Abstract
Introduction and importance
Adrenal Leiomyomas are infrequent tumors with only a few cases reported to date. They are difficult to differentiate from malignant adrenal tumors due to non-specific findings on clinical examination and imaging studies.
Case presentation
We discuss the case of a 49-year old male who had been experiencing generalized abdominal pain for 14 months and was found to have a mass on ultrasonography. Further evaluation with Contrast-enhanced Computerized Tomography (CECT) revealed an uneven soft tissue density mass in the retroperitoneal region of the left side. The histopathological examination of the excised mass was suggestive of a mesenchymal tumor, which was further confirmed as leiomyoma by immunohistochemistry.
Clinical discussion
Adrenal Leiomyomas are rare smooth muscle tumors that present with heterogeneously enhancing mass on radiologic imaging. On histopathological examination, spindle cells arranged in lobules and fascicles can be appreciated. Positive staining for desmin and smooth muscle actin in immunohistochemistry confirms the diagnosis.
Conclusion
Identification of the type of tumor in any adrenal mass is challenging pertaining to the non-specific findings on imaging studies. So, prompt surgical resection is the mainstay of the treatment.
Keywords: Adrenal gland, Leiomyoma, Mesenchymal, Retroperitoneum
Highlights
-
•
Adrenal leiomyomas are rare tumors.
-
•
These tumors are usually identified incidentally on USG and CT scans of the abdomen & pelvis.
-
•
Histopathological and immunohistochemical studies of the resected tumor mass aid in reaching a definitive diagnosis.
1. Introduction
Leiomyomas are benign mesenchymal tumors originating from smooth muscles. Adrenal Leiomyomas are uncommon tumors with a median age of involvement at 34.5 years and a female preponderance. Immunodeficient states, such as HIV-AIDS, are one of the most common risk factors for this tumor [1]. These tumors are difficult to distinguish from malignant adrenal tumors due to non-specific findings on clinical examination and imaging studies. These tumors are usually identified as incidentalomas during ultrasonography (USG) and computerized tomography (CT) scans of the abdomen and pelvis [2]. A definitive diagnosis of such incidentalomas is made by histopathological examination and immunohistochemical studies of the specimen [3].
Here, we present a case of an incidental finding of left adrenal leiomyoma in a 49-year male who presented with abdominal pain and non-specific symptoms like loss of appetite, and weight loss. This work has been reported in line with the SCARE criteria [4].
2. Case presentation
A 49-year male presented in the outpatient department with the complaint of insidious onset generalized abdominal pain for fourteen months. The pain was continuous, unrelieved by analgesics, and was associated with few episodes of nausea and vomiting. He had a loss of appetite and had lost 12 kg of body weight over the past 14 months. He denied having burning micturition during this period. He is on medication for Hypertension and Type-2 Diabetes Mellitus for 8 years. He is a non-smoker and doesn't consume alcohol or any recreational drugs. Moreover, there was no similar illness in his parents and siblings.
On examination, he was afebrile and his vitals were stable along with normal blood pressure of 138/84 mmHg. The abdomen was soft and non-tender, with no renal angle pain or any palpable mass. Examination of other systems was grossly intact. Table 1 shows the results of laboratory tests of blood parameters. And a urine routine examination showed 10–14 RBCs (Red Blood Cells) per high power field.
Table 1.
Laboratory values of blood investigations.
