Abstract
Small cell lung cancer (SCLC) transformation is a rare resistance mechanism to anaplastic lymphoma kinase-tyrosine kinase inhibitors (ALK-TKIs), for which cytotoxic chemotherapy is often initiated. However, no case has been reported so far in which the SCLC component disappeared after chemotherapy and the tumor responded to ALK-TKI treatment again. A 41-year-old, never-smoker man was diagnosed with multiple metastatic lung adenocarcinoma harboring ALK gene rearrangements. After tumor re-growth was treated with alectinib, histological analysis of re-biopsy of the primary lesion showed combined small cell carcinoma, and cytotoxic chemotherapy was administered. After resistance to chemotherapy developed, the third biopsy of the primary lesion showed the original ALK gene rearrangements without the SCLC component. Alectinib was re-administered, and partial response was obtained. Biopsy for ALK-positive lung cancer that progressed after chemotherapy for SCLC transformation might be useful for decision-making regarding the therapeutic strategy.
Keywords: Non-small cell lung cancer, Small cell transformation, Alectinib, Anaplastic lymphoma kinase
Abbreviations
- ALK
anaplastic lymphoma kinase
- CEA
carcinoembryonic antigen
- EGFR
epidermal growth factor receptor
- FISH
fluorescence in situ hybridization
- IHC
immunohistochemistry
- NSCLC
non-small cell lung cancer
- SCLC
small cell lung cancer
- SLX
sialyl-Lewis X-i antigen
- TKI
tyrosine kinase inhibitor
1. Introduction
Anaplastic lymphoma kinase (ALK) gene rearrangements are present in 3–5% of patients with non-small cell lung cancer (NSCLC). In the past decade, various tyrosine kinase inhibitors (TKIs) showed a dramatic and durable clinical benefit against ALK-positive NSCLC. Nevertheless, drug resistance and recurrent disease still develop in the vast majority of initial responders. The resistance mechanisms in patients with ALK-positive NSCLC comprised ALK gene alterations, such as ALK point mutations and copy-number gains, bypass signaling activation through the activation of other oncogenes, and small cell lung cancer (SCLC) transformation [1,2]. Although standard therapeutic strategies have not yet been established for patients with SCLC transformed from ALK-positive adenocarcinoma, standard therapies for SCLC are recommended for patients with SCLC transformed from epidermal growth factor receptor (EGFR)-mutant adenocarcinoma [3]. However, whether subsequent re-challenge with TKI after chemotherapy provides clinical benefit is not known.
A case of adenocarcinoma harboring ALK gene rearrangements that transformed to SCLC following alectinib treatment is reported. After resistance to cytotoxic chemotherapy developed, the third biopsy of the primary lesion showed the original ALK gene rearrangements without the SCLC component, and alectinib re-challenge showed partial response. This case report shows the importance of repeated biopsy for decision-making regarding therapeutic strategies in ALK-positive lung cancer with SCLC transformation.
2. Case description
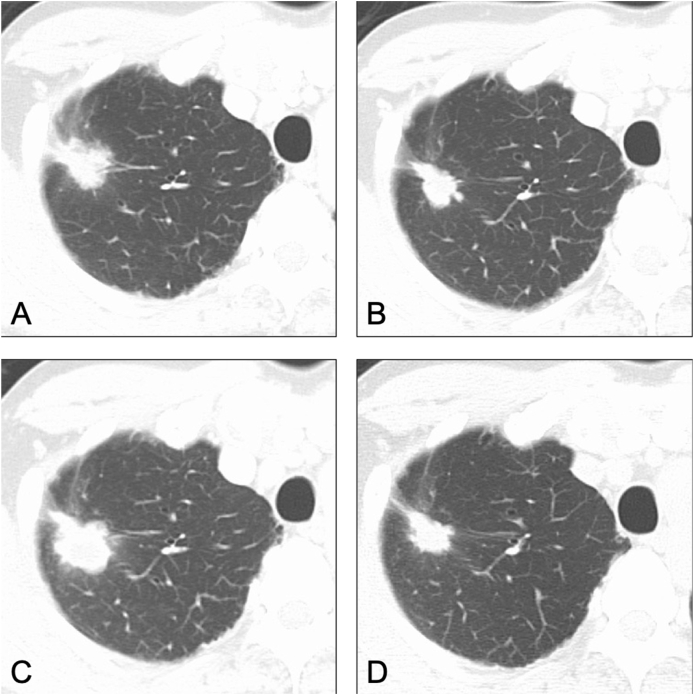
In March 2010, a 41-year old man with no history of smoking underwent a medical examination for epigastralgia. The echocardiogram showed a massive pericardial effusion, and an emergent pericardial puncture was performed. Multiple metastatic lung cancer (cT4N3M1c) was diagnosed by computed tomography and positron emission tomography (Fig. 1). Cytological examination of the pericardial effusion showed adenocarcinoma. The patient subsequently underwent 4 regimens of chemotherapy (cisplatin plus pemetrexed as the first-line treatment, S-1 as the second-line treatment, amrubicin as the third-line treatment, and docetaxel as the fourth-line treatment), but disease progression was observed.
