Abstract
Background: There is evidence of a high psychological toll from the COVID-19 pandemic in healthcare workers. This paper was aimed at conducting a systematic review and meta-analysis of studies reporting levels of depression among healthcare workers during the COVID-19 and estimating the pooled prevalence of depression. Methods: We searched for cross-sectional studies listed on PubMed from 1 December 2019 to 15 September 2020 that reported prevalence of depression in healthcare workers, nurses, medical doctors, and COVID-19 frontline professionals. The pooled proportions of depression were calculated with random effects models. Results: We identified 57 studies from seventeen countries. The pooled prevalence of depression in healthcare workers was 24% (95% CI: 20–28%), 25% for nurses (95% CI: 18–33%), 24% for medical doctors (95% CI: 16–31%), and 43% for frontline professionals (95% CI: 28–59%). Conclusions: The proportion of depression in nurses and medical doctors during the COVID-19 pandemic was similar to that found in the general population as previously reported in other meta-analyses conducted with smaller numbers of studies. Importantly, almost half of the frontline healthcare workers showed increased levels of depression. There is need for a comprehensive, international response to prevent and treat common mental health problems in healthcare workers.
Keywords: depressive symptoms, COVID-19, nurses, medical doctors, frontline, pooled prevalence
1. Introduction
The new coronavirus (SARS-CoV-2) was first identified in a wet market in Wuhan, Hubei province, China, in December 2019 [1]. This virus causes a highly infectious acute respiratory syndrome (COVID-19) that can be associated with serious pneumonia and eventually lead to death. Due to its rapid spread around the world, the World Health Organization [2] declared the COVID-19 as a pandemic in March 2020, and from its identification to this date (12th November 2020), more than 51.9 million people have been confirmed as cases worldwide, with 1.2 million deaths [3]. The enormous impact on people’s physical and mental health, and on economic systems worldwide, is one of the main challenges for society in this century [4].
Healthcare workers (HCW) are a fundamental part of the global response to COVID-19. Because of their close personal exposure to patients with COVID-19, their risk of infection is very high. A recent study reports HCW to be at an 11.6 times higher risk of infection than the general population, although this risk decreases to 3.4 after accounting for the differences in testing frequency between HCW and the general community [5]. Besides this higher risk of infection, several observational studies conducted during the COVID-19 pandemic have shown that health professionals are at a higher risk of developing psychological problems [6]. Growing patient load and working under pressure in resource-deprived settings might increase psychological stress among HCW [7,8]. They are also more exposed to prolonged work shifts, lack of adequate equipment (i.e., protective equipment (PPE)), and fear of infecting themselves or relatives [9,10]. This fear, in turn, may be associated with anxiety, depression, and insomnia [11,12,13].
HCW thus constitute one of the groups most vulnerable to psychological distress, requiring immediate interventions to improve their wellbeing and the healthcare system capacity. Two very recent systematic reviews and meta-analyses on the prevalence of anxiety and depression have been published, reporting the pooled prevalence among HCW. The first one, conducted by Pappa et al. [14] in April 2020, included a total of thirteen cross-sectional studies (all of them conducted in China except one, from Singapore) reporting a pooled prevalence of anxiety of 23.2% and 22.8% for depression. The second [15] was based on seven studies conducted in China and found an increased risk of anxiety and depression in HCW, compared with other professionals (OR = 1.61; 95%CI 1.33 to 1.96 and OR = 1.32; 95%CI 1.09 to 1.60, respectively).
Due to the rapid, evolving nature of this health emergency, an increasing number of other studies from different countries addressing mental health problems among HCW have been published in recent months. Thus, the present study is aimed at updating and extending the previous work of Pappa et al. [14] and da Silva and Neto [15] by conducting a systematic review and meta-analysis of studies published afterwards reporting a global prevalence of anxiety and depression among HCW during the COVID-19 outbreak.
2. Materials and Methods
The present study followed the PRISMA guidelines for reporting systematic reviews and meta-analysis [16] (Supplementary Table S1).
2.1. Search Strategy
The search strategy (Supplementary Table S2) included all cross-sectional studies informing about the prevalence of depression that were published from 1 December 2019 to 15 September 2020. The search was conducted by two researchers (MPM and JBN) using MEDLINE via PubMed. Briefly, they focused on depression, although an anxiety term was additionally included to examine whether these articles also included relevant information about depression. Depression could be measured either using diagnostic tools (e.g., structured interviews) or standardized scales to assess depressive symptomatology. As our main objective was to calculate the overall prevalence of depression, in case we found a study using scales, we considered the presence of depression reported according to a certain cut-off point for that given scale. Thus, henceforth we use the term “depression” to refer to either a full-blown diagnosis or presence of depression according to a cut-off point.
Search terms also included samples of HCW, nurses, medical doctors, and/or frontline HCW. There was no language restriction. We inspected references from selected articles to detect additional studies. In case of disagreement, a third and fourth reviewer (JS and IL) were consulted to reach a consensus.
2.2. Selection Criteria
The following inclusion criteria for studies were used: (1) studies providing cross-sectional data on the proportion of depression during the COVID-19 outbreak; (2) studies conducted with samples of health care workers; (3) studies in which the assessment methods for depression were described; and (4) studies for which the full-text was available. Studies that used other specific samples (e.g., adolescents and patients) and review articles were excluded from the present study.
We extracted the following data using a pre-designed form: country, sample size, prevalence rates of depression, proportion of women, average age, instruments used to assess depression, response rate, and sampling methods.
2.3. Assessment of Methodological Quality
Two independent reviewers (JS and JBN) rated the methodological validity of selected articles before their inclusion in the review using the Joanna Briggs Institute (JBI) standardized critical appraisal instrument for prevalence studies [17]. This tool uses nine criteria to evaluate quality with a score ranging from zero (‘No’) to one (‘Yes’).
In case of disagreement between the two reviewers, there was a discussion to resolve it between them or with a third reviewer (PGG).
2.4. Statistical Analysis
We used a generic inverse variance method with a random effect model [18]. To check heterogeneity across studies, we calculated the Hedges Q statistic (a p value < 0.10 indicates statistical significance) and the I2 statistic and 95% confidence interval [19]. I2 values between 25% and 50% are considered low, 50%–75% moderate, and 75% or greater high [20]. Different study designs or demographic characteristics may explain the heterogeneity. Thus, we calculated meta-regression and carried out subgroup analyses [21] to find potential sources of heterogeneity [22]. A sensitivity analysis was also made by omitting studies one by one. This allowed us to learn how each individual study influenced the overall result. Publication bias was determined by visually inspecting a funnel plot. Since funnel plots might inaccurately assess publication bias in meta-analyses of proportion studies [23], we additionally calculated Egger’s [24] and Begg’s tests [25], with p values < 0.05 indicating publication bias.
Despite the fact that one inclusion criterion for a given study was the use of HCW samples, we were interested in separately calculating the pooled prevalence for the following groups: HCW in general (with no distinction of the type of worker or working in the frontline), nurses, medical doctors, and frontline HCW. Frontline HCW were those who provided direct care to patients with a diagnosis of infection by COVID-19 or who worked in units where care was provided. Additionally, for practical purposes, the pediatric HCW, physical therapists, and laboratory HCW were considered as HCW. Statistical analyses were conducted with STATA statistical software (version 10.0; College Station, TX, USA) and R [26].
3. Results
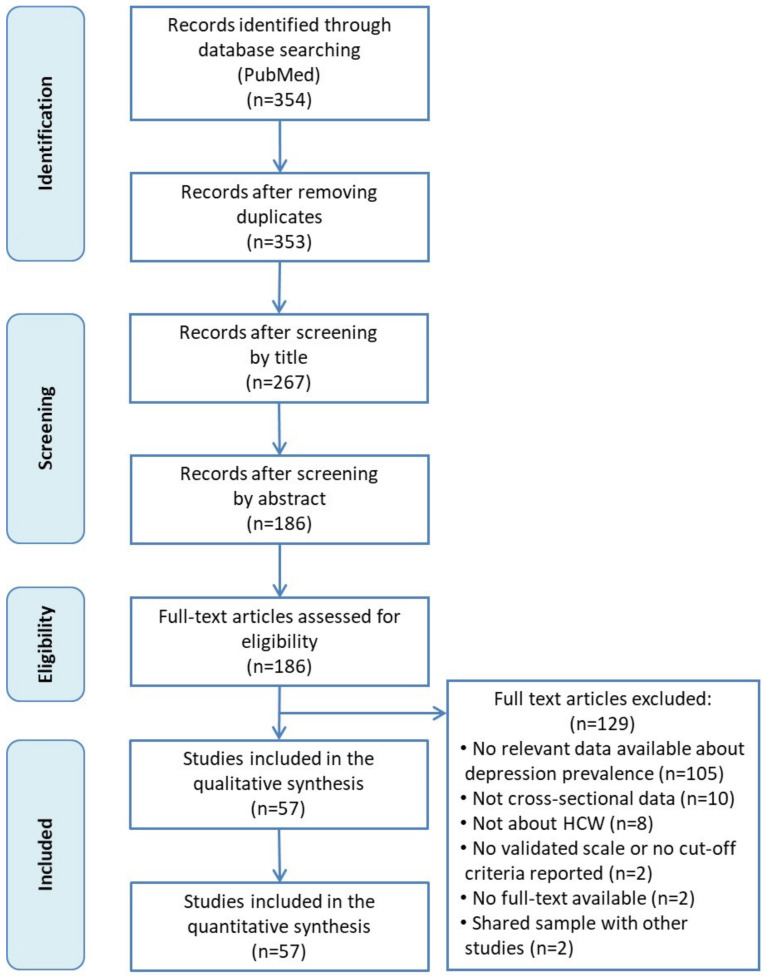
Flowchart of the search strategy and study selection process is shown in Figure 1. We initially identified 354 studies. After removing duplicates and studies after the first screening, 186 articles were read in full. Finally, a total of 57 studies were included in the present meta-analysis [6,12,13,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80].
