Abstract
Objectives
To test the relationship between increasing severity of obesity, calculated risk and observed outcomes.
Methods
Patients with symptoms suggestive of coronary artery disease (CAaD) (n=10 003) were stratified according to body mass index (BMI). We compared risk factors, pooled risk scores and physicians’ perception of risk. Cox regression tested the association between BMI and (1) presence of obstructive CAD and (2) composite clinical endpoints (death, cardiovascular death, unstable angina hospitalisation and myocardial infarction).
Results
BMI was ≥30 kg/m2 in 48% of patients and ≥35 in 20%. Increasingly obese patients were younger, female and non-smoking but with higher prevalence of hypertension, diabetes, black race and sedentary lifestyle. Pooled risk estimates of CAD were highest in those with mid-range BMI. In contrast, physicians’ estimation of the likelihood of significant CAD based on clinical impression increased progressively with BMI. For a 10% increase in the Diamond-Forrester probability of CAD, the adjusted OR for obstructive CAD was 1.5 (95% CI 1.4 to 1.5) in patients with BMI <35, but only 1.2 (95% CI 1.1 to 1.3) in those with BMI ≥35 (interaction p<0.001). Framingham Risk Score increased across increasing BMI categories. However, there was a strong and consistent inverse relationship between degree of obesity and all three composite clinical endpoints over a median 25 months of follow-up.
Conclusions
Despite perceptions of higher risk and higher risk scores, increasingly obese patients had obstructive CAD less frequently than predicted and had fewer adverse clinical outcomes. There is a need for risk assessment tools and guidelines that account for obesity.
Trial registration number
INTRODUCTION
Commonly used clinical risk prediction tools substantially overestimate the true prevalence of obstructive coronary artery disease (CAD) and the risk of adverse cardiovascular (CV) events in contemporary patients.1,2 One potential explanation for such discrepancies is that patient characteristics and medical treatments are different than those in the populations that were used to develop the pooled risk prediction tools. One of the most dramatic changes in patient characteristics is the steep increase in the prevalence of obesity in the past three decades.3 During this time period, the overall age-adjusted prevalence of obesity in the USA has doubled, and in 2016, it was reported to be 37.7%, with 5.5% of men and 9.9% of women having WHO class 3 obesity (body mass index (BMI) ≥40 kg/m2).3
Obesity is a risk factor for the development of CAD and may also increase the rate of disease progression.4–9 However, the assessment of suspected CAD in patients with obesity is complicated by the fact that those symptoms that are suspicious for cardiac ischaemia may also be attributable to obesity-associated non-cardiac conditions such as deconditioning, obstructive sleep apnoea and musculoskeletal problems. Additionally, the severity of the symptoms may increase in proportion to the degree of obesity. Thus, treating clinicians may have a higher degree of concern for cardiac ischaemia as the severity of obesity increases. None of the commonly used scoring systems for predicting the likelihood of obstructive CAD or risk of CV events account for the presence or the extent of obesity in the patients being assessed.10 Notably, the original Framingham cohort and the offspring cohort had a prevalence of obesity of ~16% and overweight was ~33%. This is less than half the prevalence currently seen in US adults. Furthermore, current guidelines for evaluation of stable ischaemic heart disease do not address the additional complexities surrounding the evaluation of obese patients.11–13
Clinical decision making could be enhanced if there were data available from prospective controlled studies that shed light on topics related to obesity, presence of CAD and risk of events. The Prospective Multicenter Imaging Study for Evaluation of Chest Pain (PROMISE) trial evaluated a large population of patients with suspected CAD, approximately half of whom were obese. We used this modern, well-characterised population to determine the association of obesity with risk factor burden, symptoms, risk scores and the actual observed prevalence of obstructive CAD and subsequent adverse cardiac events.
METHODS
Study cohort and design
The PROMISE trial was a pragmatic comparative effectiveness trial that randomised stable, symptomatic patients without known CAD to either an initial strategy of anatomic testing with ECG-gated coronary computed tomographic angiography (CTA) or stress testing.14,15 All study procedures were approved by appropriate local or central institutional review boards, and all participants provided written informed consent. For patients in the stress-testing arm, the choice of test was left up to the treating clinician (exercise ECG, stress echocardiography or nuclear myocardial perfusion imaging). Randomisation was stratified by study site and by the stress test type prespecified by the provider. All tests were performed and interpreted by local physicians who were responsible for all subsequent clinical decisions including the use of invasive coronary angiography (Cath). Obstructive CAD was defined as ≥50% stenosis in the left main coronary artery or ≥70% in any major vessel as determined by CTA or Cath. The study results have been reported previously15 and showed equivalence of clinical outcomes in the two randomised arms after a median of 25 months of follow-up. The updated Diamond-Forrester clinical prediction rule was used to determine the pretest probability of obstructive CAD.2 This updated classification system still uses only three components: age, gender and characterisation of chest pain. However, the predictive value of each component was re-evaluated, and the overall model was recalibrated in 2011. The Framingham Risk Score, which gives an estimate of 10-year risk of cardiac events, was calculated for all patients at study entry.16 This widely used risk score incorporates traditional coronary risk factors but does not take into account the presence or severity of obesity. We evaluated three composite clinical endpoints: (1) death/myocardial infarction (MI)/unstable angina hospitalisation (UAH), (2) CV death/MI/UAH or (3) CV death/MI. The study conformed to the Declaration of Helsinki.
