Abstract
Introduction:
The prevalence of e-cigarette use has increased dramatically in the last decade in the U.S. Understanding the prevalence, patterns of use, and risk factor associations of e-cigarette use in pregnant women is particularly important as this could have potential health implications for the mother and the developing child.
Methods:
Using Behavioral Risk Factor Surveillance System Survey data from 2016 to 2018, adult women of reproductive age (18–49 years) who reported being pregnant (n=7,434) were studied. Self-reported current e-cigarette use was the main exposure. Other measures included combustible cigarette smoking status, and high-risk behaviors (including other tobacco, marijuana, or heavy alcohol use; binge drinking; and others). All analyses were done in 2019.
Results:
Approximately 2.2% of pregnant women reported current e-cigarette use, of whom 0.6% reported daily use. The highest prevalence of e-cigarette use was observed in the youngest age group of pregnant women (3.2%), with 41.7% of all pregnant current users being aged 18–24 years. There was a marked increase in the prevalence of current use of e-cigarettes among pregnant women from 1.9% in 2016 to 3.8% in 2018. Approximately 46% of pregnant current e-cigarette users reported concomitant cigarette smoking. Compared with pregnant never e-cigarette users, pregnant current e-cigarette users had a higher prevalence of other tobacco product use, marijuana use, heavy alcohol intake, binge drinking, and other high-risk behaviors.
Conclusions:
These findings underscore the need to strengthen prevention and policy efforts specifically in the vulnerable subgroup of pregnant women.
INTRODUCTION
Since their introduction into the U.S. market in 2007, awareness about e-cigarettes and their subsequent use has increased, with ever-use of e-cigarettes among adults increasing from 1.8% in 2010 to 15.3% in 2016.1–3 Current use of e-cigarettes among adults has also increased significantly from 0.3% in 2010 to 4.5% in 2016,2,4 affirming the increased popularity of these products.
Although many pregnant smokers are aware of the harms associated with smoking during pregnancy, and are motivated to stop smoking,5,6 there has been an increasing prevalence of use of e-cigarettes among pregnant women, with a sizeable proportion of these women being never smokers, which could potentially be due to the general perception of e-cigarettes as being less harmful than cigarette smoking.1,6–9 Combustible cigarette smoking in pregnancy has declined, with a reduction in prevalence from 14.3% in 2011 to 10.9% in 2015.10 However, the exact prevalence of e-cigarette use among pregnant women is uncertain, with estimates varying widely from 0.6% to 15%, potentially due to the limited sample sizes.7,11–14
Smoking during pregnancy is a major modifiable risk factor for increased fetal and maternal morbidity and mortality, causally associated with increased incidence of low birth weight, preterm birth, stillbirth, ectopic pregnancy, placental abruption, and sudden infant death syndrome.6–8,15–17 It could also have lifelong implications for the fetus post-delivery, as it has been associated with increased incidence of respiratory illness and reduced lung function,17–20 as well as negative behavioral outcomes (including attention–deficit hyperactivity disorder, conduct disorder, and antisocial behavior) in these children after birth, often persisting into adulthood.17,20,21 With more than 4,000 chemicals present in cigarette smoke, it is difficult to isolate the effect of nicotine20; however, several animal studies have linked some of these adverse outcomes to the nicotine present in cigarettes.18,20–22 Given that nicotine concentrations in e-cigarettes are as high as 59 mg/mL in some devices,23 their use in pregnant women is concerning. In addition, studies have shown a correlation between the use of e-cigarettes and other high-risk behaviors such as alcohol use, marijuana use, and sensation-seeking behaviors, which may increase overall risk of negative outcomes in pregnancy.24–26
Considering the vulnerability of pregnant women and the developing fetus, updated, high-quality, population-level data are needed to better understand the burden of e-cigarette use in pregnant women, to inform further regulation of e-cigarettes and the creation of public health campaigns targeting this subpopulation. Therefore, using the nationally representative Behavioral Risk Factor Surveillance System (BRFSS) surveys from 2016 to 2018, this study aims to describe the use of e-cigarettes among pregnant women in the U.S. In addition, this study assesses the trends of e-cigarette use in this 3-year period and examines the relationship between e-cigarette use and other high-risk behaviors including cigarette smoking, other tobacco use, alcohol and marijuana use, binge drinking, and intravenous drug use.