| S.N. | Blood parameters | Obtained value | Reference range |
|---|---|---|---|
| 1. | Hemoglobin(Hb) | 11.5 g/dl | 14–18 g/dl |
| 2. | Total Leukocyte Count(TLC) | 5900/μl | 4000–1100/μl |
| 3 | Platelet count | 204,000/μl | 150,000–300,000/μl |
| 4. | Urea | 6.9 mmol/l | 1.8–7.1 mMol/l |
| 5. | Creatinine | 188 μmol/l | 60–130 μmol/l |
| 6. | Sodium | 135 mEq/l | 135–145 mEq/l |
| 7. | Potassium | 4.1 mEq/l | 3.5–5.2 mEq/l |
| 8. | Prothrombin time(PT) | 12.6 s | 10–13 s |
| 9. | International normalized ratio(INR) | 0.93 | 0.9–1.15 |
| 10. | Random Blood Sugar(RBS) | 5 mMol/l | 3.8–7.8 mMol/l |
| 11. | Alanine transferase(ALT) | 14 U/l | 5–45 U/l |
| 12. | Aspartate Aminotransferase(AST) | 13 U/l | 5–40 U/l |
| 13. | Alkaline Phosphatase(ALP) | 71 U/l | <306 U/l |
| 14. | Total bilirubin(TB) | 22 g/l | 3–21 g/l |
| 15. | Direct Bilirubin (DB) | 6 g/l | 0–5 g/l |
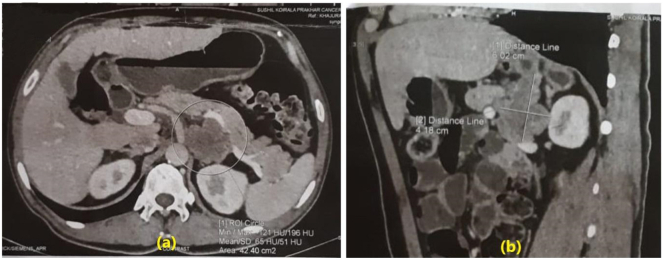
He underwent USG of the abdomen and pelvis to determine the cause of his abdominal pain, which revealed a heterogeneous mass with suspected necrotic changes above the left kidney. For further characterization of mass, CECT of the abdomen and pelvis was done which showed an irregular soft tissue density mass in the retroperitoneal region of the left side measuring approximately 6 cm × 4 cm infiltrating the posterior aspect of the body of the stomach, medial aspect of the adrenal gland, right crus of the diaphragm and splenic artery and renal vein. Also, the mass was abutting the pancreas and abdominal aorta with a loss of the fat plane. Post-contrast study shows heterogeneous enhancement with central poorly enhancing areas, likely necrotic changes (Fig. 1). With suspicion of pheochromocytoma, the patient's 24-hr urine examination was done which revealed Vanillylmandelic acid (VMA) level of 24.27 (normal range < 13.6 mg/24 h) and Metanephrine level of 83.04 (normal range = 73–808 μg/24 h).
Fig. 1.
(a): Transverse section CECT of abdomen & pelvis showing an adrenal mass in the left retroperitoneum.
(b): Sagittal section CECT of abdomen & pelvis showing left-sided adrenal mass.
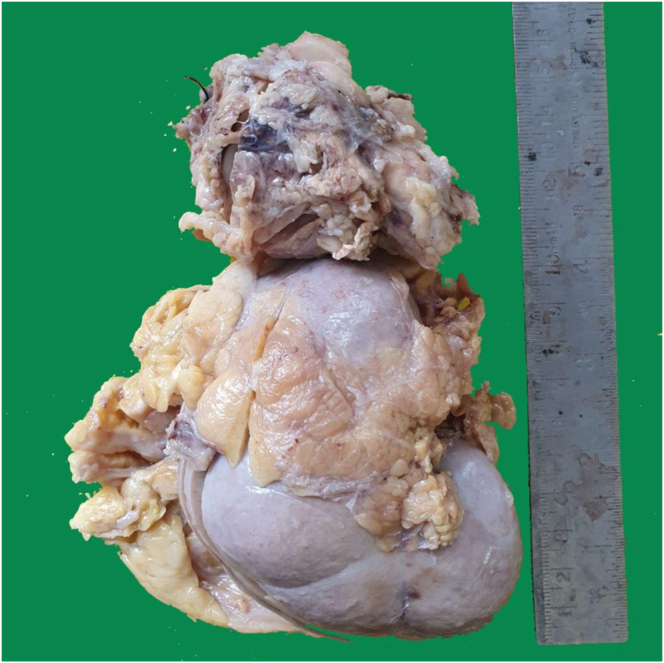
Thus, with a preoperative diagnosis of left adrenal mass, laparoscopic left adrenalectomy along with resection of mass from the invading renal vein was planned. During the surgery, resection of the invading mass from the renal vein caused excessive bleeding rendering the patient hemodynamically unstable. The renal vein was irreparably damaged and bleeding was uncontrollable. Thus, the vascular supply to the left adrenal gland and left kidney was ligated and the adrenal and kidney were mobilized from the surrounding area and removed. The tumor was a large lobulated, well-defined mass encasing the left renal vein and surrounded by a desmoplastic reaction. Thus resected specimen was sent for histopathological examination (Fig. 2).
Fig. 2.