Figure 1.
Flowchart of the study selection.
The results are organized as follows: Table 1 shows the characteristics of those studies (46) that reported prevalence rates of depression in HCW (without distinction in the type of workers); Table 2 displays characteristics of studies reporting data from nurses (14); Table 3 characteristics for medical doctors (10); and Table 4 for frontline HCW (12).
Table 1.
Characteristics of the studies included in the meta-analysis based on samples of healthcare workers.
| Author (Publication Year) | Population | Country | Mean Age (SD) | % Females (n) | Sample Size (n) | Response Rate (%) | Sampling Method | Depression Assessment |
Time Frame Assessment | Diagnostic Criteria | Prevalence | Quality Assessment * | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| % | n | ||||||||||||
| Chen J. et al. (2020) | HCW | China | 36.54 (8.57) | 68.63% (619) | 902 | NR | Convenience sampling | PHQ-9 | Last 2 weeks | ≥10 | 18.29% | 165 | 7 |
| Chen Y. et al. (2020) | Pediatric HCW | China | 32.6 (6.5) | 90.48% (95) | 105 | 84.68% | NR | SDS | Past several days | ≥53 | 29.52% | 31 | 7 |
| Chew et al. (2020) | HCW | India, Singapore | 29 (NR) | 64.3% (583) | 906 | 90.60% | NR | DASS-21 | Last week | ≥14 | 5.30% | 48 | 8 |
| Di Tella et al. (2020) | HCW | Italy | 42.9 (11.2) | 72.4% (105) | 145 | NR | Convenience sampling | BDI-II | Last 2 weeks | >13 | 31.03% | 45 | 6 |
| Dosil Santamaría et al. (2020) | HCW | Spain | 42.8 (10.2) | 80.29% (338) | 421 | NR | Snowball sampling | DASS-21 | Last week | ≥14 | 16.86% | 71 | 7 |
| Elbay et al.(2020) | HCW | Turkey | 36.05 (8.69) | 56.8% (251) | 442 | NR | Convenience sampling | DASS-21 | Last week | ≥14 | 47.06% | 208 | 7 |
| Elhadi et al. (2020) | HCW | Libya | 33.3 (7.4) | 51.94% (387) | 745 | 93.13% | Convenience sampling | HADS | Last week | >10 | 56.38% | 420 | 8 |
| Gallopeni et al. (2020) | HCW | Kosovo | 39 (10.37) | 61.32% (363) | 592 | NR | NR | HADS | Last week | >10 | 38.68% | 229 | 7 |
| Gupta A.K. et al. (2020) | HCW | Nepal | 29.5 (6.1) | 52.67% (79) | 150 | NR | Snowball sampling | PHQ-9 | Last 2 weeks | ≥10 | 8.00% | 12 | 6 |
| Gupta S. et al. (2020) | HCW | India | NR | 36.12% (406) | 1124 | 79.45% | Quota sampling | HADS | Last week | >7 | 31.49% | 354 | 8 |
| Huang & Zhao (2020) | HCW | China | NR | NR | 2250 | 85.30% | Convenience sampling | CES-D | Last 2 weeks | >28 | 19.82% | 446 | 7 |
| Kannampallil et al. (2020) | HCW | USA | NR | 54.96% (216) | 393 | 28.58% | NR | DASS-21 | Last week | ≥10 | 27.23% | 107 | 6 |
| Keubo et al. (2020) | HCW | Cameroon | NR | 54.45% (159) | 292 | NR | Snowball sampling | HADS | Last week | >10 | 43.49% | 127 | 6 |
| Khanna et al. (2020) | HCW | India | 42.5 (12.05) | 43.44% (1023) | 2355 | NR | NR | PHQ-9 | Last 2 weeks | ≥10 | 11.21% | 264 | 7 |
| Koksal et al. (2020) | HCW | Turkey | 35.6 (8.5) | 70.1% (492) | 702 | NR | NR | HADS | Last week | >7 | 36.89% | 259 | 7 |
| Krammer et al. (2020) | HCW | Switzerland | 42.6 (13.5) | 74.00% (74) | 85 | 76.92% | Convenience sampling | PHQ-9 | Last 2 weeks | ≥10 | 15.29% | 13 | 7 |
| Lai et al. (2020) | HCW | China | NR | 76.69% (964) | 1257 | 68.69% | Convenience sampling | PHQ-9 | Last 2 weeks | ≥10 | 14.80% | 186 | 8 |
| Lam et al. (2020) | HCW | China | NR | 75.21% (701) | 932 | 59.51% | Convenience sampling | PHQ-9 | Last 2 weeks | ≥9 | 24.36% | 227 | 7 |
| Li et al. (2020) | HCW | China | NR | 100% (4369) | 4369 | 82.17% | Convenience sampling | PHQ-9 | Last 2 weeks | ≥10 | 14.21% | 621 | 8 |
| Liang et al. (2020) | HCW | China | NR | 81.31% (731) | 899 | NR | Convenience sampling | PHQ-9 | Last 2 weeks | ≥10 | 24.25% | 218 | 7 |
| Lin et al. (2020) | HCW | China | NR | NR | 2316 | NR | Convenience sampling | PHQ-9 | Last 2 weeks | >5 | 46.89% | 1086 | 6 |
| Liu et al. (2020) | Pediatric HCW | China | NR | 85.52% (1737) | 2031 | NR | Convenience sampling | DASS-21 | Last week | ≥14 | 7.09% | 144 | 7 |
| Lu et al. (2020) | HCW | China | NR | 77.64% (1785) | 2299 | 94.88% | NR | HAMD | Last week | ≥7 | 11.66% | 268 | 8 |
| Magnavita et al. (2020) | HCW | Italy | NR | 70.10% (417) | 595 | 73.46% | Convenience sampling | GADS | Last 2 weeks | ≥2 | 20.34% | 121 | 8 |
| Naser et al. (2020) | HCW | Jordan | NR | 56,1% (653) | 1163 | NR | Convenience sampling | PHQ-9 | Last 2 weeks | ≥10 | 44.71% | 520 | 7 |
| Ning et al. (2020) | HCW | China | NR | 72.88% (446) | 612 | NR | Snowball sampling | SDS | Past several days | ≥53 | 25.00% | 153 | 7 |
| Que et al. (2020) | HCW | China | 31.06 (6.99) | 69.06% (1578) | 2285 | NR | Convenience sampling | PHQ-9 | Last 2 weeks | ≥10 | 12.82% | 293 | 7 |
| Sahin et al. (2020) | HCW | Turkey | NR | 66.03% (620) | 939 | NR | Convenience sampling | PHQ-9 | Last 2 weeks | ≥10 | 37.59% | 353 | 7 |
| Salopek-Žiha et al. (2020) | HCW | Croatia | NR | NR | 124 | NR | Convenience sampling | DASS-21 | Last week | ≥14 | 11.29% | 14 | 5 |
| Si et al. (2020) | HCW | China | NR | 70.68% (610) | 863 | 76.00% | Convenience sampling | DASS-21 | Last week | ≥14 | 6.03% | 52 | 8 |
| Song et al. (2020) | HCW | China | 34 (8.2) | 64.3% (NR) | NR | Convenience sampling | CES-D | Last 2 weeks | ≥16 | 25.18% | 3733 | 7 | |
| Stojanov et al. (2020) | HCW | Serbia | 40.5 (8.37) | 66.17% (133) | 201 | NR | NR | SDS | Past several days | ≥60 | 15.92% | 32 | 6 |
| Suryavanshi et al. (2020) | HCW | India | NR | 51.27% (101) | 197 | 20.40% | Snowball sampling | PHQ-9 | Last 2 weeks | ≥10 | 22.34% | 44 | 6 |
| Teng et al. (2020) | HCW | China | NR | NR | 338 | NR | Snowball sampling | PHQ-9 | Last 2 weeks | ≥5 | 34.62% | 117 | 6 |
| Teo et al. (2020) | Laboratory HCW | Singapore | 34 (NR) | 73.77% (90/122) | 103 | 84.43% | NR | SDS | Past several days | ≥60 | 37.86% | 39 | 7 |
| Vanni et al. (2020) | HCW | Italy | 47 (10.37) | 65.22% (30) | 46 | 90.20% | Convenience sampling | DASS-21 | Last week | ≥14 | 26.09% | 12 | 7 |
| Wang H. et al. (2020) | HCW | China | NR | 85.84% (897) | 1045 | 73.18% | Convenience sampling | HADS | Last week | >10 | 13.59% | 142 | 7 |
| Wang L.Q. et al. (2020) | HCW | China | 37 (NR) | 77.37% (212) | 274 | NR | Convenience sampling | PHQ-9 | Last 2 weeks | ≥10 | 16.06% | 44 | 6 |
| Wang S. et al. (2020) | Pediatric HCW | China | 33.75 (8.41) | 90.24% (111) | 123 | 52.44% | Convenience sampling | SDS | Past several days | ≥50 | 25.20% | 31 | 7 |
| Wang W. et al. (2020) | HCW | China | 33.5 (8.89) | 64.52% (1291) | 2001 | 72.06% | Convenience sampling | HADS | Last week | >7 | 35.03% | 701 | 8 |
| Wankowicz et al. (2020) | HCW | Poland | 40.25 (5.25) | 52.15% (230) | 441 | NR | NR | PHQ-9 | Last 2 weeks | >5 | 70.75% | 312 | 7 |
| Xiao et al. (2020) | HCW | China | NR | 67.22% (644) | 958 | NR | Convenience sampling | HADS | Last week | >7 | 57.31% | 549 | 6 |
| Xiaoming et al. (2020) | HCW | China | 33.25 (8.26) | 77.93% (6874) | 8817 | 90.62% | Convenience sampling | PHQ-9 | Last 2 weeks | ≥10 | 9.41% | 830 | 8 |
| Yang et al. (2020) | Physical therapists | South Korea | NR | 47.69% (31) | 65 | 89.04% | Convenience sampling | PHQ-9 | Last 2 weeks | ≥10 | 18.46% | 12 | 7 |
| Zhang et al. (2020) | HCW | China | NR | 82.73% (1293) | 1563 | 80.32% | Convenience sampling | PHQ-9 | Last 2 weeks | ≥10 | 17.21% | 269 | 8 |
| Zhu et al. (2020) | HCW | China | NR | 85.03% (4304) | 5062 | 77.07% | Convenience sampling | PHQ-9 | Last 2 weeks | ≥10 | 13.45% | 681 | 8 |
Note. * Quality score based on the Joanna Briggs Institute (JBI) standardized critical appraisal instrument for prevalence studies [17] (see Supplementary Table S3). NR = not reported; BDI-II = Beck depression inventory-second edition; CES-D = Center for Epidemiologic Studies-Depression scale; DASS-21 = Depression, Anxiety and Stress scales; GADS = Goldberg Anxiety and Depression Scale; HADS = Hospital Anxiety and Depression Scale; HAMD = Hamilton Depression Rating Scale; PHQ-9 = Patient Health Questionnaire; SDS = Zung’s Self-Rating Depression Scale.
