Abstract
The accumulation of socioeconomic stressors, such as being a single parent and having a limited income, is associated with childhood maladjustment and prospective poor health. Evidence suggests both positive and negative parenting strategies (e.g., warmth and praise; criticism and neglect) may account for the relationship between socioeconomic adversity and child outcomes. However, despite the common co-occurrence of parental depression and socioeconomic stress, models of cumulative socioeconomic risk and parenting have yet to be tested in parents who are also coping with depression. In a sample of children whose parents have a history of depression, this study extends findings from a previous report (i.e., Sullivan et al. in J Fam Psychol 33:883–893, 2019) to test whether behavioral observations of parenting account for the association between a cumulative risk index of socioeconomic stress and child psychological problems in the same sample of 179 children (Mage = 11.46 years, SDage = 2.00) of parents with depression. Both positive and negative parenting accounted for the relationship between socioeconomic risk and both child- and parent-reported externalizing problems, whereas no evidence emerged for parenting accounting for the relation between cumulative risk and internalizing problems. This study highlights the central role socioeconomic stress plays in child maladjustment among parents coping with depression, as well as how parenting may be a critical mechanism linking socioeconomic stress and child externalizing problems.
Keywords: Cumulative SES risk, Parent depression, Child internalizing, Child externalizing, Parenting
Recent surges in income inequality put the major public health concern of childhood poverty at the forefront of political debate. In the US, over 15 million children—one in five—live at or below the federal poverty line, increasing their risk of negative outcomes, such as psychological disease, chronic illness, and early death [1, 2]. Further, the accumulation of risk factors, including those specific to socioeconomic status (SES) such as low income and single parenthood, is associated with increased levels of child internalizing and externalizing problems [3, 4]. In addition to the burdens associated with low SES, many families must also cope with the cross-contextual risk factor of parental depression. In a previous study (i.e., [3]), we found that cumulative SES risk, a construct in which we summed risk factors particular to social class and resource possession (e.g., single parenthood, low income), was related to childhood internalizing problems, particularly for girls, in a sample of parents with a history of depression. This finding held even after accounting for levels of parent depressive symptoms. In the current study, we investigate why cumulative SES risk was related to childhood problems in the same sample of 179 children (mean age = 11.46 years) of parents with depression. Specifically, we sought to examine whether parenting behaviors may explain the association between increases in poverty-related risk and child behavioral problems in a sample of parents with a history of depression.
Cumulative SES Risk, Parental Depression, and Parenting Practices
Research asserts a strong relationship between having inadequate access to financial (e.g., living below the poverty line) and social (e.g., failing to complete high school) resources and disruptions in parenting quality. In their Family Stress Model, Conger and Conger [5] argue that the stress of coping with these limitations translates to disrupted parenting, including using fewer positive parenting strategies (e.g., decreased warmth, sensitivity, and responsiveness) and more negative parenting strategies (e.g., neglect and increased criticism), resulting in childhood maladjustment. For example, a single parent living near poverty who was unable to finish high school may be more likely to endorse elevated stress levels and subsequently yell in response to their child misbehaving relative to a caregiver in a family without these stressors. Importantly, parenting quality is closely tied to the development and maintenance of childhood externalizing (e.g., disruptive behaviors [6]) and internalizing (e.g., anxiety [7], depression [8]) behaviors. As such, parenting difficulties among those living in poverty may link economic stress and child well-being.
Despite its strong theoretical and empirical basis, the Family Stress Model has some important limitations. Notably, it considers low SES out of the context of theoretically-relevant co-occurring challenges. Depression is closely intertwined with both socioeconomic [9] and parenting [10] challenges. Parental depression often co-occurs in high-stress environments, and it is another strong predictor of disrupted parenting and poor child outcomes [10–12]. Further, meta-analytic evidence indicates that concurrent poverty and maternal depression are related to worse child outcomes when compared to maternal depression alone [10], and parenting practices may explain the relationship between maternal depression and child well-being [13]. Accordingly, children growing up with the cross-contextual risk factors of low SES and parental depression are likely at more elevated risk of deleterious outcomes relative to children coping with stress in only one of these contexts.
Recent work highlights a poor understanding of the co-occurrence of low SES and parental depression. Specifically, research on parental depression often statistically removes the variability attributed to SES, rather than testing the relationship between SES-related stress and child outcomes [14]. Further, the Family Stress Model suggests that parents coping with economic stress are more likely to experience psychological distress, such as depressive symptoms, disrupting parenting and, in turn, child well-being [15]. Accordingly, research analyzing the role SES plays in child well-being in samples of parents with depression is necessary to effectively triage intervention efforts to support optimal child development. We thus analyzed our research questions in a sample of children (mean age = 11.46) who have a parent with a history of depression.
Complicating matters, assessing SES is challenging. A strong theoretical basis supports operationalizing SES with a cumulative risk scale (where one dichotomizes and sums the absence and presence of risk factors, such as being a single parent or having limited financial resources), positing that youth who cope with a singular socioeconomic stressor fare better relative to children coping with multiple socioeconomic stressors [16, 17]. This approach allows researchers to test questions regarding the variability in socioeconomic factors and how this variability relates to childhood outcomes. Indeed, some research suggests that increased cumulative socioeconomic risk is related to harmful parenting practices (e.g., child maltreatment [18]). Accordingly, it may be that the variability in SES-related risk is related to variability in parenting practices, such that increased levels of cumulative SES risk factors relate to decreases in positive and increases in negative parenting practices. Notably, models of the relationship between parenting and SES conceptualized from a cumulative risk framework have yet to be tested in caregivers with depression.
Does Parenting Explain the Connection Between Cumulative SES Risk and Child Internalizing and Externalizing Problems?