Statistical analyses
Patients were categorised according to WHO guidelines based on BMI. Baseline patient characteristics and calculated risk scores are reported as mean (SD) for continuous variables and percentages for categorical variables. Characteristics and risk scores were compared across BMI categories using Kruskal-Wallis test for continuous variables and χ2 test for categorical variables. Logistic regression models were used to investigate the association between Diamond-Forrester probability of obstructive CAD and CAD assessed by Cath or CTA. If a patient received CTA as his or her initial non-invasive test and subsequently received Cath, then only the Cath results were used to assess CAD. ORs and 95% CIs were reported with respect to a 10% increase in Diamond-Forrester risk prediction. In separate logistic regression models, we used a two-way interaction to assess whether BMI categories (≥35 vs <35) modified the relationship between Diamond-Forrester and CAD. Prediction of CAD by Diamond-Forrester score was assessed by c-statistics by BMI category (≥35 vs <35). Models for CAD were adjusted for chest pain as the primary symptom, smoking (ever/never), diabetes, hypertension, history of peripheral artery or cerebrovascular disease, sedentary lifestyle, depression, family history of premature CAD and dyslipidaemia. After testing for the proportional hazard assumption, Cox regression models assessed the association between BMI, continuous and categorical (≥35 vs <35), and the three composite clinical endpoints. Fine-Gray models were calculated to account for the competing risk of non-CVD death for the relevant composite endpoints. In separate models, we used a two-way interaction to assess whether the initial non-invasive test modality modified the relationship between BMI and outcomes. Models for outcomes adjusted for the same variables as above plus age and sex. All statistical calculations were carried out using SAS V.9.4.
RESULTS
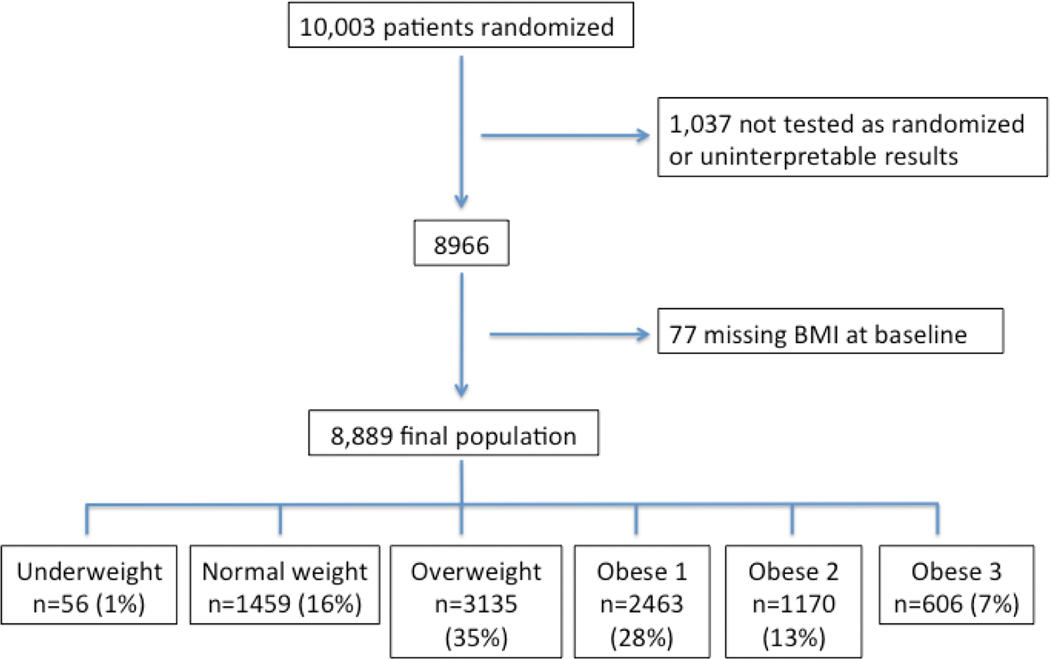
In the PROMISE trial, a total of 10 003 patients were enrolled between 2010 and 2013. figure 1 shows the flow of patients through the study. There were 8889 patients who were tested as randomised, had interpretable test results and had BMI data available. All analyses in this paper refer to this subgroup of subjects. Among these, 7378 (83%) were categorised as overweight or obese, and 28%, 13% and 7% had class 1, 2 or 3 obesity, respectively (table 1). With increasing levels of adiposity as defined by BMI, there were fewer white patients and more black patients (table 1). More obese patients tended to be younger; the mean age difference between the normal weight group and those with class 3 obesity was 4.2 years. There were differences in the distribution of men and women across BMI categories, with higher percentages of female patients in the underweight, normal weight and most obese categories but fewer in the overweight and mildly obese groups. The presence of several major CV risk factors (hypertension, diabetes and sedentary lifestyle) increased linearly with higher levels of obesity, and the presence of metabolic syndrome was even more strongly related to BMI. In contrast, smoking was inversely related to BMI.
Figure 1.
CONSORT diagram. BMI, body mass index; CONSORT, Consolidated Standards of Reporting Trials.
Table 1.
