Abstract
As of February 2020, over 2800 cases of lung injury associated with vapes have been reported in all 50 states (Cullen et al., 2019) [1]. This case is about a 29-year-old female with a five-year history of vaping tetrahydrocannabinol (THC) who presented with symptoms consistent with e-cigarette, or vaping, product-use associated lung injury (EVALI). This case report is unique because this patient clinically improved on a lower dose of corticosteroids compared to other reported cases of EVALI. Additionally, this case report highlights the importance and difficulty of excluding other disease processes prior to treating patients for EVALI, particularly during the coronavirus disease 2019 (COVID-19) global pandemic.
Keywords: Tetrahydrocannabinol; THC; e-Cigarette, or vaping; Product-use associated lung injury; EVALI; Vaping; Vape; Corticosteroid; Treatment; Infection; Diagnosis of exclusion
Highlights
-
•
Patients with EVALI may experience resolution of their disease with a lower dose of systemic corticosteroids.
-
•
EVALI is a diagnosis of exclusion that requires a thorough infectious disease workup, which may hinder timely treatment.
-
•
While steroids have been used to treat EVALI, there are currently no evidence-based treatment guidelines for EVALI.
1. Background
Recreational electronic cigarettes (e-cigarettes), or vapes, have steadily gained popularity among teenagers and young adults [1]. Over 27% of high school and 10% of middle school students reported current e-cigarette use in 2019 [1]. E-cigarettes typically contain nicotine, flavorings, and other substances such as tetrahydrocannabinol (THC) [2]. E-cigarette, or vaping, product-use associated lung injury (EVALI) is an increasingly recognized syndrome which has been reported throughout the United States. During the initial 2019 outbreak of this disease, 76.9% of patients reported using THC-containing products while 56.8% reported using nicotine-containing products, suggesting an increased prevalence of the lung injury occurring in those vaping THC [3]. Patients who develop EVALI can present with dyspnea, fever, emesis, diarrhea, and cough with symptoms rapidly improving after vaping cessation and corticosteroid administration [4]. Currently, the Centers for Disease Control and Prevention report that corticosteroids may be helpful in treating EVALI; however, there are currently no evidence-based treatment guidelines for EVALI [5]. The current literature illustrates successful treatment of EVALI with high-dose corticosteroids regimens, to include intravenous (IV) methylprednisolone ranging from 120 mg to 500 mg daily [4,6,7]. Characteristic imaging findings for EVALI include basilar-predominant consolidation and ground-glass opacities, often with sub-pleural sparing [4]. This case report is unique in that not only did this patient develop symptoms two weeks after vaping cessation, but she also clinically improved on a lower dose of corticosteroids compared to that of other published cases. Additionally, this case highlights the importance of an expeditious infectious disease work-up and the difficult decision faced by clinicians who must use their clinical acumen to rule out infectious etiologies with pending laboratory results.
2. Case presentation
A 29-year-old female without significant past medical history presented to the emergency department (ED) with a one-week history of intermittent fevers up to 102.0 °F and a three-day history of watery, non-bloody bowel movements and non-bloody, non-bilious emesis. She was initially evaluated in the ED 3 days prior and was discharged home on oral amoxicillin with the diagnosis of pneumonitis. The month prior, the patient had completed a cross-country road trip from San Diego, California to Maryland with several day trips in Arizona and Utah. This patient vaped daily for 5 years, going through one canister of THC over 4–5 days with the last vaping episode being two weeks prior to the onset of symptoms. At admission, the patient met Systemic Inflammatory Response Syndrome (SIRS) criteria for sepsis with tachycardia, fever of 100.7 °F, and a white blood cell count of 12,700 cells/mm [3]. Initial chest x-ray on admission showed mild patchy alveolar opacities bilaterally in the basilar lung fields concerning for atypical pneumonitis, which also provided a source for the sepsis diagnosis (Fig. 1).