METHODS
The BRFSS is the largest health survey system in the world, established by the Centers for Disease Control and Prevention to collect information on the health-related risk behaviors, chronic health conditions, and use of preventive services among U.S residents aged >18 years from all 50 states as well as the District of Columbia and three U.S territories.27 Cross-sectional BRFSS survey data from 2016 to 2018 were pooled and analyzed.
The BRFSS is a publicly available data set with de-identified data, and consequently the present analysis did not require IRB review.
Study Population
There was a total of 1,373,755 participants in the BRFSS surveys from 2016 to 2018. Of these, 219,925 adult women of reproductive age (18–49 years) with information on their pregnancy status were included. Participants were categorized as pregnant or not pregnant based on their response to the question: To your knowledge, are you now pregnant? All further analyses were conducted in the subgroup of women who reported being pregnant (n=7,434).
Measures
Participants were categorized as ever e-cigarette users who responded yes to the question: Have you ever used an e-cigarette or other electronic vaping product, even just one time in your entire life? They were then further classified into current/former user based on their response to the question: Do you now use e-cigarettes or other electronic vaping products every day, some days, or not at all? Participants who reported use every day or some days were classified as current users, and then subclassified as daily (“everyday”) or occasional users (“somedays”).
Participants were categorized as ever or never cigarette smokers based on their response to the question: Have you smoked at least 100 cigarettes in your entire life? Ever smokers were further categorized as current/former smokers based on their response to the question: Do you now smoke cigarettes every day, some days, or not at all?
Other tobacco use was defined as those who currently use chewing tobacco, snuff, or snus; heavy alcohol use as having more than seven drinks per week; binge drinking as having four or more drinks on one occasion; and marijuana use as using marijuana on ≥1 days in the last 30 days. Other high-risk behaviors is a composite variable in BRFSS defined as those who in the past year, had injected any drugs other than those prescribed, been treated for any sexually transmitted disease, or given or received money or drugs in exchange for sex.
Demographic factors included age, race/ethnicity, marital status, education level, employment, and metropolitan area. Income was defined using federal poverty cut offs for each state, considering the number of adults and children in the home. All variables were self-reported.
Statistical Analysis
To ensure representativeness of the data, the BRFSS uses design weighting and iterative proportional fitting.28 Sampling design elements and design weights were applied to all analyses. Proportions and weighted percentages in each subgroup were obtained using the “svy: subpop” command.
The overall analytic goal was to describe the prevalence and trends of e-cigarette use in pregnant women. Sociodemographic factors and high-risk behaviors were examined across all respondents by pregnancy status and reported as weighted percentages. E-cigarette use prevalence was then examined in the overall population and among subcategories defined by pregnancy status and age. Trends in e-cigarette use prevalence were assessed from 2016 to 2018 and tested using logistic regression with survey year as a continuous variable.
Among pregnant women, the overall prevalence of dual use of e-cigarettes and combustible cigarette smoking was examined, with further analysis stratified by BRFSS age categories. To further assess polytobacco use patterns among e-cigarette using pregnant women, cigarette smoking patterns were assessed by e-cigarette use status, and vice-versa.
All analyses were conducted using Stata, version 15.1 with the significance level set at p=0.05 (two-sided). Data were analyzed in 2019.
RESULTS
There were 7,434 pregnant adult women of reproductive age (18–49 years) within the study population. About 54.2% of participants were aged 18–29 years. Almost half were white, 56.5% were married, 57.6% currently employed, and 55.8% were living >200% above the poverty line (Table 1). Compared with non-pregnant women, pregnant women were more likely to be younger and married and other sociodemographic characteristics were distributed similarly across the two groups (Appendix Table 1).
Table 1.
