Abstract
Lung cancer metastases to the pancreas are rare but potentially life-threatening. Oftentimes, the presence of symptoms is indicative of extensive disease burden. This report describes a case of primary lung adenocarcinoma metastasizing to the head of the pancreas presenting as obstructive jaundice. The patient was a 61-year-old female veteran who presented with a chronic dyspnea, weight loss, and 3-weeks of nausea and vomiting found to have jaundice, elevated alkaline phosphatase levels, hyperbilirubinemia, and transaminitis. Imaging of her chest revealed large pulmonary parenchymal nodules throughout both lungs with a large left lower lobe mass and consolidation. Abdominal imaging showed a large heterogeneous mass in the pancreatic head, a grossly dilated common bile duct, and enlarged retroperitoneal lymph nodes contiguous with the mass. Pancreatic head biopsies revealed metastatic cancer cells from her lung adenocarcinoma which was confirmed via cytology and the presence of thyroid transcription factor − 1 and cytokeritin-7 expression and the absence of tumor protein 63 staining. Lung adenocarcinomas commonly metastasize to the bones, liver, and central nervous system but very rarely to the pancreas. There have been only a few reported cases of pancreatic tumors that manifested clinically as a result of primary lung cancer metastases however, even though uncommon, hematogenous spread of cancerous tissue should be considered on the differential as a cause for obstructive jaundice in the setting of lung adenocarcinoma.
Keywords: Lung adenocarcinoma, Malignant obstructive jaundice, Pancreatic metastasis, Rare metastasis, Thyroid transcription factor 1, Cytokeratin 7
Abbreviations: TTF-1, Thyroid Transcription Factor – 1; CK-7, Cytokeratin – 7; CK, Cytokeratin; P63, Tumor Protein 63; CNS, Central Nervous System
1. Introduction
Lung adenocarcinoma, a non-small cell lung cancer, represents approximately 40% of all lung cancer diagnoses [1]. Due to its aggressive nature, it remains one of the most common causes of cancer death in the United States for both men and women. Although it has a high affiliation with smokers; it is the most common lung cancer in non-smokers and women. Tumors often arise peripherally rather than centrally and have the ability the metastasize at an early stage. Some studies looking at metastatic patterns noted that lung adenocarcinomas commonly spread to the liver, adrenal glands, bones, and kidneys. Invasion into the pancreas was rare and was only seen in 5% of all cases [2]. This report describes a case of primary lung adenocarcinoma metastasizing to the head of the pancreas presenting as obstructive jaundice.
2. Case
The patient was a 61-year-old, non-smoking, female veteran with a past medical history of hypertension, who presented with a chronic cough, dyspnea, significant 50-pound weight loss, and three weeks of nausea and vomiting. The patient was found to be cachexic with scleral icterus, jaundice, and dry mucous membranes, but had normal bowel sounds without pain, distension, or organomegaly. Respiratory examination was significant for decreased breath sounds in the left lower lung fields. She was tachycardic and hypotensive and labs were significant for hyponatremia with a sodium level of 131 mEq/L and a bicarbonate level of 32 mEq/L. Liver function labs revealed an elevated alkaline phosphatase level of 215 u/L, a total bilirubin level of 5.8 mg/dL, and an aspartate aminotransferase and alanine aminotransferase level of 58 u/L and 36 u/L, respectively. Computed tomography of her chest was done to evaluate her respiratory symptoms which revealed innumerable pulmonary parenchymal nodules throughout both lungs with a large mass extending into the lingula as well as the superior segment of the left lower lobe. There was also pleural effusion around the mass as well (Fig. 1). Abdominal ultrasonography was significant for a severely dilated common bile duct and a moderately distended gall bladder, however, follow up imaging with computed tomography showed a large heterogeneous mass in the pancreatic head which measured approximately 4.5 cm. A grossly dilated common bile duct and enlarged retroperitoneal lymph nodes contiguous with the mass were also seen (Fig. 2). She required biopsies of her lung mass as well as emergent biliary stenting via endoscopic retrograde cholangiopancreatography to relieve her biliary obstruction. Biopsies of both the lung mass and the pancreatic head revealed cell clusters with high nuclear pleomorphism, and prominent nuclei with immunohistological staining positive for thyroid transcription factor−1 (TTF-1), and cytokeratin-7 (CK-7) staining without tumor protein 63 (p63) expression suggesting lung adenocarcinoma as the primary origin of her tumors. Further imaging and work up also revealed the presence of metastases to the brain as well. Due to her widespread tumor burden, radiation therapy and adjunctive chemotherapy were immediately initiated.