Patient demographics/characteristics, symptoms and cardiac medications based on WHO body mass index categories
| Underweight BMI <18.5 n=56 (1%) | Normal 18.5–24.9 n=1459 (16%) | Overweight 25.0–29.9 n=3135 (35%) | Obese 1 30.0–34.9 n=2463 (28%) | Obese 2 35.0–39.9 n=1170 (13%) | Obese 3 ≥40 n=606 (7%) | P value | |
|---|---|---|---|---|---|---|---|
| Age, years* | 61.2 (8.57) | 62.7 (8.94) | 61.3 (8.48) | 60.3 (7.86) | 59.1 (7.42) | 58.5 (6.84) | <0.001 |
| Female sex | 42/56 (75.0) | 899/1459 (61.6) | 1499/3135 (47.8) | 1216/2463 (49.4) | 655/1170 (56.0) | 367/606 (60.6) | <0.001 |
| Race | <0.001 | ||||||
| White | 49/55 (89.1) | 1250/1445 (86.5) | 2655/3111 (85.3) | 2066/2446 (84.5) | 973/1154 (84.3) | 476/603 (78.9) | |
| Black | 4/55 (7.3) | 107/1445 (7.4) | 272/3111 (8.7) | 299/2446 (12.2) | 154/1154 (13.3) | 112/603 (18.6) | |
| Asian | 1/55 (1.8) | 65/1445 (4.5) | 118/3111 (3.8) | 29/2446 (1.2) | 5/1154 (0.4) | 2/603 (0.3) | |
| Ethnicity | 0.063 | ||||||
| Hispanic or Latino | 3/55 (5.5) | 82/1446 (5.7) | 253/3118 (8.1) | 196/2448 (8.0) | 85/1163 (7.3) | 41/605 (6.8) | |
| Not Hispanic or Latino | 52/55 (94.5) | 1364/1446 (94.3) | 2865/3118 (91.9) | 2252/2448 (92.0) | 1078/1163 (92.7) | 564/605 (93.2) | |
| Cardiac risk factors | |||||||
| Hypertension | 31/56 (55.4) | 698/1459 (47.8) | 1855/3135 (59.2) | 1754/2463 (71.2) | 915/1170 (78.2) | 506/606 (83.5) | <0.001 |
| Diabetes | 6/56 (10.7) | 153/1459 (10.5) | 417/3135 (13.3) | 645/2463 (26.2) | 382/1170 (32.6) | 281/606 (46.4) | <0.001 |
| Dyslipidaemia | 27/56 (48.2) | 894/1459 (61.3) | 2160/3135 (68.9) | 1744/2463 (70.8) | 801/1170 (68.5) | 391/606 (64.5) | <0.001 |
| Smoker (ever/never) | 35/56 (62.5) | 798/1459 (54.7) | 1581/3134 (50.4) | 1282/2463 (52.1) | 565/1170 (48.3) | 282/606 (46.5) | <0.001 |
| Family history of premature CAD | 19/55 (34.5) | 458/1451 (31.6) | 981/3129 (31.4) | 765/2455 (31.2) | 396/1167 (33.9) | 197/605 (32.6) | 0.610 |
| Sedentary lifestyle | 23/56 (41.1) | 570/1456 (39.1) | 1348/3130 (43.1) | 1247/2459 (50.7) | 699/1170 (59.7) | 414/606 (68.3) | <0.001 |
| Metabolic syndrome | 4/56 (7.1) | 118/1459 (8.1) | 430/3135 (13.7) | 1564/2463 (63.5) | 806/1170 (68.9) | 443/606 (73.1) | <0.001 |
| Primary presenting symptom | |||||||
| Chest pain | 47/56 (83.9) | 1087/1458 (74.6) | 2292/3134 (73.1) | 1801/2461 (73.2) | 815/1168 (69.8) | 421/606 (69.5) | 0.011 |
| Dyspnoea | 6/56 (10.7) | 188/1458 (12.9) | 441/3134 (14.1) | 383/2461 (15.6) | 203/1168 (17.4) | 117/606 (19.3) | <0.001 |
| Medication use | |||||||
| Aspirin | 15/55 (27.3) | 582/1366 (42.6) | 1302/2981 (43.7) | 1108/2381 (46.5) | 526/1135 (46.3) | 277/589 (47.0) | 0.006 |
| Statin | 15/55 (27.3) | 546/1366 (40.0) | 1382/2981 (46.4) | 1160/2381 (48.7) | 524/1135 (46.2) | 275/589 (46.7) | <0.001 |
| Beta-blocker | 17/55 (30.9) | 284/1366 (20.8) | 658/2981 (22.1) | 645/2381 (27.1) | 319/1135 (28.1%) | 188/589 (31.9) | <0.001 |
| ACEi or ARB | 16/55 (29.1) | 397/1366 (29.1) | 1110/2981 (37.2) | 1183/2381 (49.7) | 642/1135 (56.6) | 377/589 (64.0) | <0.001 |
Data are n/N (%) except where indicated.
Mean (SD).
ACEi, angiotensin-converting enzyme inhibitor; ARB, angiotensin receptor blocker; BMI, body mass index; CAD, coronary artery disease.
Increasingly obese patients were less likely to have chest pain and more likely to have dyspnoea as their presenting symptom (table 1). However, among those with chest pain, its typicality as assessed by the treating physician was not different across obesity categories. Significant differences were found in use of cardiac medications based on BMI category, with those in the higher categories more likely to take angiotensin-converting enzyme inhibitors/angiotensin receptor blockers and beta-blockers (table 1).