Evidence suggests parenting strategies (e.g., parental warmth and praise; criticism and neglect) may account for the relationship between cumulative SES risk and child problems [15, 19]. Indeed, Conger and Conger [15] posited that disruptions in parenting may be a mechanism explaining poor child well-being among families coping with economic stress, a notion long supported by seminal developmental literature [20]. In their early work, Conger and colleagues [21] demonstrated that increased stress due to economic pressure translated to parental irritability and familial tension in a sample of 12 year-old youth. This stress then permeated the parent-child dyad, increasing disruptive behavior patterns and perpetuating the development of externalizing problems [21]. Recent data also support this model. For example, in a rural sample of primarily White families, Neppl et al. [22] found that economic pressure, evaluated when children were 2 years-old, related to observations of parenting evaluated during early childhood (including harsh and positive characteristics), which, in turn, predicted child externalizing behavior, assessed between the ages of six and ten. Further research including longitudinal and experimental designs in babies, toddlers, and young children [23, 24], as well as a study examining a multigenerational sample of grandparents, parents, and children approximately 12 years old [25], support the indirect path through parenting linking socioeconomic stress and child behavior problems. Taken together, both seminal and current data support Conger and Conger’s [15] model.
Whereas theory indicates parenting is an important component in the context of both disruptive (i.e., externalizing) and anxious/depressive (i.e., internalizing) behaviors, the role of parenting in the development of disruptive behaviors is much better understood [26]. Further, empirical evidence from Conger and colleagues’ [15] study revealed that disrupted parenting better accounted for the relation between economic pressure and externalizing (R2 = 0.19) relative to internalizing (R2 = 0.08) behaviors. Finally, recent meta-analytic work indicates disrupted parenting is a stronger mediator of externalizing problems relative to internalizing problems in the context of parental depression [13]. Thus, relative to the relation between cumulative risk and internalizing problems, it may be the case that parenting strategies better explain the relation between cumulative risk and externalizing behaviors in a sample of parents with depression.
Assessment of Parenting Practices: Importance of Observations
Assessing the constructs of parenting and SES in the context of high levels of parent depression necessitates the use of observational data. Studies evaluating whether parenting functions as a mechanism of child misbehavior often rely on caregiver reports [27], which only weakly associate with observational data [28]. This weak association is particularly marked among at-risk populations, such as parents dealing with depression or income-related stress [27]. Using trained observers of parent-child interactions is the gold-standard measure of parenting quality. It carries many advantages over parent-reported data (e.g., reducing reporter bias, improving reliability, and drawing from standardized rating criteria [29, 30]). As such, given the purpose of this study is to examine the relationship between SES stressors and child well-being in the context of parental depression, it is important to use observational data to validly assess parenting behaviors.
Current Study
In our previous study, we found that cumulative SES risk was related to child internalizing and externalizing problems, particularly for girls [3]. This finding was still present even after controlling for observations of parent depression. What was left unclear, however, was why cumulative SES risk related to child problems. Extending our previous research [3] and using the same sample of children of parents with depression, this study tests whether observations of parenting practices explain the link between socioeconomic stress (measured using a cumulative risk index) and child internalizing and externalizing problems. As evidence suggests parenting plays a different role in the development and course of child internalizing versus externalizing problems [26], we hypothesized that observed parenting practices would better explain the relationship between cumulative SES risk and child externalizing problems than socioeconomic adversity and child internalizing problems. The current study uses observational data of parenting practices, parent and child reports of behavior problems, and a structural analytic framework to test our hypotheses. Importantly, we evaluate these hypotheses in a sample of children growing up with a parent who has a history of Major Depressive Disorder (MDD) during their child’s lifetime.
Method
Participants
This study is a secondary analysis of baseline data from a previous study of a prevention intervention program of 242 children from 180 different families (see Compas et al. [31]). For this study, in families with multiple children, one child was randomly selected for study analyses, resulting in a sample of 180 children (49.4 % females; Mage = 11.46; SD = 2.00) whose parents had a history of depression. Families were recruited from the Burlington, Vermont and Nashville, Tennessee areas. Mothers typically completed study procedures (88.9 %; Mage = 41.96), and a notable minority (i.e., 31.7 %) of the sample had college degrees. Most children were White; however, 25.6 % of the sample identified as a racial minority. US Census 2000 data indicate the sample was representative of the regions from which it was drawn.
Procedure
All study procedures received Institutional Review Board approval. Families were recruited using flyers, newspaper and radio advertisements, and referrals from physicians. To determine eligibility, parents were first telephone screened and then interviewed in person. Parents with past or current MDD during the lifetime of their child(ren) met inclusion criteria. Based on the Structured Clinical Interview for DSM-IV [32], parents were excluded if they had a history of Bipolar I Disorder, Schizophrenia, or Schizoaffective Disorder (see Compas et al. [33], for additional detail). Youth ages 9 to 15 years old were eligible if they were free of lifetime diagnoses of Autism Spectrum Disorders, Intellectual Disorder, Bipolar I Disorder, and Schizophrenia, and if they did not meet criteria for current MDD, Conduct Disorder or Alcohol/Substance Use Disorders (see Compas et al. [33], for training of individuals who conducted diagnostic interviews and reliability in the current project), as determined by the Schedule for Affective Disorders and Schizophrenia for School-Age Children- Present and Lifetime Version [34]. Eligible families then participated in the baseline assessment, during which the data used in this project were collected.
Measures
Demographic Information
Parents and youth provided demographic information about themselves (e.g., age and education) and their families (e.g., household income).
Cumulative Socioeconomic Status Risk
We dichotomized and summed measures of family income (i.e., below $25,000 per year = 1), household use of public assistance (i.e., no = 0; yes = 1), education (i.e., high school degree or less = 1), single-parent status (i.e., no = 0; yes = 1), and teen parent status (i.e., at the time of the child’s birth, the parent was more than 20 years old = 0; less than 20 years old = 1) to create a five-point cumulative SES risk scale. We generated a continuous proportion scale, dividing the number of endorsed risks by the number of total possible risks for which each participant had data, to accommodate the 16.11 % and 1.11 % of parents who were missing data on one or two, respectively, SES measures. Scores could range from 0 to 1.0, and a score of 0.2 approximates endorsing one risk factor. Refer to Beach et al. [35] and Brody et al. [17] for other examples of the operationalization of SES using a cumulative risk framework.