Demographic Characteristics of Pregnant Women in the BRFSS
| Characteristics | Currently pregnant (n=7,434) Crude (95% CI) |
|---|---|
| Age, years | |
| 18–24 | 28.2 (26.3, 30.1) |
| 25–29 | 26.0 (24.3, 27.8) |
| 30–34 | 27.8 (26.0, 29.6) |
| 35–49 | 18.0 (16.5, 19.6) |
| Race | |
| White | 49.3 (47.3, 51.4) |
| Black or African American | 12.7 (11.5, 14.1) |
| Hispanic | 27.0 (25.0, 29.0) |
| Other | 11.0 (9.6, 12.6) |
| Marital status | |
| Married | 56.5 (54.5, 58.5) |
| Divorced | 5.8 (4.9, 6.7) |
| Widowed | 0.9 (0.5, 1.9) |
| Single | 36.8 (34.8, 38.8) |
| Education | |
| Less than high school | 15.6 (13.9, 17.5) |
| High school/Some college | 53.7 (51.7, 55.8) |
| College graduate | 30.6 (28.9, 32.4) |
| Employment status | |
| Employed | 57.6 (55.5, 59.6) |
| Unemployed | 36.1 (34.1, 38.2) |
| Student | 6.3 (5.4, 7.4) |
| Retired | 0.0 (0.0, 0.1) |
| Income | |
| Below poverty line | 22.9 (21.1, 24.8) |
| Within 100%–200% above poverty l | 21.3 (19.5, 23.2) |
| >200% above poverty | 55.8 (53.6, 57.9) |
| Metropolitan area | |
| Center city | 30.6 (26.0, 35.6) |
| Same county as center city | 25.2 (19.5, 31.8) |
| Suburban county | 22.5 (18.0, 27.6) |
| Outside metropolitan area | 21.8 (18.3, 25.7) |
| Smoking status | |
| Current | 7.0 (6.1, 8.0) |
| Former | 18.6 (17.1, 20.3) |
| Never | 74.4 (72.6, 76.1) |
| Other tobacco usea | 0.7 (0.5, 1.0) |
| Heavy alcohol use | 1.7 (1.3, 2.4) |
| Marijuana use | 5.9 (3.7, 9.2) |
| Binge drinking | 3.8 (3.1, 4.7) |
| Other high risk behaviorsb | 9.2 (8.0, 10.6) |
| E-cigarette use, % | |
| Current | 2.2 (1.7, 2.8) |
| Daily | 0.6 (0.4, 0.9) |
| Occasional | 1.5 (1.1, 2.1) |
| Former | 21.0 (19.3, 22.9) |
| Never | 76.8 (74.9, 78.6) |
Notes: Results presented as % (95% CI). Weighted percentages are reported. n is the unweighted sample size in the dataset.
Defined as current use of chewing tobacco, snuff, or snus every day or some days.
Individuals who injected any drugs other than those prescribed in the last year, been treated for any sexually transmitted disease in the past year, or given or received money or drugs in exchange for sex in the past year.
BRFSS, Behavioral Risk Factor Surveillance System.
Among pregnant women, 7.0% reported current cigarette smoking, 0.7% used other tobacco products, 5.9% used marijuana, 1.7% drank alcohol heavily, 3.8% reported binge drinking in the last 30 days, and 9.2% reported other high-risk behaviors (Table 1).
Current e-cigarette use prevalence among pregnant women was 2.2%, with 0.6% of pregnant women reporting daily use. Additionally, approximately 21.0% reported former e-cigarette use (Table 1). The prevalence of current e-cigarette use was highest among those aged 18–24 years (3.2%), followed by those aged 25–29 years (2.3%) (Appendix Table 3).
The prevalence of current e-cigarette use among pregnant women was 1.9% in 2016, 1.6% in 2017, and 3.8% in 2018, corresponding to an absolute prevalence difference of −0.2% from 2016 to 2017 (p=0.66) and 2.2% from 2017 to 2018 (p=0.009). A similar increase in the prevalence of use of e-cigarettes was observed among non-pregnant women (Figure 1, Appendix Table 2).
Figure 1.
