Abstract
Purpose
Depression affects millions of people worldwide and is prevalent among those with diabetes. The purpose of this review was to synthesize recent research on depression and adherence to dietary and physical activity recommendations in persons with type 2 diabetes (T2DM).
Methods
This systematic review is a sub-analysis of a NIH-funded model-testing meta-analysis. Thirteen electronic databases were searched using terms: depression, adherence, T2DM, diabetes. Selected studies: were reported in English between 2000–2012, focused on adults with T2DM, and measured depression and dietary and/or physical activity adherence.
Results
Twenty-seven studies involving 7,266 participants were selected; participants were 54% female and 62 years of age, on average. When reported, depression prevalence in study samples ranged from 4.5% to 74%. Six intervention studies targeted diabetes treatment, with or without depression treatment; no studies focused solely on treating depression. Twenty-one descriptive studies examined relationships between depression and diet/physical activity adherence, finding a negative association. Only 2 of the 6 intervention studies examined this relationship; findings were inconsistent.
Conclusion
Depression was associated with lower adherence to diabetes self-care, as evidenced primarily by descriptive studies; results of intervention studies were conflicting. Future research should focus on the effects of treating depression on diabetes health outcomes.
Depression affects 121 million people worldwide and in 2002 was the leading cause of disability, accounting for 4.5% of the global burden of disease.1,2 Depression is an acute or chronic mental disorder presenting as “a depressed mood, loss of interest or pleasure, feelings of guilt or low self-worth, disturbed sleep or appetite, low energy, and poor concentration.”2
Depression is more prevalent among people with diabetes than among the general population.3,4 Diabetes is a serious metabolic condition that affects more than 346 million adults worldwide, a number expected to double by the year 2030. Type 2 diabetes (T2DM) is the most common form of diabetes and arises due to obesity and other conditions that cause insulin resistance. Complications of diabetes resulted in 3.4 million deaths in 2004, 80% of which occurred in low to middle income countries.6 The reported global prevalence of depression among diabetes cohorts comprised of different ethnic groups has ranged from 11% to 71.8%.5 A meta-analysis of 42 studies conducted in 2001 found that adults with diabetes were twice as likely to have depression as those without diabetes, reporting an 11% prevalence of major depression and a 31% prevalence of major and mild depression combined in those with diabetes.7 Fewer than 25% of those suffering from depression are treated effectively.2
Depression can substantially inhibit people’s fulfillment of their daily responsibilities.2 Studies have shown that people diagnosed with both diabetes and depression are less likely to adhere to lifestyle changes, i.e. recommended diet and physical activity changes, resulting in poor glycemic control and increased diabetes-related complications, such as retinopathy, nephropathy, and cardiac dysfunction.8 Researchers have examined the relationship between depression, diabetes self-care, sometimes referred to as self-management, behaviors — diet, physical activity, medication self-administration, blood glucose monitoring, and/or foot care — and glycemic control.9–13,14,15 Egede (2005) found that depressed mood inhibited adherence to self-care behaviors by decreasing the desire to seek treatment, thus making the behaviors key mediators of the link between depression and poor diabetes outcomes.4 Few studies have focused on the effects that depression or depressive symptoms have on two important lifestyle changes (diet and physical activity [PA]). These two behaviors are the cornerstones of the non-pharmacological approach to preventing16–18 and treating T2DM.19
The purpose of this systematic review is to explore and synthesize recent research that examined the association between depression and adherence to lifestyle changes (diet and PA) in people with T2DM, inform future intervention development, identify gaps in the literature, and suggest recommendations for future research. This review includes studies conducted from 2000 to the present, seeking to update and narrow the focus of Egede’s previous review,4 concentrating only on diet and PA behaviors. The research questions for this systematic review, focused on persons with T2DM, were:
What are the characteristics of studies conducted since 2000 that have focused on depression and dietary and PA adherence?
What relationships have been reported between the diagnosis and/or symptoms of depression and adherence to diet and PA recommendations?
Recent emphasis on patient-centered diabetes care, or “empowerment,” has challenged the concepts of “adherence” and “compliance.”20 However, the majority of studies conducted during the last decade used these terms and thus, the term “adherence” was used when searching for and referencing these studies.
Methods
This systematic review is a sub-analysis of a model-testing meta-analysis involving the examination of variables predictive of diabetes outcomes. The set of models that is being examined in the meta-analysis includes psychological (e.g., depression, stress, anxiety), motivational (e.g., self-efficacy, health beliefs), and diabetes-related knowledge factors in predicting diabetes outcomes, such as glycemic control and quality of life, with behavioral lifestyle factors (e.g., adherence to diet and physical activity) as mediating variables. PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines and other published protocols for systematic reviews were followed.21,22 Both published journal articles and unpublished dissertation studies that examined the relationship between depression and dietary and/or physical activity adherence in T2DM were sought. Studies were included if they: 1) were written in English and reported between 2000–2012; 2) included a sample of adults diagnosed with T2DM; and 3) measured depression and dietary and/or PA adherence. Studies were excluded if the type of diabetes was not clearly specified or the sample was mixed with regard to type of diabetes.
Search Strategy
A total of 13 electronic databases were searched. Primary sources included: PubMed, Cumulative Index to Nursing and Allied Health Literature (CINAHL), Web of Science, Education Resources Information Center (ERIC), ProQuest Dissertations & Theses, and PsychINFO. Search terms and their synonyms appropriate for each database were depression, adherence, type 2 diabetes, and diabetes. Approximately 7.5% of included studies were obtained from ancestry searches of the reference list from each article that met the inclusion criteria.
Data Extraction
The initial search resulted in 183 citations. The first screening of titles and abstracts according to the inclusion criteria resulted in a total of 46 studies. A secondary screening of the full text of each study resulted in 27 studies in the sample, or 15% of the original number of studies located in the search. (See the flow diagram in Figure 1.) A data extraction table (Table 1) was developed to summarize information on each study.
Figure 1.