Fig. 1.
Imaging findings at the time of initial diagnosis A, B) Chest computed tomography scan shows a primary lesion in the right upper lobe and a massive pericardial effusion. C, D) F18 fluorodeoxyglucose positron emission tomography scan shows uptake by the primary lesion, mediastinal lymph nodes, and pelvic bone.
In January 2012, a biopsy of the primary lesion in the right upper lobe was performed, and both immunohistochemistry (IHC) and fluorescence in situ hybridization (FISH) showed adenocarcinoma with ALK rearrangement. The drug regimen was changed to 300 mg alectinib twice daily, which is the approved dosage in Japan. He eventually achieved a partial response. After 4 years of alectinib treatment, no metastases appeared, but the primary lesion progressed (Fig. 2A).
Fig. 2.
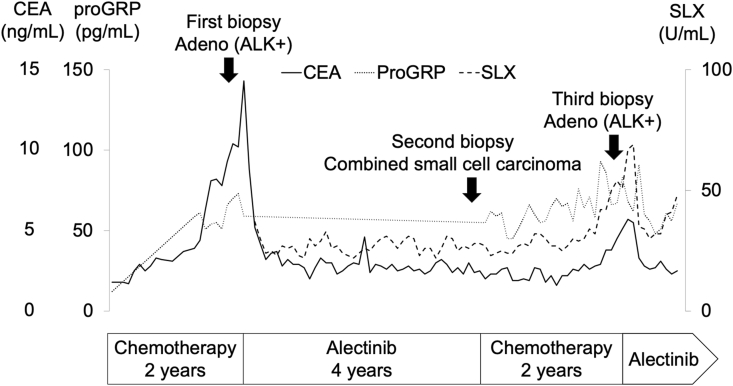
Computed tomography findings A) Progression of the primary lesion after 4 years of alectinib treatment. B) Partial response during cytotoxic chemotherapy for SCLC. C) Progression of the primary lesion after 2 years of cytotoxic chemotherapy for SCLC. D) Partial response after alectinib rechallenge.
Histological analysis based on re-biopsy showed combined small cell carcinoma, in which the SCLC components were CD56 (+), synaptophysin (+), TTF-1 (−), and ALK-1 (−), and the adenocarcinoma components were CD56 (−), synaptophysin (−), TTF-1 (+), and ALK-1 (+) (Fig. 3A). Two regimens of cytotoxic chemotherapy for SCLC (cisplatin plus irinotecan as the sixth-line treatment and amrubicin as the seventh-line treatment) showed a partial response (Fig. 2B), but serum tumor markers such as carcinoembryonic antigen (CEA) and sialyl-Lewis X-i antigen (SLX) increased gradually (Fig. 4). Imaging findings showed progression of the primary lesion and multiple brain metastases (Fig. 2C).
Fig. 3.
Pathological findings A) The second biopsy sample shows combined small cell carcinoma. SCLC components are positive for CD56 and synaptophysin, and adenocarcinoma components are positive for TTF-1 and ALK-1. B) The third biopsy sample shows only adenocarcinoma without SCLC components. Immunohistopathological analysis shows positive staining for TTF-1 and ALK-1, but negative staining for CD56 and synaptophysin.
Fig. 4.
Clinical course during the sequential treatment and tumor marker levels. CEA and SLX levels are re-elevated after disease progression during cytotoxic treatment for SCLC transformation. Alectinib is re-administered after the third biopsy, which results in a partial response and decreased CEA and SLX levels.
The third biopsy of the primary lesion showed only adenocarcinoma, with CD56 (−), synaptophysin (−), TTF-1 (+), and ALK-1 (+), and disappearance of the SCLC component (Fig. 3B). Alectinib was re-administered, which resulted in a partial response and decreased CEA and SLX levels (Fig. 2, Fig. 4). The tumor response was maintained for 8 months after the rechallenge without cranial irradiation or surgery.
3. Discussion
Several cases of EGFR-mutant adenocarcinoma that transformed to SCLC and responded to TKIs again after development of resistance to chemotherapy have been reported [4,5]. To the best of our knowledge, however, this is the first case of successful re-challenge by ALK-TKI in an ALK-positive NSCLC in which the SCLC component disappeared after chemotherapy for SCLC transformation. After transformation, cytotoxic chemotherapy reduced the SCLC component, and the proportion of ALK rearrangement-positive cancer cells increased in the heterogeneous tumors. This may explain why alectinib re-challenge was effective again.