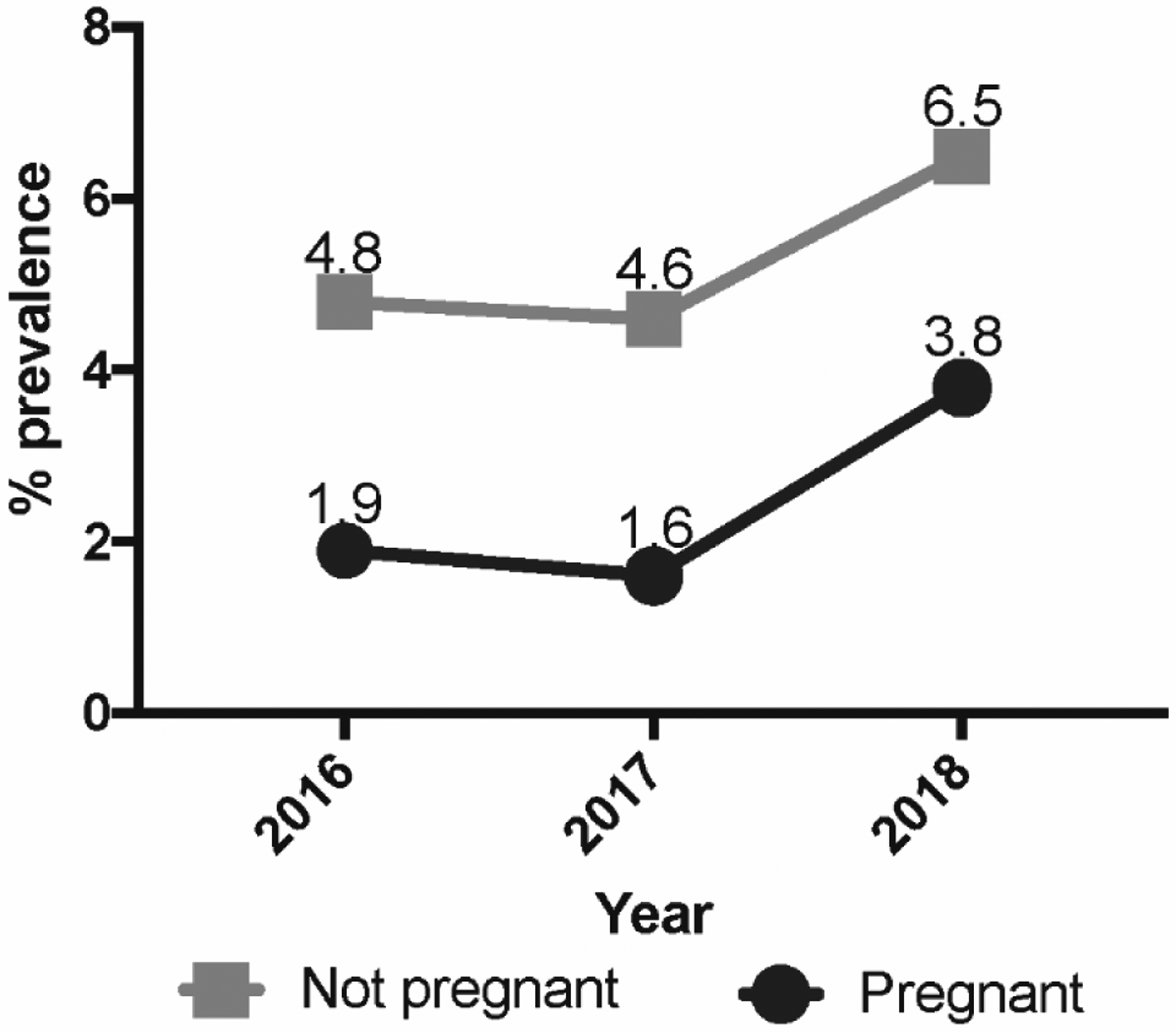
Trends in e-cigarette use among adult pregnant women, 2016 to 2018.
The majority of pregnant e-cigarette users were young (69.2% aged <30 years), white (63.3%), single (57.6%), and employed (61.7%) (Appendix Table 4).
The overall prevalence of dual use of e-cigarettes and cigarette smoking among pregnant women was 1.1%. Examining subcategories defined by age, pregnant women aged 35–49 years had the highest prevalence of dual use (1.5%) (Appendix Figure 1).
Among current e-cigarette users, 46.3% also reported to be current cigarette smokers, whereas 30.3% had never smoked combustible cigarettes (Figure 2A, Appendix Table 5).
Figure 2.
