al. Mental health during the COVID-19 pandemic: Protocol for a Living Systematic Review of Symptom Levels, Factors Associated with Symptoms, and Intervention Effectiveness. https://osf.io/g2hwf/download.
- 37.Wang C., Pan R., Wan X., Tan Y., Xu L., McIntyre R.S., Choo F.N., Tran B., Ho R., Sharma V.K., Ho C. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav. Immun. 2020;87:40–48. doi: 10.1016/j.bbi.2020.04.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Xiao H, Zhang Y, Kong D, Li S, Yang N. The effects of social support on sleep quality of medical staff treating patients with coronavirus disease 2019 (COVID-19) in January and February 2020 in China. Medical science monitor: international medical journal of experimental and clinical research. 2020;26:e923549–1. [DOI] [PMC free article] [PubMed]
- 39.Alenazi T.H., BinDhim N.F., Alenazi M.H., Tamim H., Almagrabi R.S., Aljohani S.M. Prevalence and predictors of anxiety among healthcare workers in Saudi Arabia during the COVID-19 pandemic. Journal of infection and public health. 2020;13(11):1645–1651. doi: 10.1016/j.jiph.2020.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Burhamah W., AlKhayyat A., Oroszlányová M., AlKenane A., Almansouri A., Behbehani M. The psychological burden of the COVID-19 pandemic and associated lockdown measures: experience from 4000 participants. J. Affect. Disord. 2020;277:977–985. doi: 10.1016/j.jad.2020.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chew N.W., Lee G.K., Tan B.Y., Jing M., Goh Y., Ngiam N.J. A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain Behav. Immun. 2020;88:559–565. doi: 10.1016/j.bbi.2020.04.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chi X., Becker B., Yu Q., Willeit P., Jiao C., Huang L. Prevalence and psychosocial correlates of mental health outcomes among Chinese college students during the coronavirus disease (covid-19) pandemic. Front. Psychiatr. 2020;11:803. doi: 10.3389/fpsyt.2020.00803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cortés-Álvarez N.Y., Pineiro-Lamas R., Vuelvas-Olmos C.R. Psychological effects and associated factors of COVID-19 in a Mexican sample. Disaster Med. Public Health Prep. 2020;14(3):413–424. doi: 10.1017/dmp.2020.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ettman C.K., Abdalla S.M., Cohen G.H., Sampson L., Vivier P.M., Galea S. Prevalence of depression symptoms in US adults before and during the COVID-19 pandemic. JAMA network open. 2020;3(9) doi: 10.1001/jamanetworkopen.2020.19686. (e) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Fu W., Wang C., Zou L., Guo Y., Lu Z., Yan S. Psychological health, sleep quality, and coping styles to stress facing the COVID-19 in Wuhan, China. Transl. Psychiatry. 2020;10(1):1–9. doi: 10.1038/s41398-020-00913-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Odriozola-González P., Planchuelo-Gómez Á Irurtia-Muñiz MJ., de Luis-García R. 2020. Psychological symptoms of the outbreak of the COVID-19 crisis and confinement in the population of Spain. [DOI] [PubMed] [Google Scholar]
- 47.Huang Y., Zhao N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiatr. Res. 2020:112954. doi: 10.1016/j.psychres.2020.112954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kazmi S.S.H., Hasan K., Talib S., Saxena S. COVID-19 and lockdwon: a study on the impact on mental health. Available at SSRN. 2020;3577515 [Google Scholar]
- 49.Lai J., Ma S., Wang Y., Cai Z., Hu J., Wei N. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA network open. 2020;3(3) doi: 10.1001/jamanetworkopen.2020.3976. (e) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Li X., Lu P., Hu L., Huang T., Lu L. Factors associated with mental health results among workers with income losses exposed to COVID-19 in China. Int. J. Environ. Res. Publ. Health. 2020;17(15):5627. doi: 10.3390/ijerph17155627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Liang P., Wang Y., Shi S., Liu Y., Xiong R. Prevalence and factors associated with postpartum depression during the COVID-19 pandemic among women in Guangzhou, China: a cross-sectional study. BMC Psychiatr. 2020;20(1):1–8. doi: 10.1186/s12888-020-02969-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Liu N., Zhang F., Wei C., Jia Y., Shang Z., Sun L. Prevalence and predictors of PTSS during COVID-19 outbreak in China hardest-hit areas: Gender differences matter. Psychiatry research. 2020:112921. doi: 10.1016/j.psychres.2020.112921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Liu C.