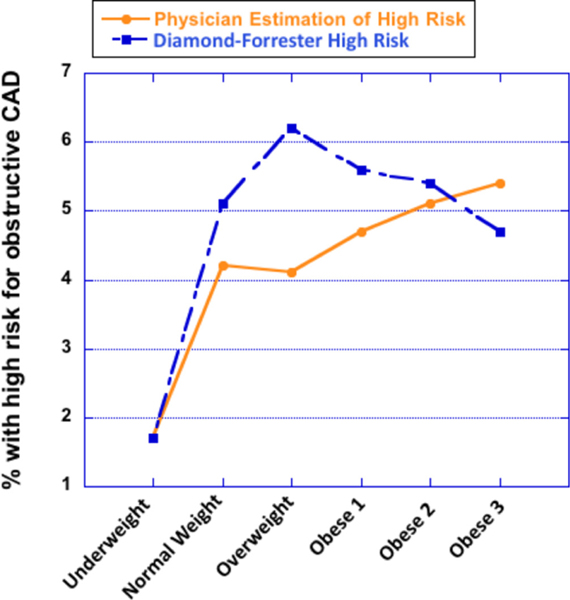
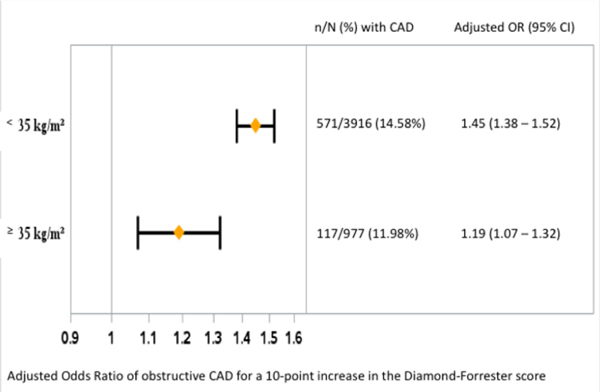
A high pretest likelihood of obstructive CAD (>70%) based on the updated Diamond-Forrester predictive model2 showed an inverted U-shaped relationship with BMI. The highest and lowest BMI categories had fewer high-risk patients than mid-range BMI (table 2, figure 2). Those with class 2 or 3 obesity had updated Diamond-Forrester pretest probabilities that were comparable with the normal weight group. In contrast, the treating physicians’ estimation of a high likelihood of significant CAD (71%–90% probability) increased progressively with BMI (figure 2). The actual prevalence of obstructive CAD was determined in all patients undergoing CTA and in those who had Cath following the non-invasive testing (table 2). The observed prevalence of obstructive CAD by CTA or Cath was 14.6% in those with BMI <35% and 12.0% in those with BMI ≥35 (p=0.04). The two-way interaction between the updated Diamond-Forrester probability and BMI category (<35 vs ≥35) suggested that BMI modified the association between Diamond-Forrester predictions and the actual presence of obstructive CAD (p<0.001; figure 3). For a 10-point increase in the updated Diamond-Forrester probability of obstructive CAD, the odds of obstructive CAD by CTA or Cath increased more in those with BMI<35 (adjusted OR 1.45, 95% CI 1.38 to 1.52) compared with those with BMI≥35 (adjusted OR 1.19, 95% CI 1.07 to 1.32) (figure 3). The c-statistic for predicting CAD with the Diamond-Forrester risk score was 0.71 (95% CI 0.69 to 0.73) for the BMI ≤35 group and 0.66 (95% CI 0.61 to 0.71) for the BMI >35 group.
Table 2.
Risk scores and assessment of coronary artery disease (CAD) likelihood by WHO body mass index categories and presence of obstructive CAD by invasive angiography or CT angiography
| Underweight (n=56) | Normal (n=1459) | Overweight (n=3135) | Obese 1 (n=2463) | Obese 2 (n=1170) | Obese 3 (n=606) | P value | |
|---|---|---|---|---|---|---|---|
| 10-year CVD risk | |||||||
| Framingham Risk Score (2008) | <0.001 | ||||||
| Mean (SD) | 15.5 (11.80) | 18.0 (13.40) | 20.9 (14.29) | 23.6 (15.82) | 22.6 (15.80) | 22.7 (14.96) | |
| Low risk (<10%) | 15/56 (26.8) | 484/1457 (33.2) | 726/3134 (23.2) | 434/2461 (17.6) | 245/1168 (21.0) | 104/606 (17.2) | <0.001 |
| Intermediate risk (10%–20%) | 28/56 (50.0) | 500/1457 (34.3) | 1139/3134 (36.3) | 857/2461 (34.8) | 410/1168 (35.1) | 227/606 (37.5) | 0.128 |
| High risk (>20%) | 13/56 (23.2) | 473/1457 (32.5) | 1269/3134 (40.5) | 1170/2461 (47.5) | 513/1168 (43.9) | 275/606 (45.4) | <0.001 |
| Likelihood of CAD | |||||||
| Diamond and Forrester (2011) | <0.001 | ||||||
| Mean (SD) | 35.3 (17.41) | 39.2 (18.29) | 42.4 (18.16) | 41.1 (18.39) | 38.8 (18.09) | 37.0 (17.82) | |
| Low risk (<30%) | 32/56 (57.1) | 658/1459 (45.1) | 1091/3135 (34.8) | 974/2463 (39.5) | 544/1170 (46.5) | 314/606 (51.8) | <0.001 |
| Intermediate risk (30%–70%) | 23/56 (41.1) | 729/1459 (50.0) | 1860/3135 (59.3) | 1353/2463 (54.9) | 564/1170 (48.2) | 261/606 (43.1) | <0.001 |
| High risk (>70%) | 1/56 (1.8) | 72/1459 (4.9) | 184/3135 (5.9) | 136/2463 (5.5) | 62/1170 (5.3) | 31/606 (5.1) | 0.628 |
| Physician’s estimation of likelihood of significant CAD | <0.001 | ||||||
| Very low (<10%) | 6/56 (10.7) | 105/1455 (7.2) | 216/3130 (6.9) | 135/2461 (5.5) | 64/1170 (5.5) | 31/606 (5.1) | |
| Low (10%–30%) | 17/56 (30.4) | 502/1455 (34.5) | 1014/3130 (32.4) | 762/2461 (31.0) | 350/1170 (29.9) | 170/606 (28.1) | |
| Intermediate (31%–70%) | 32/56 (57.1) | 784/1455 (53.9) | 1772/3130 (56.6) | 1442/2461 (58.6) | 690/1170 (59.0) | 365/606 (60.2) | |
| High (71%–90%) | 1/56 (1.8) | 60/1455 (4.1) | 123/3130 (3.9) | 112/2461 (4.6) | 64/1170 (5.5) | 33/606 (5.4) | |
| Very high (>90%) | 0/56 (0.0) | 4/1455 (0.3) | 5/3130 (0.2) | 10/2461 (0.4) | 2/1170 (0.2) | 7/606 (1.2) | |
| Obstructive CAD | |||||||
| Obstructive CAD by CTA or Cath | 2/29 (6.9) | 104/764 (13.6) | 230/1743 (13.2) | 205/1326 (15.5) | 70/631 (11.1) | 37/332 (11.1) | 0.067 |
| Obstructive CAD by CTA | 0/26 (0.0) | 73/707 (10.3) | 178/1627 (10.9) | 161/1229 (13.1) | 48/581 (8.3) | 27/291 (9.3) | 0.013 |
| Obstructive CAD by Cath | 2/4 (50.0) | 73/131 (55.7) | 170/317 (53.6) | 142/251 (56.6) | 58/110 (52.7) | 21/68 (30.9) | 0.010 |
Data are n/N (%) except where indicated.