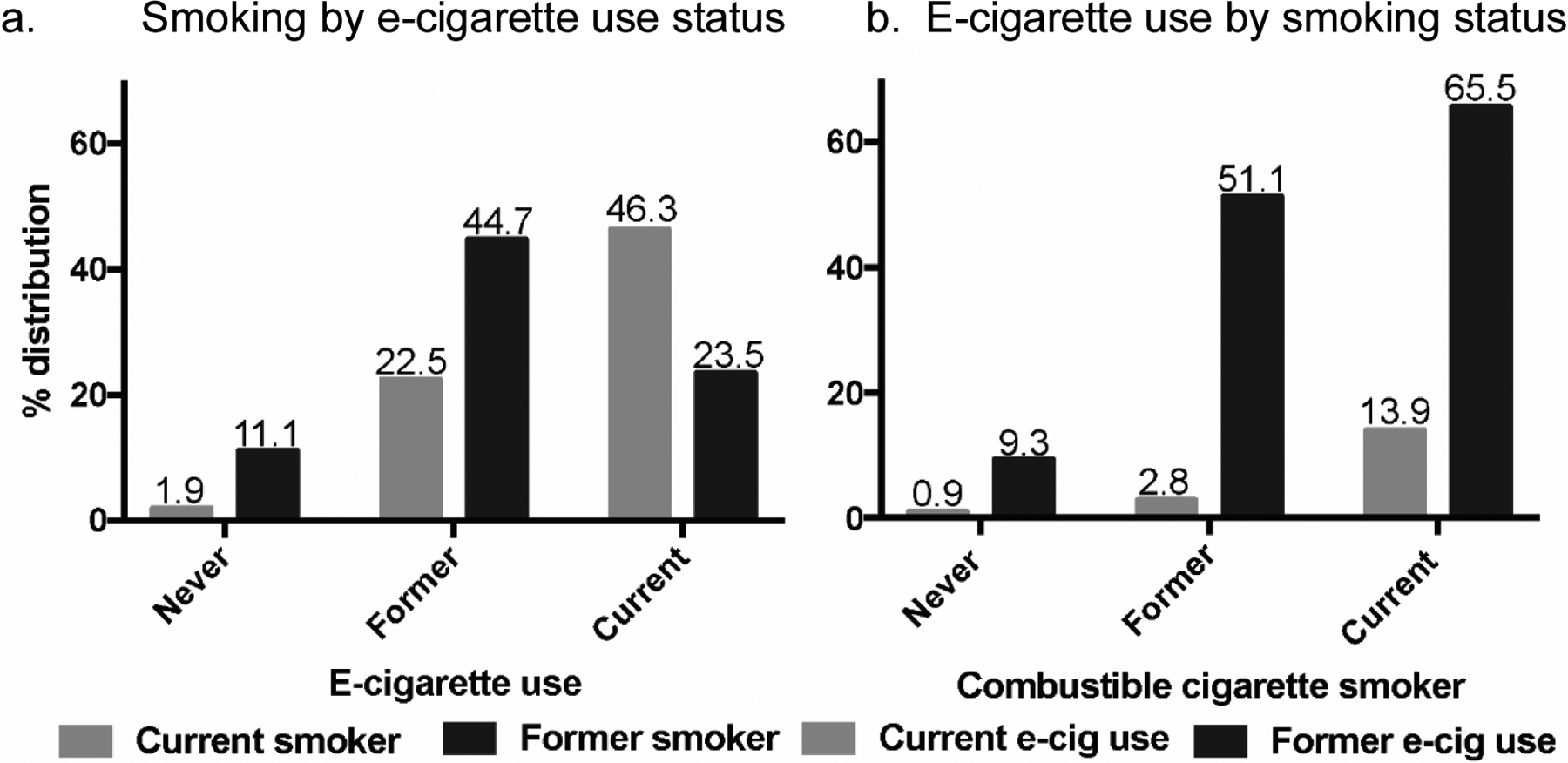
E-cigarette use and smoking patterns among pregnant women.
Among current combustible cigarette smoking pregnant women, 13.9% were also current users of e-cigarettes. Approximately 51.1% of former smokers were former e-cigarette users (Figure 2B, Appendix Table 6).