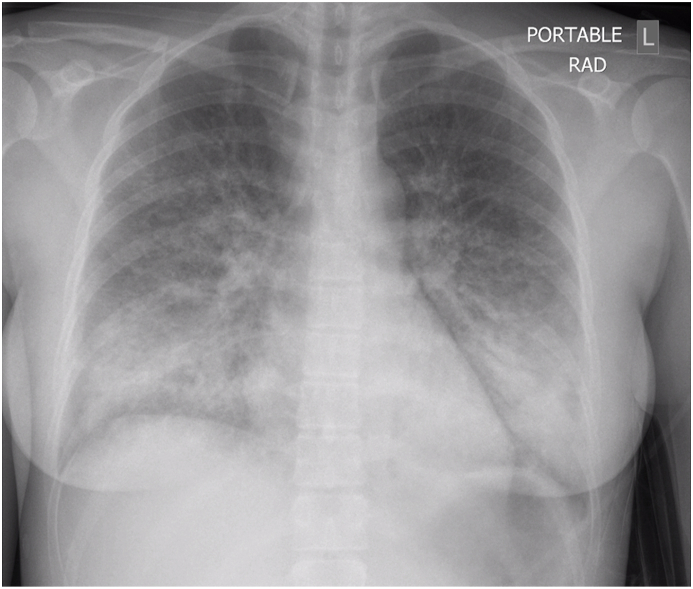
Fig. 1.

Anterior-posterior (AP) portable chest radiograph on admission showing mixed interstitial and alveolar infiltrates in the bilateral lower lungs. There are no localized consolidation or confluence noted.
Since the patient met SIRS criteria with opacities noted on her chest x-ray, an infectious work-up was started and treatment with IV ceftriaxone and azithromycin was initiated. A high-resolution computed tomography (CT) chest demonstrated bibasilar symmetric peripheral predominant septal interstitial thickening with subpleural sparing and traction bronchiectasis with additional areas of multifocal ground glass opacities. This finding broadened the differential diagnosis to include EVALI, infection, and autoimmune etiologies. A robust inpatient infectious and autoimmune work-up was conducted (Table 1). Two days later, patient developed a new 2 L per minute oxygen requirement. Repeat high resolution CT chest showed interval worsening of the patient's ground glass opacities in addition to moderate bibasilar pleural effusions concerning for a superimposed infectious process (Fig. 2).
Table 1.
Patient's laboratory work-up.
| Patient's Laboratory Work-up. | |
|---|---|
| Gomori methenamine silver stain | Coccidioides immitis/sp. antibody |
| 1, 3 Beta-D glucan | Legionella pneumophila urine antigen |
| Respiratory PCR | Streptococcus pneumonia antigen |
| Sputum culture | Leptospirosis IgM antibody |
| BAL gram stain & culture | Hantavirus immunoglobulins |
| BAL acid fast culture & PAS stain | Parvovirus B19 IgM antibody |
| BAL fungal culture & smears | Human Immunodeficiency Virus |
| Stool PCR | Acute hepatitis panel |
| Stool ova & parasites | ANA, IFA |
| Entamoeaba histolytica | Rheumatoid factor |
| Stool calprotectin & lactoferrin | GBM antibody |
| Blastomycosis dermatitidis antibody | ANCA panel |
PCR, polymerase chain reaction; BAL, bronchoalveolar lavage; PAS, periodic acid Schiff; IgM, immunoglobulin; ANA, antinuclear antibody; IFA, immunofluorescence assay; GBM, glomerular basement membrane; ANCA, anti-neutrophil cytoplasmic antibody.
