Abstract
The emergence of multidrug-resistant bacteria is a worldwide health problem. Antimicrobial peptides have been recognized as potential alternatives to conventional antibiotics, but still require optimization. The proline-rich antimicrobial peptide Bac7(1-16) is active against only a limited number of Gram-negative bacteria. It kills bacteria by inhibiting protein synthesis after its internalization, which is mainly supported by the bacterial transporter SbmA. In this study, we tested two different lipidated forms of Bac7(1-16) with the aim of extending its activity against those bacterial species that lack SbmA. We linked a C12-alkyl chain or an ultrashort cationic lipopeptide Lp-I to the C-terminus of Bac7(1-16). Both the lipidated Bac-C12 and Bac-Lp-I forms acquired activity at low micromolar MIC values against several Gram-positive and Gram-negative bacteria. Moreover, unlike Bac7(1-16), Bac-C12, and Bac-Lp-I did not select resistant mutants in E. coli after 14 times of exposure to sub-MIC concentrations of the respective peptide. We demonstrated that the extended spectrum of activity and absence of de novo resistance are likely related to the acquired capability of the peptides to permeabilize cell membranes. These results indicate that C-terminal lipidation of a short proline-rich peptide profoundly alters its function and mode of action and provides useful insights into the design of novel broad-spectrum antibacterial agents.
Keywords: lipidation, antimicrobial peptide, lipopeptide, membrane permeabilization, antibiotic resistance, antimicrobial agent, broad-spectrum activity
1. Introduction
The consequences of the spread of multidrug-resistant pathogens are recognized as a global health problem and reduce the chances of successful treatment of infections [1]. Moreover, resistance to last-resort antibiotics, such as colistin, for the treatment of Gram-negative infections is spreading rapidly [2,3]. In this scenario, it is crucial to develop molecules with new or improved activities against bacteria and low toxicity against the host. Antimicrobial peptides (AMPs), also known as host defence peptides (HDPs), are natural defence effectors produced by animals and plants to counteract microorganisms [4,5] and have been proposed as potential alternatives to conventional drugs [6,7].
Most AMPs are cationic and amphipathic molecules that are attracted to the negatively charged bacterial membranes, resulting in perturbation and damage to the lipid bilayer [8]. As a result, AMPs generally exhibit a broad spectrum of activity and low selectivity against cell targets [9]. In contrast, the group of proline-rich antimicrobial peptides (PrAMPs) act on bacterial intracellular targets without apparent membrane damage [10,11]. Among PrAMPs, those from insects and mammals represent the best studied examples [12,13,14].
Several PrAMPs have been shown to require specific bacterial membrane proteins (such as SbmA and the MdtM complex) to enter the bacterial cytoplasm [15,16,17], and this restricts their antibacterial activity to bacteria, among the Gram-negative, that express these transporters [18]. Within bacterial cells, PrAMPs inhibit the elongation phase of protein synthesis by binding in the exit tunnel of the ribosome [19,20,21,22] and probably other functions associated with the chaperone DnaK [23].
Some N-fragments of the mammalian PrAMP Bac7, Bac7(1-16) and Bac7(1-35), display antimicrobial activity at micromolar concentrations against Gram-negative pathogens including Acinetobacter baumannii, Salmonella spp., and Klebsiella pneumoniae, but not against Staphylococcus aureus and other Gram-positive species [24,25,26,27].
Narrow-spectrum antibacterial agents may attenuate the selection and spread of bacterial resistance if the causative agent of the infection is known. However, in severe infections where treatment must be initiated before the pathogen is identified, a broad-spectrum agent is preferable [28,29]; hence the need to optimize PrAMPs to broaden their spectrum of activity. The natural antimicrobial efficacy and safety of AMPs have been improved by various strategies [30]. A well-documented method to enhance the efficacy of AMPs is the conjugation of the peptide with aliphatic fatty acids, resulting in synthetic lipopeptides [31]. Studies of synthetic lipopeptides evidenced that acylated AMPs exhibit improved cell selectivity and excellent activity, especially against Gram-positive bacteria [32,33,34].
Previously, we screened a library of Arg-rich ultrashort cationic antimicrobial lipopeptides (USCLs) based on the Arg-X-Trp-Arg-NH2 peptide moiety conjugated to a fatty acid. Lp-I was identified as the candidate that exhibited the highest antimicrobial activity against Gram-positive bacteria with low cytotoxicity [35]. In contrast, adding a lipid moiety to PrAMPs to broaden their spectrum of activity has hardly been investigated. A first attempt was made by linking aliphatic groups to the N-terminus of short consensus sequences derived from different PrAMPs, resulting in new derivatives with moderate antimicrobial activity [36].
In this study, we investigated the effects of lipidation of the PrAMP Bac7(1-16) to extend its antimicrobial activity to bacterial species lacking dedicated transport systems. Two different derivatives were synthesized, in which Bac7(1-16) was linked at its C-terminus to a C12-alkyl chain or to the ultrashort cationic lipopeptide Lp-I. The lipidated forms were tested for their antimicrobial activity against a broad panel of bacterial species, their cytotoxicity was assessed on human erythrocytes and nucleated cells, and their tendency to select bacterial resistance was evaluated. The results of this study indicated that the addition of a lipid component to the peptide strongly influences not only the spectrum of activity, but also the mechanism of action and the rate of appearance of resistant mutants. These findings contribute to the understanding of the effects of PrAMP lipidation and will be useful in the development of innovative and more effective antimicrobial agents.
2. Results
2.1. Bac-C12 and Bac-Lp-I Design
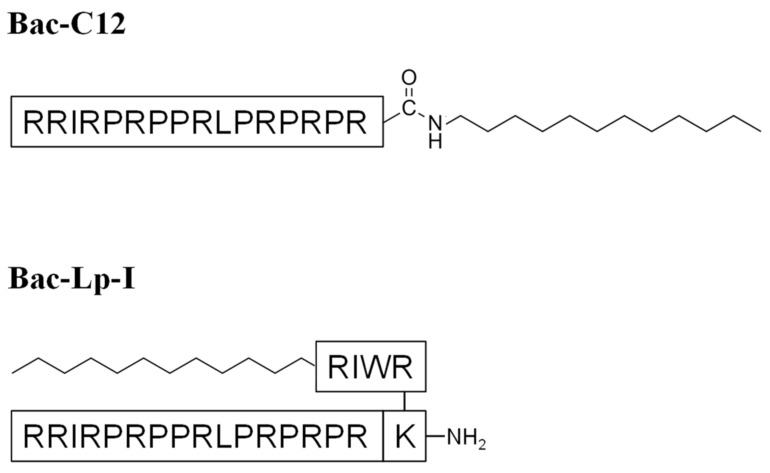
Two different lipidated Bac7(1-16) derivatives were designed as schematically shown in Figure 1. The C-terminus of Bac7(1-16) was linked by an amide bond to a dodecylamine (C12-alkyl chain), obtaining the lipopeptide Bac-C12. The length of the hydrocarbon tail (C12) allowed to obtain sufficient solubility of the molecule. The second derivative, Bac-Lp-I, was designed by joining Bac7(1-16) and the previously characterized ultrashort lipopeptide Lp-I [35], constituted by the tetrapeptide RWIR linked at the N-terminus to a C12 fatty acid. Lp-I was linked to Nε of Bac7(1-16) modified at the C-terminus with an additional C-terminal lysine (Figure 1).
Figure 1.
Chemical structures of Bac-C12 (MW: 2244.03) and Bac-Lp-I (MW: 2998.02).
2.2. Antimicrobial Activity of Bac-C12 and Bac-Lp-I
We compared the antimicrobial activity of the two different lipidated forms of Bac7(1-16) with that of the original peptides Bac7(1-16) and Lp-I against a panel of Gram-positive and Gram-negative reference strains and against a clinical isolate of Escherichia coli O18K1H7 (Table 1). In general, both Bac-C12 and Bac-Lp-I displayed a broadened spectrum of activity against Gram-positive and Gram-negative bacteria and, in most cases, better antimicrobial activity than the original molecules.