Table 2.
Characteristics of the studies included in the meta-analysis based on samples of nurses.
| Author (Publication Year) | Population | Country | Mean Age (SD) | % Females (n) | Sample Size (n) | Response Rate (%) | Sampling Method | Depression Assessment | Time Frame Assessment | Diagnostic Criteria | Prevalence | Quality Assessment * | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| % | n | ||||||||||||
| An et al. (2020) | Nurses | China | 32.2 (7.61) | 90.75% (1001) | 1103 | NR | Snowball sampling | PHQ-9 | Last 2 weeks | ≥10 | 15.96% | 176 | 7 |
| Dal’Bosco et al. (2020) | Nurses | Brazil | NR | 79% (89.8) | 88 | 18.49% | Convenience sampling | HADS | Last week | >7 | 25.00% | 22 | 6 |
| Gupta S. et al. (2020) | Nurses | India | NR | NR | 207 | 79.45% | Quota sampling | HADS | Last week | >7 | 38.65% | 80 | 6 |
| Keubo et al. (2020) | Nurses | Cameroon | NR | NR | 168 | NR | Snowball sampling | HADS | Last week | >10 | 44.05% | 74 | 5 |
| Lai et al. (2020) | Nurses | China | NR | 90.84% (694) | 764 | 68.69% | Convenience sampling | PHQ-9 | Last 2 weeks | ≥10 | 15.45% | 118 | 8 |
| Liu Y. et al. (2020) | Nurses | China | NR | NR | 1173 | NR | Convenience sampling | DASS-21 | Last week | ≥14 | 6.31% | 74 | 6 |
| Ning et al. (2020) | Nurses | China | NR | 97.97% (289) | 295 | NR | Snowball sampling | SDS | Past several days | ≥53 | 30.17% | 89 | 6 |
| Pouralizadeh et al. (2020) | Nurses | Iran | 36.34 (8.74) | 95.2% (420) | 441 | NR | NR | PHQ-9 | Last 2 weeks | ≥10 | 37.41% | 165 | 7 |
| Que et al. (2020) | Nurses | China | 35.94 (8.17) | 97.75% (195) | 208 | NR | Convenience sampling | PHQ-9 | Last 2 weeks | ≥10 | 12.02% | 25 | 6 |
| Sahin et al. (2020) | Nurses | Turkey | NR | NR | 254 | NR | Convenience sampling | PHQ-9 | Last 2 weeks | ≥10 | 42.13% | 107 | 5 |
| Tu et al. (2020) | Frontline Nurses | China | 34.44 (5.85) | 100% (100) | 100 | 100% | Cluster Sampling | PHQ-9 | Last 2 weeks | ≥5 | 46.00% | 46 | 8 |
| Wang H. et al. (2020) | Nurses | China | NR | NR | 773 | 73.18% | Convenience sampling | HADS | Last week | >10 | 13.58% | 105 | 7 |
| Xiong et al. (2020) | Nurses | China | NR | 97.31 (217) | 223 | 61.80% | Convenience sampling | PHQ-9 | Last 2 weeks | ≥10 | 6.73% | 15 | 7 |
| Zhu J. et al. (2020) | Frontline Nurses | China | NR | NR | 86 | NR | Convenience sampling | SDS | Past several days | ≥50 | 43.02% | 37 | 5 |
Note. * Quality score based on the Joanna Briggs Institute (JBI) standardized critical appraisal instrument for prevalence studies [17] (see Supplementary Table S3). NR = not reported; DASS-21 = Depression, Anxiety and Stress scales; HADS = Hospital Anxiety and Depression Scale; PHQ-9 = Patient Health Questionnaire; SDS = Zung’s Self-Rating Depression Scale.
Table 3.
Characteristics of the studies included in the meta-analysis based on samples of medical doctors.
| Author (Publication Year) | Population | Country | Mean Age (SD) | % Females (n) | Sample Size (n) | Response Rate (%) | Sampling Method | Depression Assessment | Time Frame Assessment | Diagnostic Criteria | Prevalence | Quality Assessment * | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| % | n | ||||||||||||
| Almater et al. (2020) | MD | Saudi Arabia | 32.9 (9.6) | 43.9% (47) | 107 | 30.60% | Convenience sampling | PHQ-9 | Last 2 weeks | ≥10 | 28.97% | 31 | 6 |
| Gupta S. et al. (2020) | MD | India | NR | NR | 749 | 79.45% | Quota sampling | HADS | Last week | >7 | 28.17% | 211 | 7 |
| Keubo et al. (2020) | MD | Cameroon | NR | NR | 74 | NR | Snowball sampling | HADS | Last week | >10 | 39.19% | 29 | 5 |
| Lai et al. (2020) | MD | China | NR | 54.77% (270) | 493 | 68.69% | Convenience sampling | PHQ-9 | Last 2 weeks | ≥10 | 13.79% | 68 | 8 |
| Liu Y. et al. (2020) | MD | China | NR | NR | 858 | NR | Convenience sampling | DASS-21 | Last week | ≥14 | 8.16% | 70 | 6 |
| Ning et al. (2020) | MD | China | NR | 49.53% (157) | 317 | NR | Snowball sampling | SDS | Past several days | ≥53 | 20.19% | 64 | 6 |
| Que et al. (2020) | MD | China | 33.69 (7.44) | 63.49% (546) | 860 | NR | Convenience sampling | PHQ-9 | Last 2 weeks | ≥10 | 12.91% | 111 | 7 |
| Sahin et al. (2020) | MD | Turkey | NR | NR | 580 | NR | Convenience sampling | PHQ-9 | Last 2 weeks | ≥10 | 35.69% | 207 | 6 |
| Wang H. et al. (2020) | MD | China | NR | NR | 149 | 73.18% | Convenience sampling | HADS | Last week | >10 | 17.45% | 26 | 6 |
| Zhu J. et al. (2020) | Frontline MD | China | NR | 64.56% (51) | 79 | NR | Convenience sampling | SDS | Past several days | ≥50 | 45.57% | 36 | 6 |
Note. * Quality score based on the Joanna Briggs Institute (JBI) standardized critical appraisal instrument for prevalence studies [17] (see Supplementary Table S3). NR = not reported; DASS-21 = Depression, Anxiety and Stress scales; HADS = Hospital Anxiety and Depression Scale; PHQ-9 = Patient Health Questionnaire; SDS = Zung’s Self-Rating Depression Scale.
Table 4.
Characteristics of the studies included in the meta-analysis based on samples of frontline healthcare workers.
| Author (Publication Year) | Population | Country | Mean Age (SD) | % Females (n) | Sample Size (n) | Response Rate (%) | Sampling Method | Depression Assessment |
Time Frame Assessment | Diagnostic Criteria | Prevalence | Quality Assessment * | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| % | n | ||||||||||||
| Cai et al. (2020) | Frontline HCW | China | 30.6 (8.8) | 68.82% (819) | 1173 | NR | Non-probabilistic sampling | PHQ-9 | Last 2 weeks | ≥10 | 14.32% | 168 | 7 |
| Kannampallil et al. (2020) | Frontline HCW | USA | NR | 51.38% (112) | 218 | 15.85% | NR | DASS-21 | Last week | ≥10 | 27.98% | 61 | 5 |
| Lai et al. (2020) | Frontline HCW | China | NR | NR | 522 | 68.69% | Convenience sampling | PHQ-9 | Last 2 weeks | ≥10 | 18.01% | 94 | 7 |
| Luceño-Moreno et al. (2020) | Frontline HCW | Spain | 43.88 (10.82) | 86.40% (1228) | 1422 | 92.40% | Non probabilistic sampling | HADS | Last week | ≥7 | 51.34% | 730 | 8 |
| Sandesh et al. (2020) | Frontline HCW | Pakistan | NR | 42.86% (48) | 112 | NR | Convenience sampling | DASS-21 | Last week | ≥14 | 72.32% | 81 | 5 |
| Stojanov et al. (2020) | Frontline HCW | Serbia | 39.1 (7.3) | 65.25% (77) | 118 | NR | NR | SDS | Past several days | ≥60 | 17.80% | 21 | 6 |
| Tu et al. (2020) | Frontline Nurses | China | 34.44 (5.85) | 100% (100) | 100 | 100% | Cluster Sampling | PHQ-9 | Last 2 weeks | ≥5 | 46.00% | 46 | 8 |
| Wang H. et al. (2020) | Frontline HCW | China | NR | NR | 401 | 73.18% | Convenience sampling | HADS | Last week | >10 | 16.46% | 66 | 7 |
| Wang W. et al. (2020) | Frontline HCW | China | NR | 59.46% (393) | 661 | 72.06% | Convenience sampling | HADS | Last week | >7 | 45.99% | 304 | 8 |
| Wankowicz et al. (2020) | Frontline HCW | Poland | 40.47 (4.93) | 56.31% (116) | 206 | NR | NR | PHQ-9 | Last 2 weeks | >5 | 99.51% | 205 | 6 |
| Zhou et al. (2020) | Frontline HCW | China | 35.77 (8.13) | 81.19% (492) | 606 | NR | NR | PHQ-9 | Last 2 weeks | >5 | 57.59% | 349 | 7 |
| Zhu J. et al. (2020) | Frontline HCW | China | 34.16 (8.06) | 83.03% (137) | 165 | NR | Convenience sampling | SDS | Past several days | ≥50 | 44.24% | 73 | 6 |
Note. * Quality score based on the Joanna Briggs Institute (JBI) standardized critical appraisal instrument for prevalence studies [17] (see Supplementary Table S3). NR = not reported; DASS-21 = Depression, Anxiety and Stress scales; HADS = Hospital Anxiety and Depression Scale; PHQ-9 = Patient Health Questionnaire; SDS = Zung’s Self-Rating Depression Scale.
