Abstract
Pneumothorax is the presence of air in the pleural space that can result in the partial or complete collapse of a lung. Cigarette and cannabis smoking are also well-known risk factors. Vaping, on the other hand, is not as well-established as little is known about the impact electronic cigarettes have on the development of pneumothoraces despite their use rapidly increasing over the past decade. While the long-term adverse health effects of vaping are still unknown, the acute adverse events of vaping that have occurred are concerning. Pneumothoraces due to electronic cigarettes have been rarely reported so far but the body of literature illustrating an association is growing. We hope to contribute to it by presenting a case of a 19-year-old male who presented with an e-cigarette induced pneumothorax. It is our hope that this case brings more evidence to the dangers of e-cigarette use.
Keywords: Vaping, e-cigarette, Pneumothorax
Introduction
E-cigarette or vaping associated lung injury (EVALI) is an inflammatory response in the lungs triggered by using a device typically called e-cigarettes or vape pens to inhale a vapor created from heating up a liquid containing various substances, such as nicotine, cannabinoids, artificial flavors, and other additives. According to the Centers of Disease Control (CDC), a total of 2807 hospitalized EVALI cases or deaths have been reported as of February 18, 2020. Among these patients, the majority have been male with a median age of 24 years and no documented underlying lung disease [1,2]. While the long-term adverse health effects of vaping are still unknown, the acute events (e.g., pneumonitis, acute respiratory distress syndrome) that have occurred are of great concern [3]. Intriguingly, pneumothoraces due to vaping have been rarely reported so far but the body of literature illustrating an association is growing. We hope to contribute to it by presenting a case of a 19-year-old male without any prior history of pulmonary disease who presented with an e-cigarette induced pneumothorax.
Case presentation
Patient is a 19-year-old male with no significant medical history who presented to the hospital secondary to shortness of breath and significant left-sided chest discomfort that began less than 24 hours ago. He reported vaping for a few minutes and then subsequently experiencing left-sided chest pressure and discomfort without radiation that he rated 9 out of 10 in severity. He stated that the pain was sharp in nature and worsened with deep inspiration and certain movements. He denied any personal or family history of heart disease, lung disease, or hypercoagulability. He denied recent travel, trauma, or immobilization. He had never experienced this type of pain before. Upon further inquiry about his e-cigarette use, he stated that he had been using his JUUL e-cigarette, which uses a nicotine formula, “every minute of every day” for one year. Previously, he smoked 10 cigarettes daily for one year before switching to the JUUL e-cigarette to help him quit smoking cigarettes. Despite switching to JUUL, he did continue to smoke 1–2 cigarettes monthly as well as 2-3 marijuana joints weekly.