-Y., Yang Y-z, Zhang X.-M., Xu X., Dou Q.-L., Zhang W.-W. The prevalence and influencing factors for anxiety in medical workers fighting COVID-19 in China: a cross-sectional survey. Available at SSRN. 2020;3548781 doi: 10.1017/S0950268820001107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ma Y.-F., Li W., Deng H.-B., Wang L., Wang Y., Wang P.-H. Prevalence of depression and its association with quality of life in clinically stable patients with COVID-19. J. Affect. Disord. 2020;275:145–148. doi: 10.1016/j.jad.2020.06.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Moghanibashi-Mansourieh A. Assessing the anxiety level of Iranian general population during COVID-19 outbreak. Asian Journal of Psychiatry. 2020:102076. doi: 10.1016/j.ajp.2020.102076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Maroufizadeh S, Pourshaikhian M, Pourramzani A, Sheikholeslami F, Moghadamnia MT, Alavi SA. Prevalence of Anxiety and depression in general population of Iran during the COVID-19 pandemic: a web-based cross-sectional study. 10.21203/rs.3.rs-39082/v1. [DOI] [PMC free article] [PubMed]
- 57.Peng M., Mo B., Liu Y., Xu M., Song X., Liu L. Prevalence, risk factors and clinical correlates of depression in quarantined population during the COVID-19 outbreak. J. Affect. Disord. 2020;275:119–124. doi: 10.1016/j.jad.2020.06.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Pisano L., Galimi D., Cerniglia L. 2020. A qualitative report on exploratory data on the possible emotional/behavioral correlates of Covid-19 lockdown in 4-10 years children in Italy. [Google Scholar]
- 59.Que J., Le Shi J.D., Liu J., Zhang L., Wu S., Gong Y. Psychological impact of the COVID-19 pandemic on healthcare workers: a cross-sectional study in China. General psychiatry. 2020;(3):33. doi: 10.1136/gpsych-2020-100259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Rossi R., Socci V., Talevi D., Mensi S., Niolu C., Pacitti F., Di Marco A., Rossi A., Siracusano A., Di Lorenzo G. COVID-19 pandemic and lockdown measures impact on mental health among the general population in Italy. Front. Psychiatr. 2020 Aug 7;11:790. doi: 10.3389/fpsyt.2020.00790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Shevlin M., McBride O., Murphy J., Miller J.G., Hartman T.K., Levita L. 2020. Anxiety, depression, traumatic stress, and COVID-19 related anxiety in the UK general population during the COVID-19 pandemic. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Sun L., Sun Z., Wu L., Zhu Z., Zhang F., Shang Z. Prevalence and risk factors of acute posttraumatic stress symptoms during the COVID-19 outbreak in Wuhan, China. J. Affect. Disord. 2021;283:123–129. doi: 10.1016/j.jad.2021.01.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Mihret S., Biset G., Muluneh A. 2020. Psychological Impacts of COVID-19 among College Students in Dessie Town, Amhara Region, Ethiopia; Cross-sectional Study. [DOI] [Google Scholar]
- 64.Ying Y., Kong F., Zhu B., Ji Y., Lou Z., Ruan L. Mental health status among family members of health care workers in Ningbo, China during the Coronavirus Disease 2019 (COVID-19) outbreak: a Cross-sectional Study. BMC Psychiatr. 2020;20:379. doi: 10.1186/s12888-020-02784-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Zhang C., Yang L., Liu S., Ma S., Wang Y., Cai Z. Survey of insomnia and related social psychological factors among medical staff involved in the 2019 novel coronavirus disease outbreak. Front. Psychiatr. 2020;11:306. doi: 10.3389/fpsyt.2020.00306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Hossain M.M., Sultana A., Purohit N. Mental health outcomes of quarantine and isolation for infection prevention: a systematic umbrella review of the global evidence. Available at SSRN. 2020;3561265 doi: 10.4178/epih.e2020038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Pfefferbaum B., North C.S. Mental health and the Covid-19 pandemic. N. Engl. J. Med. 2020 Aug 6;383(6):510–512. doi: 10.1056/NEJMp2008017. [DOI] [PubMed] [Google Scholar]
- 68.Rogers J.P., Chesney E., Oliver D., Pollak T.A., McGuire P., Fusar-Poli P., Zandi M.S., Lewis G., David A.S. Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: a systematic review and meta-analysis with comparison to the COVID-19 pandemic. The Lancet Psychiatry. 2020 Jul 1;7(7):611–627. doi: 10.1016/S2215-0366(20)30203-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data and material can be available where appropriate.