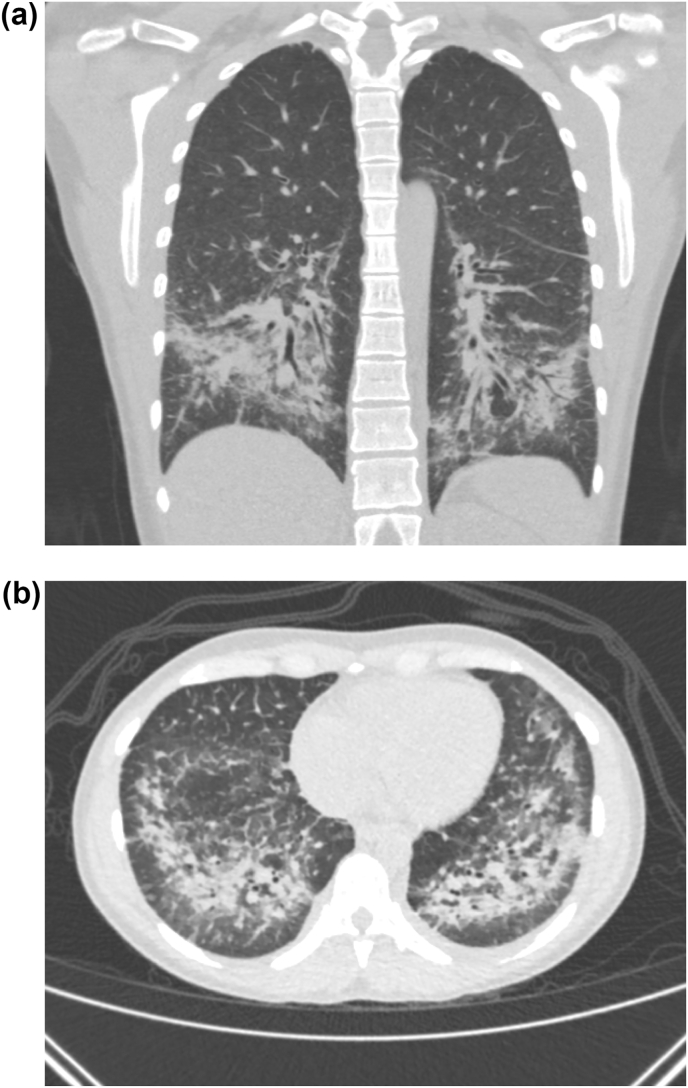
Fig. 2.
CT Chest High Resolution, coronal (2a) and axial (2b) view on hospital day 2. Interval worsening of bibasilar and peripherally predominant consolidations with associated interstitial thickening and bronchiectasis. Subpleural sparing and multiple subpleural nodules are seen within the upper lobes.
Bronchoscopy was then performed, grossly revealing mildly hyperemic tissue within the bronchi, but no focal lesions or secretions. Bronchoalveolar lavage (BAL) fluid analysis revealed alveolar macrophages and ciliated respiratory epithelial cells but no organisms on gram stain with negative bacterial and fungal cultures. Transbronchial biopsy was benign and suggestive of organizing pneumonia with a nonspecific differential, which is consistent with previously reported pathological findings of EVALI [8,9]. Despite empiric antibiotic coverage, the patient continued to clinically decline on day 3 of admission with worsening subjective dyspnea, increased work of breathing, and an increasing oxygen requirement. Repeat chest radiograph showed interval worsening of her bilateral basilar predominant patchy opacities with involvement of the right middle and upper lobes (Fig. 3).
Fig. 3.
AP chest radiograph on hospital day 3. Illustrates interval worsening of patchy lower lobe predominant opacities, now involving the mid-lungs bilaterally and right upper lung. Indistinctness of the pulmonary vasculature.