CTA, computed tomographic angiography; CVD, cardiovascular disease; 90 days of randomization Cath, invasive coronary angiography.
Figure 2.
Pooled risk models versus physician assessment of probability of obstructive coronary artery disease (CAD). Percentage of patients in each body mass index category who were classified as being at high risk of having obstructive CAD by the treating physician or by the updated Diamond-Forrester prediction model.
Figure 3.
Obesity and the observed frequency of obstructive coronary artery disease (CAD). OR (shown on X-axis) of having obstructive CAD for a 10-point increase in the updated Diamond-Forrester score in the patients with body mass index (BMI) <35 or ≥35 kg/m2 (models for CAD were adjusted for chest pain as the primary symptom, smoking [ever/never], diabetes, hypertension, history of peripheral artery or cerebrovascular disease, sedentary lifestyle, depression, family history of premature CAD and dyslipidaemia). The interaction term between BMI ≥35 and the updated Diamond-Forrester pretest probability was significant at p<0.001, indicating that the more obese patients had less frequent prevalence of obstructive CAD than predicted by the risk tool.
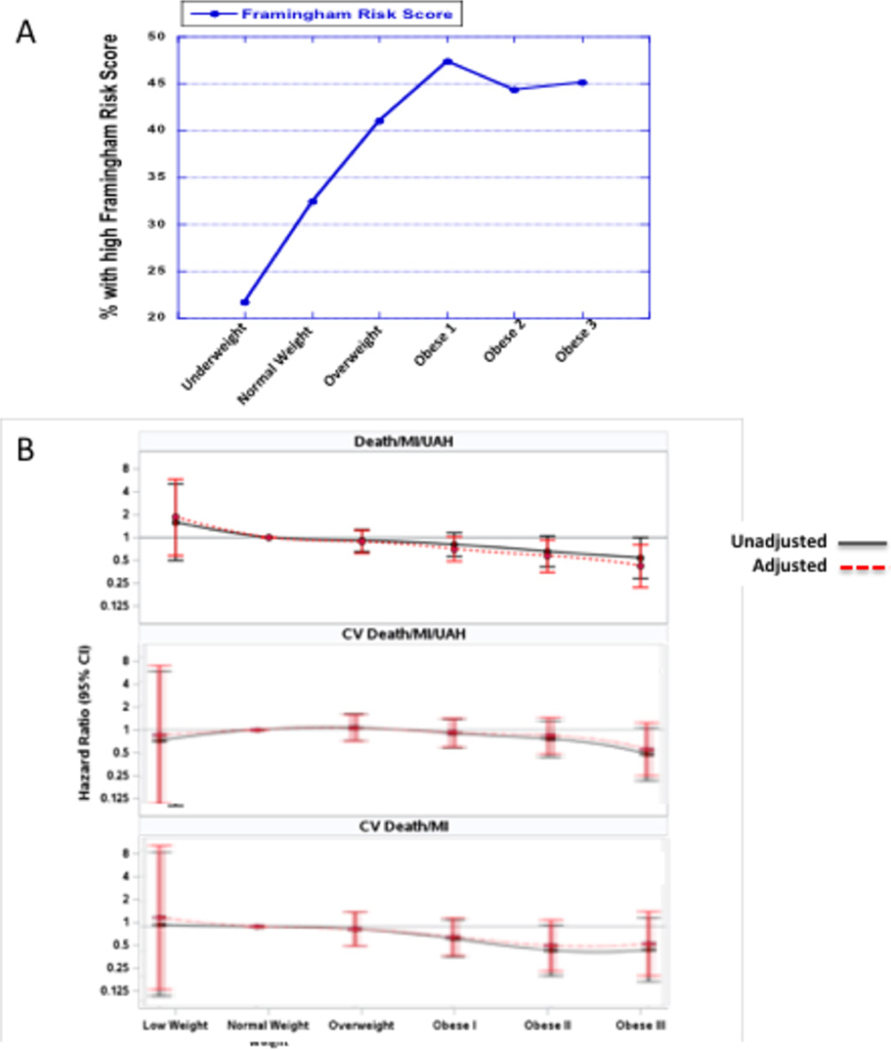
A high Framingham risk, defined as >20% predicted risk of CV events over 10 years, was increasingly prevalent as BMI increased (figure 4A). In contrast, we observed a strong and consistent inverse relationship between measures of obesity and all three composite clinical endpoints over a median 25 months of follow-up in adjusted and unadjusted models (table 3, figure 4B). Sensitivity analysis adjusting only for the Diamond-Forrester score produced similar results (online supplementary table 1). Competing risk models were created for the relevant outcomes, and we found no meaningful or significant changes in the HRs or their CIs (online supplementary table 2). For every 1-unit increase in BMI, the risk of CV death/MI/UAH decreased (adjusted HR 0.96, 95% CI 0.94 to 0.99; p=0.005). For patients with BMI≥35 (n=1776), the risk of CV death/MI/UAH was lower compared with patients with BMI <35 (adjusted HR 0.62, 95% CI 0.41 to 0.91, p=0.016). For patients with BMI ≥40 (n=606), the risk of CV death/MI/UAH was lower compared with patients with BMI <40 (adjusted HR 0.45, CI 0.22 to 0.92, p=0.03). The testing modality that was used (anatomic vs functional) did not modify the association between BMI and any of the three composite endpoints (all interaction p=NS).
Figure 4.