Among pregnant current e-cigarette users, 3.6% reported other tobacco use, compared with 0.5% of never users. Of the pregnant current e-cigarette users, 46.8% reported marijuana use, 12.0% were heavy alcohol users, 24.1% reported binge drinking in the past 30 days, and 22.6% reported other high-risk behaviors. Among never users, the percentages of pregnant women who reported similar behaviors were 3.1%, 1.3%, 2.6%, and 6.0% respectively (Figure 3, Appendix Table 7).
Figure 3.
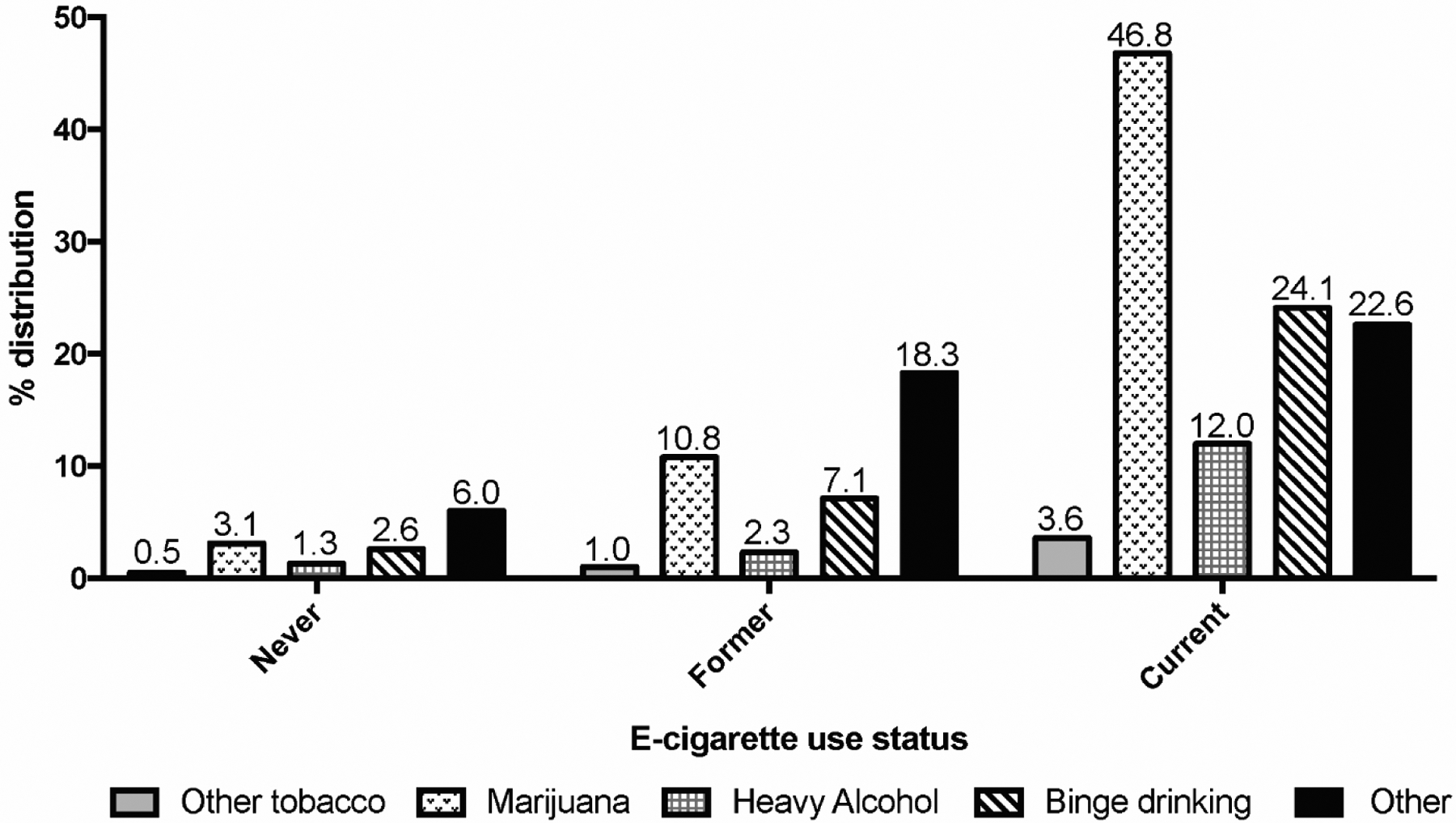
Prevalence of high-risk behaviors among pregnant women by e-cigarette use status.