Approximately half of the studies were conducted in China (n = 24), but we also found studies from India (n = 4), Italy (n = 3), Turkey (n = 3), Singapore (n = 2), and one study from each of the following countries: Cameroon, Croatia, Jordan, Kosovo, Libya, Nepal, Poland, Serbia, South Korea, Spain, Switzerland, and the USA. The sample size ranged from 46 to 14,825 participants, and the mean age ranged from 29 to 47 years. All studies except one included both men and women, with women predominating in most of the studies that reported this (40 out of 43). All studies used online questionnaires and all except two used non-random methods. Twenty-three studies reported response rate, ranging from 20.4% to 94.9%. All studies measured depression using standardized scales, most commonly the Patient Health Questionnaire-9 (PHQ-9, n = 21 studies), the Depression, Anxiety, and Stress Scale (DASS-21, n = 8 studies), and the Hospital Anxiety and Depression Scale (HADS, n = 8 studies).
The risk of bias ranged from 5 to 8, with a mean score of 6.95 (Supplementary Table S3, Table 1). The most common limitations were (a) recruitment of participants not appropriate (56 studies), (b) response rate not reported or large number of non-responders (33 studies), and (c) sample size too small to ensure good precision of the final estimate (19 studies).
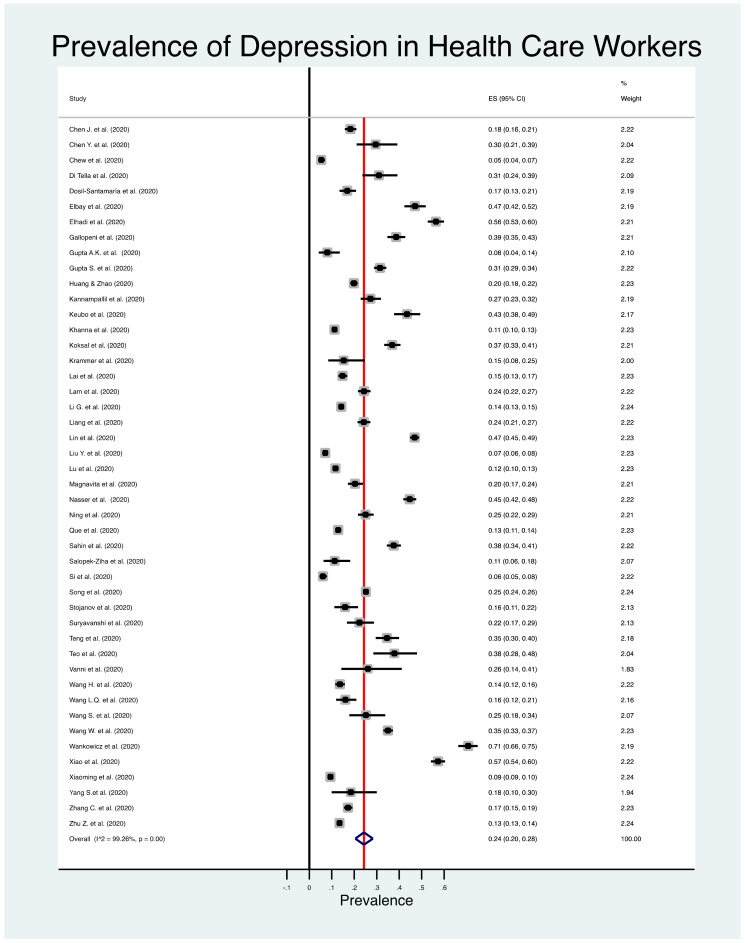
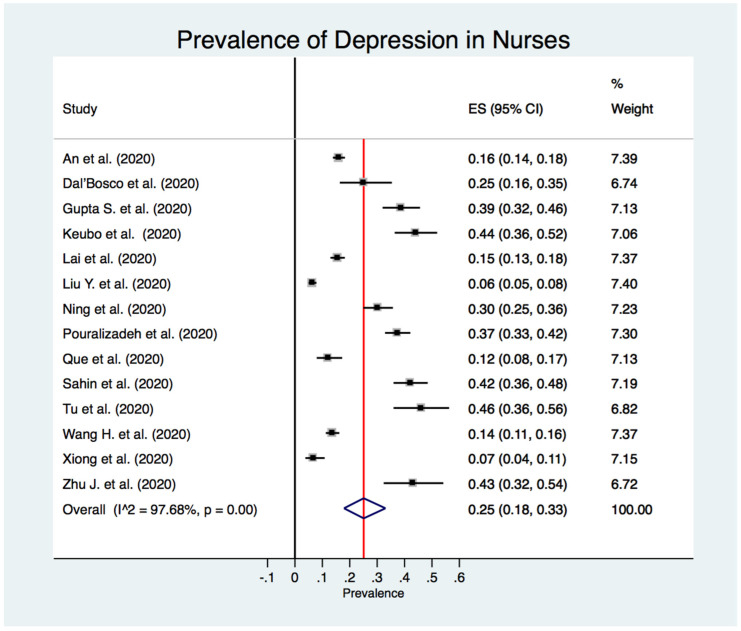
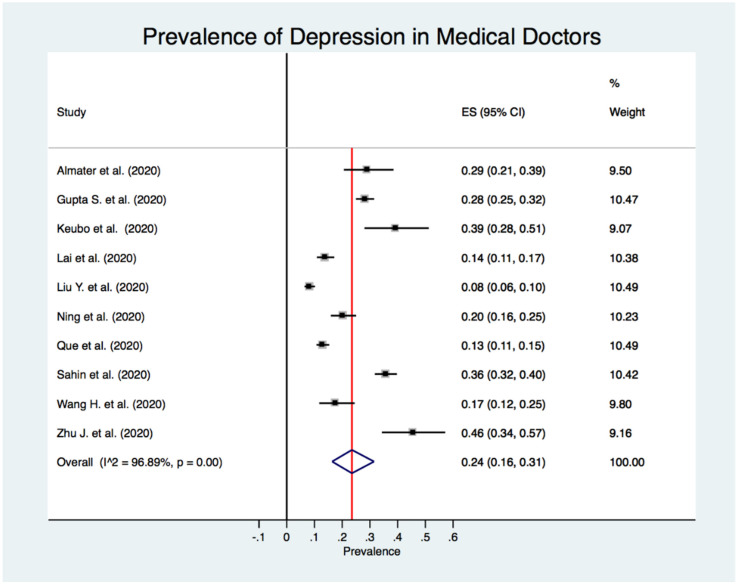
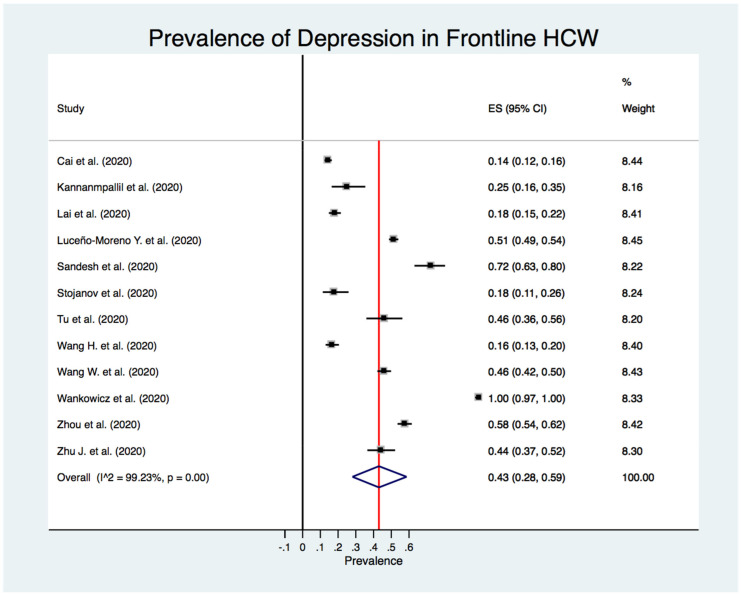
Figure 2 shows the estimated overall prevalence of depression in HCW (24%; 95% CI: 20%–28%), 25% in nurses (95% CI: 18%–33%) (Figure 3), 24% in medical doctors (95% CI: 16%–31%) (Figure 4), and 43% in frontline HCW (95% CI: 28%–59%) (Figure 5), with significant heterogeneity between studies (Q test: p < 0.001) across these four categories. Additionally, the prevalence of depression in frontline HCW was significantly higher than in HCW overall (p < 0.05).