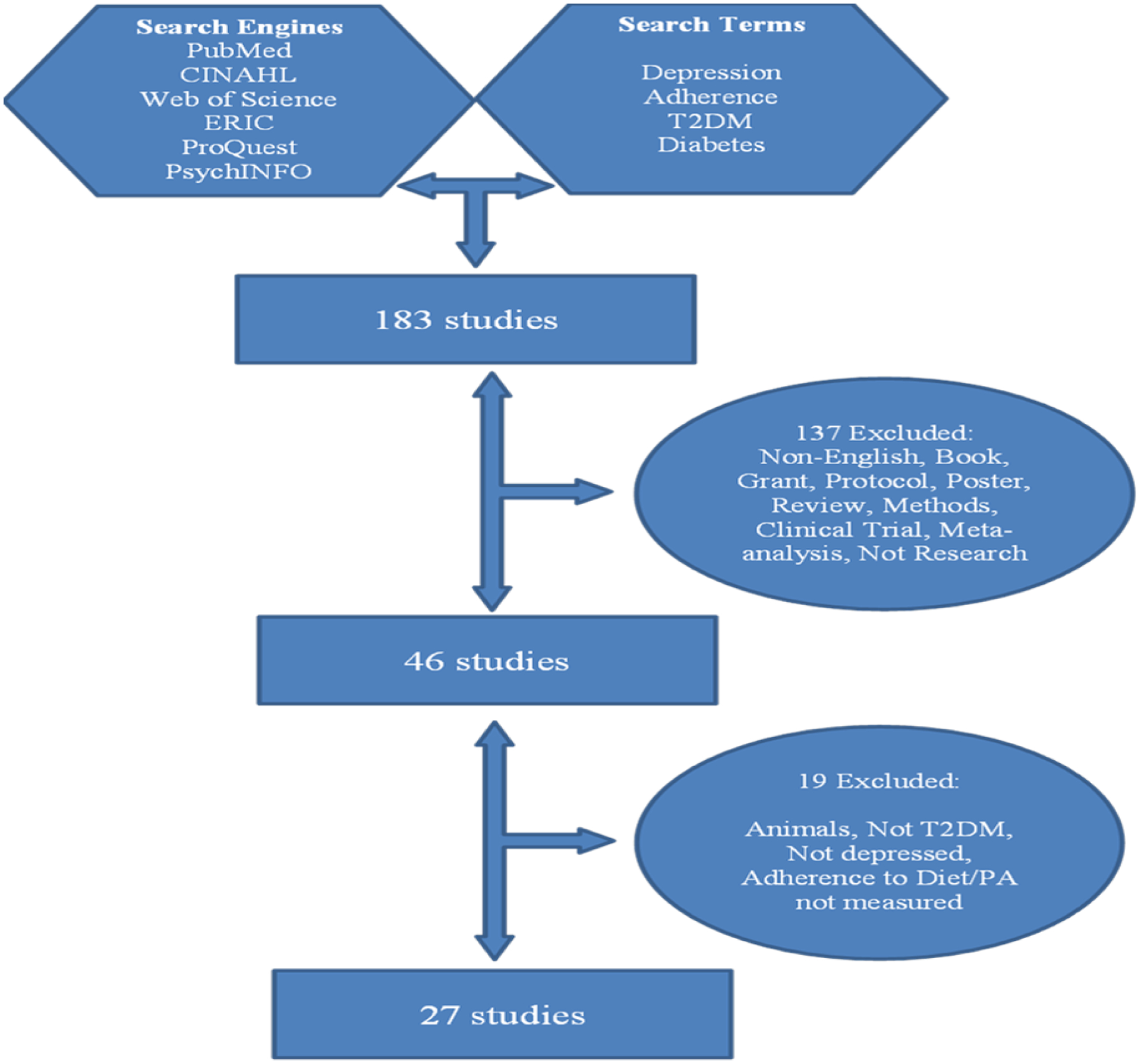
Flow Diagram of Sample Selection
Table 1:
Characteristics of Studies
| Author/Date | Purpose | Subjects | Design/Setting | Intervention(s) | Depression/Diet/PA Instruments | Major Findings | Conclusions |
|---|---|---|---|---|---|---|---|
| Ahlgren et al. 2004 (31) | Develop instrument to measure DM diet satisfaction & outcomes | 239 T2DM (180 w/ clinical data); 54% female; mean age=64, DM duration=10 yrs, A1C=7.5 | Mixed methods: focus groups & mailed survey Rockwood Clinic, Spokane, WA |
NA | Satisfaction w/ meal plan SF-12 Health Survey [Mental Component] Medical chart data for dep history |
16% w/ major dep; SF-12 [MC]= 48.7±10.7. Dep re to less satisfaction w/ ability to handle DM away from home (p<.05) & craving sweets (p<.01). Concern re to cost of diet (p<.01). Dietary adh re to A1C (r=−0.18, p<.01). |
Satisfaction w/ ability to manage DM diet may re to co-morbidities. |
| Bell et al. 2010 (32) |
Evaluate association b/t depression & DM self-mgmt in ethnically diverse sample of rural older adults | 696 T2DM; 49% female; 42.4% White, 31.6% AA, 26% Native Amer; mean age=74.1, DM duration=12.5 yrs | Population-based cross-sectional survey Diverse rural, community in NC |
NA | CES-D (modified cutoff ≥9) SDSCA: diet, PA |
16% w/ CES-D ≥9. Dep sxs neg associated w/ PA (adj OR=0.5; 95% CI 0.2,0.9) & healthy eating (adj OR=0.6; CI 0.4,1.1). Healthful eating: CES-D≥9=6.5%, CES-D<9=24.2%. PA (exercising 5–7 days): CES-D≥ 9=5.5%, CES-D<9=19%. | Dep sxs assoc. w/ poor adh to PA & healthy eating but not w/ other self-mgmt behaviors. Recommend community-based programs for minority rural elders. |
| Castillo et al. 2010 (13) | Evaluate outcomes of a DM education program provided by community health workers (CHWs) in Latino community | 70 T2DM (33 completed dep scale); 75.7% female; 100% Hispanic; attrition=33%; mean age=58.2, DM duration=11.8 yrs, A1C=8.4 | Mixed methods: one-group pre-test, post-test design & focus groups Community settings in Chicago (churches, schools, etc.) |
Diabetes Empowerment Education Program; culturally appropriate adult ed. strategies 8 2-hr ed. modules over 10 wks by trained CHWs |
PHQ-9 Quick Depression Assessment Scale SDSCA: diet, PA |
47.1% w/ dep. A1C: baseline 8.4±1.96; 3-mo post-intervention 7.8±1.7 (p<.001). Dep: baseline 8.2±6.2; 3-mo 6.2±5.7 (p=.04). Healthy diet: baseline 3.3±2.2; 3-mo 4.9±1.5 (p<.000). 30-min PA: baseline 2.8±2.3; 3-mo 4.0±2.3 (p=.013). |
Resulted in positive short-term effects. Recommend further research: larger sample, RCT, long-term impact. |
| Cypress 2008 (24)[dissertation] | Explore illness perceptions, life goals, & DM self-mgmt behaviors in Hispanic vs. non-Hispanic men | 140 T2DM; 100% male; 50% Hispanic, 44% White, 3.6% AA, 1.4% Native Amer; mean age=66.6, DM duration=11 yrs, BMI=30, A1C=6.9 |
Descriptive DM education centers & community settings; Central, Western & Northern NM |
NA | CES-D SDSCA: diet, PA |
Low rates of dep; mean CES-D= 9.8±7.9. No sig diff in dep b/t Hispanics (10.6±8.6) vs non-Hispanics (8.9±7.0) (p=.29). No sig diff in self-mgmt behaviors b/t Hispanics & non-Hispanics. No relationship b/t dep sxs & diet/PA adh. |
No differences b/t Hispanic & non-Hispanic men re to dep & self-mgmt behaviors. |
| Daly et al. 2009 (33) | Identify relationships b/t barriers to DM self-mgmt behaviors & glycemic control | 253 T2DM; 57% female; 85% White, 15% non-White; mean age=60.2, DM duration=10.1 yrs, A1C=7.1% |
Cross-sectional; medical record review & mailed survey; random sample Out-patient clinics, mid-western medical center |
NA | PHQ-9 Self-Care Behaviors Survey for Patients w/ Diabetes |
Mean dep, PHQ-9=7.9±7.0. Dep corr w/ higher A1C (r=0.22, p=.001). Dep interfered w/ meal plan, corr w/ higher A1C (r=0.18, p. ≤.01). Dep interfered w/ PA, corr w/ higher A1C (r=0.11, NS). After controlling for predictors, A1C 0.04% higher for every 1-point increase in dep score. |
Main barriers across most self-mgmt behaviors were cost & dep. Pt adh may improve w/ dep treatment. |
| Fisher et al. 2010 (23) | Evaluate relationships b/t depression, DM distress & disease mgmt. behaviors, glycemic control | 463 T2DM; 51.5% female; 28% non-White; mean age= 58.8, A1C =8.1, BMI=34.8 | Descriptive pre-intervention survey Primary care clinics & education centers, CA |
NA | PHQ-8 Diet: Starting the Conversation PA: Community Healthy Activities Model Program for Seniors |
15.3% w/ major dep; 51.3% w/ DM distress. Higher DM distress associated w/ higher A1C & lower PA. Dep not associated w/ A1C or PA but negatively associated w/ diet adh. |
Dep selectively re to disease mgmt. Dep measures may be assessing other aspects of mood besides dep. Recommend ongoing screening for clinical dep & DM distress. |
| Fisher 2003 (34)[dissertation] | Assess relationship b/t adjustment distress living w/ DM, dep, & stages of chg for exercise (PA) | 125 T2DM; 54% female; 96% White, 2.4% Asian Amer, 0.8% AA; mean age=62.3, DM duration=4.4 yrs, A1C=9.4 |
Cross-sectional, mail survey Diabetes suburban hospital out-patient clinics, MA |
NA | Short Geriatric Dep (SGD) Scale Stages of Change-exercise Processes of Change Scale-exercise Confidence Scale Decisional Balance Scale |
18.4% w/ dep; SGD=2.9 ±3.0. Most in advanced stages of change. Sig (p<.05) relationships b/t stages of chg & dep.Highest dep in contemplation stage, lowest in maintenance stage. Dep sig re to adjustment distress. |
Negative emotions re to living w/ DM may be linked to lower self-efficacy for exercise. |
| Gary et al. 2000 (35) | Examine dep & relationships w/ A1C, BP, lipids, BMI; & medita-tional role of self-mgmt behaviors on relationship b/t dep & metabolic control | 183 T2DM; 76% female; 100% AA; mean age=59, BMI=33, A1C=8.6 | Cross-sectional analysis of Project Sugar baseline data Recruited from 2 primary care clinics, East Baltimore, MD |