Observed Parenting
We used a global coding system, the Iowa Family Interaction Rating Scales (IFIRS) [36, 37], to code two 15-min parent-child interactions featuring a recent pleasant (e.g., going on a family vacation) and stressful (e.g., mother had a bad day at work) activity. Coders used a nine-point scale reflecting the frequency and intensity of the behavior, as well as the affective nature of the behavior. A score of one indicated the behavior or affect was absent, and a nine indicated the behavior or affect was frequent and intensely expressed during the interaction. Coders attended weekly training meetings to prevent coder drift. Independent coders double-coded videotaped interactions for individual and dyad-level behavioral and emotional characteristics and then met to establish consensus on codes greater than two points apart. Interrater reliability prior to consensus coding was 0.73 across both the discussion of the pleasant activity as well as the difficult time. For details on the comprehensive coder training program, refer to Compas et al. [38].
We created latent factors of positive and negative parenting interactions using similar indicators from previously established composites [39]. To assess positive parenting, we used six behavioral codes (α = 0.81): (1) warmth (e.g., parental support for the child); (2) child-centered behaviors (e.g., parental displays of awareness of the child’s needs); (3) positive reinforcement (i.e., parental responsiveness to their child’s appropriate behavior); (4) quality time (e.g., parental promotion of opportunities for mutual enjoyment); (5) listener responsiveness (e.g., parental behaviors validating the child); and (6) child monitoring (e.g., parental expressions indicating specific knowledge concerning the child’s life). To assess negative parenting, we used four behavioral codes (α = 0.70): (1) neglect/distancing (e.g., parental attempts to minimize interactions with child); (2) sadness (e.g., parental expressions of emotional distress/depression); (3) hostility (e.g., parental anger/criticism directed toward the child); and (4) the inverse of positive mood (e.g., displaying [low levels] of happiness and optimism). Following procedures used previously with the IFIRS codes [36, 37], we averaged scores for the six positive parenting and four negative parenting behavioral codes across the two 15-minute interactions. The validity of the IFIRS system as a whole, as well as the indicators of positive parenting, has been well-established [36, 37, 40, 41].
Parent Depressive Symptoms
We assessed levels of parent depressive symptoms using the Beck Depression Inventory-II (BDI-II [42]), which is a 21-item, self-report measure with a four-point scale ranging from zero to three. The BDI-II has demonstrated adequate internal consistency and validity in distinguishing the severity of current MDD (α = 0.94 in this sample) [42, 43].
Child Internalizing and Externalizing Problems
Parents completed the Child Behavior Checklist (CBCL), and children completed the parallel Youth Self Report (YSR) [44]. These measures included 118 items assessing a wide range of child problem behaviors that parents and children rate as not true (0), somewhat or sometimes true (1), or very true (2). The CBCL and YSR each have substantial reliability and validity data [45]. We used the subscales representing internalizing (e.g., depressive/withdrawn and anxious behaviors) and externalizing (e.g., rule-breaking and aggressive behaviors) problems. Alpha coefficients demonstrated adequate internal consistency for internalizing (CBCL: 0.85; YSR: 0.91) and externalizing (CBCL: 0.84; YSR: 0.84) problems.
Results
Data Analytic Plan
We conducted analyses using Mplus version 8.1 [46]. Positive parenting indicators were missing 6.1 % of data, and child internalizing and externalizing problem indicators were missing 2.2 % of data. Only one participant endorsed all five cumulative SES risks, and visual inspection of their data revealed marked deviations from the overall sample patterns. As such, we elected to conservatively drop this participant, resulting in a sample size of 179. To account for the small percentage of missing data as well as skew, we used Mplus’s maximum likelihood-robust (MLR) estimator with full information maximum likelihood (FIML) estimation. On average, families endorsed experiencing one cumulative SES risk stressor (Table 1), paralleling previous cumulative risk research [47]. On average, low to moderate levels of negative parenting behaviors characterized the videotaped interactions. Positive parenting indicators were more variable, with parents, on average, displaying minimal levels of child monitoring and positive reinforcement, low levels of quality time, and moderate levels warmth, listener responsiveness, and child-centered behaviors. A more detailed discussion of the cumulative risk scale is presented in Sullivan et al. [3].
Table 1.
Means and standard deviations of study variables
| Variable | M (SD) |
|---|---|
| Cumulative SES Risk (possible range: 0–1.0) |
0.23 (0.26) |
| Self-reported Parent Depression Levels (Beck Depression Inventory-II) |
18.97 (12.41) |
| Observed Positive Parenting Indicators (possible range: 1–9) |
|
| Listener responsiveness | 6.02 (1.14) |
| Child-centered behaviors | 5.93 (1.13) |
| Positive reinforcement | 2.37 (1.23) |
| Quality time | 3.32 (0.81) |
| Warmth | 4.90 (1.38) |
| Child monitoring | 1.31 (0.97) |
| Observed Negative Parenting Indicators (possible range: 1–9) |
|
| Hostility | 3.89 (1.67) |
| Sadness | 4.93 (1.24) |
| Positive mood (reverse-scored) | 5.06 (1.03) |
| Neglecting/distancing | 2.88 (1.38) |
| Parent-reported Problems (Child Behavior Checklist raw scores) |
|
| Internalizing | |
| Withdrawn | 3.34 (2.97) |
| Anxious | 5.97 (4.19) |
| Somatic | 2.54 (2.55) |
| Externalizing | |
| Rule breaking | 2.58 (2.68) |
| Aggressive | 7.20 (6.05) |
| Child-reported Problems (Youth Self Report raw scores) |
|
| Internalizing | |
| Withdrawn | 3.69 (2.93) |
| Anxious | 5.54 (4.62) |
| Somatic | 4.37 (3.49) |
| Externalizing | |
| Rule breaking | 2.87 (2.59) |
| Aggressive | 6.57 (4.82) |
Positive Parenting
Using Hu and Bentler’s [48] recommendations, we evaluated the fit of a structural equation model testing the indirect path from cumulative SES risk through positive parenting to parent and child-reported internalizing and externalizing problems, controlling for parent depressive symptoms, child age, and child gender. For parent-reported outcomes, the model demonstrated adequate fit (RMSEA = 0.065, 90 % CI [0.047, 0.083], CFI = 0.927, SRMR = 0.058). For child-reported outcomes, model demonstrated moderate fit (RMSEA = 0.055, 90 % CI [0.034, 0.074], CFI = 0.953, SRMR = 0.058). All indicators loaded significantly onto their respective factors (see Fig. 1). Child internalizing and externalizing problems were correlated. Parent depressive symptoms correlated positively with cumulative SES risk (see Fig. 1).