Pooled risk score for clinical events versus observed clinical outcomes. (A) Percentage of patients classified as high risk with Framingham score (>20% predicted 10-year event rate) by WHO body mass index (BMI) obesity categories. (B) Composite clinical outcomes by BMI category: death/myocardial infarction (MI)/unstable angina hospitalisation (UAH); cardiovascular (CV) death/MI/UAH; CV death/MI. Bottom two graphs are adjusted for risk of competing events (non-cardiac death).
Table 3.
Absolute event rates for clinical endpoints based on WHO body mass index Categories
| Clinical endpoint | Overall (n=8889) | Underweight (n=56) | Normal (n=1459) | Overweight (n=3135) | Obese 1 (n=2463) | Obese 2 (n=1170) | Obese 3 (n=606) |
|---|---|---|---|---|---|---|---|
| Death/MI/UAH | 264/8889 (3.0%) | 3/56 (5.4%) | 51/1459 (3.5%) | 101/3135 (3.2%) | 70/2463 (2.8%) | 27/1170 (2.3%) | 12/606 (2.0%) |
| CV death/MI/UAH | 213/8889 (2.4%) | 1/56 (1.8%) | 37/1459 (2.5%) | 87/3135 (2.8%) | 57/2463 (2.3%) | 23/1170 (2.0%) | 8/606 (1.3%) |
| CV death/MI | 130/8889 (1.5%) | 1/56 (1.8%) | 26/1459 (1.8%) | 54/3135 (1.7%) | 32/2463 (1.3%) | 11/1170 (0.9%) | 6/606 (1.0%) |
Data are n/N (%).
CV, cardiovascular;MI, myocardial infarction; UAH, unstable angina hospitalisation.
DISCUSSION
Obesity was present in approximately half of the patients in the PROMISE trial, which enrolled a broadly representative sample of patients in North America being evaluated for possible CAD. Across the spectrum of BMIs, we observed significant differences in both favourable and unfavourable demographic features and individual CV risk factors. There was an inverted U-shaped relationship between BMI category and high pretest probability of obstructive CAD based on pooled risk scores. In contrast, physicians thought that a high probability of obstructive CAD increased uniformly with increasing BMI. The actual prevalence of CAD observed at Cath or CTA was slightly lower in those with BMI ≥35 (12.0%) compared with those with lower BMI (14.6%). Although Framingham Risk Score increased with increasing BMI, the actual clinical events over 25 months of follow-up decreased with increasing BMI.
Despite the growing number of patients in the highest obesity categories,3,17 current guidelines related to evaluation of chest pain are largely silent on the topic of obesity as a confounding condition.11 In part, this is due to a paucity of randomised trial data that would provide the evidence base needed to correctly address the issues of risk assessment and optimal testing strategies. Unlike many published trials that excluded patients with severe obesity, the PROMISE trial did not have a BMI cut-off and hence included large numbers of patients with class 2 and 3 obesity. We found a relatively complex constellation of competing risk factors across the BMI categories. Patients with BMI ≥35 kg/m2 were more likely to have adverse CV risk factors of hypertension, diabetes, sedentary lifestyle and black race. Accordingly, there was a much higher prevalence of metabolic syndrome as BMI increased (table 1). However, the patients with class 2 or 3 obesity tended to have protective factors because they were younger, more likely to be non-smokers and more likely to be female. Age and gender are dominant risk factors for CAD, and hence, differences in these characteristics between groups may have relatively large effects on outcomes. Obese patients were more likely to have dyspnoea as their presenting symptom, one that may be less specific for CAD. Of note, in those patients who had chest pain as the presenting symptom (the vast majority), the typicality of the pain was not different across BMI categories.
Treating physicians tended to believe that more obese patients had a higher pretest probability of obstructive CAD. In comparison, the predictive model suggested a decrease in the probability of obstructive CAD with BMI ≥35. The reasons for the discordance in perceived and calculated risk are not clear. Clinicians usually consider a broader array of patient characteristics than those included in pooled risk scores. In fact, the observed prevalence of obstructive CAD was slightly lower in those with BMI ≥35. This does not indicate that CAD is less prevalent in patients with obesity. Rather, these findings suggest that treating clinicians either: (1) tend to overestimate the probability of CAD in more obese subjects or (2) are uncomfortable in excluding CAD on the basis of routine clinical assessment tools. Application of the Diamond-Forrester score (or other scores) might have been a useful supplement to clinical impressions. However, even this quantitative scoring approach appeared to be less powerful in the most obese patients wherein the same 10-point increase in the predicted probability of CAD was associated with a significantly lower OR of actually finding obstructive CAD (figure 3). Since the Diamond-Forrester score is based only on gender, age and symptoms as predictive variables, this finding may suggest that the assessment of symptoms is less informative in increasingly obese patients.
We observed an even more striking dissociation between clinical events predicted by the Framingham Risk Score and the observed clinical outcomes, using any of three different, adjudicated, composite endpoints. While the percentage of patients considered to be at high risk by Framingham criteria (predicted event rate >20%/10 years) increased across BMI categories, the observed clinical event rates consistently decreased, with HRs approaching 0.5 in the most obese patients. While the absolute event rates were low overall, the data indicated that not all severely obese patients are at high risk.
Higher BMIs have been associated with more favourable outcomes in patients with heart failure,18 known ischaemic heart disease19,20 and suspected CAD.9 These counterintuitive associations, which have been referred to as the ‘obesity paradox’, may be due to many factors, including earlier presentation, more aggressive treatment of risk factors in patients with obesity and unmeasured confounders. Although we attempted to statistically control for as many of these factors as possible, we recognise that residual confounding by unmeasured variables is still likely to be present in a study such as PROMISE.21,22 Some authors have suggested that younger ages in obese patients explain all or part of the apparent protective effects of obesity in patients with CV disease.21,23,24 While our data confirm that more obese patients were younger, the mean age difference between the normal weight group and those with class 3 obesity was 4.2 years, making it unlikely that age alone explains the lower event rates in the more obese patients.