Table 1.
Minimum inhibitory concentration (MIC) and minimal bactericidal concentration (MBC) of lipidated Bac7(1-16) derivatives and their parental peptides.
| Bacteria Strain | MIC (μM) | MBC (μM) | ||||
|---|---|---|---|---|---|---|
| Bac7(1-16) | Lp-I | Bac-C12 | Bac-Lp-I | Bac-C12 | Bac-Lp-I | |
| B. subtilis DSMZ 4181 | 1 | 4 | 4 | 2 | 4 | 2 |
| E. faecalis ATCC 29212 | >64 | 8 | 8 | 4 | 8 | 8 |
| S. aureus ATCC 25923 | >64 | 4 | 4 | 2 | 8 | 4 |
| S. aureus ATCC 29213 | >64 | 4 | 2 | 4 | 4 | 4 |
| S. epidermidis ATCC 12228 | >64 | 8 | 2 | 2 | 2–4 | 2 |
| A. baumannii ATCC 17978 | 16 | 32 | 8 | 2 | 16 | 4 |
| A. baumannii ATCC 19606 | 64 | 32 | 8 | 4 | 8 | 4 |
| B. cepacia J2315 | >64 | 16 | 2 | 8 | n.d. | 8 |
| E. coli ATCC 25922 | 2 | 8 | 8 | 4 | 8 | 8 |
| E. coli BW25113 | 4 | 8 | 4 | 4 | 4 | 16 |
| E. coli BW25113ΔsbmA | 32 | n.d. | 4 | 4 | 4 | 4 |
| E. coli O18K1H7 # | >64 | 16 | 8 | 8 | 8 | 16 |
| K. pneumoniae ATCC 700603 | 8 | 64 | 8 | 4 | 8 | 4 |
| K. pneumoniae ATCC 13883 | 4 | >64 | 4 | 4 | 32 | 8 |
| P. aeruginosa ATCC 27853 | >64 | 16 | 8 | 8 | 16 | 16 |
| P. aeruginosa PAO1 | >64 | 16 | 8 | 8 | >64 | 16 |
| S. typhimurium ATCC 14028 | 2 | 32 | 4 | 2 | 8–16 | 4 |
| S. maltophilia ATCC 13637 | >64 | 8 | 2 | 8 | 4 | 16 |
# Clinical isolates. Results derived from at least three independent experiments carried out at least in duplicate. MIC and MBC were recorded after 18 h and 24 h of incubation, respectively, for all strains with the exception of B. cepacia and S. maltophilia, needing 48 h. MIC and MBC values are reported as mode of the results. n.d. = value not determined.
Bac-C12 and Bac-Lp-I were more active than the single native peptides against Staphylococcus epidermidis ATCC 12228, Burkholderia cepacia J2315, E. coli O18K1H7, Pseudomonas aeruginosa, and Acinetobacter baumannii strains, with MIC values ranging from 2 μM to 8 μM. In contrast, lipidation did not increase efficacy against Bacillus subtilis DSMZ 4181, E. coli ATCC 25922, and Salmonella enterica serovar typhimurium ATCC 14028, where Bac7(1-16) MICs were equal to or twofold better than the lipidated variant.
Interestingly, lipidation strongly increased activity against Gram-positive Enterococcus faecalis ATCC 29212, Staphylococcus aureus strains and S. epidermidis ATCC 12228 (MIC range 2–8 μM), which were resistant to Bac7(1-16) (MIC 64 μM). Bac-C12 showed higher antimicrobial activity than Bac-Lp-I against S. aureus ATCC 29213, Stenotrophomonas maltophilia and B. cepacia. No major differences were observed in other cases, suggesting that the presence of the C-12 lipid tail played a more important role in improving antimicrobial activity than the addition of the lipotetrapeptide RWIR (Lp-I) (Table 1).
Overall, these results indicate an impressive enlargement of the inhibitory activity of the two lipidated forms of Bac7(1-16), extending to bacterial species lacking the bacterial transport system [17]. The only exception was B. subtilis, although it is generally recognized as a nonpathogenic strain [37].
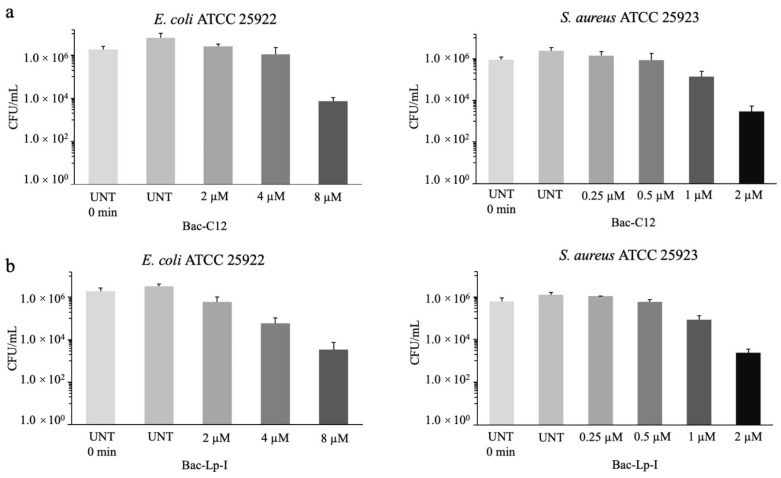
Both Bac-C12 and Bac-Lp-I showed bactericidal values (MBC) similar to or twofold higher than MICs, suggesting bactericidal activity of these derivatives. The bactericidal activity of Bac-C12 and Bac-Lp-I was also determined against E. coli ATCC 25922 and S. aureus ATCC 25923 using the viable colony count method. A 30 min exposure to Bac-C12 caused a 2.9-log reduction in E. coli and S. aureus cells (CFU/mL) at 8 μM and 2 μM, respectively, values close to the MICs (Figure 2, panel a). The effect of Bac-Lp-I against the same strains was very similar to that of Bac-C12. This derivative started to reduce the cell number of E. coli and S. aureus at 4 μM and 1 μM, respectively, at concentrations close to the MIC (Figure 2, panel b). These results indicate that lipidation does not lower the bactericidal capability of Bac7(1-16) that has been previously determined [27].
Figure 2.
Evaluation of the bactericidal activity of Bac-C12 and Bac-Lp-I on E. coli ATCC 25922 and S. aureus ATCC 25923. The bactericidal activity with Bac-C12 (panel a) and Bac-Lp-I (panel b) on E. coli ATCC 25922 and S. aureus ATCC 25923 cells was determined using a mid-logarithmic phase bacterial suspension, diluted in fresh MHB to a final concentration of 106 CFU/mL, and incubated for 30 min at 37 °C with increasing concentrations of peptide. Samples were then diluted in PBS, plated on MH agar, and incubated overnight to allow the colony counts. UNT = untreated cells. Data are the mean ± SD of three independent experiments.