NA | CES-D Medical records: dep diagnosis & med FFQ Short questionnaire: habitual PA during leisure time |
45% w/ dep, mean CES-D=16. Dep sxs marginally associated w/ suboptimal A1C, DBP, LDL & sig associated w/ chol & trig. Those with fewest dep sxs: A1C=8.3% vs. those w/ most dep sxs: A1C=8.8% (after accounting for diet, PA, smoking, SMBG, med adh). |
High prevalence of subclinical dep in AA w/ T2DM. No self-mgmt behavior mediated link b/t dep sxs & metabolic control. Dep may be major factor in poor metabolic control in AA. |
| Gilmer et al. 2008 (44) | Assess feasibility & cost of integrating DM & dep care mgmt in low-income setting | 99 T2DM; 84% female; 74% Latino; mean age=53 | Quasi-experimental 3 community clinics, San Diego County |
Added dep care manager to existing DM mgmt team | PHQ-9 SDSCA: diet, PA |
33% w/ dep; women reported more dep than men (p<.001). Avg 6.7 visits w/ dep care mgr; 69% rec’d problem-solving tx, 35% med mgmt. Intervention reduced dep sxs: 14.8 to 7.3 (SD 6.5, p<.001). |
High rates of comorbid DM & dep in Latinos. Combined DM & dep care mgmt feasible; cost is modest. |
| Giugliano et al. 2010 (36) | Examine Mediterranean-type diet, sexual function, & dep sxs in women with T2DM | 595 T2DM; 100% female; mean age= 57.6, BMI=29.5 | Descriptive, cross-sectional survey; part of Campanian Post-Prandial Hyperglycemia Study (large observational study of T2DM) Italy |
NA | Dep sxs: self-report use of antidepressants &/or counseling FFQ (adapted) Mediterranean diet scale International PA Questionnaire |
31.5% w/ dep. Higher adh to Mediterranean diet re to lower A1C, lower post-prandial glucose levels, less dep, & more PA. |
Adh to Mediterranean diet re to glycemic control, less dep, more PA, & lower sexual dysfunction on women. |
| Gonzalez et al. 2008 (37) | Examine prospective relationship b/t dep at baseline (bl) & self-mgmt adh 9 mos later | 208 T2DM; 49% female; 86% White, 7% AA, 3% Hispanic; mean age=65.5, DM duration=9.4 yrs |
Cross-sectional, longitudinal survey 2 primary care clinics, Boston |
NA | HANDS SDSCA: diet, PA |
18% w/ major dep. Higher bl dep sxs predicted lower diet adh (p=.007), less PA (p=.05). Bl & chg in dep sig predicted less adh to general diet, fruits/vegs, carb spacing, PA. |
Relationship b/t dep sxs & poorer self-mgmt is sig (effect size small to medium). Recommend testing dep interventions w/ large RCTs. |
| Gonzalez et al. 2007 (38) | Explore dose relationships b/t dep & DM self-mgmt behaviors | 879 T2DM; 48% female; 86% White; mean age=66.2, DM duration=9.5 yrs, BMI=31.4 | Cross-sectional, longitudinal survey 2 primary care clinics, Boston |
NA | HANDS SDSCA: diet, PA |
19% w/ major dep. Mean days diet adh in dep pts= 3.8±0.18 (p<.001). Mean days PA adh in dep pts= 1.96±0.19 (p<.001). Major dep sig associated w/ poorer self-mgmt over previous 7 days. | Low levels dep re to non-adh. Recommend additional research to understand role of subclinical dep sxs. |
| Katon et al. 2010 (9) | Determine if coordinated care of dep & poorly controlled DM and/or CHD improves outcomes | 214 T2DM; 52% female; 24% non-White; mean age= 56.8, A1C=8.0, BMI=36.7 | Single blind RCT Primary care clinics, integrated health care system, Washington State |
MD supervised nurse-managed care: treat to target, control risk factors, DM self-mgmt, & drug therapy for dep, HTN, lipids, glycemia Clinic visits every 2–3 wks; maintenance & follow-up |
SCL-20 PHQ-2: dep screen; cutoff ≥3 PHQ-9: cutoff ≥10 Self-reported days of adh to diet, PA Pt Global Rating of Improvement: dep |
74% w/ dep, SCL-20=1.7±0.6, PHQ-9=14±3.4. Greater improvements in intervention group: A1C (−0.58%); dep (SCL-20: diff=0.40, effect size=0.67), larger number w/ ≥50% reduction in dep, more satisfied w/ dep Rx, & likely to have chgs in dep meds. No sig diff b/t grps in pts adhering to diet & PA at least 2 days/wk. |
Intervention associated w/ improved outcomes, including dep, in dep pts w/ DM and/or CHD. |
|
McKellar et al. 2004 (43) |
Determine whether dep/dep sxs result/s in poorer outcomes due to limited self-mgmt adh |
307 T2DM; 29% female; 31% Hispanic, 45% White, 12% AA, 12% Other; 54% BMI>30 |
Telephone survey & baseline (bl) interview w/ participants of 2 RCTs 2 general medicine & 4 VA clinics |
NA |
CES-D Medical Outcomes Study 36-item Short Form [MH] 3 items: foods eaten consistent w/ DM guidelines |
Mean CES-D=11±4, SF-36 [MH]= 14±7. Dep sig impacts self-mgmt behaviors but has little direct effect on DM sxs & outcomes. |
Dep sxs interfere w/ pt’s adh to self-mgmt regimen. Dep mgmt affects pts’ QOL & DM self-mgmt goal attainment. Persons w/ DM should be screened for dep. Self-mgmt interventions may decrease dep. |
| Moreau et al. 2009 (39) | Identify adh prevalence, associated medical & psychosocial factors, & pt-MD agreement on level of pt adh | 521 T2DM; 45% female; mean age=65; DM duration 44%>10 yrs; A1C 23%≥8% | Cross-sectional survey 39 GP practices France |
NA | HADS Self-admin questionnaires: perceptions of adh to diet & PA (& meds) |
10% w/ dep. Adh w/ diet & PA lower than med. Factors independently associated w/ adh: socio-demo, BMI, A1C>8, dep, & taking meds. Dep associated w/ adh problems (OR=2.54; 95% CI=1.02,6.33). Pt-MD agreement on pt adh=70%. |
Problems w/ diet or PA adh 5–6 times more frequent than w/ med adh. Pts w/ ≥1 risk factor for adh problems should be assessed: young age, single, A1C>8%, BMI>30, dep, or perceiving meds as constraints. |