Figure 2.
Forest plot for the prevalence of depression among healthcare workers.
Figure 3.
Forest plot for the prevalence of depression among nurses.
Figure 4.
Forest plot for the prevalence of depression among medical doctors.
Figure 5.
Forest plot for the prevalence of depression among frontline healthcare workers.
Potential sources of heterogeneity were investigated across the studies. Our subgroup analysis showed that prevalence of depression was lower in studies using the DASS-21, those carried out in China, studies using convenience sampling methods and those of high methodological quality (Table 5).
Table 5.
Overall prevalence rates of depression according to study characteristics.
| Healthcare Workers | Nurses | Medical Doctors | Frontline Healthcare Workers | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No. Studies | Prevalence (%) (95% CI) |
p * | No. Studies | Prevalence (%) (95% CI) |
p * | No. Studies | Prevalence (%) (95% CI) |
p * | No. Studies | Prevalence (%) (95% CI) |
p * | |
| Depression assessment | 0.531 | 0.636 | 0.964 | 0.600 | ||||||||
| PHQ-9 | 20 | 23 (17–29) | 7 | 23 (14–34) | 4 | 22 (11–35) | 5 | 50 (18–81) | ||||
| HADS | 43 | 43 (35–51) | 4 | 29 (14–48) | 3 | 27 (18–38) | 2 | 51 (44–58) | ||||
| DASS-21 | 9 | 16 (9–24) | 1 | 6 (5–8) | 1 | 8 (6–10) | 3 | 37 (19–57) | ||||
| SDS | 5 | 26 (20–32) | 2 | 33 (28–38) | 2 | 25 (21–29) | 2 | 32 (27–38) | ||||
| CES-D | 2 | 24 (24–25) | - | - | - | - | - | - | ||||
| Other (BDI-II/HAMD/GADS) | 3 | 20 (11–31) | - | - | - | - | - | - | ||||
| Country | 0.087 | 0.031 | 0.067 | 0.235 | ||||||||
| China | 23 | 21 (16–25) | 8 | 21 (15–27) | 6 | 18 (12–24) | 7 | 33 (19–49) | ||||
| Other | 23 | 28 (21–36) | 6 | 38 (33–43) | 4 | 32 (27–38) | 5 | 57 (25–86) | ||||
| Sampling method | 0.803 | 0.058 | 0.508 | 0.900 | ||||||||
| Convenience | 29 | 23 (19–28) | 8 | 19 (11–27) | 7 | 22 (13–32) | 5 | 38 (21–57) | ||||
| Other | 7 | 25 (18–33) | 5 | 34 (21–48) | 3 | 28 (20–36) | 3 | 36 (10–63) | ||||
| Quality rating | 0.440 | 0.356 | 0.314 | 0.307 | ||||||||
| Medium (< 7) | 11 | 28 (19–37) | 8 | 29 (15–44) | 7 | 27 (15–40) | 5 | 55 (18–90) | ||||
| High (≥ 7) | 35 | 23 (19–27) | 6 | 21 (13–30) | 3 | 18 (12–24) | 7 | 34 (20–50) | ||||
* p value obtained from univariate meta-regression. In bold, significant associations.
The exclusion of studies one-by-one from the analysis did not substantially change the overall prevalence rate of depression. Thus, no single study had a disproportional impact on the overall prevalence (data not shown).
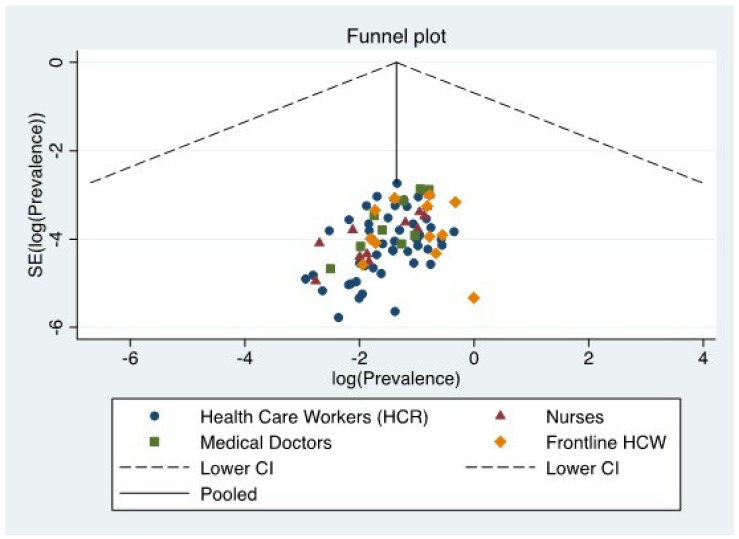
Visual inspection of the funnel plot (Figure 6) suggested a small publication bias for the prevalence estimate in HWC, nurses, and medical doctors, confirmed by significant results in the Egger’s test (p < 0.05). However, no publication bias was detected for frontline HCW (Egger’s test: p = 0.928).
Figure 6.
Funnel plot for the prevalence of depression.
4. Discussion
The present systematic review and meta-analysis identified a total of 57 cross-sectional studies reporting rates of depression among HCW. The pooled prevalence rate of depression in HCW was 24%, and when analyzing professional groups, we found that the rates were similar in nurses (25%) and medical doctors (24%), whereas up to 43% of frontline HCW report depression. The overall prevalence of depression found in HCW, nurses and medical doctors is similar to that found in a recent meta-analysis conducted from January 2020 to May 2020. This meta-analysis was based on 12 population-based studies conducted during the COVID-19 outbreak, finding that the overall prevalence was 25% in the general population [81].
Since the outbreak of COVID-19 pandemic in January 2020, the attention paid to the impact on mental health among HCW has grown exponentially, as indicated by the large number of studies found. A recent systematic review and meta-analysis of the prevalence of depression, anxiety, and insomnia among HCW during the pandemic included thirteen studies published up to 17 April 2020. In that study, the pooled prevalence of depression was 22.8%, based on ten studies [14]. A subgroup analysis for different occupational categories found that the pooled prevalence for nurses was 30.3% and for medical doctors 25.9%. These figures are slightly higher than those reported in our meta-analysis. These discrepancies might be explained by the different number of studies included. In the Pappa et al. meta-analysis, only five studies were considered in calculating separate pooled prevalence of depression for nurses and doctors, whereas our study was based on 14 and 10 studies to calculate prevalence depression in nurses and doctors, respectively. Another remarkable difference between the two meta-analyses is the origin of the samples, with the Pappa et al. study mainly focused on a Chinese population. However, our meta-analysis includes a broad range of countries from very different regions worldwide. This regional heterogeneity, along with a greater sample size, allows us to provide an updated estimation of the pooled prevalence of depression among HCW.
Our pooled prevalence of depression found in HCW (25%) is also higher compared with another systematic review and meta-analysis based on samples of HCW that reported a prevalence of 12.2% [15]. The study was conducted April–May 2020 and was based on seven cross-sectional studies, all of them conducted in China. Again, the diversity of the origin of the samples and/or the number of studies included might explain these discrepancies.
Note that all the studies included in our meta-analysis used self-reported standardized questionnaires to assess depressive symptomatology. Additionally, the use of a great variety of scales might have led to differences in the estimation of the presence of depression. In fact, our results show that those studies using the DASS-21 questionnaire reported lower prevalence rates of depression. Despite the convenience of using the same instruments and the inclusion of a diagnosis based on clinical interviews, this is not always possible in epidemiological studies.
Similarly, Muller et al. [82] conducted a rapid systematic review in May 2020 focusing on several outcomes such as mental health problems and risk or resilience factors from quantitative and qualitative data. They found a total of 19 studies, with a percentage of depression ranging from 5% to 51%, and a median of 21%. According to their systematic review, the most common risk factors for mental health problems in HCW were being a woman, being exposed to infected patients, and the worry of being infected.
An important contribution of the present meta-analysis is the calculation of the pooled prevalence of depression in frontline HCW. The prevalence is significantly higher (43%) compared with other types of HCW. The mental toll of working at the frontline during previous pandemic outbreaks, such as that of severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS), has previously been reported to be high [83,84]. The fear of being infected, stigmatization and uncertainty put these workers under extraordinary stress. A qualitative study conducted among frontline HCW in Wuhan (China) pointed up the intensive work (i.e., long working hours and use of personal protective equipment), fear of infecting others or being infected, managing relationships under stressful situations, and feeling powerless to handle patients’ conditions as common experiences during the COVID-19 outbreak [85].
However, factors contributing to increased vulnerability to depression among HCW as well as resilience characteristics (such as coping strategies) might be culturally different. Additionally, inequalities related to health systems and resources across high- and low-income countries might also contribute to the differing impact of COVID-19 on mental health among HCW from diverse settings. Furthermore, note that the first wave of COVID-19 was characterized by a high degree of uncertainty about the illness, its treatment, and its prognosis. Since the outbreak, there has been an intensive international response to fight the virus along with a research agenda aimed at finding effective treatments for infected patients and preventing the spread of the virus (e.g., vaccines). This means that COVID-19 is a rapid, evolving health challenge that requires up-to-date data to ensure appropriate surveillance of mental health, and specifically for vulnerable subpopulations such as HCW.