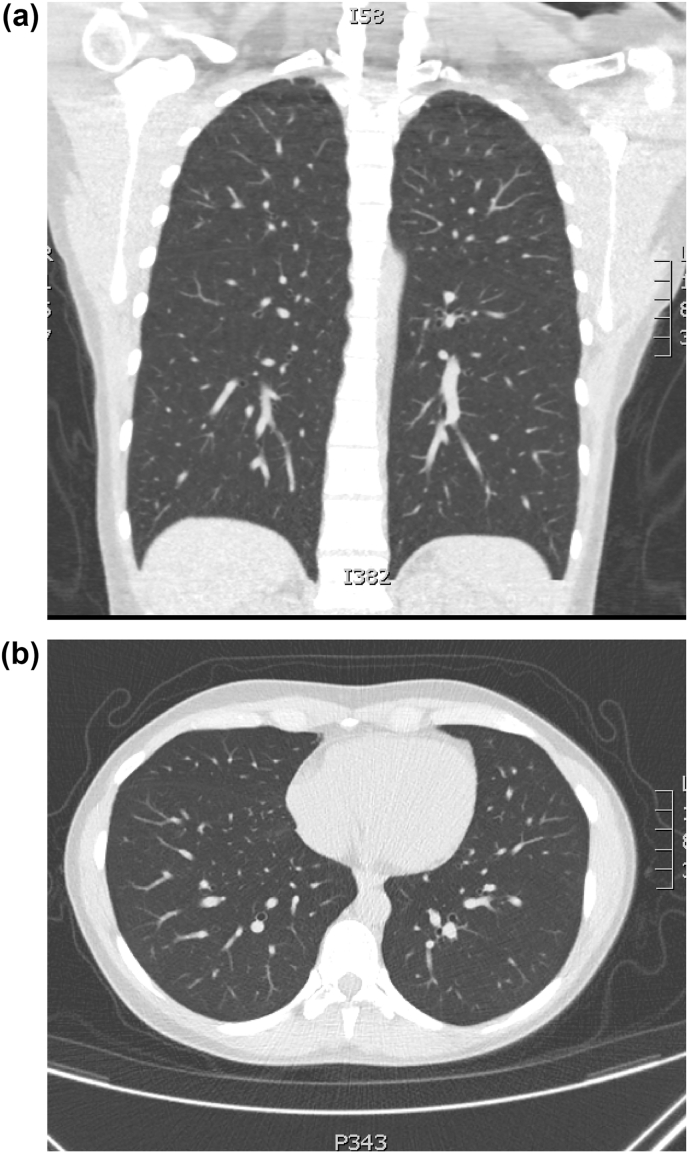
In the setting of her clinical decline while on IV antibiotics, negative results on numerous infectious labs (including a negative SARS-CoV-2 test), negative autoimmune serologies, and bronchial alveolar lavage findings inconsistent with an infectious etiology, the decision was made to discontinue antibiotics and treat the patient for presumptive EVALI. She was started on IV solumedrol 1 mg/kg/day (50 mg daily). Of note, most of her fungal lab results had not returned by the time corticosteroid therapy was initiated. The patient's symptoms improved drastically within 24 hours of initiating corticosteroids and she no longer required supplemental oxygen by day 5 of hospitalization. The patient received IV solumedrol 1mg/kg/day on days 3 through 5 and was then placed on an outpatient regimen of oral prednisone 40mg daily starting on day 6, the day of discharge. On the day of discharge, the patient received her influenza vaccination, was counseled on abstaining from vaping, and was advised to abide by Center for Disease Control's (CDC) coronavirus disease 2019 (COVID-19) guidelines to limit her risk of infection. The patient completed a rapid taper of prednisone of 20 mg daily for the first week then 10 mg daily the second week. She received a high-resolution CT chest one month following hospital discharge, which showed complete resolution of previous lung findings without evidence of resultant fibrotic changes (Fig. 4). Additionally, the patient had subjectively recovered to her baseline respiratory status. During her follow up appointment, the patient denied necessity for albuterol inhaler use and continues to abstain from vaping.
Fig. 4.
a and 4b: Coronal and axial CT chest images one month after hospital discharge.
3. Discussion
The mechanism of EVALI is poorly understood. One hypothesis is that inhaled inflammatory chemicals such as diacetyl and vitamin E lead to direct damage of the respiratory epithelium with cytotoxic effects on lung parenchyma [2]. Particularly, vitamin E inhalation from e-cigarettes is thought to promote acute lung injury via accumulation of this toxin in macrophages leading to cell death [2]. Blount et al.‘s case series further supports this theory after finding a strong correlation between the presence of vitamin E acetate in the BAL samples and EVALI [10]. However, since EVALI is a diagnosis of exclusion and vitamin E acetate testing was not readily available, vitamin E acetate levels were not measured in this patient's BAL.