Fig. 1.
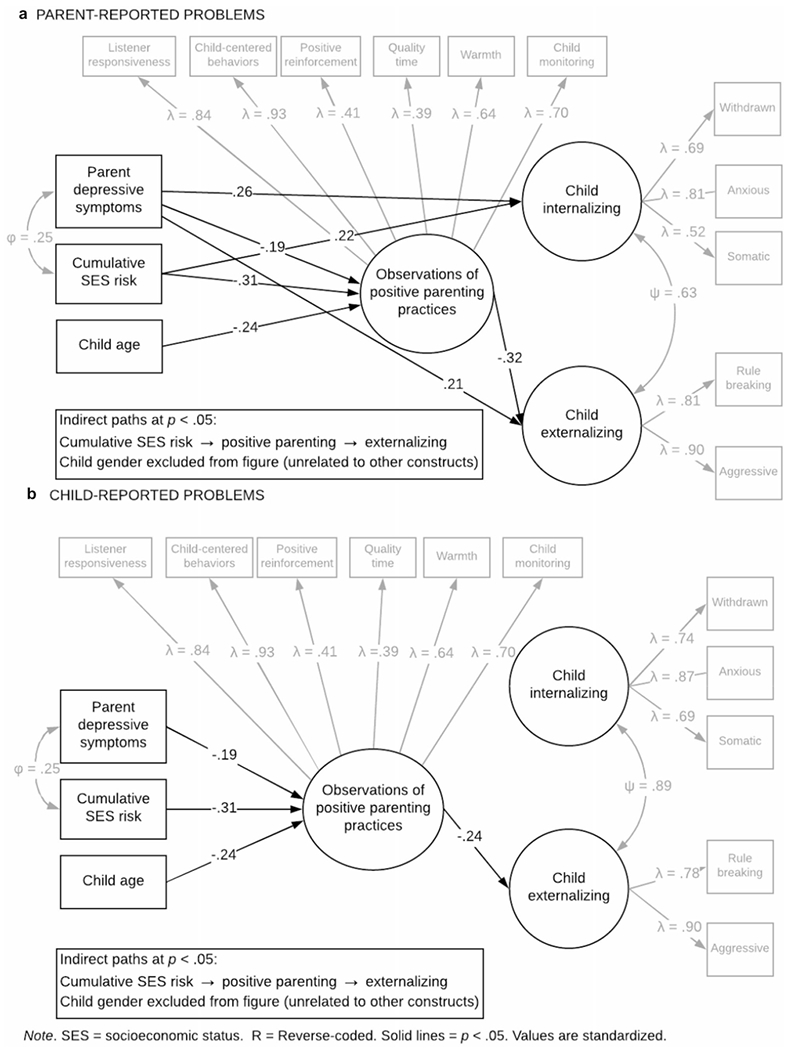
The indirect role of positive parenting on the relationship between cumulative SES risk and parent-reported (a) and child-reported (b) child internalizing and externalizing problems
As shown in Fig. 1, across reporters, the indirect path between cumulative SES risk and child externalizing through positive parenting was significant (parent report: β = 0.10, p = .01; child report: β = 0.07, p = .03). As expected, the paths from cumulative SES risk to positive parenting and from positive parenting to externalizing problems were in the negative direction. In contrast, the indirect path for both reporters between cumulative SES risk and child internalizing problems through positive parenting was nonsignificant. However, increased levels of cumulative SES risk were directly associated with increased levels of parent-reported internalizing problems (see Fig. 1a).1 Taken together, results offered support for study hypotheses, indicating that cumulative SES risk was indirectly related to externalizing, but not internalizing, problems through lower displays of positive parenting strategies.
Negative Parenting
Paralleling the procedure used for positive parenting models, we evaluated two more structural equation models, assessing whether cumulative SES risk was related to parent and child-reported problems indirectly through negative parenting. Two sets of two indicators loading onto the negative parenting latent construct were correlated to improve model fit (i.e., hostility and sadness, and sadness and neglecting/distancing, see Fig. 2). The model of parent-reported outcomes demonstrated adequate fit (RMSEA = 0.071, 90% CI [0.049, 0.092], CFI = 0.910, SRMR = 0.054), and the model of child-reported outcomes demonstrated moderate fit (RMSEA = 0.053, 90% CI [0.027, 0.077], CFI = 0.957, SRMR = 0.048). All indicators loaded significantly onto their respective factors (see Fig. 2). Child internalizing and externalizing problems, as well as parent depressive symptoms and cumulative SES risk, were modestly correlated (see Fig. 2).
Fig. 2.