Fig. 1.
(Above) Axial chest imaging on admission showing innumerable pulmonary parenchymal nodules throughout both lungs with a large peripherally located, 5.0 × 4.0 cm mass with a central area of necrosis and extensive involvement of the paratracheal and left hilar lymph nodes contiguous with the mass. The mass extended into the lingula as well as the superior segment of the left lower lobe with surrounding consolidation likely post-obstructive pneumonitis.
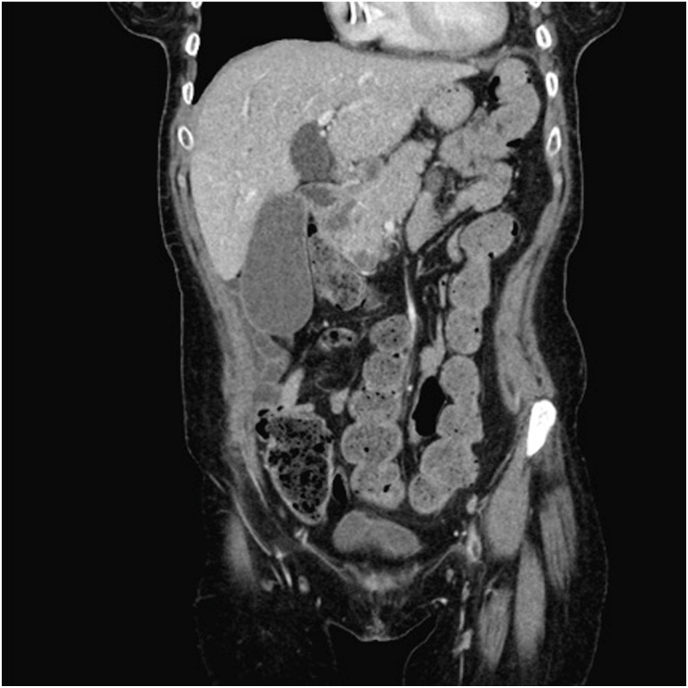
Fig. 2.
(Above) Coronal computed tomography showing a 4.0 × 4.5 cm pancreatic head mass with extension inferiorly into the retroperitoneum with a 2.7 cm biliary ductal dilation, indicating severe obstruction.
3. Discussion
Lung adenocarcinomas often present insidiously, commonly with dyspnea, cough, and unintentional weight loss. Imaging of the chest is crucial for diagnosis and staging. This patient's respiratory complaints prompted further evaluation which showed a peripherally located, 5.0 × 4.0 cm mass with a central area of necrosis and extensive involvement of the paratracheal and left hilar lymph nodes contiguous with the mass. There was also an area of pleural effusion with consolidation concerning for post-obstructive pneumonia. It is known that lung adenocarcinomas have the ability to spread to the bones, liver, and central nervous system (CNS), however, metastasis to the pancreas was only found in approximately 2%–5% of cases [3]. Most tumors usually asymptomatic and only found on autopsy [4]. This patient's abdominal imaging revealed a poorly defined 4.0 × 4.5 cm pancreatic head mass with extension inferiorly into the retroperitoneum with a 2.7 cm biliary ductal dilation, indicating severe obstruction and required advanced endoscopic intervention. Interestingly, of the few studies that looked at metastatic patterns of lung adenocarcinoma, those with pancreatic lesions were also likely to have concomitant lesions in the liver and CNS [5]. This patient had both pancreatic and CNS lesions, but not liver involvement.
The origin of the patient's pancreatic tumor was confirmed via cytology and immunohistochemistry of the pancreatic head and comparing it to the cells to her lung mass tissue. In both samples, the cells were noted to be in clusters with high nuclear-cytoplasmic ratio, nuclear pleomorphism, and prominent nuclei indicating high metastatic burden. The biopsy tissue stained for TTF-1; a primary lung marker synthesized by type 2 alveolar pneumocytes to make surfactant proteins. TTF-1 is also used to differentiate adenocarcinomas from squamous cell lung cancers since its present in 76% of adenocarcinomas [6]. In addition, the absence of p63 also confirms its glandular origin since positive staining is indicative of squamous cell lung cancers. Furthermore, the presence of Cytokeratin (CK) has been useful in differentiating origin of glandular tissue in adenocarcinomas. Lung tissue exhibits CK-7 expression whereas colorectal tissue expresses CK-20 [7]. The presence of only CK-7 in conjunction with TTF-1 and the absence of p63 expression in our patient's pancreatic tissue confirms the metastatic origin of the patient's pancreatic mass was most likely the patient's primary lung adenocarcinoma rather than a gastrointestinal source.