There are limitations to be considered when interpreting our results. First, the majority of studies included in the present meta-analysis used convenience samples, so representativeness of HCW might be jeopardized. Second, depression was mainly assessed by means of self-reported data drawn from questionnaires, which might have introduced biases such as social desirability [86], as well as being less accurate than clinical interviews. Third, the inclusion of cross-sectional studies makes it difficult to determine causal associations between the pandemic and depression. Fourth, some of the studies included in the calculation of the pooled prevalence for the three groups of HCW (i.e., nurses, medical doctors, and frontline HCW) might have also been included in the calculation of the pooled prevalence for HCW. Thus, caution should be taken when interpreting our results. Fifth, our systematic review was only conducted in a medical database (MEDLINE); thus, some articles, especially those related to psychology, might not be included. Finally, we found some sources of heterogeneity. For example, using convenience sampling methods, conducting studies in China, and using the DASS-21 questionnaire were associated with lower prevalence rates of depression. Related to this, half of the studies were carried out with Chinese samples, so the results of the present meta-analysis should be approached with caution. Future studies should endeavor to investigate the prevalence of depression among HCW in other countries, and use randomized sampling designs whenever possible, as well as longitudinal designs to determine the evolution of mental health problems in this population.
In summary, our meta-analysis shows that depression during the COVID-19 pandemic is a common mental condition among HCW, with the frontline HCW especially affected. A unified response to help HCW during the pandemic should be placed in the international agenda. Comprehensive psychological support, along with regular and intensive training for HCW, can help safeguard their well-being [87]. Common mental problems, such as depression, should be routinely assessed to detect those HCW at high risk of mental disorders and in need of intensive interventions to alleviate their symptomatology.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/jcm10153406/s1, Table S1: PRISMA checklist, Table S2: Search strategy in MEDLINE via Pubmed, Table S3: Quality assessment with the JBI Appraisal Checklist for Prevalence Studies.
Author Contributions
Conceptualization, B.O., J.B.-N., and J.S.; methodology, M.P.-M., J.B.-N., P.G.-G., and I.L.; software, J.S.; validation, B.O., J.B.-N., P.G.-G., and J.S.; formal analysis, J.S.; resources, J.S.; data curation, M.P.-M. and J.B.-N.; writing—original draft preparation, B.O., M.P.-M., J.B.-N., and P.G.-G.; writing—review and editing, B.O., J.B.-N., and J.S.; visualization, I.L. and J.S.; supervision, I.L. and J.S.; project administration, B.O. and J.S.; funding acquisition, B.O. All authors have read and agreed to the published version of the manuscript.
Funding
B.O. was supported by the Miguel Servet (CP20/00040) contract, funded by the Instituto de Salud Carlos III and co-funded by the European Union (ERDF/ESF, “Investing in your future”).
Institutional Review Board Statement
No institutional approval was necessary for this study.
Informed Consent Statement
Not applicable to this study.
Data Availability Statement
Data sharing is not applicable to this article as no new data were created or analyzed in it.
Conflicts of Interest
We declare that P.G.-G. has received grant support from Janssen, AstraZeneca and the Ilustre Colegio de Médicos de Zaragoza; she has received honoraria from AstraZeneca and Lilly; and she has received travel support from Lilly, Almirall, Lundbeck, Rovi, Pfizer and Janssen-Cilag. None of these activities was related to the current project. The remaining authors declare no conflicts of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Lu H., Stratton C.W., Tang Y.W. Outbreak of pneumonia of unknown etiology in Wuhan, China: The mystery and the miracle. J. Med. Virol. 2020;92:401–402. doi: 10.1002/jmv.25678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization (WHO) Director-General’s Opening Remarks at the Media Briefing on COVID-19. [(accessed on 12 December 2020)]; Available online: https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020#.XqySGbWV4O4.mailto.
- 3.World Health Organization (WHO) COVID-19 Weekly Epidemiological Update. World Health Organization (WHO); Geneva, Switzerland: 2020. [Google Scholar]
- 4.Campion J., Javed A., Sartorius N., Marmot M. Addressing the public mental health challenge of COVID-19. Lancet Psychiatry. 2020;7:657–659. doi: 10.1016/S2215-0366(20)30240-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nguyen L.H., Drew D.A., Graham M.S., Joshi A.D., Guo C.G., Ma W., Mehta R.S., Warner E.T., Sikavi D.R., Lo C.H., et al. Risk of COVID-19 among front-line health-care workers and the general community: A prospective cohort study. Lancet Public Health. 2020;5:e475–e483. doi: 10.1016/S2468-2667(20)30164-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhang C., Yang L., Liu S., Ma S., Wang Y., Cai Z., Du H., Li R., Kang L., Su M., et al. Survey of Insomnia and Related Social Psychological Factors Among Medical Staff Involved in the 2019 Novel Coronavirus Disease Outbreak. Front. Psychiatry. 2020;11:306. doi: 10.2139/ssrn.3542175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rana W., Mukhtar S., Mukhtar S. Mental health of medical workers in Pakistan during the pandemic COVID-19 outbreak. Asian J. Psychiatry. 2020;51:102080. doi: 10.1016/j.ajp.2020.102080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Spoorthy M.S. Mental health problems faced by healthcare workers due to the COVID-19 pandemic—A review. Asian J. Psychiatry. 2020;51:102119. doi: 10.1016/j.ajp.2020.102119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Grover S., Sahoo S., Mehra A., Avasthi A., Tripathi A., Subramanyan A., Pattojoshi A., Rao G., Saha G., Mishra K., et al. Psychological impact of COVID-19 lockdown: An online survey from India. Indian J. Psychiatry. 2020;62:354. doi: 10.4103/psychiatry.indianjpsychiatry_427_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhang W.R., Wang K., Yin L., Zhao W.F., Xue Q., Peng M., Min B.Q., Tian Q., Leng H.X., Du J.L., et al. Mental Health and Psychosocial Problems of Medical Health Workers during the COVID-19 Epidemic in China. Psychother. Psychosomat. 2020;89:242–250. doi: 10.1159/000507639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shigemura J., Ursano R.J., Morganstein J.C., Kurosawa M., Benedek D.M. Public responses to the novel 2019 coronavirus (2019-nCoV) in Japan: Mental health consequences and target populations. Psychiatry Clin. Neurosci. 2020;74:281–282. doi: 10.1111/pcn.12988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lu W., Wang H., Lin Y., Li L. Psychological status of medical workforce during the COVID-19 pandemic: A cross-sectional study. Psychiatry Res. 2020;288:112936. doi: 10.1016/j.psychres.2020.112936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Liu Y., Wang L., Chen L., Zhang X., Bao L., Shi Y. Mental Health Status of Paediatric Medical Workers in China During the COVID-19 Outbreak. Front. Psychiatry. 2020;11:702. doi: 10.3389/fpsyt.2020.00702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pappa S., Ntella V., Giannakas T., Giannakoulis V.G., Papoutsi E., Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain Behav. Immun. 2020;88:901–907. doi: 10.1016/j.bbi.2020.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Da Silva F.C.T., Neto M.L.R. Psychological effects caused by the COVID-19 pandemic in health professionals: A systematic review with meta-analysis. Prog. Neuro Psychopharmacol. Biol. Psychiatry. 2021;104:110062. doi: 10.1016/j.pnpbp.2020.110057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Moher D., Liberati A., Tetzlaff J., Altman D.G., Altman D., Antes G., Atkins D., Barbour V., Barrowman N., Berlin J.A., et al. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009;6:e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Moola S., Munn Z., Tufanaru C., Aromataris E., Sears K., Sfetc R., Currie M., Lisy K., Qureshi R., Mattis P., et al. Chapter 7: Systematic reviews of etiology and risk. In: Aromataris E., Munn Z., editors. Joanna Briggs Institute Reviewer’s Manual. The Joanna Briggs Institute; Adelaide, Australia: 2017. pp. 219–226. [Google Scholar]
- 18.DerSimonian R., Laird N. Meta-analysis in clinical trials. Control. Clin. Trials. 1986;7:177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 19.Von Hippel P.T. The heterogeneity statistic I(2) can be biased in small meta-analyses. BMC Med. Res. Methodol. 2015;15:35. doi: 10.1186/s12874-015-0024-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Higgins J.P.T., Thompson S.G., Deeks J.J., Altman D.G. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Thompson S.G., Higgins J.P.T. How should meta-regression analyses be undertaken and interpreted? Stat. Med. 2002;21:1559–1573. doi: 10.1002/sim.1187. [DOI] [PubMed] [Google Scholar]
- 22.Egger M., Schneider M., Smith G.D. Meta-analysis Spurious precision? Meta-analysis of observational studies. BMJ. 1998;316:140–144. doi: 10.1136/bmj.316.7125.140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hunter J.P., Saratzis A., Sutton A.J., Boucher R.H., Sayers R.D., Bown M.J. In meta-analyses of proportion studies, funnel plots were found to be an inaccurate method of assessing publication bias. J. Clin. Epidemiol. 2014;67:897–903. doi: 10.1016/j.jclinepi.2014.03.003. [DOI] [PubMed] [Google Scholar]