2.3. Evaluation of Cytotoxicity of Bac-C12 and Bac-Lp-I
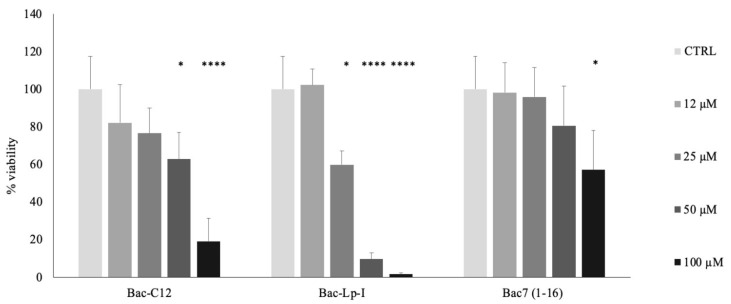
We evaluated the possible cytotoxic effects of Bac-C12 and Bac-Lp-I on human red blood cells (hRBCs) and human keratinocytes. Both lipidated peptides displayed ≤3% hemolysis even at 100 μM, the highest concentration tested, indicating that Bac-C12 and Bac-Lp-I do not damage hRBCs even at concentrations far above the microbicidal ones (Figure S1, Supplementary Materials). We then assayed the effects of the peptides on human epidermal keratinocytes (HaCaT). HaCaT cells were exposed to Bac-C12, Bac-Lp-I, or Bac7(1-16) for 24 h at various concentrations. Bac-Lp-I reduced cell viability starting at 25 μM (decrease of approximately 40%) with a further decrease in viability at 50 and 100 μM. Bac-C12 was found to be non-toxic at 25 μM but reduced keratinocyte viability at 50 μM (decrease of approximately 40%) (Figure 3). Since Bac7(1-16) affected the viability of the same cells starting from 100 μM (Figure 3), these results suggest that the addition of a lipid tail has some effects on host cells and that lipopeptides are less selective for their cell target. The addition of C-12 alone to Bac7(1-16) had a less pronounced effect than the addition of lipotetrapeptide (Bac-Lp-I). In either case, both lipidated forms acted on cells at concentrations 3–8-fold higher than the microbicidal ones. The biocompatibility of Bac-C12 was also assayed against the human line of lymphocyte precursors MEC-1. Similar results were obtained, with the decrease in cell viability at 32 μM (Figure S2, Supplementary Materials) confirming the trend highlighted in Figure 3.
Figure 3.
Cell viability of human epidermal keratinocytes HaCaT cells treated with Bac-C12, Bac-Lp-I, or Bac7(1-16). Cell viability was evaluated after 24 h incubation with indicated concentrations of peptides by using the MTT assay. PBS was used as a control. The cell viability is expressed as a percentage of MTT absorbance (570 nm) measured on untreated cells (ctrl) assumed as 100% viability. Each value represents the mean ± SEM of three independent experiments performed in triplicate. * p < 0.05 vs. untreated cells (ctrl), and **** p < 0.0001 vs. untreated cells (ctrl) (Kruskal–Wallis test and ANOVA).
2.4. Resistance Selection in E. coli by Bac-C12 and Bac-Lp-I
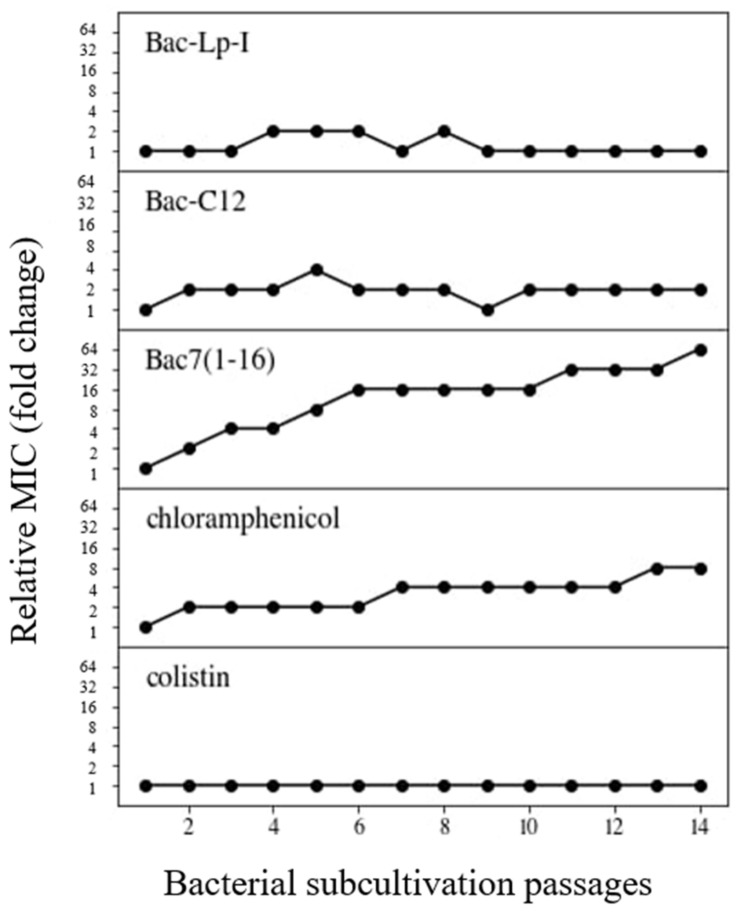
Since bacteria become resistant to most antibiotics quite quickly, we have investigated whether Bac7(1-16) derivatives at sub-MIC concentrations could select for de novo resistance in bacteria within a few generations. To detect possible appearance of resistant mutants, bacterial cultures of E. coli ATCC 25922 were subjected to 14 consecutive MIC assays performed as described in the Materials and Methods section and the presence of resistant mutants was reported as an increase in relative MIC.
Within the E. coli passages, a 2-fold increase in MIC values was observed for Bac-C12, while MIC of Bac-Lp-I did not increase at all and, if anything, showed a 2-fold variation (Figure 4 and Table S1, Supplementary Materials). This behavior was similar to that of colistin, used as a reference for a membranolytic agent, where no increase in MIC values was observed. The relative MIC of Bac7(1-16) was 64-fold higher than the initial MIC, similarly to what was observed with chloramphenicol (Figure 4). In fact, the MIC of chloramphenicol increased from 4-fold to 64-fold within three independent experiments (Figure 4 and Table S1, Supplementary Materials).
Figure 4.
Susceptibility variation of E. coli ATCC 25922 to different lipopeptides and antibiotics. Relative MIC values represent the MIC fold-change observed during 14 passages of bacterial subcultures compared to the original MIC value against the wild-type. Bacterial cells grown at the highest concentration of the antimicrobial (1/2MIC) were subcultured and used for the next MIC assay. The procedure was repeated for 14 passages. Chloramphenicol and colistin were used as reference antibiotics for non-lytic and lytic mode of action, respectively. Each plot represents a representative result of assays repeated at least two times. Whole data are reported in Table S1, Supplementary Materials.
Overall, these results indicate that bacteria become quite easily less susceptible to Bac7(1-16), while selection of a novel strain resistant to its derivatives Bac-C12 and Bac-Lp-I seems to be a more difficult event.
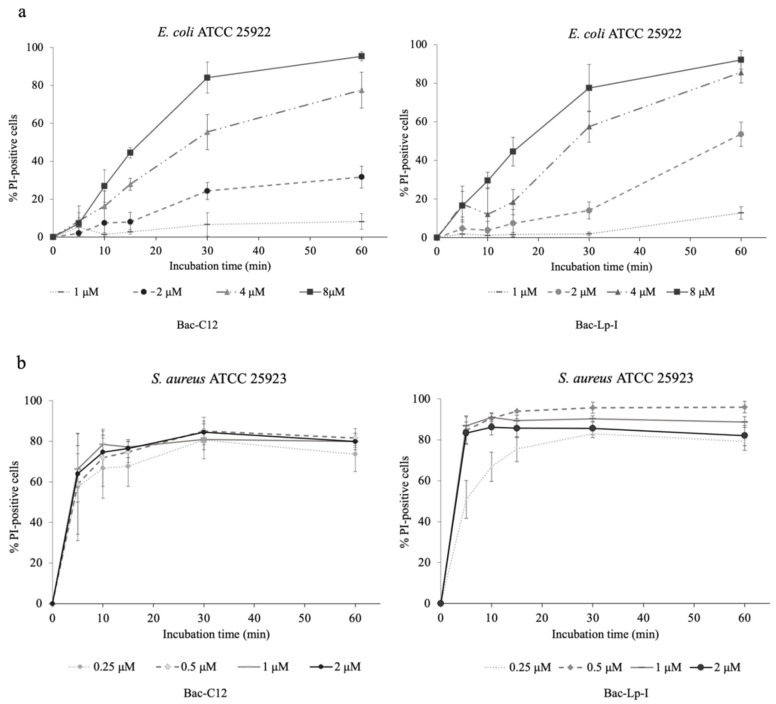
2.5. Assessment of the Integrity of the Bacterial Cell Membrane
Since the addition of an alkyl chain to peptides is expected to increase their interaction with membranes, we examined the effects of lipopeptides on membrane integrity. The propidium iodide uptake assay was performed on E. coli ATCC 25922 and S. aureus ATCC 25923 used as representatives of Gram-negative and Gram-positive strains, respectively, and exposed to Bac-C12 or Bac-Lp-I at the same concentrations used in killing experiments. Bac-C12 and Bac-Lp-I increased the number of PI-positive cells within a few minutes and in a concentration-dependent manner (Figure 5), indicating that both lipopeptides acquired the capability to permeabilize bacterial cells at the same or even lower bactericidal concentrations. By contrast, the original Bac7(1-16) did not increase the number of permeabilized cells (data not shown), in agreement with previous data [27].