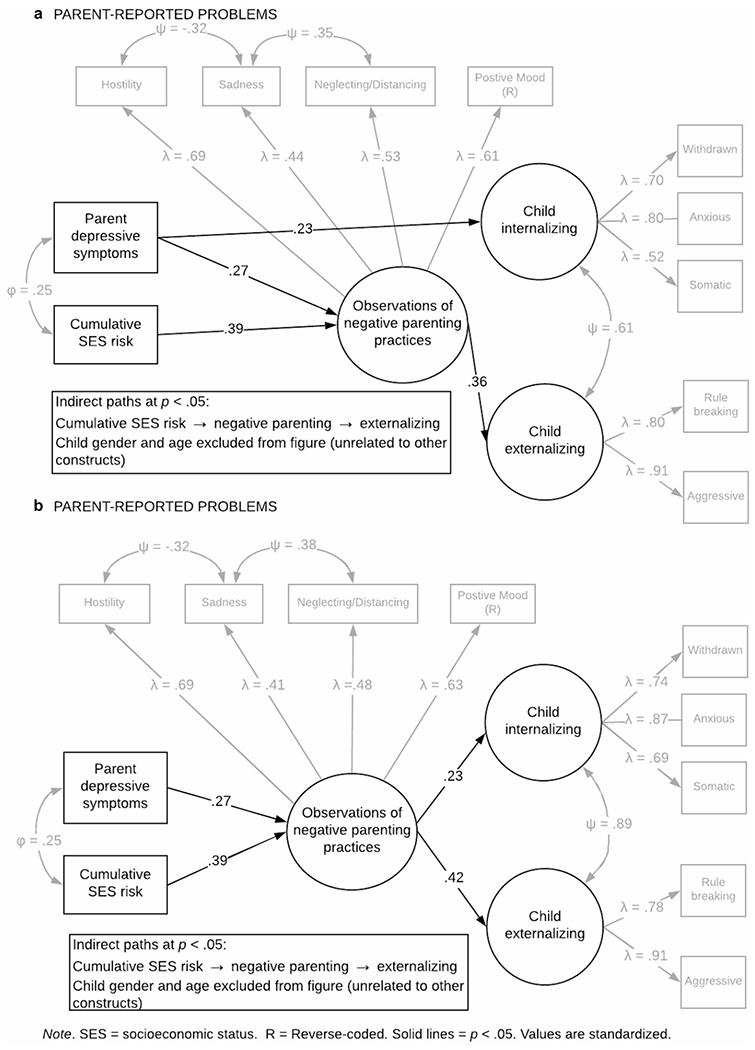
The indirect role of negative parenting on the relationship between cumulative SES risk and parent-reported (a) and child-reported (b) child internalizing and externalizing problems
As shown in Fig. 2, across reporters, the indirect path between cumulative SES risk and child externalizing through negative parenting was significant (parent report: β = 0.14, p = .01; child report: β = 0.16, p < .001). As expected, the paths from cumulative SES risk to negative parenting and from negative parenting to externalizing were in the positive direction. The indirect path between cumulative SES risk and child internalizing problems through negative parenting was nonsignificant.2 Taken together, results offered support for study hypotheses, indicating that cumulative SES risk was indirectly associated with externalizing, but not internalizing, problems through higher displays of negative parenting practices.
Sensitivity Analyses
As we used cross-sectional data to infer mediation, we conducted a series of nested model tests using Satorra-Bentler scaled chi-square statistics. Across reporters and parenting constructs, fixing the path between cumulative SES risk and externalizing problems did not result in a poorer fitting model (all χ2 diff statistics associated with ps > 0.20), whereas restricting paths between cumulative SES risk and parenting as well as parenting and externalizing problems resulted in significantly poorer fit (all χ2 diff statistics associated with ps ≤ 0.01). Taken together, these findings provide evidence favoring an indirect association between cumulative SES risk and externalizing problems through parenting practices.
Results from fixing the direct association between cumulative SES risk and internalizing problems were inconsistent. In models including positive parenting, restricting the path between parenting and internalizing did not result in poorer fitting models (all χ2 diff statistics associated with ps ≥ 0.30), whereas restricting the path between cumulative SES risk and internalizing resulted in a poorer fitting model when parents reported child internalizing (χ2 diff [3] = 6.72, p = .01) and a marginally poorer model when children reported their own internalizing χ2 diff [3] = 3.35, p = .07). These results suggest that there may be an association between cumulative SES risk and child internalizing problems; however, it is unlikely that this relation operates through positive parenting.
In the model including negative parenting and child-reported problems, whereas fixing the association between cumulative SES risk and internalizing failed to significantly change model fit (χ2 diff [3] = 1.43, p = .23), fixing the link between negative parenting and child-reported internalizing did result in a poorer fitting model (χ2 diff [3] = 4.17, p = .04). These results suggest the construct of negative parenting may be related to child-reported internalizing problems. In the model including negative parenting and parent-reported problems, fixing the path between cumulative SES risk and internalizing resulted in a poorer fitting model, approaching conventional levels of statistical significance (χ2 diff [3] = 3.34, p = .07), whereas fixing the path between negative parenting and parent-reported internalizing failed to change model fit (χ2 diff [3] = 1.41, p = .23). Drawing across models including negative parenting and child internalizing problems, it appears that, when parents reported internalizing problems, cumulative SES risk is more closely related to child internalizing. When children report their own problems, negative parenting appears to better explain variability in child internalizing.
Discussion
The purpose of this study was to investigate whether observed parenting accounted for the relationship between cumulative SES risk and child psychological problems in families where a parent has a history of depression. Based on the differential role parenting plays in child externalizing and internalizing problems [26], we hypothesized parenting would be more strongly related to externalizing problems. Supporting study hypotheses, parenting accounted for the relationship between cumulative SES risk and both child-and parent-reported externalizing problems. However, insufficient evidence was found for cumulative SES risk operating through parenting to child- or parent-reported internalizing problems. These results suggest that, as economic stressors increase, so might the importance of parenting in relation to child externalizing problems.
Although evidence suggests parenting is an important component in the development and maintenance of both childhood internalizing and externalizing behaviors [6–8], the role of parenting in the development of externalizing behaviors is much better supported and understood [26]. For example, empirical evidence from Conger and colleagues’ [15] study indicated that disrupted parenting accounted for more than twice as much variance in externalizing than internalizing behaviors. This evidence aligns with our findings, in which parenting accounted for the relationship between cumulative SES risk and child externalizing, but not internalizing, problems across reporters and parenting constructs.
In line with the Family Stress Model [15], results suggested that increasing levels of cumulative SES risk were associated with increases in positive and decreases in negative parenting, which then related to child externalizing problems. These findings are reminiscent of literature proposing parenting as a mechanism of change in behavioral parent training interventions for externalizing pathology [49]. In line with Coercion Theory [50], it may be the case that children use externalizing behaviors to elicit attention from their parents. Parents with elevated depression and stress levels may be more likely to respond ineffectively (i.e., negative reinforcement) or inconsistently [51], thereby reinforcing child misbehavior. Alternatively, in families where parent-child dyads can engage in more positive interactions (e.g., families experiencing less financial stress), children may engage in less attention-seeking behaviors and thus exhibit fewer externalizing behaviors. Further, parents in lower-income families may be preoccupied with other tasks, such as working multiple jobs and coping with the stress pertaining to finances, and thus have less time to engage in relationship-building activities with their children. In such circumstances, children may learn that “acting out” garners attention, even among busy, stressed parents coping with depressive symptoms. Our findings provide evidence favoring extending models of family stress to include parents coping with depression.