Our study has several limitations. The presence of risk factors was ascertained by history, rather than direct measurements. We did not have direct measures of overall or regional adiposity such as percentage body fat or waist circumference. The former is difficult to obtain and not feasible in a large trial such as this; the latter has theoretical advantages over BMI as a means of classifying obesity, but there are challenges in measuring waist circumference accurately, and current classification schemes for defining abdominal obesity are dichotomous rather than graded. BMI is readily available in most electronic health records, large population databases and clinical trials and has a universal definition with well-established categories. This parameter is easily measured and reproducible and has been widely studied as a measure of adiposity.25 Although BMI misclassifies some patients with respect to presence or severity of obesity, it is accurate in the large majority of patients, and in many large studies performs as well as waist circumference as a predictor of events or mortality.26 All of the diagnostic studies were interpreted locally at the site of patient enrolment. There are potentially important differences between site and core lab interpretations of imaging studies.27 The lack of core laboratory verification of test results in this analysis has implications for the assessment of accuracy of the different testing modalities but does not affect the relationship between BMI and clinical outcomes. By study design, only those receiving CTA or those who went on to invasive angiography (~10% of the total population) had documentation of obstructive CAD. Although the power of the study for endpoints related to the presence of obstructive CAD is lower than would be possible if all of the patients had undergone an anatomic study, the number of patients with an anatomic assessment is still quite large. The number of clinical events was relatively low overall (table 3), and even smaller in each BMI category. While this reduces the power of statistically detecting differences in event rates between the groups, the downward direction of the trends in event rates across rising BMI categories is in the opposite direction of the predicted risks. We do not have measurements of epicardial fat to determine the potential relationship with CAD or outcomes.
CONCLUSIONS
Obesity is very common in contemporary populations undergoing CAD evaluation and higher degrees of obesity are associated with substantial differences in risk factor burden, symptoms and pretest risk assessment. Discordances exist between physician assessment of risk, pooled risk scores and actual event rates that are more pronounced as BMI rises. These data highlight the challenges that providers face when evaluating and managing an increasingly obese patient population and support the need for more specific guidelines that incorporate anthropomorphic measures.
Supplementary Material
Key messages.
What is already known on this subject?
Obesity is thought to be a risk factor for premature and accelerated progression of coronary artery disease (CAD). However, the association between obesity and clinical outcomes is less clear. The presence or severity of obesity is not included in the commonly used risk scores for the presence of CAD (Diamond-Forrester score) or the risk of cardiovascular events (Framingham Risk Score).
What might this study add?
This large, prospective study gives insight into the perspectives and testing patterns of practising physicians. In 10 003 patients presenting with chest pain, we found complex patterns of risk factors that varied across the spectrum of body mass index (BMIs). Treating physicians predicted a higher probability of obstructive CAD in those with more severe obesity, while the Diamond-Forrester score had an inverted U shape. Actual rates of CAD were lower than expected with BMI >35. Framingham Risk Score increased across BMI categories, while adverse event rates went down with increasing BMI.
How might this impact on clinical practice?
These findings highlight the need for risk assessment tools and guidelines that account for presence and severity of obesity.
Acknowledgments
Funding The PROMISE trial was funded by National Heart, Lung, and Blood Institute grants R01 HL098237, R01 HL098236, R01 HL098305, and R01 HL098235.
SEL reports receiving fees for events adjudication committee from CVRx. NP reports ownership in Freedom Health, Inc; Physician Partners, LLC; RXAdvance, LLC; and Florida Medical Associates, LLC. KLL reports receiving grants from the National Institutes of Health. DM reports receiving grants from the National Institutes of Health, as well as personal fees from CardioDx, Medtronic, Inc and St. Jude Medical, and grants from Eli Lilly and Company, Bristol-Myers Squibb, Gilead Sciences, Inc, AGA Medical Corporation, Merck & Company, Oxygen Therapeutics and AstraZeneca. JEU reports receiving consulting fees/honoraria from Lantheus Medical Imaging; service on a data safety monitoring board for Gilead, GSK; service as an officer, director, trustee or other fiduciary role for HFSA Executive Council; other support from or service for Abbott Laboratories, Circulation/AHA – Associate Editor, Editor – Circulation Heart Failure, Pfizer/GlaxoSmithKline, Sunshine Heart; and receiving research grants from NHLBI, Otsuka. J-CT reports receiving grants from Amarin, AstraZeneca, Dalcor, Esperion, Ionis, Merck, Pfizer, Sanofi and Servier; honoraria from Dalcor, Pfizer, Sanofi and Servier; and owns a minor equity interest in Dalcor. UH reports receiving grants from the American College of Radiology Imaging Network, HeartFlow Inc and Siemens Healthcare. PSD reports receiving grant support from HeartFlow and service on a data and safety monitoring board for GE HealthCare.
Footnotes
Competing interests The other authors report no potential conflicts of interest.
Patient consent for publication Not required.
Provenance and peer review Not commissioned; externally peer reviewed.
Data availability statement Data are available in a public, open access repository.
Additional material is published online only. To view please visit the journal online (http://dx.doi.org/10.1136/heartjnl-2018-314503).