Figure 5.
Membrane-damaging activity of Bac-C12 and Bac-Lp-I on E. coli ATCC 25922 (a) and S. aureus ATCC 25923 (b). The permeabilization assay with Bac-C12 and Bac-Lp-I has been performed in MHB. Bacterial cells were treated, for different incubation times, with indicated concentrations of peptide. % PI-positive: percentage of propidium iodide-positive cells. The background level of permeabilized cells, obtained with untreated samples, was always below 2% and was subtracted to the corresponding peptide-treated sample. Data are the mean ± SD of four independent experiments.
Very similar effects on membranes were observed between Bac-C12 and Bac-Lp-I. Both peptides permeabilized more than 80% of E. coli cells after 30 min of treatment at MIC concentration (4–8 μM) (Figure 5, panel a). An even higher degree of permeabilization was observed in S. aureus cells. Bac-C12 and Bac-Lp-I damaged the cells already at 0.25 μM, a sub-MIC concentration. Bac-Lp-I at 0.5 μM permeabilized 80% of the cells within only a 10 min incubation, while Bac-C12 at 0.5 μM achieved the same percentage of permeabilized cells within 20 min (Figure 5, panel b). These results clearly show that the addition of the lipid chain dramatically changes the behavior of both derivatives and clearly suggest that cell permeabilization has become the main mechanism of killing.
3. Discussion
PrAMPs are in the spotlight for the development of new antibiotics, but their narrow spectrum of activity may hinder their further progress toward clinical use [14,18]. Therefore, in recent years, great efforts have been made to expand the antimicrobial spectrum of PrAMPs by introducing sequence modification, residue substitution, or both [27,38,39,40,41]. In this study, we tested the effect of lipidation on the mammalian PrAMP Bac7(1-16) and demonstrated that the addition of a lipid chain to Bac7(1-16) greatly enhanced its antibacterial activity. We also demonstrated that the improvement was likely associated with a modification of the killing mechanism.
Both the C12-alkylated Bac7(1-16) and the chimeric Bac-Lp-I lipopeptide displayed higher antimicrobial activity against some pathogenic species and a broad spectrum of activity targeting a larger number of bacterial species, including Gram-positive bacteria. The molecules showed an MIC of ≤ 8 μM against all bacterial species tested, regardless of whether they were Gram-positive or Gram-negative (see Table 1). In addition, the panel of pathogens tested included among the reference strains also most of the ESKAPE listed by WHO as species of greatest concern for human health [42]. Thus, Bac-C12 and Bac-Lp-I was shown to inhibit pathogens of relevant clinical interest. The extended spectrum of activity is probably related to the capability of Bac-C12 and Bac-Lp-I to act independently of the presence of the bacterial membrane proteins SbmA or MdtM. Thus, the antimicrobial mechanism of these lipopeptides acting directly on bacterial membranes is not limited to the few bacterial species expressing these transport proteins. This is also an interesting result because any mutation of the transporter that affects peptide internalization could lead to decreased susceptibility to these PrAMPs [43]. A highly efficient system of peptide transport through SbmA for the non-lytic native Bac7(1-16) might also explain the reason why the E. coli strains 25922 and BW25113 continued to be more susceptible to Bac7(1-16) than to its lipidated derivatives. Further studies, such as the determination of the level of expression of SbmA in the distinct E. coli stains, could be useful to clarify this point as well as the high potency of Bac7(1-16) against B. subtilis DSMZ 4181.
The lipidated derivatives were designed using the previously characterized PrAMP Bac7(-1-16) [24,27]. The C12 lipid tail was added to the C-terminus as it is known to play a minor role in ribosome inhibition and antimicrobial activity of the peptide [22]. The second lipopeptide, synthesized by linking Bac7(1-16) with the ultrashort lipopeptide Lp-I [35], was designed with the aim of obtaining a new molecule that had the sum of the activities of the individual peptides. The results showed that there is a slight difference between the antibacterial activity of Bac-C12 and Bac-Lp-I, suggesting that the addition of the alkyl-C12 chain rather than the addition of the ultrashort lipopeptide plays the prevalent role in enhancing the antimicrobial activity (see Table 1).
Lipidation is a commonly used approach to enhance or modulate the antimicrobial activity of AMPs such as the α-helical peptides (comprehensive review in [33]). In contrast, there is limited information on PrAMP modified by lipids. Short proline-rich lipopeptides were developed by Domalaon et al. by combining a PR-rich heptapeptide with N-terminal fatty acids of different lengths [36]. Of the lipopeptides tested, only those with a C-18 chain exerted moderate antimicrobial activity, while those with a C-12 chain were not active except when tested in combination with other compounds [36]. These results are consistent with previous observations highlighting the importance of a free N-terminus in the antimicrobial activity and mechanism of action of mammalian PrAMPs [21,44,45]. Moreover, the weak activity of the lipidated PR-rich heptapeptide suggests that a seven-residue peptide is too short and reinforces the observation that 16–17-residue peptides are the shortest ones that exhibit antimicrobial activity [21,24,44].
Mode of action analysis showed that lipidation of Bac7(1-16) clearly transformed a non-permeabilizing peptide into a markedly membrane-active molecule. Both lipidated forms destabilized the bacterial membranes of E. coli and, more pronouncedly, those of S. aureus even at sub-MIC concentrations, strongly indicating that membrane permeabilization is a process clearly correlated with bacterial killing. Interestingly, the kinetics of bacterial membrane permeabilization by Bac-C12 were very similar to those observed in the same microorganisms using the lipopeptide Lp-I [35], suggesting that the two molecules have a very similar mechanism of action.
The other two effects of Bac-C12 and Bac-Lp-I noted in this study, i.e., the lack of appearance of resistant mutants within 14 consecutive passages and the increased cytotoxicity, are much likely related to the mechanism of membrane permeabilization.
Indeed, both lipopeptides did not allow selection of de novo resistance in the treated E. coli cultures even after long exposure (14 passages), which is thus an interesting and desirable property for antibiotics. This behavior is very similar to that of the well-known permeabilizing antibiotic colistin. In contrast, Bac7(1-16), which has specific targets for internalization and activity, rapidly increased its MIC value under the same experimental conditions. This result is consistent with a modification of the killing mechanism by the addition of the lipid moiety and the acquisition of non-specific targets such as the bacterial membrane. Resistance to many AMPs can evolve at measurable rates, at least in vitro [46]. However, the MIC increase in mutants for membrane-acting AMPs is lower than that for antibiotics with specific molecular targets. Our results suggest that the acquisition of a lipid chain reduces the rates of mutant selection. This observation is consistent with a study performed on the longer fragment Bac7(1-35) [26]. This peptide is less dependent than Bac7(1-16) on SbmA for its internalization [17] and at high concentrations also exerts membrane destabilizing activity [47]. It has been shown that also Bac7(1-35) did not select resistance in A. baumannii AB5075 strain after 14 passages.