| Murata 2004 (25) | Validate food frequency (FF) as predictor of metabolic status in insulin-treated pts w/ T2DM; identify psychosocial factors (including dep) affecting dietary adh | 347 T2DM (105 excluded due to reporting ≤1000 kcal intake); 4.3% female; 66.9% White; mean age=65, DM duration=14.5 yrs, 54.8% BMI≥30 | Prospective observational study Random selection from computer pharmacy records in VA systems, NM & AZ |
NA | Geriatric Depression Scale (GDS) Diet adh: Diabetes Care Profile & FFQ PA: met-hrs/wk |
Mean GDS=7.98±6.8. Poor overall adh w/ diet guidelines; met 32% of ADA diet objectives. Least adh pts: least favorable nutrition, poorest metabolic control, more dep sxs. Factors re to dietary adh: age, social barriers to dieting, attitudes, belief that diet controls DM |
Assessment of FF, dep, perceptions of importance of diet, & social barriers to dieting should be routine DM mgmt. Pts w/ poor dietary adh should receive nutrition education. Cautiously use FF w/ Hispanics in SW. |
| Munroe 2008 (10) [dissertation] |
Examine: relationships b/t cognitive appraisals, emotional func & health behaviors; whether influenced by prevention message type |
42 T2DM; 64.3% female; 42.9% White, 33.3% AA, 11.9% Hispanic, 7.1% Native Amer, 4.8% Asian Amer; mean age=52.4, A1C=8.5 | Cross-sectional design Stratified (by gender), random assignment based on type of messaging Recruited via flyers & ads, South FL |
Prevention message via written vignette: encouragement vs. threatening message | BDI-II SCL-90R (dep & anxiety subscales) SDSCA-R: diet, PA |
Mean BDI-II=12.7±14.4. Relationship b/t dep & A1C r=0.02; dep (BDI-II) & overall diet (r=−0.22) & PA (r=−0.17); SCL-90R DEP & diet (r=−0.7) & PA (−0.11). No differences b/t grps in self-mgmt confidence. |
Link b/t depression sxs & obesity risk factors (BMI, diet, PA). DM care should include initial dep & anxiety screening for newly diagnosed pts plus periodic reassessments. |
| Parekh 2001 (26) [dissertation] |
Evaluate relationships b/t dep & glycemic control, DM self-mgmt behaviors | 795 T2DM; 53.5% female; 63.8% White, 32.8% AA, 3.4% Other; mean age=57.9, DM duration=6.4 yrs, BMI=33.5, A1C=8.2 | Mailed surveys HMO, Kaiser Permanente Health Plan, NC |
NA | BDI SDSCA: diet, PA Older Americans Resources & Services Multidimensional Functional Assessment Questionnaire: PA |
14.2% w/ dep, mean BDI=7.9± 6.9. Dep sxs not sig associated w/ glycemic control (p=.23). Dep not predictive of glycemic control beyond demographic & disease-related covariates. No diff in A1C in dep vs. not dep. Dep sxs neg associated w/ adh to PA, diet (amt, fiber, fat, sweets). |
Dep sxs negatively corr w/ adh to amt & type of diet & PA. Self-mgmt behaviors weakly re to A1C. Based on these findings, dep likely not resulting in poor control by affecting self-mgmt. |
| Park et al. 2004 (27) | Determine if dep sxs associated w/ poor self-mgmt behaviors | 168 T2DM; 40% female; mean age=49.5 | Cross-sectional survey EWHA Woman’s University Hospital, Seoul, Korea |
NA | CES-D Self-report questionnaire: diet, PA |
4.5% w/ dep, mean CES-D= 7.3±5.4. CES-D lower in adh vs non-adh pts (p<.05). Dep sxs associated w/ poor diet (OR 1.09; 95% CI 1.02,1.17) & poor PA (OR 1.10; 95% CI 1.03,1.18). Type of med insurance (company vs community) associated w/ diet & PA adh. | Dep pts 3 times more likely to have poor diet adh. Recommend monitoring & mgmt of dep sxs in DM. Further studies needed on effects of dep sxs on glycemic control. |
| Rosal 2005 (11) | Pilot study of DM self-mgmt w/ low-income Spanish-speaking Puerto Ricans | 25 T2DM; 80% female; 100% Caribbean Hispanics; mean age=62.6, DM duration=8.2 yrs, A1C=8.3 | Randomized pilot study Community health center, elder program, & community-wide database, MA |
10 wkly 2.5–3-hr grp sessions on DM knowledge, attitudes, & self-mgmt skills Delivered by RN, RD, & community assistant |
CES-D 24-hr dietary recalls Community Health Activities Model Program for Seniors PA questionnaire |
Mean CES-D=14.6±9.0.Mean intervention attendance=7.8 out of 10 sessions. 3 mos: interv grp A1C reduced by −0.80% (p=0.009). 6 mos: interv grp A1C reduced by −0.85% (p=0.01). Grp differences in reduced dep sxs at 3 mos (p=0.006) & 6 mos (p=.047). Trend towards increased PA in intervention grp. | Social nature of the intervention & focus on PA may have contributed to reduced dep. |
| Rothschild 2010 (28) [dissertation] |
Explore associations b/t fatigue, distress, & global dep w/ self-mgmt & QOL | 151 T2DM; 51.7% female; 93.2% White, 4.8% AA, 1.4% Hispanic, 0.7% Asian Amer; mean age=60.7, DM duration=12 yrs, A1C=7.3 | Survey/chart review Joslin Diabetes Center, New Albany, IN |
NA | CESD-10 (short version) SDSCA: diet, PA PAID Personal Illness Models Questionnaire |
Women reported higher dep (p=.03), antidepressant use (p=.03), & following diet (p=.02). Dep sxs or use of anti-dep meds did not predict dietary adh. |
Majority of sample did not reach cutoff score for dep. Unable to provide info on effects of dep sxs on diet adh. Diet adh consistent w/ current research (3.4–4.9 days in past wk). |
| Sacco et al. 2009 (12) | Examine effects of brief telephone coaching by undergrad psychology students on adh, A1C, DM-related sxs, dep | 62 T2DM; 58% female; 77.4% White, 14.5% AA, 8.1% Hispanic; mean age=52, DM duration=9.5 yrs, A1C=8.5%, BMI=35.8 |
RCT Diabetes Center, University of South FL Medical Clinic |
Structured telephone coaching: 1 phone call/wk for 3 mos followed by 1 bi-wkly call for 3 mos | PHQ-9 SDSCA: diet, PA |
Mean dep sxs=16.4 ±6.7. Intervention: improved diet (p<.05) & PA (p<.001); lowered dep (p<.05) & DM sxs (p<.01). No stat sig improvement in A1C. Self-efficacy mediated treatment effect on dep. Reinforcement improved self-mgmt mediated effect on PA adh. |
Intervention improved diet, PA, dep, & DM sxs. Less effectiveness in improving diet compared to PA. |