- 24.Egger M., Smith G.D., Schneider M., Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Begg C.B., Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50:1088–1101. doi: 10.2307/2533446. [DOI] [PubMed] [Google Scholar]
- 26.R Development Core Team . R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing; Vienna, Austria: 2019. [Google Scholar]
- 27.Di Tella M., Romeo A., Benfante A., Castelli L. Mental health of healthcare workers during the COVID-19 pandemic in Italy. J. Eval. Clin. Pract. 2020;26:1583–1587. doi: 10.1111/jep.13444. [DOI] [PubMed] [Google Scholar]
- 28.Dosil Santamaría M., Ozamiz-Etxebarria N., Redondo Rodríguez I., Jaureguizar Alboniga-Mayor J., Picaza Gorrotxategi M. Psychological impact of COVID-19 on a sample of Spanish health professionals. Rev. Psiquiatr. Salud Ment. 2020 doi: 10.1016/j.rpsm.2020.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Elbay R.Y., Kurtulmuş A., Arpacıoğlu S., Karadere E. Depression, anxiety, stress levels of physicians and associated factors in Covid-19 pandemics. Psychiatry Res. 2020;290:113130. doi: 10.1016/j.psychres.2020.113130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Elhadi M., Msherghi A., Elgzairi M., Alhashimi A., Bouhuwaish A., Biala M., Abuelmeda S., Khel S., Khaled A., Alsoufi A., et al. Psychological status of healthcare workers during the civil war and COVID-19 pandemic: A cross-sectional study. J. Psychosomat. Res. 2020;137:110221. doi: 10.1016/j.jpsychores.2020.110221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gallopeni F., Bajraktari I., Selmani E., Tahirbegolli I.A., Sahiti G., Muastafa A., Bojaj G., Muharremi V.B., Tahirbegolli B. Anxiety and depressive symptoms among healthcare professionals during the Covid-19 pandemic in Kosovo: A cross sectional study. J. Psychosomat. Res. 2020;137:110212. doi: 10.1016/j.jpsychores.2020.110212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gupta A.K., Mehra A., Niraula A., Kafle K., Deo S.P., Singh B., Sahoo S., Grover S. Prevalence of anxiety and depression among the healthcare workers in Nepal during the COVID-19 pandemic. Asian J. Psychiatry. 2020;54:102260. doi: 10.1016/j.ajp.2020.102260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gupta S., Prasad A.S., Dixit P.K., Padmakumari P., Gupta S., Abhisheka K. Survey of prevalence of anxiety and depressive symptoms among 1124 healthcare workers during the coronavirus disease 2019 pandemic across India. Med. J. Armed Forces India. 2020;77:S404–S412. doi: 10.1016/j.mjafi.2020.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Huang Y., Zhao N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: A web-based cross-sectional survey. Psychiatry Res. 2020;288:112954. doi: 10.1016/j.psychres.2020.112954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kannampallil T.G., Goss C.W., Evanoff B.A., Strickland J.R., McAlister R.P., Duncan J. Exposure to COVID-19 patients increases physician trainee stress and burnout. PLoS ONE. 2020;15:e0237301. doi: 10.1371/journal.pone.0237301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Keubo F.R.N., Mboua P.C., Tadongfack T.D., Tchoffo E.F., Tatang C.T., Zeuna J.I., Noupoue E.M., Tsoplifack C.B., Folefack G.O. Annales Medico-Psychologiques, Revue Psychiatrique. Volume 179. Elsevier Masson; Hoboken, NJ, USA: 2020. Psychological distress among health care professionals of the three COVID-19 most affected Regions in Cameroon: Prevalence and associated factors; pp. 141–146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Khanna R.C., Honavar S.G., Metla A.L., Bhattacharya A., Maulik P.K. Psychological impact of COVID-19 on ophthalmologists-in-training and practising ophthalmologists in India. Indian J. Ophthalmol. 2020;68:994–998. doi: 10.4103/ijo.IJO_1458_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Koksal E., Dost B., Terzi Ö., Ustun Y.B., Özdin S., Bilgin S. Evaluation of Depression and Anxiety Levels and Related Factors Among Operating Theater Workers During the Novel Coronavirus (COVID-19) Pandemic. J. Perianesth. Nurs. Off. J. Am. Soc. PeriAnesth. Nurses. 2020;35:472–477. doi: 10.1016/j.jopan.2020.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Krammer S., Augstburger R., Haeck M., Maercker A. Adjustment Disorder, Depression, Stress Symptoms, Corona Related Anxieties and Coping Strategies during the Corona Pandemic (COVID-19) in Swiss Medical Staff. Psychother. Psychosomat. Med. Psychol. 2020;70:272–282. doi: 10.1055/a-1192-6608. [DOI] [PubMed] [Google Scholar]
- 40.Lai J., Ma S., Wang Y., Cai Z., Hu J., Wei N., Wu J., Du H., Chen T., Li R., et al. Factors Associated With Mental Health Outcomes Among Health Care Workers Exposed to Coronavirus Disease 2019. JAMA Netw. Open. 2020;3:e203976. doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lam S.C., Arora T., Grey I., Suen L.K.P., Huang E.Y.-Z., Li D., Lam K.B.H. Perceived Risk and Protection From Infection and Depressive Symptoms Among Healthcare Workers in Mainland China and Hong Kong During COVID-19. Front. Psychiatry. 2020;11:686. doi: 10.3389/fpsyt.2020.00686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Li G., Miao J., Wang H., Xu S., Sun W., Fan Y., Zhang C., Zhu S., Zhu Z., Wang W. Psychological impact on women health workers involved in COVID-19 outbreak in Wuhan: A cross-sectional study. J. Neurol. Neurosurg. Psychiatry. 2020;91:895–897. doi: 10.1136/jnnp-2020-323134. [DOI] [PubMed] [Google Scholar]
- 43.Liang Y., Wu K., Zhou Y., Huang X., Zhou Y., Liu Z. Mental Health in Frontline Medical Workers during the 2019 Novel Coronavirus Disease Epidemic in China: A Comparison with the General Population. Int. J. Environ. Res. Public Health. 2020;17:6550. doi: 10.3390/ijerph17186550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lin K., Yang B.X., Luo D., Liu Q., Ma S., Huang R., Lu W., Majeed A., Lee Y., Lui L.M.W., et al. The Mental Health Effects of COVID-19 on Health Care Providers in China. Am. J. Psychiatry. 2020;177:635–636. doi: 10.1176/appi.ajp.2020.20040374. [DOI] [PubMed] [Google Scholar]
- 45.Luceño-Moreno L., Talavera-Velasco B., García-Albuerne Y., Martín-García J. Symptoms of Posttraumatic Stress, Anxiety, Depression, Levels of Resilience and Burnout in Spanish Health Personnel during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health. 2020;17:5514. doi: 10.3390/ijerph17155514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Magnavita N., Tripepi G., Di Prinzio R.R. Symptoms in Health Care Workers during the COVID-19 Epidemic. A Cross-Sectional Survey. Int. J. Environ. Res. Public Health. 2020;17:5218. doi: 10.3390/ijerph17145218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Almater A., Tobaigy M., Younis A., Alaqeel M., Abouammoh M. Effect of 2019 coronavirus pandemic on ophthalmologists practicing in Saudi Arabia: A psychological health assessment. Middle East Afr. J. Ophthalmol. 2020;27:79–85. doi: 10.4103/meajo.MEAJO_220_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Naser A.Y., Dahmash E.Z., Al-Rousan R., Alwafi H., Alrawashdeh H.M., Ghoul I., Abidine A., Bokhary M.A., Al-Hadithi H.T., Ali D., et al. Mental health status of the general population, healthcare professionals, and university students during 2019 coronavirus disease outbreak in Jordan: A cross-sectional study. Brain Behav. 2020;10:e01730. doi: 10.1002/brb3.1730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ning X., Yu F., Huang Q., Li X., Luo Y., Huang Q., Chen C. The mental health of neurological doctors and nurses in Hunan Province, China during the initial stages of the COVID-19 outbreak. BMC Psychiatry. 2020;20:436. doi: 10.1186/s12888-020-02838-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Pouralizadeh M., Bostani Z., Maroufizadeh S., Ghanbari A., Khoshbakht M., Alavi S.A., Ashrafi S. Anxiety and depression and the related factors in nurses of Guilan University of Medical Sciences hospitals during COVID-19: A web-based cross-sectional study. Int. J. Afr. Nurs. Sci. 2020;13:100233. doi: 10.1016/j.ijans.2020.100233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Que J., Shi L., Deng J., Liu J., Zhang L., Wu S., Gong Y., Huang W., Yuan K., Yan W., et al. Psychological impact of the COVID-19 pandemic on healthcare workers: A cross-sectional study in China. Gen. Psychiatry. 2020;33:e100259. doi: 10.1136/gpsych-2020-100259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Şahin M.K., Aker S., Şahin G., Karabekiroğlu A. Prevalence of Depression, Anxiety, Distress and Insomnia and Related Factors in Healthcare Workers During COVID-19 Pandemic in Turkey. J. Community Health. 2020;45:1168–1177. doi: 10.1007/s10900-020-00921-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Salopek-Žiha D., Hlavati M., Gvozdanović Z., Gašić M., Placento H., Jakić H., Klapan D., Šimić H. Differences in Distress and Coping with the COVID-19 Stressor in Nurses and Physicians. Psychiatr. Danub. 2020;32:287–293. doi: 10.24869/psyd.2020.287. [DOI] [PubMed] [Google Scholar]