In addition to a better understanding of EVALI's pathophysiology, there is also a need for consistent and clear guidelines for inpatient and outpatient treatment of EVALI. One case series reports using IV methylprednisolone 40mg every 8 hours and transitioning to a two week taper with oral prednisone once clinically improving [4]. A cohort study of 60 patients during the initial 2019 EVALI outbreak illustrates an initial IV methylprednisolone dose ranging 120–240 mg daily for 1–4 days before transitioning to 40–60 mg of oral prednisone daily [6]. Clinical improvement in 84% of these patient were attributed to steroids [6]. Another study showed clinical improvement after starting IV methylprednisolone 120–500 mg daily [7]. This patient's clinical course is notable for her symptomatic improvement after being started on a lower steroid dose of 50 mg (1 mg/kg) IV methylprednisolone daily with a two-week oral prednisone taper. This case illustrates that lower doses may be adequate in hospitalized patients without significant oxygen requirement.
Due to the patient's travel history from California to Maryland with stops in Arizona and Utah, histoplasmosis, blastomycosis, and coccidiomycosis infections were considered. Antigen testing, fungal stains, and serologic testing are often the quickest methods for diagnosing these fungal infections but these methods are not as specific as positive fungal culture data [[11], [12], [13]]. While fungal cultures are the gold standard, these cultures often take several weeks to result, which is not clinically useful in treating acute infections [[11], [12], [13]].
These fungal infections are highlighted due to the possible detrimental effects of using corticosteroids in patients with these infections. Since immunocompromised patients experience more significant pathology or dissemination as a result of fungal infection, there is concern for exacerbating the disease course with providing corticosteroids in these patients due to the blunting of the already compromised immune response [5,11,13]. In this patient, the decision to treat the patient for EVALI was made given her clinical decline while on antibiotics and the lower clinical suspicion for a fungal infection given her presentation, though definitive exclusion of a fungal etiology had not occurred. This highlights the need for clinicians to use their clinical decision-making to weigh the risk and benefits of treating a decompensating patient for suspected EVALI prior to the completion of a comprehensive infectious workup.
What is unique about this case is that this patient developed symptoms two weeks after cessation of vaping. However, it is important to note the possibility that this patient may not have been completely forthcoming and may have stopped vaping less than two weeks prior to her presentation. Nevertheless, one case series reported a range of 3–9 days between the most recent exposure to vaping and onset of EVALI symptoms [14]. With this patient's transbronchial biopsy results showing histopathological features suggestive of organizing pneumonia, it is also possible that this patient developed secondary organizing pneumonia (SOP) in response to another unknown environmental exposure other than vaping THC. However, this patient's recent history of vaping THC points to EVALI as the more likely diagnosis of exclusion.
There are currently no reliable test to diagnose EVALI and its treatment may be of detriment when other concomitant pulmonary disease is present [5]. While a thorough infectious and autoimmune work-up is necessary, it is important to acknowledge that many of these tests may not return in time to impact clinical decisions if patients continue to decompensate. Therefore, when clinicians are considering the diagnosis of EVALI, they may need to focus more on the patient's clinical presentation and clinical trajectory rather than laboratory data to guide therapy. This may especially be the case in more rural or austere settings where the medical infrastructure is not present to support expedited laboratory processing. Additionally, an important outpatient consideration is to strongly advise prior and current vaping product users to receive the influenza vaccine and to abide by CDC's guidelines to reduce the risk of the SARS-CoV-2 infection in the setting of the COVID-19 pandemic.
Disclaimer
The identification of specific products or scientific instrumentation is considered an integral part of the scientific endeavor and does not constitute endorsement or implied endorsement on the part of the author(s), DoD, or any component agency. The views expressed in this manuscript are those of the author(s) and do not necessarily reflect the official policy of the Uniformed Services University, Department of Defense or the U.S. Government.
Declaration of competing interest
None of the authors have any conflicts of interest to disclose.
Footnotes
This manuscript has been seen and approved by all of the co-authors.
This case report is clinically relevant in that e-cigarette, or vaping, product-use associated lung injury is increasingly recognized with the use of vapes and the legalization of tetrahydrocannabinol in numerous states [1]. This case report adds to the literature by illustrating a case in which a patient with EVALI experienced symptom resolution on a lower dose of systemic corticosteroid compared to that of other published case reports and series [4,6,7]. Additionally, this manuscript highlights the importance and challenge of ruling out infectious disease processes, particularly during the coronavirus disease 2019 (COVID-19) global pandemic, prior to initiating EVALI treatment.