| Sacco et al. 2007 (40) | Examine if DM-related sxs &/or self-efficacy mediate effects of adh & BMI on dep | 99 T2DM; 54% female; 78% White,13% AA, 8% Hispanic, 1% Asian Amer; mean age=53 | Cross-sectional Diabetes Center, University of South FL Medical Clinic |
NA | PHQ-9 SDSCA: diet, PA |
18% w/ major dep. Dep sig corr w/ adh, BMI, self-efficacy, & DM-related sxs. DM sxs mediated relationship b/t BMI & dep. Self-efficacy mediated relationship b/t BMI & dep, adh & dep. 35% of variance in dep explained by self-efficacy & DM sxs. | Low self-efficacy promotes dep. Obesity may lead to dep by lowering self-efficacy & increasing DM sxs. |
| Sacco et al. 2005 (29) | Examine role of adh, BMI, & self-efficacy on link b/t dep & poor DM outcomes | 56 T2DM; 55% female; 82% White, 9% Hispanic, 7% AA, 2% Asian Amer; mean age=54, DM duration=9.6 yrs | Survey Diabetes Center, University of South FL Medical Clinic |
NA | PHQ-9 SDSCA: diet, PA |
16% w/ major dep. Adh alone re to dep (p<.01). Link b/t adh & dep mediated by self-efficacy (p<.05). BMI alone re to dep (p<.01). Link b/t BMI & dep mediated by self-efficacy (p<.05). |
Lower adh resulted in higher BMI, lower self-efficacy, & more dep. Boosting self-efficacy may reduce dep & improve DM outcomes. |
| Schwartz 2000 (30) [dissertation] |
Investigate relationships b/t dep & measures of adh: A1C, PA, diet, SMBG | 31 T2DM; 100% White; age range 45–80 | Survey of volunteers in DM self-help group, South FL | NA | BDI-II Self-report questionnaire developed by authors: diet, PA |
Mean dep score=7.9±8.1. Corr b/t dep & self-reported A1C (r=.64, p<.01). Corr b/t dep & self-reported PA (r=−0.46, p<.01) & diet (r=−0.53; p<0.01). |
Pts w/ T2DM should be referred to mental health provider for dep screen. In DM pts w/ dep, emphasize adh. |
| Tovar 2007 (41) [dissertation] |
Explore relationships b/t bio-psychosocial factors & adh to diet & PA | 212 T2DM; 67% female; 62% White, 18.3 Hispanic, 17% AA, 2.8% Other; mean age=58, DM duration=12 yrs | Cross-sectional, correlational 8 out-pt clinics & community settings, SE TX & central NC Data collected from April 2006-March 2007 |
NA | CESD DM Activity Questionnaire: diet, PA |
38% w/ dep; CESD: ≤16: 7.0±4.7, ≥16: 25.4±8.0. Dep predicted adh to diet (p=.001) & PA (p=.007). Dep participants had lower adh to diet (p=.013) & PA (p=.049), compared to non-dep. |
Negative relationships b/t CESD & diet, PA adh. Early screening, treatment for dep needed. |
| Zuberi et al. 2011 (42) | Assess associations b/t dep, glycemic control, & adh to self-mgmt | 286 T2DM; 55.2% female; 64.7% DM duration >3 yrs; mean BMI=29.6 | Comparative cross-sectional study Aga Kahn University Hospital endocrine clinics, Karachi, Pakistan |
NA | HADS (dep score cut off ≥8) Self-report by interview: diet, PA |
50% w/ dep. A1C higher in dep than non-dep pts (8.5% vs. 7.7%; p<0.001). Dep pts more likely to have poor glycemic control (OR=5.57; 95% CI=2.9,10.8). Dep pts less likely to follow dietary (OR=0.45; 95% CI=0.26, 0.79) or PA recommendations (p=0.002). |
Poor outcomes explained by lower adh to self-mgmt recommendations. Suggest monitoring of dep in DM pts. |
Adh (adherence); BDI-II (Beck Depression Inventory); b/t (between); CES-D (Centers for Epidemiologic Studies-Depression); corr (correlation); dep (depression); T2DM/DM (type 2 diabetes); FFQ (Food Frequency Questionnaire); grp (group); HADS (Hospital Anxiety Depression Scale); HANDS (Harvard Dept Psychiatry/Natl Dep Screening Day Scale); med (medication[s]); mos (months); PA (Physical Activity); PHQ-9 (Nine Symptom Depression checklist of the Patient Health Questionnaire; pt (patient); self-mgmt (self-management); SCL-90R-DEP (Symptom Checklist 90-R-Depression); sig (significant[ly]); SMBG (self-monitoring blood glucose); sxs (symptoms)
The criteria developed for the parent meta-analysis upon which this review is based were used to measure methodological quality for this systematic review: study design, attrition, sample selection, and instrument reliability. Each criterion was measured on a four-point scale resulting in a maximum quality score of 13 and a minimum score of zero. The minimum methodological score accepted for this review was set at three, a low number in order to be purposely inclusive.
Results
Characteristics of the Studies
Samples and settings of primary studies.
Across the 27 studies, sample sizes ranged from 25 to 879, for a total of 7,266 participants overall; 54% was female. All study participants were diagnosed with T2DM and the weighted mean age across studies was 62 years. There were 22 studies9–13,23–26,28–30,32–35,37,38,40,41,43,44 that reported racial/ethnic backgrounds of study participants; 3 studies focused on a single racial/ethnic group (2 studies of Hispanics and 1 study of African Americans).11,13,35 Caucasians made up the majority of the samples, ranging from 42% to 100% across studies, excluding the 3 studies that were focused solely on minority groups. Studies involving mixed ethnic samples tended to have larger numbers of African Americans, followed by smaller numbers of Hispanics, Asian Americans, and Native Americans/American Indians. Classifications such as non-White and non-Hispanic were also used. Mean glycosylated hemoglobin levels (A1C) ranged from 6.9% to 9.4% across the 15 studies in which this measure was reported;9–13,23,24,26,28,30,31,33–35,39 mean BMI, reported in only 9 studies9,12,23,24,26,35,36,38,42 ranged from 29.5 to 36.7; and the prevalence of depression in the samples ranged from 4.5% to 74%. Most (85%) of the studies were conducted in the United States, with the remainder of the studies conducted in Italy, France, Korea, and Pakistan. Studies were conducted in clinics, hospitals, and various community settings (e.g. diabetes centers, health centers, and self-help groups).