The addition of the two lipid moieties also affects the biocompatibility of Bac7(1-16) toward host cells. Bac-C12 and, more significantly, Bac-Lp-I began to reduce cell viability of keratinocytes at 2–4 lower concentrations than the peptide alone. This result was quite expected, since the introduction of an alkyl chain into antimicrobial peptides often enhances the cytotoxic effects [48]. On the other hand, the difference in cytotoxicity between Bac-C12 and Bac-Lp-I was not obvious. It was generally observed that the cytotoxicity of lipopeptides increases with the length of their hydrophobic chain [48]. The tryptophan residue present in Lp-I and the linker used to link Bac7(1-16) and Lp-I contribute to increase the hydrophobicity of the molecule, perhaps making it more cytotoxic compared to Bac-C12.
It remains unclear what properties the peptide moiety in lipopeptides should have to optimize their activity. To date, it has not been possible to draw general lines and predict the behavior of antimicrobial lipopeptides, as these molecules can show very different effects due to the abundance of factors to be considered [48]. For example, in the work of Grimsey and colleagues, the same C-terminal lipidation process with a C-12 chain that improved the antimicrobial efficacy of one peptide was detrimental to another [49]. Although our data suggest that the addition of lipid moieties to Bac7(1-16) promotes a lytic mode of action, the role of the proline-rich peptide moiety in lipopeptides remains uncertain. The effect of PrAMP may be limited to the fact that it is a generic cationic peptide moiety that has sufficient length and a good ratio between polar and apolar residues and that, in combination with the proper lipid chain, exerts its antimicrobial action by destabilizing the bacterial envelope, as many other lipopeptides do. This idea can be supported by some similarities between the lipopeptides discussed in this work and other lipopeptides with quite comparable peptide and lipid contents. The MIC values exhibited by lipopeptide (RW)3K-C12 against reference strains of S. aureus, E. coli, P. aeruginosa, and A. baumannii are very similar to those of the lipopeptides synthesized in the current work [50]. The same amino acid sequence bearing the lipidated Lys at the N-terminus also showed similar activity [50]. The synthesized lipopeptide binding a C12 to the N-terminus of the peptide NH2-KRRVRWIIW-CONH2, had a profile of antimicrobial activity and toxicity quite comparable to that of Bac-C12 and Bac-Lp-I. Indeed, lipidation moderately improved the antimicrobial effect of NH2-KRRVRWIIW-CONH2 toward S. aureus, E. faecalis, P. aeruginosa, and S. typhimurium, whereas it slightly worsened activity toward E. coli. On the other hand, the fatty chain made the lipopeptide more cytotoxic than the native molecule [49].
A comparison of pros and cons between Bac-C12 and Bac-Lp-I revealed that Bac-C12 is the most promising compound for future development. Bac-C12 has an interestingly broad spectrum of activity and potent antibiotic activity and displayed only a modest decrease in biocompatibility compared to Bac7(1-16). Moreover, the synthesis of Bac-C12 is simpler than that of Bac-Lp-I. It is performed in a single step and requires the formation of only one amide bond, unlike Bac-Lp-I, which requires the linkage of two more complex compounds. Overall, these properties make it appealing not only on its own but also for possible use in combination with non-lipidated PrAMPs.
In conclusion, this study indicates that lipidation of PrAMPs is a useful strategy to enhance PrAMP activity by deeply modifying the mechanism of action and providing interesting antimicrobial molecules. Therefore, Bac-C12 deserves further studies to explore its potential as a lead compound that can be used in the new generation of antibiotic therapy.
4. Materials and Methods
4.1. Peptides Synthesis
Bac-C12, Bac-Lp-I, and Bac7(1-16) (95% pure) were purchased from NovoPro Bioscience (Shanghai, China). The purity level was verified by RP-HPLC and ESI-MS analyses. Lp-I was purchased from GenScript (Piscataway, NJ, USA) and purified to 90% purity by RP-HPLC [35]. Lipopeptides and Lp-I were dissolved in dimethyl sulfoxide (DMSO) following the manufacturer’s instructions. Any effects of DMSO on bacterial growth were excluded by control assays performed using the same DMSO concentrations present in the peptide dilutions. Bac7(1-16) was resuspended in sterile milliQ water. The chemical structures for Bac-C12 and Bac-Lp-I are shown in Figure 1.
4.2. Bacterial Culture
The bacteria used in this study, which were purchased from American Type Culture Collection (Manassas, Virginia, USA), the German Collection of Microorganisms and Cell Cultures (Leibniz Institute, Braunschweig, Germany), or Keio Collection, Japan [51], were as follows: Bacillus subtilis DSMZ 4181, Enterococcus faecalis ATCC 29212, Staphylococcus aureus ATCC 25923 and 29213, Staphylococcus epidermidis ATCC 12228, Acinetobacter baumannii ATCC 17978 and 19606, Burkholderia cenocepacia J2315, Escherichia coli ATCC 25922, BW25113, BW25113 ΔsbmA [51], and O18K1H7, Klebsiella pneumoniae ATCC 13883 and 700603, Pseudomonas aeruginosa ATCC 27853 and PAO1, Salmonella typhimurium ATCC 14028, and Stenotrophomonas maltophilia ATCC 13637. Overnight cultures of each strain were diluted 1:30 in fresh Mueller–Hinton broth (MHB; Difco) and incubated at 37 °C with shaking (140 rpm) for approximately 2 h (mid-log phase) until an optical density (OD) of ≈ 0.3 at 600 nm was achieved. E. coli BW25113 ΔsbmA was grown in MHB with the addition of 50 μg/mL kanamycin (Sigma, Milan, Italy).
4.3. Evaluation of the Antimicrobial Activity
Minimum inhibitory concentration (MIC) assays were performed as previously reported [24]. Each peptide was separately dispensed in the first wells of a 96-well microtiter plate (Sarstedt, Milan, Italy) and serially diluted twofold in MHB into the subsequent wells. A mid-log phase bacterial suspension (2.5 × 105 CFU/mL) was added in MHB to the microtiter plate wells and the microtiter plates were incubated at 37 °C. The MIC value was taken as the lowest peptide concentration that inhibited visible growth after 18 h. MIC values for B. cepacia and S. maltophilia were determined after 48 h incubation. Data represent the mode of at least three independent experiments.
The minimal bactericidal concentration (MBC) assay was performed after MIC. 10 μL aliquots from the wells without visible bacterial growth were seeded in Mueller–Hinton agar (MH agar; Difco) and incubated for 24 h to allow colony growth. The peptide concentration causing a reduction ≥ 99.9% of the initial inoculum bacteria was defined as MBC value (CLSI M26-A, Methods for Determining Bactericidal Activity of Antimicrobial Agents) as previously described [52]. Data are reported as the mode of at least three independent experiments. The bactericidal activity of the peptides was determined using a bacterial suspension in the mid-log phase of S. aureus ATCC 25923 or E. coli ATCC 25922 cells diluted to 1 × 106 CFU/mL in fresh MHB and incubated at 37 °C with each peptide used at concentrations corresponding to their MIC or sub-MIC values. After 30 min incubation, samples were diluted in phosphate-buffered saline (PBS), plated on MH agar, and incubated overnight to determine colony counts. Data represent the mean ± SD of three independent experiments.