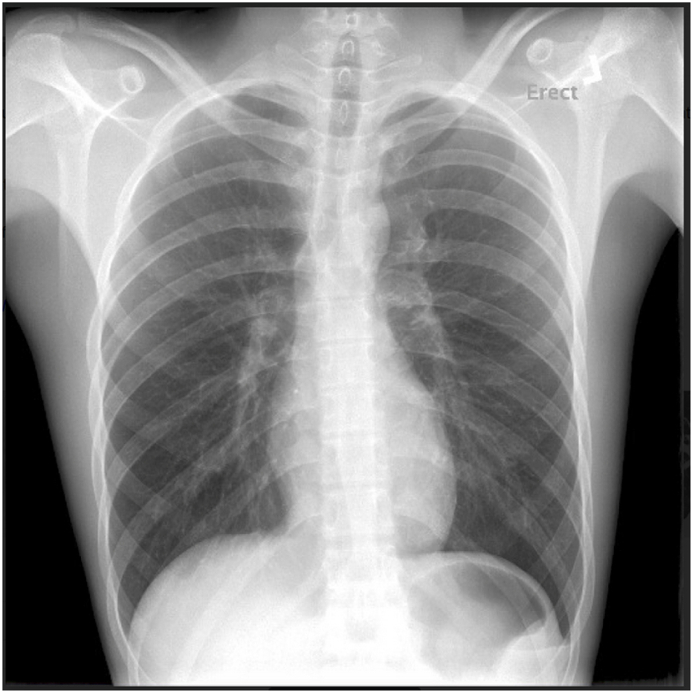
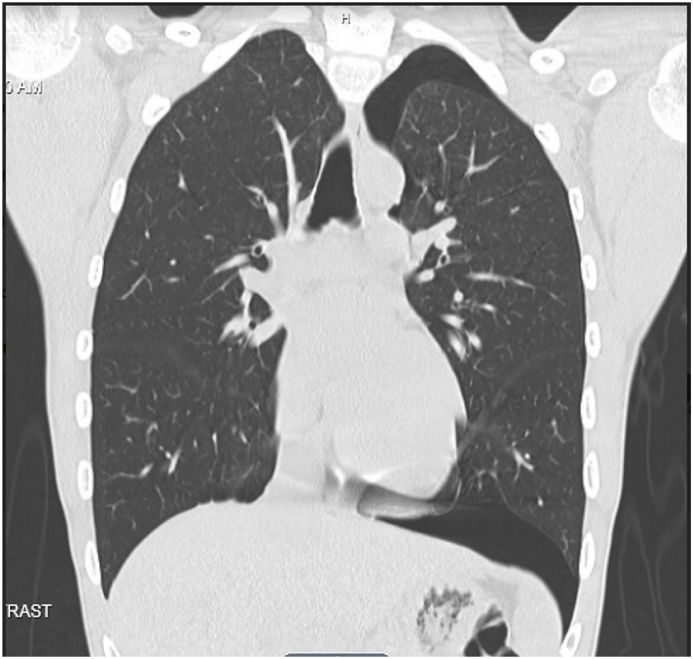
In the Emergency Department, physical examination revealed a 5′8,” 61-kg male who was in no acute respiratory distress. He was noted to be breathing comfortably, and his lungs were clear to auscultation with no rhonchi, rales, or wheezes. No crepitus was palpated in the thoracic region to indicate subcutaneous emphysema. Chest X-Ray demonstrated a small left-sided apical pneumothorax, around 10% (Image 1). He was subsequently placed on 2 L Oxygen (O2) via nasal cannula and admitted to the Observation Unit for monitoring. Computerized tomography (CT) Chest Without Contrast was done to rule out any intraparenchymal lung disease, which only confirmed the small left pneumothorax and otherwise demonstrated clear lung parenchyma (e.g., no subpleural blebs) (Image 2). No further work-up was performed. Patient was managed conservatively for two days, weaned off O2 supplementation, and then discharged after repeated chest x-ray showed no worsening if not minimal improvement in the pneumothorax.
Image 1.
A small left apical pneumothorax 2 cm at the apex (10%). No associated midline shift of the mediastinum. The cardiomediastinal contours, pulmonary vasculature, lungs and pleural spaces are otherwise within normal limits.
Image 2.
Small left pneumothorax of approximately 10%, as reported in the prior chest x-ray. The lungs appear clear.
Discussion
Pneumothorax is the presence of air in the pleural space that can result in the partial or complete collapse of a lung. Pneumothorax can be traumatic (iatrogenic vs non-iatrogenic) or spontaneous. Spontaneous pneumothoraces are classified as either primary or secondary. Primary spontaneous pneumothoraces occur in the absence of lung disease, while secondary spontaneous pneumothorax occur in the presence of lung disease such as asthma, emphysema, chronic obstructive pulmonary disease, cystic fibrosis, malignancy, necrotizing lung infections, and architectural abnormalities of the pleural membrane. Spontaneous pneumothorax classically occur in tall, thin males between the ages of 10 and 30 years, and both cigarette and cannabis smoking are well-known risk factors [4]. Vaping, on the other hand, is not as well-established as little is known about the impact e-cigarettes have on the development of pneumothoraces despite their use rapidly increasing over the past decade, particularly among adolescents and young adults.