The final sample for this review included 21 descriptive and 6 intervention studies. The descriptive studies involved the use of surveys to obtain information on depression and diet and/or PA adherence. Of the six intervention studies, four were randomized controlled trials (RCT),9–12 while two were quasi-experimental.13,44 Overall, 7 of the studies included in the review were dissertations10,24,26,28,30,34,41; 6 descriptive24,26,28,30,34,41 and 1 experimental.10
Instruments.
For depression the most frequently used measures were the Centers for Epidemiologic Studies-Depression (CES-D)11,24,27,28,32,35,41,43 and various versions of the Symptom Depression Checklist of the Patient Health Questionnaire (PHQ9).9,12,13,23,29,33,40,44 Other depression measures included the Medical Outcome Study Short Form Health Survey-Mental Component (SF-12-MC), Short Geriatric Depression scale (SGD), Harvard Department of Psychiatry National Depression Screening Day Scale (HANDS), Hospital Anxiety and Depression Scale (HAD), and Beck Depression Inventory (BDI, BDI-II). One study36 used a composite depression score involving self-reported use of antidepressant medication and use of psychological counseling. Two descriptive studies31,35 and one intervention study10 used secondary measures to validate the primary depression scales included chart reviews31,35 or the Symptom Checklist 90-R-Depression.10
There were 7 different dietary measures used across the 27 studies: the Diabetes Dietary Satisfaction and Outcomes Measure (DDSOM), Summary of Diabetes Self-Care Activities (SDSCA), Diabetes Activity Questionnaire, Food Frequency Questionnaire (FFQ), 24-hour recall, Starting Conversation Scale, and author-derived measures or self-reported dietary intake. The SDSCA scale was used in 12 studies.10,12,13,24,26,28,29,32,37,38,40,44 The second most frequently used measurements were the author-derived measures or self-report9,27,30,33,39,42,43 followed by the FFQ.25,35,36 Only 1 study34 did not measure or evaluate dietary activity and focused on PA alone.
PA was measured using 9 different scales: the DDSOM, SDSCA, Stages of Change for exercise, International Physical Activity Questionnaire, Community Health Activities Model Program for Seniors Physical Activity Questionnaire, Diabetes Activity Questionnaire, Older Americans Resources and Services Multidimensional Functional Assessment Questionnaire, Community Healthy Activities Model Program for Seniors questionnaire, and author-derived self-reported PA. The most frequently used PA measures were the SDSCA scale,10,12,13,24,26,28,29,32,37,38,40,44 followed by the author-derived self-report.9,30,33,39,42 Only one study did not measure PA.43 Intervention studies evaluated intervention effects on depression, A1C, and dietary and/or PA adherence. One intervention study10 focused on the associations of depression with A1C, diet, and PA.
Study quality.
The quality of each study was assessed according to four criteria: study design, attrition, sample selection, and instrument reliability. Most (21) of the studies included in this review were descriptive or predictive in nature. Attrition rates ranged from 0 to 49%. Sample selection coding criteria were based on the number of settings from which the sample was selected and whether the sample was a random or convenience sample. Many of the studies involved convenience sampling. Instrument reliability was based on whether the study reported the reliability of the data collection instrument(s) used. The two studies that scored highest on quality criteria, a randomized controlled trial and a predictive study,12,33 reported low attrition rates, used random samples, and provided acceptable levels of instrument reliabilities.
Intervention characteristics.
Of the six intervention9–13,44 studies in this review, three10,11,13 involved interventions targeting diabetes treatment alone; three9,12,44 targeted both depression and diabetes self-care education. None of the interventions focused on the treatment of depression alone. Diabetes interventions included diabetes self-care education delivered in a clinic, community center, or home setting (via telephone) and conducted by community health workers, registered nurses, and/or registered dietitians. In general, interventions included typical approaches to teaching self-management skills and augmenting these activities with individualized coaching, cultural adaptation, or some form of case management.
Relationship Between Depression and Adherence
Twenty of the 21 descriptive studies described a relationship between depression and dietary adherence; 2 showed no relationships and the remaining studies showed a negative relationship. Thirty-two percent of these studies provided correlations between depression and dietary adherence, ranging from −0.21 to −0.53. Of the 15 studies that examined the relationship between depression and PA, 2 showed no relationship and the rest showed a negative relationship, ranging from −0.17 to −0.46.
Only two of the six intervention studies examined relationships between depression and adherence variables; neither found a significant relationship. Of the three studies that focused on a diabetes treatment intervention, only one measured the association between depression and dietary adherence and found no relationship. Of the three studies that focused the interventions both on diabetes self-management education and treatment of depression, only one examined the relationship between depression and dietary adherence and depression and PA adherence, reporting negative relationships between each.
Discussion
Previous reviews have examined the effects of depression on diabetes self-care adherence.4,14 A recent meta-analysis conducted by Gonzalez et al.14 showed that the effect of depression on adherence varied across self-care activities but the strongest effect was on missed medical appointments. Gonzalez et al.14 also showed a significant relationship between depression and non-adherence to self-care behaviors. The results of the review reported here support the findings that depression is associated with lower adherence to diabetes self-care behaviors, primarily demonstrated in the descriptive studies included in this review. Few intervention studies, only two in this review, have examined the effect of the treatment of depression and/or diabetes education on diabetes self-care adherence.
Egede et al.,4 Katon,9 and van der Felt-Cornelis15 suggest that interventions should address depression and diabetes self-care skills in order to improve diabetes outcomes including metabolic control. Markowitz et al.46 conducted a review of diabetes and depression in persons with type 1 or type 2 diabetes to determine how treatment of depression affected metabolic control. The authors indicated that few studies have focused on treating depression and the mediating pathways that may explain effects of depression on A1C, in particular, such as adherence to recommended self-care behaviors. Their review included only one study46 that examined the effect of depression treatment on both self-care adherence (blood glucose monitoring) and diabetes outcomes (A1C). They concluded that future intervention studies should focus on the effects of combined treatments — strategies to foster diabetes self-care adherence plus treatment for depression — on achieving significant improvements in depression and glycemic control.
Given the documented prevalence of depression in persons with T2DM, intervention studies should include treatments for depression along with the usual focus on promoting self-care behaviors and adherence to improvements in dietary intake and physical activity, in particular. Our findings in this review are consistent with those of Markowitz et al.46 Studies included in this review did not demonstrate an increased focus on treating depression to improve diabetes outcomes. Therefore, the need continues for more intervention studies that explore the direct relationship between treatment of depression and these two key self-care behaviors.