4.4. In Vitro Toxicity Assays
Hemolysis assays were performed using human red blood cells (hRBCs) following the protocol of Laverty [31]. Briefly, hRBCs from human whole blood from a single donor (Cambridge Bioscience, UK) were pelleted, washed three times with equal volumes of PBS by centrifugation (15 min, 900× g), and then suspended at 8% (v/v) in PBS. 100 μL aliquots of the hRBC-PBS suspensions were added to each well of the 96 microtiter plates (Euroclone, Milan, Italy), followed by 100 μL of the lipopeptide in PBS at different concentrations. Samples were incubated at 37 °C for 1 h, then centrifuged at 1000× g (Sigma 4K15C) for 10 min, and 100 μL aliquots of the supernatant were transferred to a new 96-well microtiter plate. Hemoglobin release was measured as absorbance values at 540 nm using a Tecan microplate reader (Tecan Trading AG, Switzerland). 0% and 100% hemolysis were determined using PBS and a 1% solution of Triton X-100, respectively. Results are reported as mean ± SD of two independent experiments performed in triplicate.
Cytotoxicity was evaluated by the tetrazolium salts test (MTT) (Sigma) assay. Human immortalized epidermal keratinocyte HaCaT cells (DKFZ, Eppelheim, Germany) and the human line of lymphocyte precursors MEC-1 (ACC -497; DSMZ, Germany) were grown in high-glucose Dulbecco’s modified Eagle’s medium (DMEM) (Euroclone, Milan, Italy) and RPMI (Sigma, Milan, Italy), respectively. Both media were supplemented with 10% fetal bovine serum (FBS; Sigma, Milan, Italy), 2 mM glutamine (Sigma, Milan, Italy), 100 U/mL penicillin (Sigma, Milan, Italy), and 100 μg/mL streptomycin (Sigma, Milan, Italy). The cells were maintained at 37 °C in the presence of 5% CO2 and in a humidified incubator. The cells were seeded in 96 flat-bottom microtiter plates (Euroclon, Milan, Italy e) at a density of 2 × 104 cells/well. After 24 h, the cells were exposed to different concentrations of peptides in a complete medium and incubated for 24 h. For the last 4 h of incubation, 20 μL MTT solution (1 mg/mL in PBS; Sigma, Milan, Italy) was added to each well. After incubation, the plates were centrifuged (Sigma 4K15C) at 480× g for 10 min, the supernatant of each well was carefully removed, and 120 μL PBS was added to each well. The insoluble MTT crystals were solubilized using 100 μL 10% IGEPAL (Sigma, Milan, Italy) in 0.01N HCl, and the plates were incubated overnight at 37 °C. Absorbance values were measured at 570 nm using the plate reader spectrophotometer Nanoquant infinite M200pro (Tecan, Männedorf, Switzerland). Data are absorbance values expressed as percentages of the untreated controls and are the mean ± SD of three independent experiments with internal triplicates.
4.5. Membrane Integrity Analysis
Bacterial cell membrane integrity assessment was evaluated by measuring propidium iodide (PI) (Sigma, Milan, Italy) uptake using flow cytometry [47]. Briefly, bacterial cultures in the mid-log phase were diluted in MHB to 1 × 106 CFU/mL, and were incubated at 37 °C with MIC and sub-MIC concentrations of the peptide for different time points. PI was added to all samples at a final concentration of 10 μg/mL. At the end of each time point incubation, the bacterial cells were analyzed using a Cytomics FC 500 instrument (Beckman-Coulter, Inc., Fullerton, CA, USA). Data analysis was performed using FCS Express3 software (De Novo Software, Los Angeles, CA, USA). Data are expressed as mean ± SEM.
4.6. Resistance Selection by Serial Passages
Susceptibility to the compounds was assessed daily, by performing a serial passage protocol as previously described [26]. Briefly, MIC values for wild-type E. coli ATCC 25922 were first determined and recorded. Bacterial cells growing in the presence of the highest concentration of the antimicrobial (1/2 MIC) were harvested and inoculated into fresh MHB. These bacteria were grown and subjected to another MIC assay incubating them for 18 h at 37 °C with each of the antimicrobials. After incubation, bacteria grown at 1/2 MIC were again subcultured and used in a new MIC assay. The process was repeated for 14 passages (days). The range of peptide concentrations used for the MIC assay was adjusted and increased according to the rising MIC values (if any). Colistin (Sigma, Milan, Italy) and chloramphenicol (Sigma, Milan, Italy) were used as drug references.
4.7. Statistical Analyses
Significance of differences among groups was assessed using Prism program (GraphPad Software, San Diego, CA, USA) and an analysis of variance between groups (Kruskal–Wallis test or Bonferroni, ANOVA). Values of p ≤ 0.05 were considered statistically significant.
Acknowledgments
We thank Andrea Caporale, researcher at Consiglio Nazionale delle Ricerche, for critical reading and suggestions about the chemical structures.
Abbreviations
| AMPs | Antimicrobial peptides |
| CFU | Colony-forming unit |
| CLSI | Clinical & Laboratory Standards Institute |
| DMEM | Dulbecco’s modified Eagle’s medium |
| DMSO | Dimethyl sulfoxide |
| FBS | Fetal bovine serum |
| hRBCs | Human red blood cells |
| MBC | Minimal bactericidal concentration |
| MEC-1 | Human chronic lymphocytic leukemic B line |
| MHB | Mueller–Hinton broth |
| MIC | Minimum inhibitory concentration |
| MTT | Tetrazolium salts test |
| PBS | Phosphate-buffered saline |
| PI | Propidium iodide |
| PrAMPs | Proline-rich antimicrobial peptides |
| USCLs | Ultrashort cationic lipopeptides |
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/ijms22157959/s1.
Author Contributions
Conceptualization: M.M., M.B., M.S. and A.A.R.; methodology: F.A., M.B. and A.D.S.; validation F.A., M.B., M.M. and A.D.S.; formal analysis and investigation: F.A., M.B., M.M. and A.D.S.; data curation: F.A., M.B. and A.D.S.; writing—original draft; F.A., M.B. and M.S.; writing—review and editing: F.A., M.M., A.D.S., A.A.R., M.B. and M.S.; supervision: M.S.; funding acquisition: M.M. and M.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding. F.A. was supported by the “Made in Trieste” fellowship from the Area Science Park of Trieste, Italy.
Data Availability Statement
Data is contained within the article or Supplementary Materials.