E-cigarettes have generally been advertised to be less damaging to the lung parenchyma than traditional cigarette smoking. However, as vaping rates continue to rise, numerous cases are illustrating that this may be further and further from the truth since associated EVALI is parallelly increasing [[5], [6], [7]]. E-cigarettes may increase the risk of pneumothorax through the action of both the physiologic mechanisms and inhaled toxins. Pneumothoraces are thought to result from the spontaneous rupture of subpleural blebs or bullae or increase in pleural porosity secondary to inflammation. Pneumothoraces from e-cigarette use has been hypothesized to result from the mechanism described and toxin inhalation, as the nicotine and non-nicotine compounds inhaled are associated with lung epithelial cell injury and inflammation [7]. Another hypothesis stems from the proposed mechanism in marijuana smokers that repeated inhalation through a resistive device generates large negative intrathoracic pressure swings that result in airway barotrauma and ultimately lung collapse [8]. Our patient reported using a JUUL with nicotine liquid pods “every minute of every day” for one year. JUUL has been shown to demonstrate cytotoxicity from both nicotine and some flavor content as the nicotine concentrations have been found to be significantly higher than those of other e-cigarettes and the flavor chemicals can induce significant oxidative stress, inflammation, and alveolar-capillary barrier dysfunction [9,10]. JUUL uses nicotine salts that allow these significantly higher levels of nicotine to be inhaled more easily and with less irritation than the freebase nicotine traditionally used in tobacco products and previous generation e-cigarettes, which makes it particularly popular among smokers and young people. Although JUUL Labs claims that vaping has beneficial impacts, studies have demonstrated that JUUL, among other e-cigarettes, still leads to impairment of endothelial function that comparable to cigarettes [11,12]. Despite this, most of the cases of EVALI have been associated with the use of e-cigarettes containing THC, the concentrations of which can exceed that of dried cannabis by up to 30 times. According to the CDC, THC and vitamin E acetate, a condensing agent in vaping products that had been found in all injured lung fluid samples, may be the culprits of lung injury [13,14].
Most pneumothoraces are confirmed by upright posterior-anterior chest radiographs and may be combined with lateral radiographs in difficult cases. Typically, one will see displacement of the pleural line and an absence of lung marking between the edge of the pleura and wall of the chest. CT is more sensitive than chest radiographs in the detection of pneumothorax, especially small pneumothoraces (less than 15% of the hemithorax), and can provide more detailed information, especially where there is suspicion for underlying lung disease [15]. Subsequent management includes deciding whether air needs to be removed from the pleural space (i.e., needle aspiration or chest tube), which is determined by clinical stability and size (i.e., small: ≤3 cm at apex or ≤2 cm at hilum, versus large: >3 cm at apex or >2 cm at hilum). Afterwards, patients should follow-up in about 1–2 weeks as an outpatient, and a chest radiograph should be performed to ensure lung expansion. At this time, patients should be re-evaluated for any potential diagnoses missed during the initial evaluation that would indicate a secondary pneumothorax [16]. Our patient only required observation with O2 supplementation for 24 hours before being discharged from the hospital and encouraged to follow-up with the pulmonary clinic two weeks after hospitalization. At his follow-up appointment, he underwent a chest x-ray that revealed an almost resolved pneumothorax, but we did not perform any further work-up on the patient to delineate whether or not he had a predisposition to develop a pneumothorax (e.g., alpha-1 antitrypsin deficiency) as his CT at the hospital had revealed clear lung parenchyma. He was encouraged to quit e-cigarettes and follow-up on an as needed basis. Patients discharged from the hospital after inpatient treatment of pneumothorax secondary to e-cigarette use should be encouraged to discontinue use of e-cigarette or vaping products. To this day, our patient has avoided e-cigarettes but, unfortunately, has gone back to smoking cigarettes and marijuana daily.
Conclusion
Although long-term health effects from vaping are not well known, CT studies have demonstrated that vaping-associated respiratory disease has presented with various pulmonary patterns including acute eosinophilic pneumonia, organizing pneumonia, bronchiolitis, acute respiratory distress syndrome, diffuse alveolar hemorrhage, hypersensitivity pneumonitis, the rare giant-cell interstitial pneumonitis and now pneumothorax [17]. Vaping has not yet been established as a risk factor for pneumothorax, but it is well on its way to doing so as more and more cases come to light, such as ours. Practitioners should take more care to inquire about vaping when asking patients about their smoking history and subsequently counsel them on cessation. It is our hope that this case brings more evidence to the dangers of e-cigarette use.
Declaration of competing interest
We have no relevant conflicts of interest to disclose.