In addition to more intervention studies, there is also a need for more qualitative studies that explore patients’ and health care providers’ perceptions of treating both depression and promoting adherence. The need for qualitative studies in minority groups is particularly significant, because individual ethnic groups may experience depression symptomatology differently.47 Based on individual and/or collective perceptions of depression of a given racial/ethnic group, preferred treatments for depression, as well as for diabetes, could differ.47 Even for this quantitative review, ethnicity was not consistently reported. In the meta-analysis conducted by Gonzalez et al.14 some of the studies did not report ethnicity of their participants but for those in which ethnicities were reported, many, if not most, were Caucasian. Recognizing and addressing racial/ethnic responses to depression should be a goal for future qualitative and quantitative studies in people diagnosed with diabetes and depression.
The six intervention studies used the more common, validated scales for depression: the PHQ,9,12,13,44 CES-D,11 and the BDI-II.10 For the dietary and PA adherence measure, most of the studies used the validated SDSCA10,12,13,44 scale for diabetes adherence. Even though these scales collect self-reported adherence data, which can result in biased information,27 they have been deemed both reliable and valid. However, intervention studies9,11 also included 24-hour dietary recall and self-reported days of following guidelines to measure dietary adherence, both of which can be less reliable. There was more consistency across descriptive studies than intervention studies in the measures that were used. Consistent use of validated measures for lifestyle behaviors, specifically for intervention studies, enables better cross-study comparisons of interventions and outcomes. Of note, the two studies9,11 that used dietary recall and self-reported days of following guidelines were RCTs; results showed a significant improvement in A1C but no improvement in dietary and PA adherence.
RCTs are considered the gold standard for intervention studies. In this review, the intervention studies yielded conflicting results. Two RCTs11,12 and two quasi-experimental studies13,44 in this review reported a decrease in depression symptoms as a result of an intervention. One quasi-experimental study10 examined the relationship between depression and dietary behaviors and found no relationship. One RCT12 and two quasi-experimental13,44 studies reported significant intervention effects on diet and PA adherence. Two RCTs9,11 and one quasi-experimental10 study reported no significant effects on the two lifestyle changes of diet and PA.
Strengths and Limitations
This review focused on the two main lifestyle behaviors, dietary and PA adherence, that have been demonstrated to have a large impact on health outcomes in T2DM. It has been shown that these two lifestyle changes, especially diet, are important for diabetes prevention and glycemic control; but they are the most challenging lifestyle changes both for persons with diabetes as well as their health care providers. Studies have shown that dietary modifications can improve metabolic control,19,48 decreasing A1C by 2.9%-age points within a 6-month period.49 So, it is only fitting that researchers examine these behavioral mediators when examining diabetes and other comorbidities, such as depression.
There were several limitations of this review that should be noted. First, studies were limited to those reported between the years 2000 to 2012. Secondly, this review included both published and unpublished studies, which can be both a limitation as well as a strength. Inclusion of unpublished studies, such as dissertations, has been criticized because they tend to be of lesser quality.22 However, including only published studies interjects publication bias into the review.22
Conclusions and Implications
The results from this review support previous findings that depression is associated with lower adherence to diabetes self-care, but the few studies of interventions designed to treat depression and improve diet and PA adherence have shown inconsistent results. Future research should focus on examining the specific role of depression in adherence to diet and PA and the potential direct effects of depression treatment on health outcomes in T2DM. The model-testing meta-analysis currently in progress, of which this review is a sub-analysis, will provide information on these issues when completed. If depression indeed is directly related to lower diabetes diet and PA adherence, depression treatment must become a more significant aspect of recommended guidelines for diabetes care.49 Thus, the number of people with diabetes who have undiagnosed or subclinical depression could potentially decrease by improving adherence, which leads to better overall health outcomes.
Acknowledgments
This publication was made possible by grant #5R01NR011450 from the National Institute of Nursing Research (NINR) at the National Institutes of Health to Sharon A. Brown. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of NINR.
Contributor Information
Lisa L. Sumlin, School of Nursing, The University of Texas at Austin.
Theresa J. Garcia, College of Nursing & Health Sciences, Texas A&M University–Corpus Christi.
Sharon A. Brown, Joseph H. Blades Centennial Memorial, Professor of Nursing, School of Nursing, The University of Texas at Austin.
References
- 1.World Health Statistics (2007). http://www.who.int/whosis/whostat2007_10highlights.pdf
- 2.World Health Organization (WHO): Depression (2010). http://www.who.int/mental_health/management/depression/definition/en/
- 3.American Diabetes Association: Living with diabetes (2011). http://www.diabetes.org/living-with-diabetes/women/depression.html
- 4.Egede LE. Effect of depression on self-management behaviors and health outcomes in adults with type 2 diabetes. Curr Diabetes Rev. 2005;1:235–243. [DOI] [PubMed] [Google Scholar]
- 5.Egede LE, Ellis C. Diabetes and depression: Global perspectives. Diabetes Res Clin Pract. 2010;87:302–312. [DOI] [PubMed] [Google Scholar]
- 6.World Health Organization (WHO): Diabetes (2010). http://www.who.int/mediacentre/factsheets/fs312/en/
- 7.Anderson RJ, Freedland KE, Clouse RE, Lustman PJ. The prevalence of comorbid depression in adults with diabetes. Diabetes Care. 2001;24:1069–1078. [DOI] [PubMed] [Google Scholar]
- 8.de Groot M, Aderson R., Freedland KE, Clouse RE, Lustman PJ. Association of depression and diabetes complications: a meta-analysis. Psychosom Med. 2001;63:619–630. [DOI] [PubMed] [Google Scholar]
- 9.Katon WJ, Lin EH, Von Korff M, et al. Collaborative care for patients with depression and chronic illnesses. N Engl J Med. 2010; 363:2611–2620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Munroe CD. Behavioral risk factors, cognitive appraisals, and psychological distress in type 2 diabetes. PhD thesis 2008. [Google Scholar]
- 11.Rosal MC, Olendzki B, Reed GW, Gumieniak O, Scavron J, Ockene I. Diabetes self-management among low-income Spanish-speaking patients: A pilot study. Ann Behav Med. 2005;29:225–235. [DOI] [PubMed] [Google Scholar]
- 12.Sacco WP, Malone JI, Morrison AD, Friedman A, Wells K. Effect of a brief, regular telephone intervention by paraprofessional for type 2 diabetes. J Behav Med. 2009;32: 349–359. [DOI] [PubMed] [Google Scholar]
- 13.Castillo A, Giachell A, Bates R, Concha J, Ramirez V, Sanchez C, Pinsker E, Arrom J. Community-based diabetes education for Latinos: The diabetes empowerment education program. Diabetes Educ. 2010;36:586–94. [DOI] [PubMed] [Google Scholar]