Gross specimen of the left kidney and adrenal gland showing enlarged adrenal gland.
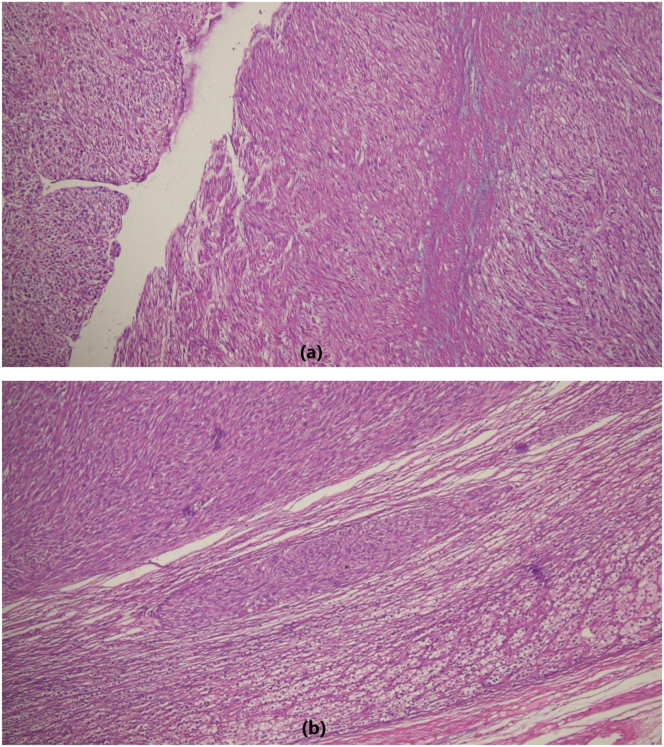
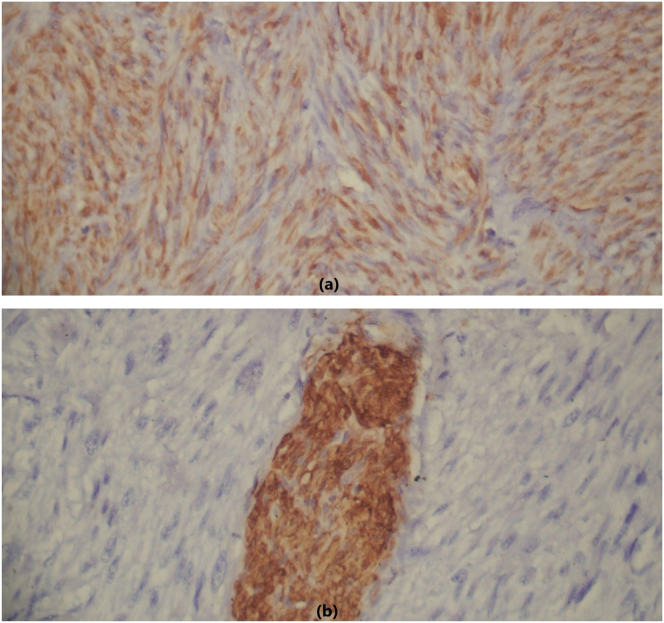
The gross specimen was sent for histopathological investigation as two specimens. The first specimen was a left kidney with perinephric fat with an intact capsule measuring 11.5 cm × 9 cm × 5 cm. The cut section showed grey-brown renal parenchyma with well-maintained cortico-medullary differentiation. The second specimen was a globular left adrenal gland measuring 8 cm × 6 cm 3.5 cm with a rough and irregular surface which showed encapsulated grey-white solid homogeneous areas without hemorrhage and necrosis. Contrary to the presumptive post-operative diagnosis, histological examination of the adrenal specimen showed circumscribed mass composed of spindle cells arranged in fascicles and bundles with oval cigar-shaped nuclei, vesicular chromatin, and inconspicuous nucleoli. Occasional mitotic figures are also seen (Fig. 3). Microscopic examination of the renal specimen showed unremarkable kidney tissues with preserved architecture. The renal vein stump resection margin was free of tumor. Confirmation of the adrenal leiomyoma is done with immunohistochemistry which showed moderately strong cytoplasmic desmin and SMA (Smooth Muscle Actin) positivity whereas S-100 is negative in the tumor cells (Fig. 4).
Fig. 3.
Fascicles and bundles of tumor cells showing cigar-shaped nuclei H&E X40 (a), well-circumscribed tumor cells with native adrenal cortical cells H&E X100 (b).