In models testing the potential indirect role of observed positive parenting practices, cumulative SES risk was directly associated with internalizing problems at conventional levels of statistical significance for parent-reported problems and approaching conventional levels of significance for child-reported problems. In models including negative parenting practices, the association between cumulative SES risk and internalizing problems was absent. These findings suggest that variables other than parenting may account for the cumulative SES risk → internalizing problems relationship, and the reporter matters. For instance, a complementary model suggests that children’s internalization of poverty-related stress explains the development of childhood behavior problems, in particular internalizing problems, in the context of socioeconomic stress [52]. As such, high-quality caregiving may be insufficient in mitigating the influence of such environmental risks, whereas a mechanism such as youth coping may better account for the relationship between cumulative SES risk and child internalizing problems. Alternatively, the signal for the relationship between cumulative SES risk and child internalizing problems may be better captured in a larger sample featuring a broader age range of children. The average age of onset for externalizing disorders is generally younger than that of internalizing disorders [53]. Given the average age of children in this sample (11.46 years), it may be the case that internalizing problems are better identified among older adolescents. Finally, it is important to consider the assessment literature: children are stronger reporters of their internal states relative to parents [54], lending more credibility to models in which children reported on their internalizing problems.
Findings must be considered in the context of several limitations. First, the cross-sectional design of this study limits claims of causality and directionality. Whereas we theorized that cumulative SES risk predicts child behavior problems, it may be the case that child behavior problems tax family resources. Additionally, as this report constitutes a secondary analysis of baseline data, study exclusions from the initial project carry over into this study, including the exclusion of caregivers and children with some psychiatric diagnoses. As such, these data likely underrepresent families with children or caregivers with pathology higher in severity. Secondly, per census data, whereas the racial makeup of this sample was representative of the geographic region from which this sample was recruited, parents of color made up a much smaller proportion of the study sample relative to White parents. Given the complex relationship between race, SES, and stress, further research testing this model in samples with more parents of color is necessary. Third, model fit for SEMs with parent-reported outcomes indicated RMSEA and CFI values slightly inconsistent with conventional guidelines (e.g., Hu & Bentler [48]). We included these models in our report as the rigor multi-informant outcomes conferred outweighed the limitation. Finally, our original analyses [3] included gender as a moderator; however, including gender as a moderator within the context of a mediation model requires a larger sample size, and future research should consider the influence gender might have on models of socioeconomic stress, parenting, and child well-being.
Despite these limitations, this study was methodologically rigorous in several ways. One, it was multi-informant, and models were largely consistent across parent- and child-report. Two, the use of observational data increases the validity of the findings, particularly in families where cumulative SES risk or depressive symptoms were high, given research suggesting that parents coping with these characteristics are less reliable with other forms of reporting [27].
Findings from this study shed light on several future research avenues. Importantly, scientists must examine this model in a broader age range of children including both younger children, who may be even more vulnerable to the deleterious effects of maladjustment [55], and older children, who may be more vulnerable to the development of internalizing symptoms [53]. Further, whereas this study stresses the import of parenting, the role of other broader systems and policies must be considered. Decreasing the wealth gap and improving access to resources among underserved communities may also buffer the stress and, consequently, parenting difficulties families face. In conclusion, findings from this study highlight the central role socioeconomic stress plays in child maladjustment when a parent has a history of depression, and they point to parenting as a potential resource that clinicians can leverage to reduce externalizing problems and improve the trajectories of youth growing up in these contexts.
Summary
The accumulation of socioeconomic stressors is associated with childhood psychological and physical problems. Further, evidence suggests both positive and negative parenting strategies (e.g., warmth and praise; criticism and neglect) may account for the relationship between socioeconomic adversity and child outcomes, with models of family functioning indicating that increases in socioeconomic stress relate to problematic parenting practices. Parents coping with socioeconomic stress are also often coping with comorbid depression. However, despite this frequent co-occurrence, studies of parental depression and child well-being frequently statistically eliminate the variability associated with SES. In a sample of children whose parents have a history of depression, this study extends findings from a previous report (i.e., [3]) to test whether behavioral observations of positive and negative parenting account for the association between a cumulative risk index of socioeconomic stress and child psychological externalizing and internalizing problems in the same sample of 179 children of parents with depression. We found that both positive and negative parenting accounted for the relationship between socioeconomic risk and both child- and parent-reported externalizing problems, whereas no evidence emerged for parenting accounting for the relation between cumulative risk and internalizing problems. This study highlights the central role socioeconomic stress plays in child maladjustment and provides support for generalizing models of family stress to families in which a parent has a history of depression. Further, results emphasize the importance of parenting as a mechanism linking socioeconomic stress and child externalizing problems, even among parents coping with depression.
Funding
This research was supported by the National Institute of Child Health and Human Development [grant F31HD098825 to (A) S.) and the National Institute of Mental Health [Grants R01MH069940 to (B) C. and R01MHO69928 to R. F.]. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Conflict of interest All authors have no conflicts of interest.
Ethical Approval All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent Informed consent was obtained from all individual participants included in this study.
Research Involving Human and/or Animal Participants This articled does not contain any studies with animals performed by any of the authors.
1 A direct path from cumulative SES risk to child reported internalizing approaching conventional levels of statistical significance also emerged in a model of positive parenting (p = .06).
2 Whereas the paths from cumulative SES risk to negative parenting and negative parenting to child-reported internalizing problems were statistically significant, the indirect path from cumulative SES risk to child-reported internalizing problems through negative parenting approached (p = .06) but did not reach conventional levels of statistical significance.