Some reports have shown that the loss of tumor suppressor genes, such as RB1 and Tp53, plays an important role in transformation to SCLC during treatment with ALK-TKIs or EGFR-TKIs [[6], [7], [8]]. In the present case, comprehensive genomic profiling could not be performed due to poor biopsy samples, and the genetic background of SCLC transformation was unknown. However, the absence of a smoking history and tumor progression after long-term molecular targeted therapy suggested that the SCLC components were not originally present, but rather that SCLC transformation was caused by the selective pressure of alectinib treatment.
Serum pro-gastrin-releasing peptide precursor (ProGRP) and neuron-specific enolase (NSE) have been reported to be useful predictive markers for SCLC transformation during the development of resistance to ALK-TKIs [9]. In the present case, there was no correlation between SCLC transformation and ProGRP. On the other hand, CEA and SLX levels were re-elevated after disease progression during cytotoxic treatment for SCLC transformation. No elevation of CEA or SLX was observed when transformation to SCLC was confirmed by the re-biopsy. Thus, these tumor markers may be useful for predicting the majority of the histological subtypes in heterogeneous lung cancers.
In conclusion, the present case is the first to show that re-challenge with ALK-TKIs is effective after chemotherapy failure for SCLC transformation. Repeat biopsy at progression might be useful for decision-making regarding the therapeutic strategy for ALK-positive lung cancer with SCLC transformation.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author contributions
AY drafted the manuscript. TY reviewed the manuscript. AY, TY, YF, and TY were responsible for final approval of the version to be submitted.
Declaration of competing interest
None.
Acknowledgments
None.
References
- 1.Gainor J.F., Dardaei L., Yoda S. Molecular mechanisms of resistance to first- and second-generation ALK inhibitors in ALK-rearranged lung cancer. Canc. Discov. 2016;6:1118–1133. doi: 10.1158/2159-8290.CD-16-0596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Katayama R., Friboulet L., Koike S. Two novel ALK mutations mediate acquired resistance to the next-generation ALK inhibitor alectinib. Clin. Canc. Res. 2014;20:5686–5696. doi: 10.1158/1078-0432.CCR-14-1511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Marcoux N., Gettinger S.N., O'Kane G. EGFR-mutant adenocarcinomas that transform to small-cell lung cancer and other neuroendocrine carcinomas: clinical outcomes. J. Clin. Oncol. 2018;37:278–285. doi: 10.1200/JCO.18.01585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lee S., Joo J., Kwak M. Role of chemotherapy with epidermal growth factor receptor-tyrosine kinase inhibitor (EGFR-TKI) rechallenge in small cell transformation after EGFR-TKI failure: a case report. OncoTargets Ther. 2018;11:3943–3947. doi: 10.2147/OTT.S164764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nishioka N., Yamada T., Harita S. Successful sequential treatment of refractory tumors caused by small cell carcinoma transformation and EGFR-T790M mutation diagnosed by repeated genetic testing in a patient with lung adenocarcinoma harboring epidermal growth factor receptor mutations: a case report. Respir. Med. Case. Rep. 2018;25:261–263. doi: 10.1016/j.rmcr.2018.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Levacq D., D'Haene N., Wind R. Histological transformation of ALK rearranged adenocarcinoma into small cell lung cancer: a new mechanism of resistance to ALK inhibitors. Lung Canc. 2016;102:38–41. doi: 10.1016/j.lungcan.2016.10.012. [DOI] [PubMed] [Google Scholar]
- 7.Norkowski E., Ghigna M.R., Lacroix L. Small-cell carcinoma in the setting of pulmonary adenocarcinoma: new insights in the era of molecular pathology. J. Thorac. Oncol. 2013;8:1265–1271. doi: 10.1097/JTO.0b013e3182a407fa. [DOI] [PubMed] [Google Scholar]
- 8.Oser M.G., Niederst M.J., Sequist L.V. Transformation from non-small-cell lung cancer to small-cell lung cancer: molecular drivers and cells of origin. Lancet Oncol. 2015;16:e165–e172. doi: 10.1016/S1470-2045(14)71180-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Oya Y., Yoshida T., Uemura T. Serum ProGRP and NSE levels predicting small cell lung cancer transformation in a patient with ALK rearrangement-positive non-small cell lung cancer: a case report. Oncology Letters. 2018;16:4219–4222. doi: 10.3892/ol.2018.9158. [DOI] [PMC free article] [PubMed] [Google Scholar]