Fig. 4.
These tumor cells show moderate-intensity cytoplasmic positivity for SMA (a) and S-100 negativity [Note the S100 positive nerve bundle which acts as an internal control] (b).
The postoperative period was uneventful and the patient recovered well. His vitals were stable at the time of discharge. All appropriate laboratory parameters had normalized before discharge. The patient is on regular follow-up, doing well, and is satisfied with the treatment.
3. Clinical discussion
Leiomyoma is a benign tumor that usually arises in organs where smooth muscle cells are abundant [5]. The uterus and gastrointestinal tract have been the most reported sites [6], [7], [8]. Adrenal leiomyoma is a rare solid tumor that develops from the smooth muscle of the adrenal vein and its tributaries [6], [9]. Due to the increased precision of imaging modalities (USG and CT scans) the detection of adrenal masses has risen [8].
Adrenal masses usually present as flank pain, with or without radiation, palpable flank mass, and hematuria [2]. Our patients presented with generalized abdominal pain for 14 months which was continuous and was not relieved by analgesics.
Pheochromocytoma, Cortical Carcinoma, Adrenal leiomyoma present with heterogeneously enhancing masses on different imaging modalities but cannot be differentiated solely based on imaging [10], [11]. Generally, Adrenal leiomyoma does not exhibit metabolic activity [5]. In our case, there was an increase in the level of VMA i.e. 24.37 mg with a normal value of metanephrine on a 24-hr urine examination so keeping pheochromocytoma as a differential, the biopsy was sent for histopathological and immunohistochemical studies to confirm the nature of the tumor.
On gross pathologic examination, adrenal leiomyoma presents as a firm, well-circumscribed tan mass with central hyalinization and the histology reveals spindle cells with a bland appearance against a background of hyalinization and fibrosis [6]. Similarly in our case, the cut section showed encapsulated grey-white solid homogeneous firm areas with whorling patterns. Histopathological examination showed a well-circumscribed mass composed of spindle cells arranged in fascicles and bundles with oval to cigar-shaped nuclei, vesicular chromatin, and inconspicuous nucleoli which were suggestive of mesenchymal tumor of the adrenal gland.
Immunohistochemically, leiomyoma has positive desmin and SMA with negative S-100 which plays a vital role in confirmation [12]. Our case also had similar findings on immunohistochemistry which helped to make a final diagnosis of Adrenal leiomyoma.
Complete surgical excision is the gold standard for the treatment of adrenal leiomyoma [5], [13]. Indications for surgical resection of adrenal masses include patients presenting with symptoms of biochemically functioning tumors and/or masses greater than 6 cm in diameter and mass less than 4 cm and/or non-functioning masses require follow-up postoperatively [2]. The surgical resection can be carried out through laparoscopic, hand-assisted laparoscopic, and open transabdominal techniques [12], [13], [14]. In our case, the removal of invasive tumor mass in the renal vein caused irreparable damage to its leading to uncontrollable bleeding and hemodynamic instability. So, laparoscopic left adrenalectomy with left nephrectomy was done. The tumor was resected with a negative tumor margin so the prognosis is good.
4. Conclusion
Adrenal leiomyomas are extremely rare tumors that are discovered as incidental findings. Imaging studies are non-specific and identification of the type of tumor is often challenging. So, prompt surgical resection of the mass along with the histopathological examination and immunohistochemical studies should be done as a part of both therapeutic and diagnostic purposes.
Ethical approval
Not required.
Funding
None
CRediT authorship contribution statement
Sansar Babu Tiwari (SBT), Surya Prakash Joshi (SPJ), Suraj Shrestha(SS)= Study concept, Data collection, and surgical therapy for the patient
Sujan Sharma (SS), Sujan Timilsina (ST), Surya Prakash Joshi (SPJ), Anil Bist(AB) = Writing- original draft preparation
Sujan Timilsina (ST), Sujan Sharma (SS), Suraj Shrestha(SS) = Editing and writing
Sansar Babu Tiwari (SBT)= Senior author and manuscript reviewer
All the authors read and approved the final manuscript.
Guarantor
Sujan Sharma accepts full responsibility for the work and/or the conduct of the study, has access to the data, and controls the decision to publish.
Registration of research studies
Not applicable
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Declaration of competing interest
None
Acknowledgment
None.