DISCUSSION
Using BRFSS, the largest nationally representative data on e-cigarette use to date, this study found that e-cigarette use during pregnancy is substantial, with a prevalence of 2.2% in this cohort. Given that there were approximately 4 million live births annually in the U.S. in 2016 and 2017,29 this translates to approximately 88,000 babies potentially exposed to e-cigarettes each year in utero. Also concerning is that the prevalence of e-cigarette use doubled between 2016 and 2018 in pregnant adult women, with about 30% of pregnant current e-cigarette users having never smoked combustible cigarettes. This is concerning as it shows that cigarette-naïve women have taken up e-cigarettes for reasons other than cessation, exposing their fetuses to the potential harms associated with e-cigarettes.
The overall prevalence in this study differs somewhat from estimates obtained in the Population Assessment of Tobacco and Health Survey and in the National Health Interview Survey (NHIS), where the prevalence of current e-cigarette use among pregnant women were reported as 4.9% and 3.3% respectively.12,13 This could be due to the slightly different age demographics of the women included in the studies, difference in sampling methodology, and a chance variation with small samples sizes, as there are 7,434 women in the BRFSS compared to 388 in the Population Assessment of Tobacco and Health Survey and 1,071 in the National Health Interview Survey.
Approximately 70% of pregnant e-cigarette users were aged <30 years, with the highest prevalence of current use reported among the youngest age group of 18–24 years (3.2%). These observations are similar to other studies which show a decrease in the odds of using e-cigarettes with increasing age,30 and are reflective of the distribution of use of e-cigarettes in the general population, with the youngest age group having the highest burden of use.3,31
E-cigarettes contain nicotine, as well as propylene glycol and glycerin delivered in an aerosol vapor.7,23,32,33 They also contain potentially harmful volatile organic compounds (e.g., benzene) and heavy metals (e.g., lead), albeit at lower levels than in cigarette smoke.32,34,35 Nicotine has been established to be a highly addictive substance that readily crosses the placenta into the fetus, where it may have teratogenic effects, causing neurodevelopmental and pulmonary abnormalities.1,6,7,32,35 Additionally, formaldehyde and acrolein, present in e-cigarette aerosols, have been linked with DNA damage and mutagenesis,32 and flavoring chemicals, including diacetyl and benzaldehyde, have been found to be cytotoxic to human embryonic stem cells and pulmonary fibroblasts,36 and associated with respiratory disease when inhaled.32,35 Highlighting the potential dangers of e-cigarette use, the 2016 report of the Surgeon General stated that, “The use of products containing nicotine poses dangers to youth, pregnant women, and fetuses. The use of products containing nicotine in any form among youth, including in e-cigarettes, is unsafe.”35 Furthermore, in utero fetal exposure to nicotine has been associated with long-term adverse respiratory and neurobehavioral effects that could persist into adulthood.18,21
Among pregnant combustible cigarette smokers in this study, a larger proportion were current or former users of e-cigarettes compared with never smokers. In addition, almost half of current e-cigarette users reported current cigarette smoking. Several studies have shown that current smokers are more likely to have tried or currently use e-cigarettes than people who never smoked,37,38 and other studies speculate that many pregnant e-cigarette users might be cigarette smokers who started using e-cigarettes when they discovered they were pregnant in a bid to stop or reduce their cigarette smoking.9 This could be attributed to the assumption that e-cigarettes are a safer alternative to cigarette smoking.1,7,9,39,40 However, many e-cigarette users continue to smoke combustible cigarettes, and the concomitant use of e-cigarettes has been associated with higher odds of nicotine dependence and long-term dual use.30,41
The overall prevalence of dual use of e-cigarettes and cigarette smoking among pregnant women in this study was 1.1%, and interestingly, the age group with the highest prevalence of dual use was the oldest age group of 35–49 years. Although there is limited information on the dual use prevalence in pregnancy, this observation is contrary to studies that find the highest burden of dual use among younger age groups.9,40 Dual use patterns are interesting as they could be interpreted from different perspectives. Although some studies suggest that a subgroup of highly motivated pregnant smokers who are aware that smoking is harmful to their babies take up e-cigarettes as a means of quitting smoking,16,40,42 others deem dual use to be more indicative of higher levels of nicotine dependence.43,44
The current position of the American College of Obstetricians and Gynecologists is that nicotine exposure of any form is a significant health risk for the developing fetal brain and lungs, and that e-cigarettes have not been proven to have any effect on smoking cessation.45 In addition, given the limited data available on the health effects of e-cigarettes, their use in pregnant women is strongly discouraged.45 The U.S. Preventive Services Task Force also reiterates this, recommending behavioral interventions and proven pharmacological interventions to aid smoking cessation instead.46 However, it is interesting to note that despite the public health messages on e-cigarette use, the prevalence trends show an increase in e-cigarette use among pregnant women from 2016 to 2018, with a more drastic increase observed from 2017 to 2018 among pregnant women, compared with non-pregnant women. These findings are reflective of trends observed in the general population, with an increase in use of e-cigarettes from 2017 to 2018, particularly among the younger population.31 This suggests that more aggressive public health campaigns concerning the potential harms associated with e-cigarette use need to be directed at vulnerable subpopulations.