Conflicts of Interest
A.A.R., M.S., and M.B. are co-inventors of Lp-I, the Ultra Short Cationic Lipopeptide used in this study (European patent application No. 17425081.1-1453; title: Short and ultra-short antimicrobial lipopeptides and use thereof). A.A.R. is CEO of Arta Peptidion srls. The study was not funded by the Arta Peptidion Company, and it had no influence on the study design or on the content of this manuscript.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Zaman S.B., Hussain M.A., Nye R., Mehta V., Mamun K.T., Hossain N. A Review on Antibiotic Resistance: Alarm Bells are Ringing. Cureus. 2017;9:e1403. doi: 10.7759/cureus.1403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Miano T.A., Lautenbach E., Wilson F.P., Guo W., Borovskiy Y., Hennessy S. Attributable Risk and Time Course of Colistin-Associated Acute Kidney Injury. Clin. J. Am. Soc. Nephrol. 2018;13:542–550. doi: 10.2215/CJN.06980717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Molchanova N., Hansen P.R., Franzyk H. Advances in Development of Antimicrobial Peptidomimetics as Potential Drugs. Molecules. 2017;22:1430. doi: 10.3390/molecules22091430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bahar A.A., Ren D. Antimicrobial Peptides. Pharmaceuticals. 2013;6:1543–1575. doi: 10.3390/ph6121543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brown K.L., Hancock R.E. Cationic host defense (antimicrobial) peptides. Curr. Opin. Immunol. 2006;18:24–30. doi: 10.1016/j.coi.2005.11.004. [DOI] [PubMed] [Google Scholar]
- 6.Boto A., De La Lastra J.M.P., González C.C. The Road from Host-Defense Peptides to a New Generation of Antimicrobial Drugs. Molecules. 2018;23:311. doi: 10.3390/molecules23020311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mookherjee N., Anderson M.A., Haagsman H.P., Davidson D.J. Antimicrobial host defence peptides: Functions and clinical potential. Nat. Rev. Drug Discov. 2020;19:311–332. doi: 10.1038/s41573-019-0058-8. [DOI] [PubMed] [Google Scholar]
- 8.Shai Y. Mode of Action of Membrane Active Antimicrobial Peptides. Peptide Sci. 2002;66:236–248. doi: 10.1002/bip.10260. [DOI] [PubMed] [Google Scholar]
- 9.Matsuzaki K. Control of cell selectivity of antimicrobial peptides. Biochim. Biophys. Acta Biomembr. 2009;276:6483–6496. doi: 10.1016/j.bbamem.2008.09.013. [DOI] [PubMed] [Google Scholar]
- 10.Nicolas P. Multifunctional Host Defense Peptides: Intracellular-Targeting Antimicrobial Peptides. FEBS J. 2009;276:6483–6496. doi: 10.1111/j.1742-4658.2009.07359.x. [DOI] [PubMed] [Google Scholar]
- 11.Scocchi M., Mardirossian M., Runti G., Benincasa M. Non-Membrane Permeabilizing Modes of Action of Antimicrobial Peptides on Bacteria. Curr. Top. Med. Chem. 2016;16:76–88. doi: 10.2174/1568026615666150703121009. [DOI] [PubMed] [Google Scholar]
- 12.Li W., Tailhades J., O′Brien-Simpson N.M., Separovic F., Otvos L., Hossain M.A., Wade J.D. Proline-rich antimicrobial peptides: Potential therapeutics against antibiotic-resistant bacteria. Amino Acids. 2014;46:2287–2294. doi: 10.1007/s00726-014-1820-1. [DOI] [PubMed] [Google Scholar]
- 13.Otvos J.L. The short proline-rich antibacterial peptide family. Cell. Mol. Life Sci. 2002;59:1138–1150. doi: 10.1007/s00018-002-8493-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Scocchi M., Tossi A., Gennaro R. Proline-rich antimicrobial peptides: Converging to a non-lytic mechanism of action. Cell. Mol. Life Sci. 2011;68:2317–2330. doi: 10.1007/s00018-011-0721-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Berthold N., Hoffmann R. Cellular uptake of apidaecin 1b and related analogs in Gram-negative bacteria reveals novel antibacterial mechanism for proline-rich antimicrobial peptides. Protein Pept. Lett. 2014;21:391–398. doi: 10.2174/09298665113206660104. [DOI] [PubMed] [Google Scholar]
- 16.Krizsan A., Knappe D., Hoffmann R. Influence of theyjiL-mdtMGene Cluster on the Antibacterial Activity of Proline-Rich Antimicrobial Peptides Overcoming Escherichia coli Resistance Induced by the Missing SbmA Transporter System. Antimicrob. Agents Chemother. 2015;59:5992–5998. doi: 10.1128/AAC.01307-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mattiuzzo M., Bandiera A., Gennaro R., Benincasa M., Pacor S., Antcheva N., Scocchi M. Role of the Escherichia coli SbmA in the antimicrobial activity of proline-rich peptides. Mol. Microbiol. 2007;66:151–163. doi: 10.1111/j.1365-2958.2007.05903.x. [DOI] [PubMed] [Google Scholar]
- 18.Graf M., Mardirossian M., Nguyen F., Seefeldt A.C., Guichard G., Scocchi M., Innis C.A., Wilson D.N. Proline-rich antimicrobial peptides targeting protein synthesis. Nat. Prod. Rep. 2017;34:702–711. doi: 10.1039/C7NP00020K. [DOI] [PubMed] [Google Scholar]
- 19.Mardirossian M., Grzela R., Giglione C., Meinnel T., Gennaro R., Mergaert P., Scocchi M. The Host Antimicrobial Peptide Bac71-35 Binds to Bacterial Ribosomal Proteins and Inhibits Protein Synthesis. Chem. Biol. 2014;21:1639–1647. doi: 10.1016/j.chembiol.2014.10.009. [DOI] [PubMed] [Google Scholar]
- 20.Roy R.N., Lomakin I.B., Gagnon M.G., Steitz T.A. The Mechanism of Inhibition of Protein Synthesis by the Proline-Rich Peptide Oncocin. Nat. Struct. Mol. Biol. 2015;22:466–469. doi: 10.1038/nsmb.3031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Seefeldt A.C., Nguyen F., Antunes S., Pérébaskine N., Graf M., Arenz S., Inampudi K.K., Douat C., Guichard G., Wilson D.N., et al. The proline-rich antimicrobial peptide Onc112 inhibits translation by blocking and destabilizing the initiation complex. Nat. Struct. Mol. Biol. 2015;22:470–475. doi: 10.1038/nsmb.3034. [DOI] [PubMed] [Google Scholar]
- 22.Seefeldt A.C., Graf M., Pérébaskine N., Nguyen F., Arenz S., Mardirossian M., Scocchi M., Wilson D.N., Innis C.A. Structure of the mammalian antimicrobial peptide Bac7(1–16) bound within the exit tunnel of a bacterial ribosome. Nucleic Acids Res. 2016;44:2429–2438. doi: 10.1093/nar/gkv1545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zahn M., Berthold N., Kieslich B., Knappe D., Hoffmann R., Sträter N. Structural Studies on the Forward and Reverse Binding Modes of Peptides to the Chaperone DnaK. J. Mol. Biol. 2013;425:2463–2479. doi: 10.1016/j.jmb.2013.03.041. [DOI] [PubMed] [Google Scholar]
- 24.Benincasa M., Scocchi M., Podda E., Skerlavaj B., Dolzani L., Gennaro R. Antimicrobial Activity of Bac7 Fragments against Drug-Resistant Clinical Isolates. Peptides. 2004;25:2055–2061. doi: 10.1016/j.peptides.2004.08.004. [DOI] [PubMed] [Google Scholar]
- 25.Benincasa M., Pelillo C., Zorzet S., Garrovo C., Biffi S., Gennaro R., Scocchi M. The Proline-Rich Peptide Bac7(1-35) Reduces Mortality from Salmonella Typhimurium in a Mouse Model of Infection. BMC Microbiol. 2010;10:178. doi: 10.1186/1471-2180-10-178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dolzani L., Milan A., Scocchi M., Lagatolla C., Bressan R., Benincasa M. Sub-MIC effects of a proline-rich antibacterial peptide on clinical isolates of Acinetobacter baumannii. J. Med. Microbiol. 2019;68:1253–1265. doi: 10.1099/jmm.0.001028. [DOI] [PubMed] [Google Scholar]