Contributor Information
Sujan Sharma, Email: sharmasujan@iom.edu.np.
Sujan Timilsina, Email: sujan.s10@iom.edu.np.
Surya Prakash Joshi, Email: surya.joshi091@iom.edu.np.
References
- 1.Sakellariou M., Dellaportas D., Peppa M., Schizas D., Pikoulis E., Nastos K. Review of the literature on leiomyoma and leiomyosarcoma of the adrenal gland: a systematic analysis of case reports. In Vivo. 2020;34(5):2233–2248. doi: 10.21873/invivo.12034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pramod S.V., Siregar S., Safriadi F., Hernowo B.S., Firdaus G.I. The largest adrenal leiomyoma: a case report and literature review. Urol Case Rep. 2020;29 doi: 10.1016/j.eucr.2019.101106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Corti M., De Carolis L., Campitelli A., Haab G.A., Veliz L.O. Adrenal leiomyoma: a rare tumor presented as an incidentaloma in a patient with AIDS. Mathews J. HIV/AIDS. 2016;(2):1–4. https://www.mathewsopenaccess.com/scholarly-articles/adrenal-leiomyoma-a-rare-tumor-presented-as-an-incidentaloma-in-a-patient-with-aids.pdf Available from: [Google Scholar]
- 4.SCARE Group. Agha R.A., Franchi T., Sohrabi C., Mathew G., Kerwan A. The SCARE 2020 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 5.Parelkar S.V., Sampat N.P., Sanghvi B.V. Case report of bilateral adrenal leiomyoma with review of literature. Pediatr. Surg. Int. 2013;29(6):655–658. doi: 10.1007/s00383-013-3264-1. [DOI] [PubMed] [Google Scholar]
- 6.Lin J., Wasco M.J., Korobkin M., Doherty G., Giordano T.J. Leiomyoma of the adrenal gland presenting as a non-functioning adrenal incidentaloma: case report and review of the literature. Endocr. Pathol. 2007;18(4):239–243. doi: 10.1007/s12022-008-9013-7. [DOI] [PubMed] [Google Scholar]
- 7.Nishida S., Tanimura A., Takasaki S. Surgically resected adrenal leiomyoma: report of a case. Surg. Today. 1995;25(5):455–457. doi: 10.1007/BF00311827. [DOI] [PubMed] [Google Scholar]
- 8.Alteer M., Ascott-Evans B.H., Conradie M. Leiomyoma: a rare cause of adrenal incidentaloma. J. Endocrinol. Metab. Diabetes S. Afr. 2013;18(1):71–74. doi: 10.1080/22201009.2013.10872308. [DOI] [Google Scholar]
- 9.Armed forces Institute of Pathology (U.S.) Lack E.E. Tumors of the Adrenal Gland and Extra-adrenal Paraganglia. Amer Registry of Pathology; 1997. Universities associated for research and education in pathology. 468p. [Google Scholar]
- 10.Meher D., Dutta D., Giri R., Kar M. Adrenal leiomyoma mimicking adrenal malignancy: diagnostic challenges and review of literature. J. Endocrinol. Metab. 2015;5(5):304–308. doi: 10.14740/jem318w. [DOI] [Google Scholar]
- 11.Albano D., Agnello F., Midiri F. Imaging features of adrenal masses. Insights Imaging. 2019;10(1):1. doi: 10.1186/s13244-019-0688-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gibbs K.E., White A., Kaleya R. Laparoscopic management of an adrenal leiomyoma in an AIDS patient. A case report and review of the literature. JSLS. 2005;9(3):345–348. https://www.ncbi.nlm.nih.gov/pubmed/16121885 [PMC free article] [PubMed] [Google Scholar]
- 13.Khor A.C.-M., Rajaratnam N. Bilateral adrenal leiomyoma: a rare tumor with unusual presentation. J. Endocrinol. Metab. 2020;10(3–4):106–109. doi: 10.14740/jem655. [DOI] [Google Scholar]
- 14.Chang T.-H., Lee Y.-C., Liu C.-C., Huang C.-H., Wu W.-J. Adrenal leiomyoma treated by hand-assisted laparoscopic adrenalectomy: a case report. Kaohsiung J. Med. Sci. 2006;22(11):575–579. doi: 10.1016/S1607-551X(09)70355-9. [DOI] [PMC free article] [PubMed] [Google Scholar]