Patients with pancreatic involvement are at high risk of poor outcomes with a 5-year survival rate as low as 5% [8]. Treatment options for widespread disease remains limited to surgical resection or radiation. Although non-small cell lung cancer such as adenocarcinomas are less responsive to radiation therapy, it can be used for inoperable tumors to improve quality of life, especially in tumors that involve the chest or brain. Due to the high risk of relapse, current guidelines recommend adjunctive chemotherapy usually with a cytotoxic agent such as cisplatin or carboplatin. Due to extensive disease burden, this patient received a combination of brain radiation and a regimen consisting of carboplatin, pemetrexed, and pembrolizumab. She underwent multiple whole brain radiation sessions; however, her treatment course was complicated by severe pneumonia after initiating chemotherapy and the patient passed away from sepsis.
4. Conclusion
There have been only a few reported cases of pancreatic metastases that manifested clinically due to primary lung cancer. However, prompt recognition is imperative in order to prevent poor outcomes. Our case demonstrates that even though uncommon, metastatic spread should be considered on the differential as a cause for obstructive jaundice in the setting of suspected lung cancer.
Declaration of competing interest
No disclosures, conflicts of interest, or competing interests to declare.
No prior publications.
Consent was obtained by patient's family for publication of case report.
There are no conflicts of interest to disclose and the institute's Department of Pulmonary and Critical Care at Rutgers University Hospital New Jersey Medical School and VA New Jersey Healthcare System East Orange Veterans Affairs is fully aware of this submission.
All authors listed have contributed to the project and had full access to all aspects of the research and writing process. All equally contributed patient data collection and interpretation, as well as drafting and approving of the final report.
Acknowledgements
We would like to thank Rutgers University New Jersey Medical School and the New Jersey Healthcare System at East Orange Veterans Affairs for making this case report possible.
References
- 1.Myers D.J., Wallen J.M. StatPearls Publishing; 2020. Lung Adenocarcinoma. [Updated 2020 Jun 26]. in: StatPearls [Internet]. Treasure Island (FL)https://www.ncbi.nlm.nih.gov/books/NBK519578/ Jan- [Google Scholar]
- 2.Triantopoulou C., Kolliakou E., Karoumpalis I., Yarmenitis S., Dervenis C. Metastatic disease to the pancreas: an imaging challenge. Insights Imag. 2012;3(2):165–172. doi: 10.1007/s13244-011-0144-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Crippa S., Angelini C., Mussi C., Bonardi C., Romano F., Sartori P., Uggeri F., Bovo G. Surgical treatment of metastatic tumors to the pancreas: a single center experience and review of the literature. World J. Surg. 2006 Aug;30(8):1536–1542. doi: 10.1007/s00268-005-0464-4.PMID:16847716. [DOI] [PubMed] [Google Scholar]
- 4.Matt L., Sehgal R. Metastatic non-small-cell lung cancer to the liver and pancreas. Gastrointest. Canc. Res. 2014;7(2):61–62. [PMC free article] [PubMed] [Google Scholar]
- 5.Milovanovic I.S., Stjepanovic M., Mitrovic D. Distribution patterns of the metastases of the lung carcinoma in relation to histological type of the primary tumor: an autopsy study. Ann. Thorac. Med. 2017;12(3):191–198. doi: 10.4103/atm.ATM_276_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stenhouse G., Fyfe N., King G., Chapman A., Kerr K.M. Thyroid transcription factor 1 in pulmonary adenocarcinoma. J. Clin. Pathol. 2004;57(4):383–387. doi: 10.1136/jcp.2003.007138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Su Y.C., Hsu Y.C., Chai C.Y. Role of TTF-1, CK20, and CK7 immunohistochemistry for diagnosis of primary and secondary lung adenocarcinoma. Kaohsiung J. Med. Sci. 2006 Jan;22(1):14–19. doi: 10.1016/S1607-551X(09)70214-1. PMID: 16570563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Masetti M., Zanini N., Martuzzi F., Fabbri C., Mastrangelo L., Landolfo G., Fornelli A., Burzi M., Vezzelli E., Jovine E. Analysis of prognostic factors in metastatic tumors of the pancreas: a single-center experience and review of the literature. Pancreas. 2010 Mar;39(2):135–143. doi: 10.1097/MPA.0b013e3181bae9b3. PMID: 19820422. [DOI] [PubMed] [Google Scholar]