No papers closely related to the submitted manuscript has been published or submitted for publication elsewhere.
Contributor Information
Jessica Lilley, Email: jessica.lilley@usuhs.edu.
Shena Kravitz, Email: shena.kravitz@gmail.com.
References
- 1.Cullen K.A., Gentzke A.S., Sawdey M.D. E-cigarette use among youth in the United States, 2019. J. Am. Med. Assoc. 2019;322(21):2095–2103. doi: 10.1001/jama.2019.18387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Alexander L.E.C., Bellinghausen A.L., Eakin M.N. What are the mechanisms underlying vaping-induced lung injury? J. Clin. Invest. 2020;130(6):2754–2756. doi: 10.1172/JCI138644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Perrine C.G., Pickens C.M., Boehmer T.K. Characteristics of a multistate outbreak of lung injury associated with E-cigarette use, or vaping — United States, 2019. Morb. Mortal. Wkly. Rep. 2019;68(39):860–864. doi: 10.15585/mmwr.mm6839e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kalininskiy A., Bach C.T., Nacca N.E. E-cigarette, or vaping, product use associated lung injury (EVALI): case series and diagnostic approach. Lancet Respir Med. 2019;7(12):1017–1026. doi: 10.1016/S2213-2600(19)30415-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jatlaoui T.C., Wiltz J.L., Kabbani S. Update: interim guidance for health care providers for managing patients with suspected E-cigarette, or vaping, product use–associated lung injury — United States, november 2019. Morb. Mortal. Wkly. Rep. 2019;68(46):1081–1086. doi: 10.15585/mmwr.mm6846e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Blagev D.P., Harris D., Dunn A.C., Guidry D.W., Grissom C.K., Lanspa M.J. Clinical presentation, treatment, and short-term outcomes of lung injury associated with e-cigarettes or vaping: a prospective observational cohort study. Lancet. 2019;394(10214):2073–2083. doi: 10.1016/S0140-6736(19)32679-0. [DOI] [PubMed] [Google Scholar]
- 7.Davidson K. Outbreak of electronic-cigarette–associated acute lipoid pneumonia — North Carolina. MMWR Morb. Mortal. Wkly. Rep. 2019;68 doi: 10.15585/mmwr.mm6836e1. July–August 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cedano J., Sah A., Cedeno-Mendoza R., Fish H., Remolina C. Confirmed E-cigarette or vaping product use associated lung injury (EVALI) with lung biopsy; A case report and literature review. Respir Med Case Rep. 2020;30 doi: 10.1016/j.rmcr.2020.101122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Panse P.M., Feller F.F., Butt Y.M. Radiologic and pathologic correlation in EVALI. Am. J. Roentgenol. 2020;215(5):1057–1064. doi: 10.2214/AJR.20.22836. [DOI] [PubMed] [Google Scholar]
- 10.Blount B.C., Karwowski M.P., Shields P.G. Vitamin E acetate in bronchoalveolar-lavage fluid associated with EVALI. N. Engl. J. Med. 2020;382(8):697–705. doi: 10.1056/NEJMoa1916433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Azar M.M., Hage C.A. Clinical perspectives in the diagnosis and management of histoplasmosis. Clin. Chest Med. 2017;38(3):403–415. doi: 10.1016/j.ccm.2017.04.004. [DOI] [PubMed] [Google Scholar]
- 12.McBride J.A., Gauthier G.M., Klein B.S. Clinical manifestations and treatment of blastomycosis. Clin. Chest Med. 2017;38(3):435–449. doi: 10.1016/j.ccm.2017.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gabe L.M., Malo J., Knox K.S. Diagnosis and management of coccidioidomycosis. Clin. Chest Med. 2017;38(3):417–433. doi: 10.1016/j.ccm.2017.04.005. [DOI] [PubMed] [Google Scholar]
- 14.Triantafyllou G.A., Tiberio P.J., Zou R.H. Vaping-associated acute lung injury: a case series. Am. J. Respir. Crit. Care Med. 2019;200(11):1430–1431. doi: 10.1164/rccm.201909-1809LE. [DOI] [PubMed] [Google Scholar]