- 14.Gonzalez JS, Peyrot M, McCarl LA, et al. Depression and diabetes treatment nonadherence: A meta-analysis. Diabetes Care. 2008;31:2398–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Katon W, van der Felt-Cornelis C. Treatment of depression in patients with diabetes: Efficacy, effectiveness, and maintenance trials, and new service models. In Katon W, Maj M, Sartorius N, eds. Depression and diabetes. West Sussex, UK: John Wiley & Sons, Ltd.; 2010. [Google Scholar]
- 16.Ali MK, Echouffo-Tcheugui J, Williamson DF. How effective were lifestyle interventions in real-world settings that were modeled on the diabetes prevention program? Health Aff. 2012;31:67–75. [DOI] [PubMed] [Google Scholar]
- 17.The Diabetes Prevention Program (DPP) Research Group. The Diabetes Prevention Program (DPP): Description of lifestyle intervention. Diabetes Care. 2002;25:2165–2171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tuomilehto J, Lindstrom J, Eriksson JG, et al. Finnish Diabetes Prevention Study Group. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N England J Med. 2001;344:1343–1350. [DOI] [PubMed] [Google Scholar]
- 19.Al-Sinani M, Min Y, Ghebremeskel K, Qazaq HS. Effectiveness of and adherence to dietary and lifestyle counseling: Effect on metabolic control in type 2 diabetic Omani patients. Sultan Qaboos Univ Med J. 2010;10:341–349. [PMC free article] [PubMed] [Google Scholar]
- 20.Anderson RM, Funnell MM. Compliance and adherence are dysfunctional concepts in diabetes care. Diabetes Educ. 2000;26:597–604. [DOI] [PubMed] [Google Scholar]
- 21.Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PloS Med. 2009; 6:e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fink A Conducting Research Literature Reviews: From the Internet to Paper. 2nd ed. Thousand Oaks, CA: Sage Publications; 2005;136–144. [Google Scholar]
- 23.Fisher L, Glasgow RE, Strycker LA. The relationship between diabetes distress and clinical depression with glycemic control among patients with type 2 diabetes. Diabetes Care. 2010;33:1034–1036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cypress M Perceptions, goals and health behaviors in Hispanic and non-Hispanic men with type 2 diabetes. PhD Thesis, University of New Mexico. May 2008. [Google Scholar]
- 25.Murata GH, Shah JH, Duckworth WC, Wendel CS, Mohler MJ, Hoffman RM. Food frequency questionnaires results correlate with metabolic control in insulin-treated veterans with type 2 diabetes: The diabetes outcome in veterans study. J Am Diet Assoc. 2004;104:1816–1826. [DOI] [PubMed] [Google Scholar]
- 26.Parekh PI. Depression in adults with diabetes mellitus: Risk factors and relationship to glycemic control. PhD thesis April 2001. [Google Scholar]
- 27.Park H, Hong Y, Lee H, Ha E, Sung Y. Individuals with type 2 diabetes and depressive symptoms exhibited lower adherence with self-care. J Clin Epidemiol. 2004;57:978–984. [DOI] [PubMed] [Google Scholar]
- 28.Rothschild CL. Emotional distress as a key construct in the personal model of diabetes management: associations of fatigue, diabetes-specific distress, and depressive symptomatology with quality of life in type 2 diabetes mellitus. PhD thesis August 2010. [Google Scholar]
- 29.Sacco WP, Wells KJ, Vaughan CA, Friedman A, Perez S, Matthew R. Depression in adults with type 2 diabetes: The role of adherence, body mass index, and self-efficacy. Health Psychol. 2005;24:630–634. [DOI] [PubMed] [Google Scholar]
- 30.Schwartz SS. The role of depression in adherence to treatment in a diabetic self-help group. PhD thesis March 2000. [Google Scholar]
- 31.Ahlgren SS, Shultz JA, Massey LK, Hicks BC, Wysham C. Development of a preliminary diabetes dietary satisfaction and outcome measure for patients with type 2 diabetes. Qual Life Res. 2004; 13:819–832. [DOI] [PubMed] [Google Scholar]
- 32.Bell RA, Andrews JS, Arcury TA, Snively BM, Golden SL, Quandt SA. Depressive symptoms and diabetes self-management among rural older adults. Am J Health Behav. 2010; 34:36–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Daly JM, Hartz AJ, Xu Y, et al. An assessment of attitudes, behaviors and outcomes of patients with type 2 diabetes. J Am Board of Fam Med. 2009;22:280–290. [DOI] [PubMed] [Google Scholar]
- 34.Fisher KL. The effects of distress and depression on exercise behaviors of type 2 diabetics: Applying the transtheoretical model. PhD Thesis 2003. [Google Scholar]
- 35.Gary TL, Crum RM, Copper-Patrick L, Ford D, Brancati FL. Depressive symptoms and metabolic control in African-Americans with type 2 diabetes. Diabetes Care. 2000;23: 23–29. [DOI] [PubMed] [Google Scholar]
- 36.Giugliano F, Maiorino MI, Di Palo C, et al. Adherence to Mediterranean diet and sexual function in women with type 2 diabetes. J Sex Med. 2010;7:1883–1890. [DOI] [PubMed] [Google Scholar]
- 37.Gonzales JS, Safren SA, Delahanty LM, et al. Symptoms of depression prospectively predict poorer self-care in patients with type 2 diabetes. Diabetes Med. 2008;25:1102–1107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gonzalez JS, Safren SA, Cagliero E, et al. Depression, self-care, and medication adherence in type 2 diabetes: relationships across the full range of symptom severity. Diabetes Care. 2007;30:2222–2227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Moreau A, Aroles V, Souweine G, et al. Patient versus general practitioner perception of problems with treatment adherence in type 2 diabetes: from adherence to concordance. Eur J Gen Pract. 2009;15:147–153. [DOI] [PubMed] [Google Scholar]
- 40.Sacco WP, Wells KJ, Friedman A, Matthew R, Perez S, Vaughan CA. Adherence, body mass index, and depression in adults with type 2 diabetes: the mediational role of diabetes symptoms and self-efficacy. Health Psychol. 2007;26:693–700. [DOI] [PubMed] [Google Scholar]
- 41.Tovar EG. Relationships between psychosocial factors and adherence to diet and exercise in adults with type 2 diabetes: a test of a theoretical model. PhD thesis July 2007. [Google Scholar]
- 42.Zuberi SI, Syed EU, Bhatti JA. Association of depression with treatment outcomes in type 2 diabetes mellitus: A cross-sectional study from Karachi, Pakistan. BMC Psychiatry. 2011;11:27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.McKellar JD, Humphreys K, & Piette JD. Depression increases diabetes symptoms by complicating patients’ self-care adherence. Diabetes Educ. 2004;30:485–492. [DOI] [PubMed] [Google Scholar]
- 44.Gilmer TP, Walker C, Johnson ED, Philis-Tsimkas A, Unutzer J. Improving treatment of depression among Latinos with diabetes using Project Dulce and IMPACT. Diabetes Care. 2008;3:1324–1326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lustman PJ, Clouse RE. Depression in diabetic patients: The relationship between mood and glycemic control. J of Diabetes Complications. 2005;19:113–122. [DOI] [PubMed] [Google Scholar]
- 46.Markowitz SM, Gonzalez JS, Wilkinson JL, Safren SA. A review of treating depression in diabetes: emerging findings. Psychosomatics. 2011;52:1–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Held RF, DePue J, Rosen R, et al. Patient and healthcare provider views of depressive symptoms and diabetes in American Somoa. Cultur Divers Ethnic Minor Psychol. 2010;16:461–467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Andrews RC, Cooper AR, Montgomery AA, et al. Diet or diet plus physical activity versus usual care in patients with newly diagnosed type 2 diabetes: the early ACTID randomized controlled trial. Lancet. 2011;378:129–139. [DOI] [PubMed] [Google Scholar]
- 49.American Diabetes Association. Standards of medical care in diabetes−-2011. Diabetes Care. 34(suppl):S11–61. [DOI] [PMC free article] [PubMed] [Google Scholar]