- 54.Sandesh R., Shahid W., Dev K., Mandhan N., Shankar P., Shaikh A., Rizwan A. Impact of COVID-19 on the Mental Health of Healthcare Professionals in Pakistan. Cureus. 2020;12:e8974. doi: 10.7759/cureus.8974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Si M.Y., Su X.Y., Jiang Y., Wang W.J., Gu X.F., Ma L., Li J., Zhang S.K., Ren Z.F., Ren R., et al. Psychological impact of COVID-19 on medical care workers in China. Infect. Dis. Poverty. 2020;9:113. doi: 10.1186/s40249-020-00724-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Song X., Fu W., Liu X., Luo Z., Wang R., Zhou N., Yan S., Lv C. Mental health status of medical staff in emergency departments during the Coronavirus disease 2019 epidemic in China. Brain Behav. Immun. 2020;88:60–65. doi: 10.1016/j.bbi.2020.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Stojanov J., Malobabic M., Stanojevic G., Stevic M., Milosevic V., Stojanov A. Quality of sleep and health-related quality of life among health care professionals treating patients with coronavirus disease-19. Int. J. Soc. Psychiatry. 2020;67:175. doi: 10.1177/0020764020942800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.An Y., Yang Y., Wang A., Li Y., Zhang Q., Cheung T., Ungvari G.S., Qin M.-Z., An F.-R., Xiang Y.-T. Prevalence of depression and its impact on quality of life among frontline nurses in emergency departments during the COVID-19 outbreak. J. Affect. Disord. 2020;276:312–315. doi: 10.1016/j.jad.2020.06.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Suryavanshi N., Kadam A., Dhumal G., Nimkar S., Mave V., Gupta A., Cox S.R., Gupte N. Mental health and quality of life among healthcare professionals during the COVID-19 pandemic in India. Brain Behav. 2020;10:e01837. doi: 10.1002/brb3.1837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Teng Z., Huang J., Qiu Y., Tan Y., Zhong Q., Tang H., Wu H., Wu Y., Chen J. Mental health of front-line staff in prevention of coronavirus disease 2019. Zhong Nan Da Xue Xue Bao Yi Xue Ban J. Cent. South Univ. Med. Sci. 2020;45:613–619. doi: 10.11817/j.issn.1672-7347.2020.200241. [DOI] [PubMed] [Google Scholar]
- 61.Teo W.Z.Y., Soo Y.E., Yip C., Lizhen O., Chun-Tsu L. The psychological impact of COVID-19 on “hidden” frontline healthcare workers. Int. J. Soc. Psychiatry. 2020:284–289. doi: 10.1177/0020764020950772. [DOI] [PubMed] [Google Scholar]
- 62.Tu Z.H., He J.W., Zhou N. Sleep quality and mood symptoms in conscripted frontline nurse in Wuhan, China during COVID-19 outbreak: A cross-sectional study. Medicine. 2020;99:e20769. doi: 10.1097/MD.0000000000020769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Vanni G., Materazzo M., Santori F., Pellicciaro M., Costesta M., Orsaria P., Cattadori F., Pistolese C.A., Perretta T., Chiocchi M., et al. The Effect of Coronavirus (COVID-19) on Breast Cancer Teamwork: A Multicentric Survey. In Vivo. 2020;34:1685–1694. doi: 10.21873/invivo.11962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Wang H., Huang D., Huang H., Zhang J., Guo L., Liu Y., Ma H., Geng Q. The psychological impact of COVID-19 pandemic on medical staff in Guangdong, China: A cross-sectional study. Psychol. Med. 2020:1–9. doi: 10.1017/S0033291720002561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Wang L.Q., Zhang M., Liu G.M., Nan S.Y., Li T., Xu L., Xue Y., Wang L., Qu Y.D., Liu F. Psychological impact of coronavirus disease (2019) (COVID-19) epidemic on medical staff in different posts in China: A multicenter study. J. Psychiatr. Res. 2020;129:198–205. doi: 10.1016/j.jpsychires.2020.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Wang S., Xie L., Xu Y., Yu S., Yao B., Xiang D. Sleep disturbances among medical workers during the outbreak of COVID-2019. Occup. Med. 2020;70:364–369. doi: 10.1093/occmed/kqaa074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Wang W., Song W., Xia Z., He Y., Tang L., Hou J., Lei S. Sleep Disturbance and Psychological Profiles of Medical Staff and Non-Medical Staff During the Early Outbreak of COVID-19 in Hubei Province, China. Front. Psychiatry. 2020;11:733. doi: 10.3389/fpsyt.2020.00733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Wańkowicz P., Szylińska A., Rotter I. Assessment of Mental Health Factors among Health Professionals Depending on Their Contact with COVID-19 Patients. Int. J. Environ. Res. Public Health. 2020;17:5849. doi: 10.3390/ijerph17165849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Cai Q., Feng H., Huang J., Wang M., Wang Q., Lu X., Xie Y., Wang X., Liu Z., Hou B., et al. The mental health of frontline and non-frontline medical workers during the coronavirus disease 2019 (COVID-19) outbreak in China: A case-control study. J. Affect. Disord. 2020;275:210–215. doi: 10.1016/j.jad.2020.06.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Xiao X., Zhu X., Fu S., Hu Y., Li X., Xiao J. Psychological impact of healthcare workers in China during COVID-19 pneumonia epidemic: A multi-center cross-sectional survey investigation. J. Affect. Disord. 2020;274:405–410. doi: 10.1016/j.jad.2020.05.081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Xiaoming X., Ming A., Su H., Wo W., Jianmei C., Qi Z., Hua H., Xuemei L., Lixia W., Jun C., et al. The psychological status of 8817 hospital workers during COVID-19 Epidemic: A cross-sectional study in Chongqing. J. Affect. Disord. 2020;276:555–561. doi: 10.1016/j.jad.2020.07.092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Xiong H., Yi S., Lin Y. The Psychological Status and Self-Efficacy of Nurses During COVID-19 Outbreak: A Cross-Sectional Survey. Inquiry. 2020;57:46958020957114. doi: 10.1177/0046958020957114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Yang S., Kwak S.G., Ko E.J., Chang M.C. The Mental Health Burden of the COVID-19 Pandemic on Physical Therapists. Int. J. Environ. Res. Public Health. 2020;17:3723. doi: 10.3390/ijerph17103723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Zhou Y., Wang W., Sun Y., Qian W., Liu Z., Wang R., Qi L., Yang J., Song X., Zhou X., et al. The prevalence and risk factors of psychological disturbances of frontline medical staff in china under the COVID-19 epidemic: Workload should be concerned. J. Affect. Disord. 2020;277:510–514. doi: 10.1016/j.jad.2020.08.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Zhu J., Sun L., Zhang L., Wang H., Fan A., Yang B., Li W., Xiao S. Prevalence and Influencing Factors of Anxiety and Depression Symptoms in the First-Line Medical Staff Fighting Against COVID-19 in Gansu. Front. Psychiatry. 2020;11:386. doi: 10.3389/fpsyt.2020.00386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Zhu Z., Xu S., Wang H., Liu Z., Wu J., Li G., Miao J., Zhang C., Yang Y., Sun W., et al. COVID-19 in Wuhan: Sociodemographic characteristics and hospital support measures associated with the immediate psychological impact on healthcare workers. EClinicalMedicine. 2020;24:100443. doi: 10.1016/j.eclinm.2020.100443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Chen J., Liu X., Wang D., Jin Y., He M., Ma Y., Zhao X., Song S., Zhang L., Xiang X., et al. Risk factors for depression and anxiety in healthcare workers deployed during the COVID-19 outbreak in China. Soc. Psychiatry Psychiatr. Epidemiol. 2020;56:47–55. doi: 10.1007/s00127-020-01954-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Chen Y., Zhou H., Zhou Y., Zhou F. Prevalence of self-reported depression and anxiety among pediatric medical staff members during the COVID-19 outbreak in Guiyang, China. Psychiatry Res. 2020;288:113005. doi: 10.1016/j.psychres.2020.113005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Chew N.W.S., Lee G.K.H., Tan B.Y.Q., Jing M., Goh Y., Ngiam N.J.H., Yeo L.L.L., Ahmad A., Ahmed Khan F., Napolean Shanmugam G., et al. A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain. Behav. Immun. 2020;88:559–565. doi: 10.1016/j.bbi.2020.04.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Dal’Bosco E.B., Messias Floriano L.S., Skupien S.V., Arcaro G., Martins A.R., Correa Anselmo A.C. Mental health of nursing in coping with COVID-19 at a regional university hospital. Rev. Bras. Enferm. 2020;73 doi: 10.1590/0034-7167-2020-0434. [DOI] [PubMed] [Google Scholar]
- 81.Bueno-Notivol J., Gracia-García P., Olaya B., Lasheras I., López-Antón R., Santabárbara J. Prevalence of depression during the COVID-19 outbreak: A meta-analysis of community-based studies. Int. J. Clin. Health Psychol. 2020:21–100196. doi: 10.1016/j.ijchp.2020.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Muller A.E., Hafstad E.V., Himmels J.P.W., Smedslund G., Flottorp S., Stensland S., Stroobants S., Van de Velde S., Vist G.E. The mental health impact of the covid-19 pandemic on healthcare workers, and interventions to help them: A rapid systematic review. medRxiv. 2020 doi: 10.1016/j.psychres.2020.113441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Wu P., Fang Y., Guan Z., Fan B., Kong J., Yao Z., Liu X., Fuller C.J., Susser E., Lu J., et al. The psychological impact of the SARS epidemic on hospital employees in China: Exposure, risk perception, and altruistic acceptance of risk. Can. J. Psychiatry. 2009;54:302–311. doi: 10.1177/070674370905400504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Lee S.M., Kang W.S., Cho A.R., Kim T., Park J.K. Psychological impact of the 2015 MERS outbreak on hospital workers and quarantined hemodialysis patients. Compr. Psychiatry. 2018;87:123–127. doi: 10.1016/j.comppsych.2018.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Liu Q., Luo D., Haase J.E., Guo Q., Wang X.Q., Liu S., Xia L., Liu Z., Yang J., Yang B.X. The experiences of health-care providers during the COVID-19 crisis in China: A qualitative study. Lancet Glob. Health. 2020;8:e790–e798. doi: 10.1016/S2214-109X(20)30204-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Ahmed M.Z., Ahmed O., Aibao Z., Hanbin S., Siyu L., Ahmad A. Epidemic of COVID-19 in China and associated Psychological Problems. Asian J. Psychiatry. 2020;51:102092. doi: 10.1016/j.ajp.2020.102092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Tomlin J., Dalgleish-Warburton B., Lamph G. Psychosocial Support for Healthcare Workers During the COVID-19 Pandemic. Front. Psychol. 2020;11:1960. doi: 10.3389/fpsyg.2020.01960. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data sharing is not applicable to this article as no new data were created or analyzed in it.