References
- 1.US Department of Health & Human Services Children’s Bureau (2019) Child Poverty. http://www.nccp.org/topics/childpoverty.html. Accessed 25 Mar 2020
- 2.Oh DL, Jerman P, Silvério Marques S et al. (2018) Systematic review of pediatric health outcomes associated with childhood adversity. BMC Pediatr 18:1–19. 10.1186/s12887-018-1037-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sullivan ADW, Benoit R, Breslend NL et al. (2019) Cumulative socioeconomic status risk and observations of parent depression: are there associations with child outcomes? J Fam Psychol 33:883–893. 10.1037/fam0000567 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Evans GW, Li D, Whipple SS (2013) Cumulative risk and child development. Psychol Bull 139:1342–1396. 10.1037/a0031808 [DOI] [PubMed] [Google Scholar]
- 5.Conger R, Wallace LE, Sun Y et al. (2002) Economic pressure in African American families: a replication and extension of the family stress model. Dev Psychol 38:179–193. 10.1037//0012-1649.38.2.179 [DOI] [PubMed] [Google Scholar]
- 6.Patterson GR (1982) Coercive family process. Castalia, Oregon [Google Scholar]
- 7.Drake KL, Ginsburg GS (2012) Family factors in the development, treatment, and prevention of childhood anxiety disorders. Clin Child Fam Psychol Rev 15:144–162. 10.1007/s10567-011-0109-0 [DOI] [PubMed] [Google Scholar]
- 8.McLeod BD, Weisz JR, Wood JJ (2007) Examining the association between parenting and childhood depression: a meta-analysis. Clin Psychol Rev 27:986–1003. 10.1016/j.cpr.2007.03.001 [DOI] [PubMed] [Google Scholar]
- 9.Lorant V, Deliège D, Eaton W et al. (2003) Socioeconomic inequalities in depression: a meta-analysis. Am J Epidemiol 157:98–112. 10.1093/aje/kwf182 [DOI] [PubMed] [Google Scholar]
- 10.Goodman SH, Rouse MH, Connell AM et al. (2011) Maternal depression and child psychopathology: a meta-analytic review. Clin Child Fam Psychol Rev 14:1–27. 10.1007/s10567-010-0080-1 [DOI] [PubMed] [Google Scholar]
- 11.Ertel KA, Rich-Edwards JW, Koenen KC (2011) Maternal depression in the United States: nationally representative rates and risks. J Women’s Heal 20:1609–1617. 10.1089/jwh.2010.2657 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vreeland A, Gruhn MA, Watson KH et al. (2019) Parenting in context: associations of parental depression and socioeconomic factors with parenting behaviors. J Child Fam Stud. 10.1007/s10826-019-01338-3 [DOI] [Google Scholar]
- 13.Goodman SH, Simon HFM, Shamblaw AL, Kim CY (2020) Parenting as a mediator of associations between depression in mothers and children’s functioning: a systematic review and meta-analysis. Clin Child Fam Psychol Rev 23:427–460. 10.1007/s10567-020-00322-4 [DOI] [PubMed] [Google Scholar]
- 14.Gotlib IH, Goodman SH, Humphreys KL (2020) Studying the intergenerational transmission of risk for depression: current status and future directions. Curr Dir Psychol Sci 29:174–179. 10.1177/0963721420901590 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Conger R, Conger KJ (2002) Resilience in Midwestern families: selected findings from the first decade of a prospective, longitudinal study. J Marriage Fam 64:361–373. 10.1111/j.1741-3737.2002.00361.x [DOI] [Google Scholar]
- 16.Evans GW (2003) A multimethodological analysis of cumulative risk and allostatic load among rural children. Dev Psychol 39:924–933. 10.1037/0012-1649.39.5.924 [DOI] [PubMed] [Google Scholar]
- 17.Brody GH, Yu T, Chen E et al. (2013) Is resilience only skin deep? Rural African Americans’ socioeconomic status-related risk and competence in preadolescence and psychological adjustment and allostatic load at age 19. Psychol Sci 24:1285–1293. 10.1177/0956797612471954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Berger LM, Brooks-Gunn J (2005) Socioeconomic status, parenting knowledge and behaviors, and perceived maltreatment of young low-birth-weight children. Soc Serv Rev 79:237–267. 10.1086/428957 [DOI] [Google Scholar]
- 19.Gach EJ, Ip KI, Sameroff AJ, Olson SL (2018) Early cumulative risk predicts externalizing behavior at age 10: the mediating role of adverse parenting. J Fam Psychol 32:92–102. 10.1037/fam0000360 [DOI] [PubMed] [Google Scholar]
- 20.McLoyd VC (1998) Socioeconomic disadvantage and child development. Am Psychol 53:185–204. 10.1037/0003-066X.53.2.185 [DOI] [PubMed] [Google Scholar]
- 21.Conger KJ, Conger R (1994) Differential parenting and change in sibling differences in delinquency. J Fam Psychol 8:287–302. 10.1037/0893-3200.8.3.287 [DOI] [Google Scholar]
- 22.Neppl TK, Senia JM, Donnellan MB (2016) Effects of economic hardship: testing the family stress model over time. J Fam Psychol 30:12–21. 10.1037/fam0000168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jeon S, Neppl TK (2019) Economic pressure, parent positivity, positive parenting, and child social competence. J Child Fam Stud 28:1402–1412. 10.1007/s10826-019-01372-1 [DOI] [Google Scholar]
- 24.Weisleder A, Cates CB, Dreyer BP et al. (2016) Promotion of positive parenting and prevention of socioemotional disparities. Pediatrics. 10.1542/peds.2015-3239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lee DB, Assari S, Miller AL et al. (2019) Positive parenting moderates the effect of socioeconomic status on executive functioning: a three-generation approach. J Child Fam Stud 28:1878–1885. 10.1007/s10826-019-01411-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Forehand RL, Jones DJ, Parent J (2013) Behavioral parenting interventions for child disruptive behaviors and anxiety: what’s different and what’s the same. Clin Psychol Rev 33:133–145. 10.1016/j.cpr.2012.10.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Herbers JE, Garcia EB, Obradović J (2017) Parenting assessed by observation versus parent-report: moderation by parent distress and family socioeconomic status. J Child Fam Stud 26:3339–3350. 10.1007/s10826-017-0848-8 [DOI] [Google Scholar]
- 28.Hendriks AM, Van der Giessen D, Stams GJJM, Overbeek G (2018) The association between parent-reported and observed parenting: a multi-level meta-analysis. Psychol Assess 30:621–633. 10.1037/pas0000500 [DOI] [PubMed] [Google Scholar]