References
- 1.Hollingsworth Helen. 2020. E-cigarette or Vaping Product Use Associated Lung Injury (EVALI)https://www.uptodate.com/contents/e-cigarette-or-vaping-product-use-associated-lung-injury-evali Retrieved October 2020, from UpToDate at. [Google Scholar]
- 2.Centers for Disease Control and Prevention . 2020. Outbreak of Lung Injury Associated with the Use of E-Cigarette, or Vaping, Products. Office on Smoking and Health.https://www.cdc.gov/tobacco/basic_information/e-cigarettes/severe-lung-disease.html National Center for Chronic Disease Prevention and Health Promotion. Retrieved January 2021, from. [Google Scholar]
- 3.Traboulsi H., Cherian M., Abou Rjeili M., Preteroti M., Bourbeau J., Smith B.M., Eidelman D.H., Baglole C.J. Inhalation toxicology of vaping products and implications for pulmonary health. Int. J. Mol. Sci. 2020;21(10):3495. doi: 10.3390/ijms21103495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Light R., Lee G. 2020. Pneumothorax in Adults: Epidemiology and Etiology.https://www.uptodate.com/contents/pneumothorax-in-adults-epidemiology-and-etiology Retrieved October 2020, from UpToDate at. [Google Scholar]
- 5.Aubrey A. As vaping illnesses rise, doctors warn of possible 'irreversible damage' to lungs. 2019. https://www.npr.org/sections/health-shots/2019/09/19/762306652/as-vaping-illnesses-rise-doctors-warn-of-possible-irreversible-damage-to-lungs September 19. Retrieved October 2020, from.
- 6.Sharma M., Anjum H., Bulathsinghala C.P., Buch M., Surani S.R. A case report of secondary spontaneous pneumothorax induced by vape. Cureus. 2019;11(11) doi: 10.7759/cureus.60675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bonilla A., Blair A.J., Alamro S.M., Ward R.A., Feldman M.B., Dutko R.A., Karagounis T.K., Johnson A.L., Folch E.E., Vyas J.M. Recurrent spontaneous pneumothoraxes and vaping in an 18-year-old man: a case report and review of the literature. J. Med. Case Rep. 2019;13(1):283. doi: 10.1186/s13256-019-2215-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Johnson M.K., Smith R.P., Morrison D. Large lung bullae in marijuana smokers. Thorax. 2000;55:340–342. doi: 10.1136/thorax.55.4.340. https://doi: 10.1136/thorax.55.4.340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Omaiye E.E., McWhirter K.J., Luo W., Pankow J.F., Talbot P. High-nicotine electronic cigarette products: toxicity of JUUL fluids and aerosols correlates strongly with nicotine and some flavor chemical concentrations. Chem. Res. Toxicol. 2019;32(6):1058–1069. doi: 10.1021/acs.chemrestox.8b00381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Muthumalage T., Lamb T., Friedman M.R. E-cigarette flavored pods induce inflammation, epithelial barrier dysfunction, and DNA damage in lung epithelial cells and monocytes. Sci. Rep. 2019;9:19035. doi: 10.1038/s41598-019-51643-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rao P., Liu J., Springer M.L. JUUL and combusted cigarettes comparably impair endothelial function. Tobacco regulatory science. 2020;6(1):30–37. doi: 10.18001/TRS.6.1.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yingst J.M., Hrabovsky S., Hobkirk A., Trushin N., Richie J.P., Foulds J. Nicotine absorption profile Among regular users of a pod-based electronic nicotine delivery system. JAMA Netw Open. 2019;2(11) doi: 10.1001/jamanetworkopen.2019.15494. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ali M., Khan K., Buch M. A case series of vaping-induced lung injury in a community hospital setting. Case Reports in Pulmonology. 2020;2020:7. doi: 10.1155/2020/9631916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Boudi F.B., Patel S., Boudi A., Chan C. Vitamin E acetate as a plausible cause of acute vaping-related illness. Cureus. 2019;11(12) doi: 10.7759/cureus.6350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Luh S.P. Review: diagnosis and treatment of primary spontaneous pneumothorax. J. Zhejiang Univ. - Sci. B. 2010;11(10):735–744. doi: 10.1631/jzus.B1000131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Light R., Lee G. 2020. Treatment of Primary Spontaneous Pneumothorax in Adults.https://www.uptodate.com/contents/treatment-of-primary-spontaneous-pneumothorax-in-adults Retrieved January 2021, from UpToDate at. [Google Scholar]
- 17.Lilly C.M., Khan S., Waksmundzki-Silva K., Irwin R.S. Vaping-associated respiratory distress syndrome: case classification and clinical guidance. Critical care explorations. 2020;2(2) doi: 10.1097/CCE.0000000000000081. [DOI] [PMC free article] [PubMed] [Google Scholar]