REFERENCES
- 1.Cheng VY, Berman DS, Rozanski A, et al. Performance of the traditional age, sex, and angina typicality-based approach for estimating pretest probability of angiographically significant coronary artery disease in patients undergoing coronary computed tomographic angiography: results from the multinational coronary CT angiography evaluation for clinical outcomes: an international multicenter registry (confirm). Circulation 2011;124:2423–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Genders TSS, Steyerberg EW, Alkadhi H, et al. A clinical prediction rule for the diagnosis of coronary artery disease: validation, updating, and extension. Eur Heart J 2011;32:1316–30. [DOI] [PubMed] [Google Scholar]
- 3.Flegal KM, Kruszon-Moran D, Carroll MD, et al. Trends in obesity among adults in the United States, 2005 to 2014. JAMA 2016;315:2284–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jahangir E, De Schutter A, Lavie CJ. The relationship between obesity and coronary artery disease. Transl Res 2014;164:336–44. [DOI] [PubMed] [Google Scholar]
- 5.Wilson PWF, D’Agostino RB, Sullivan L, et al. Overweight and obesity as determinants of cardiovascular risk: the Framingham experience. Arch Intern Med 2002;162:1867–72. [DOI] [PubMed] [Google Scholar]
- 6.Manson JE, Colditz GA, Stampfer MJ, et al. A prospective study of obesity and risk of coronary heart disease in women. N Engl J Med 1990;322:882–9. [DOI] [PubMed] [Google Scholar]
- 7.Rexrode KM, Carey VJ, Hennekens CH, et al. Abdominal adiposity and coronary heart disease in women. JAMA 1998;280:1843–8. [DOI] [PubMed] [Google Scholar]
- 8.McGillHCJr McMahan CA, Herderick EE, et al. Pathobiological determinants of atherosclerosis in youth Research Group. obesity accelerates the progression of coronary atherosclerosis in young men. Circulation 2002;105:2712–8. [DOI] [PubMed] [Google Scholar]
- 9.Hulten EA, Bittencourt MS, Preston R, et al. Obesity, metabolic syndrome and cardiovascular prognosis: from the partners coronary computed tomography angiography registry. Cardiovasc Diabetol 2017;16:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Goff DC, Lloyd-Jones DM, Bennett G, et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American heart association Task force on practice guidelines. J Am Coll Cardiol 2014;63::2935–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fihn SD, Blankenship JC, Alexander KP, et al. ACC/AHA/AATS/PCNA/SCAI/STS focused update of the Guideline for the diagnosis and management of patients with stable ischemic heart disease: a report of the American College of Cardiology/American heart association Task force on practice guidelines, and the American association for thoracic surgery, preventive cardiovascular nurses association, Society for cardiovascular angiography and interventions, and society of thoracic surgeons. J Am Coll Cardiol 2014;2014:1929–49. [DOI] [PubMed] [Google Scholar]
- 12.Montalescot G, Sechtem U, Achenbach S, et al. 2013 ESC guidelines on the management of stable coronary artery disease: the task force on the management of stable coronary artery disease of the European Society of cardiology. Eur Heart J 2013;34:2949–3003. [DOI] [PubMed] [Google Scholar]
- 13.Mancini GBJ, Gosselin G, Chow B, et al. Canadian cardiovascular Society guidelines for the diagnosis and management of stable ischemic heart disease. Can J Cardiol 2014;30:837–49. [DOI] [PubMed] [Google Scholar]
- 14.Douglas PS, Hoffmann U, Lee KL, et al. Prospective multicenter imaging study for evaluation of chest pain: rationale and design of the promise trial. Am Heart J 2014;167:796–803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Douglas PS, Hoffmann U, Patel MR, et al. Outcomes of anatomical versus functional testing for coronary artery disease. N Engl J Med 2015;372:1291–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.D’Agostino RB, Vasan RS, Pencina MJ, et al. General cardiovascular risk profile for use in primary care: the Framingham heart study. Circulation 2008;117:743–53. [DOI] [PubMed] [Google Scholar]
- 17.Ogden CL, Carroll MD, Lawman HG, et al. Trends in obesity prevalence among children and adolescents in the United States, 1988–1994 through 2013–2014. JAMA 2016;315:2292–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Oga EA, Eseyin OR. The obesity paradox and heart failure: a systematic review of a decade of evidence. J Obes 2016;2016:9040248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Niedziela J, Hudzik B, Niedziela N, et al. The obesity paradox in acute coronary syndrome: a meta-analysis. Eur J Epidemiol 2014;29:801–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Holroyd EW, Sirker A, Kwok CS, et al. British cardiovascular intervention Society and National Institute of cardiovascular outcomes research. The relationship of body mass index to percutaneous coronary intervention outcomes: does the obesity paradox exist in contemporary percutaneous coronary intervention cohorts? insights from the British cardiovascular intervention Society registry. JACC Cardiovasc Interv 2017;10:1283–92. [DOI] [PubMed] [Google Scholar]
- 21.Charnigo R, Guglin M. Obesity paradox in heart failure: statistical artifact or impetus to rethink clinical practice? Heart Fail Rev 2017;22:13–23. [DOI] [PubMed] [Google Scholar]
- 22.O’Brien EC, Thomas LE. Untangling the paradox: obesity as prognostic marker in prevalent cardiovascular disease. Am Heart J 2016;172:170–2. [DOI] [PubMed] [Google Scholar]
- 23.Guglin M, Baxi K, Schabath M. Anatomy of the obesity paradox in heart failure. Heart Fail Rev 2014;19:621–35. [DOI] [PubMed] [Google Scholar]
- 24.Fonarow GC, Srikanthan P, Costanzo MR, et al. An obesity paradox in acute heart failure: analysis of body mass index and inhospital mortality for 108,927 patients in the acute decompensated heart failure national registry. Am Heart J 2007;153:74–81. [DOI] [PubMed] [Google Scholar]
- 25.Global BMI Mortality Collaboration, Di Angelantonio E, Bhupathiraju S, ShN B, et al. Body-Mass index and all-cause mortality: individual-participant-data meta-analysis of 239 prospective studies in four continents. Lancet 2016;388:776–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Litwin SE. Which measures of obesity best predict cardiovascular risk? J Am Coll Cardiol 2008;52:616–9. [DOI] [PubMed] [Google Scholar]
- 27.Lu MT, Meyersohn NM, Mayrhofer T, et al. Central core laboratory versus site interpretation of coronary CT angiography: agreement and association with cardiovascular events in the promise trial. Radiology 2018;287:87–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.