- 27.Mardirossian M., Sola R., Beckert B., Valencic E., Collis D.W.P., Borišek J., Armas F., Di Stasi A., Buchmann J., Syroegin E.A., et al. Peptide Inhibitors of Bacterial Protein Synthesis with Broad Spectrum and SbmA-Independent Bactericidal Activity against Clinical Pathogens. J. Med. Chem. 2020;63:9590–9602. doi: 10.1021/acs.jmedchem.0c00665. [DOI] [PubMed] [Google Scholar]
- 28.Melander R.J., Zurawski D.V., Melander C. Narrow-spectrum antibacterial agents. MedChemComm. 2018;9:12–21. doi: 10.1039/C7MD00528H. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kollef M.H. Broad-Spectrum Antimicrobials and the Treatment of Serious Bacterial Infections: Getting It Right Up Front. Clin. Infect. Dis. 2008;47:S3–S13. doi: 10.1086/590061. [DOI] [PubMed] [Google Scholar]
- 30.Ting D.S.J., Beuerman R.W., Dua H.S., Lakshminarayanan R., Mohammed I. Strategies in Translating the Therapeutic Potentials of Host Defense Peptides. Front. Immunol. 2020;11:983. doi: 10.3389/fimmu.2020.00983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Laverty G., McLaughlin M., Shaw C., Gorman S.P., Gilmore B.F. Antimicrobial Activity of Short, Synthetic Cationic Lipopeptides. Chem. Biol. Drug Des. 2010;75:563–569. doi: 10.1111/j.1747-0285.2010.00973.x. [DOI] [PubMed] [Google Scholar]
- 32.Chu-Kung A.F., Bozzelli K.N., Lockwood N.A., Haseman J.R., Mayo K.H., Tirrell M.V. Promotion of Peptide Antimicrobial Activity by Fatty Acid Conjugation. Bioconjugate Chem. 2004;15:530–535. doi: 10.1021/bc0341573. [DOI] [PubMed] [Google Scholar]
- 33.Li W., Separovic F., O′Brien-Simpson N.M., Wade J.D. Chemically modified and conjugated antimicrobial peptides against superbugs. Chem. Soc. Rev. 2021;50:4932–4973. doi: 10.1039/D0CS01026J. [DOI] [PubMed] [Google Scholar]
- 34.Serrano G.N., Zhanel G.G., Schweizer F. Antibacterial Activity of Ultrashort Cationic Lipo-β-Peptides. Antimicrob. Agents Chemother. 2009;53:2215–2217. doi: 10.1128/AAC.01100-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Armas F., Pacor S., Ferrari E., Guida F., Pertinhez T.A., Romani A.A., Scocchi M., Benincasa M. Design, Antimicrobial Activity and Mechanism of Action of Arg-Rich Ultra-Short Cationic Lipopeptides. PLoS ONE. 2019;14:e0212447. doi: 10.1371/journal.pone.0212447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Domalaon R., Sanchak Y., Koskei L.C., Lyu Y., Zhanel G.G., Arthur G., Schweizer F. Short Proline-Rich Lipopeptide Potentiates Minocycline and Rifampin against Multidrug- and Extensively Drug-Resistant Pseudomonas aeruginosa. Antimicrob. Agents Chemother. 2018;62 doi: 10.1128/AAC.02374-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hong H.A., Huang J.-M., Khaneja R., Hiep L.V., Urdaci M.C., Cutting S.M. The safety ofBacillus subtilisandBacillus indicusas food probiotics. J. Appl. Microbiol. 2008;105:510–520. doi: 10.1111/j.1365-2672.2008.03773.x. [DOI] [PubMed] [Google Scholar]
- 38.Bluhm M.E., Knappe D., Hoffmann R. Structure-activity relationship study using peptide arrays to optimize Api137 for an increased antimicrobial activity against Pseudomonas aeruginosa. Eur. J. Med. Chem. 2015;103:574–582. doi: 10.1016/j.ejmech.2015.09.022. [DOI] [PubMed] [Google Scholar]
- 39.Knappe D., Adermann K., Hoffmann R. Oncocin Onc72 is efficacious against antibiotic-susceptible Klebsiella pneumoniaeATCC 43816 in a murine thigh infection model. Peptide Sci. 2015;104:707–711. doi: 10.1002/bip.22668. [DOI] [PubMed] [Google Scholar]
- 40.Kopeikin P.M., Zharkova M.S., Kolobov A.A., Smirnova M.P., Sukhareva M.S., Umnyakova E.S., Kokryakov V.N., Orlov D.S., Milman B.L., Balandin S.V., et al. Caprine Bactenecins as Promising Tools for Developing New Antimicrobial and Antitumor Drugs. Front. Cell. Infect. Microbiol. 2020;10:552905. doi: 10.3389/fcimb.2020.552905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mardirossian M., Sola R., Beckert B., Collis D.W.P., Di Stasi A., Armas F., Hilpert K., Wilson D.N., Scocchi M. Proline-Rich Peptides with Improved Antimicrobial Activity against E. coli, K. pneumoniae, and A. baumannii. ChemMedChem. 2019;14:2025–2033. doi: 10.1002/cmdc.201900465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Pendleton J.N., Gorman S.P., Gilmore B.F. Clinical relevance of the ESKAPE pathogens. Expert Rev. Anti-Infect. Ther. 2013;11:297–308. doi: 10.1586/eri.13.12. [DOI] [PubMed] [Google Scholar]
- 43.Pränting M., Negrea A., Rhen M., Andersson D.I. Mechanism and Fitness Costs of PR-39 Resistance in Salmonella enterica Serovar Typhimurium LT2. Antimicrob. Agents Chemother. 2008;52:2734–2741. doi: 10.1128/AAC.00205-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gagnon M.G., Roy R.N., Lomakin I.B., Florin T., Mankin A.S., Steitz T.A. Structures of proline-rich peptides bound to the ribosome reveal a common mechanism of protein synthesis inhibition. Nucleic Acids Res. 2016;44:2439–2450. doi: 10.1093/nar/gkw018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Mardirossian M., Barrière Q., Timchenko T., Müller C., Pacor S., Mergaert P., Scocchi M., Wilsona D.N. Fragments of the Nonlytic Proline-Rich Antimicrobial Peptide Bac5 Kill Escherichia coli Cells by Inhibiting Protein Synthesis. Antimicrob. Agents Chemother. 2018;62 doi: 10.1128/AAC.00534-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Andersson D.I., Hughes D., Kubicek-Sutherland J.Z. Mechanisms and consequences of bacterial resistance to antimicrobial peptides. Drug Resist. Updat. 2016;26:43–57. doi: 10.1016/j.drup.2016.04.002. [DOI] [PubMed] [Google Scholar]
- 47.Podda E., Benincasa M., Pacor S., Micali F., Mattiuzzo M., Gennaro R., Scocchi M. Dual Mode of Action of Bac7, a Proline-Rich Antibacterial Peptide. Biochim. Biophys. Acta Gen. Subj. 2006;1760:1732–1740. doi: 10.1016/j.bbagen.2006.09.006. [DOI] [PubMed] [Google Scholar]
- 48.Rounds T., Straus S.K. Lipidation of Antimicrobial Peptides as a Design Strategy for Future Alternatives to Antibiotics. Int. J. Mol. Sci. 2020;21:9692. doi: 10.3390/ijms21249692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Grimsey E., Collis D.W., Mikut R., Hilpert K. The effect of lipidation and glycosylation on short cationic antimicrobial peptides. Biochim. Biophys. Acta Biomembr. 2020;1862:183195. doi: 10.1016/j.bbamem.2020.183195. [DOI] [PubMed] [Google Scholar]
- 50.Albada H.B., Prochnow P., Bobersky S., Langklotz S., Schriek P., Bandow J.E., Metzler-Nolte N. Tuning the Activity of a Short Arg-Trp Antimicrobial Peptide by Lipidation of a C- or N-Terminal Lysine Side-Chain. ACS Med. Chem. Lett. 2012;3:980–984. doi: 10.1021/ml300148v. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Baba T., Ara T., Hasegawa M., Takai Y., Okumura Y., Baba M., Datsenko K.A., Tomita M., Wanner B.L., Mori H. Construction of Escherichia coli K-12 in-frame, single-gene knockout mutants: The Keio collection. Mol. Syst. Biol. 2006;2:2006–2008. doi: 10.1038/msb4100050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Mardirossian M., Pompilio A., Degasperi M., Runti G., Pacor S., Di Bonaventura G., Scocchi M. D-BMAP18 Antimicrobial Peptide Is Active In vitro, Resists to Pulmonary Proteases but Loses Its Activity in a Murine Model of Pseudomonas aeruginosa Lung Infection. Front. Chem. 2017;5:40. doi: 10.3389/fchem.2017.00040. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data is contained within the article or Supplementary Materials.