- 29.Metzler CW, Sanders MR, Rusby JC (2014) Multiple levels and modalities of measurement in a population-based approach to improving parenting. Emerging Methods in Family Research. Springer, Cham, pp 197–214 [Google Scholar]
- 30.Seifer R (2005) Who should collect our data: parents or trained observers? In: Teti D (ed) Handbook of Research Methods in Developmental Science. Blackwell, Malden, pp 123–137 [Google Scholar]
- 31.Compas BE, Forehand RL, Thigpen J et al. (2015) Efficacy and moderators of a family group cognitive-behavioral preventive intervention for children of parents with depression. J Consult Clin Psychol 83:541–553. 10.1037/a0039053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.First M, Spitzer R, Gibbon M, Williams J (1997) User’s guide for the structured clinical interview for DSM-IV axis I disorders (SCID-I): clinician version. Am Psychiatr Publ, Washington, D.C. [Google Scholar]
- 33.Compas BE, Forehand RL, Keller G et al. (2009) Randomized controlled trial of a family cognitive-behavioral preventive intervention for children of depressed parents. J Consult Clin Psychol 77:1007–1020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kaufman J, Birmaher B, Brent D et al. (1997) Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): initial reliability and validity data. J Am Acad Child Adolesc Psychiatry 36:980–988. 10.1097/00004583-199707000-00021 [DOI] [PubMed] [Google Scholar]
- 35.Beach SRH, Lei MK, Brody GH et al. (2014) Nonsupportive parenting affects telomere length in young adulthood among African Americans: mediation through substance use. J Fam Psychol 28:967–972. 10.1037/fam0000039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Melby JN, Conger RD, Book R, Reuter M, Lucy L, Repinski D (1998) The Iowa family interaction rating scales, 5th edn. Unpublished manuscript, Ames Institute for Social and Behavioral Research, Iowa State University [Google Scholar]
- 37.Melby JN, Conger RD (2001) The Iowa family interaction rating scales: instrument summary. In Kerig PK, Lindahl KM (eds) Family observational coding systems. Lawrence Erlbaum, Mahway, NJ, pp. 33–58 [Google Scholar]
- 38.Compas BE, Champion JE, Forehand RL et al. (2010) Coping and parenting: mediators of 12-month outcomes of a family group cognitive-behavioral preventive intervention with families of depressed parents. J Consult Clin Psychol 78:623–634. 10.1037/a0020459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lim JH, Wood BL, Miller BD, Simmens SJ (2011) Effects of paternal and maternal depressive symptoms on child internalizing symptoms and asthma disease activity: mediation by interparental negativity and parenting. J Fam Psychol 25:137–146. 10.1037/a0022452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Alderfer MA, Fiese BH, Gold JI et al. (2008) Evidence-based assessment in pediatric psychology: family measures. J Pediatr Psychol 33:1046–1061. 10.1093/jpepsy/jsm083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lim JH, Wood BL, Miller BD (2008) Maternal depression and parenting in relation to child internalizing symptoms and asthma disease activity. J Fam Psychol 22:264–273. 10.1037/0893-3200.22.2.264 [DOI] [PubMed] [Google Scholar]
- 42.Beck AT, Steer RA, Ball R, Ranieri WF (1996) Comparison of Beck depression inventories -IA and -II in psychiatric outpatients. J Pers Assess 67:588–597. 10.1207/s15327752jpa6703_13 [DOI] [PubMed] [Google Scholar]
- 43.Steer RA, Ball R, Ranieri WF, Beck AT (1999) Dimensions of the Beck depression inventory-II in clinically depressed outpatients. J Clin Psychol 55:117–128. [DOI] [PubMed] [Google Scholar]
- 44.Achenbach T, Rescorla L (2001) Manual for the ASEBA school-age forms & profiles: an integrated system of multi-informant assessment. ASEBA, Burlington [Google Scholar]
- 45.Achenbach T (1991) The child behavior checklist manual. University of Vermont, Burlington [Google Scholar]
- 46.Muthén LK, Muthén BO (1998-2017) Mplus user’s guide, 8th edn. Muthén & Muthén, Los Angeles, CA [Google Scholar]
- 47.Evans GW, Kim P (2007) Childhood poverty and health: cumulative risk exposure and stress dysregulation. Psychol Sci 18:953–957. 10.1111/j.1467-9280.2007.02008.x [DOI] [PubMed] [Google Scholar]
- 48.Hu LT, Bentler PM (1999) Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Model 6:1–55. 10.1080/10705519909540118 [DOI] [Google Scholar]
- 49.Forehand RL, Lafko N, Parent J, Burt KB (2014) Is parenting the mediator of change in behavioral parent training for externalizing problems of youth? Clin Psychol Rev 34:608–619. 10.1016/j.cpr.2014.10.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Patterson GR (2004) The early development of coercive family process. In: Reid J, Patterson G, Synder J (eds) Antisocial behavior in children and adolescents: a developmental analysis and model for intervention. American Psychological Association, Washington, D.C., pp 25–44 [Google Scholar]
- 51.Lunkenheimer E, Lichtwarck-Aschoff A, Hollenstein T et al. (2016) Breaking down the coercive cycle: how parent and child risk factors influence real-time variability in parental responses to child misbehavior. Parenting 16:237–256. 10.1080/15295192.2016.1184925 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Santiago CDC, Wadsworth ME, Stump J (2011) Socioeconomic status, neighborhood disadvantage, and poverty-related stress: prospective effects on psychological syndromes among diverse low-income families. J Econ Psychol 32:218–230. 10.1016/j.joep.2009.10.008 [DOI] [Google Scholar]
- 53.Kessler RC, Amminger GP, Aguilar-Gaxiola S et al. (2007) Age of onset of mental disorders: a review of recent literature. Curr Opin Psychiatry 20:359–364. 10.1097/YCO.0b013e32816ebc8c [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.De Los Reyes A, Augenstein TM, Wang M et al. (2015) The validity of the multi-informant approach to assessing child and adolescent mental health. Psychol Bull 141:858–900. 10.1037/a0038498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Dunn EC, Soare TW, Zhu Y et al. (2019) Sensitive periods for the effect of childhood adversity on DNA methylation: results from a prospective, longitudinal study. Biol Psychiatry 85:838–849. 10.1016/j.biopsych.2018.12.023 [DOI] [PMC free article] [PubMed] [Google Scholar]