Associations have been observed between marijuana and alcohol use and adverse fetal outcomes such as low birth weight, shorter birth length, increased rate of premature birth, and neurocognitive developmental impairment.47–49 E-cigarette use has been linked to an increased incidence of marijuana and alcohol use, and other high-risk behaviors including risky sexual behavior,26,50–52 which could compound the negative effects of these behaviors on fetal outcomes. This study confirms these associations, as pregnant current e-cigarette users had the highest prevalence of use of other tobacco products and marijuana, heavy alcohol intake, binge drinking, and other high-risk behaviors, including injection drug use, treatment for sexually transmitted diseases in the past year, and exchanging sex for drugs or money. Never users had the lowest prevalence of these behaviors. This relationship could be partially explained by the association between e-cigarette use and the personality trait of sensation seeking, where individuals seek experiences that fuel their desire for varied sensations and experiences.53–55
The increase in e-cigarette use among pregnant women as well as the higher risk of concomitant high-risk behaviors warrant close attention by regulatory agencies, given their interest in e-cigarette use patterns in vulnerable populations.56 It is important to monitor the content of e-cigarette advertisements, necessitating them to highlight the potential dangers associated with their use to vulnerable individuals such as pregnant women. It is also critical to ensure that the potential harms of e-cigarette use on fetal health are clearly labeled on e-cigarette packages. In addition, this study provides justification to conduct longitudinal studies to explore maternal and fetal health effects of e-cigarette use in pregnancy, as well as long-term outcomes in offspring born to these women. This study will also support aggressive public health education strategies to reduce e-cigarette use in pregnancy and could also inform clinical practice, encouraging physicians to dedicate more time to asking pregnant women about e-cigarette use, and counseling and referring them for help when needed.
Limitations
This study has a few limitations. It is cross-sectional, and thus no directionality of use of e-cigarettes and traditional cigarettes or other high-risk behaviors could be ascertained. There were no data available on duration and intensity of e-cigarette use, and it is difficult to tell to what degree dual use prevalence might capture active quit attempts or if current use spanned the pregnancy period. Also, recall bias might influence e-cigarette use reporting, leading to an underestimation of e-cigarette use prevalence, and social desirability bias might lead to an under-reporting of other high-risk behaviors in pregnancy. Lastly, other high-risk behaviors were defined based on behavior within the past year for each participant and not restricted to the time of pregnancy.
Despite these limitations, this study provides the most up-to-date information on the prevalence and use patterns of e-cigarettes and other high-risk behaviors in the unique subgroup of pregnant women.
CONCLUSIONS
The prevalence of e-cigarette use among pregnant women in the U.S. is 2.2%, with a two-fold increase in prevalence of use from 2016 to 2018. The youngest age group (18–24 years) had the highest burden of use. Among pregnant women, current e-cigarette users had a higher prevalence of concurrent cigarette smoking, other tobacco use, marijuana use, heavy alcohol intake, binge drinking, and other high-risk behaviors including intravenous drug use and exchange of sex for money, compared with never e-cigarette users. These findings are important for tobacco regulation strategies and set a baseline for future monitoring of e-cigarette use trends in this select population. They also highlight the need for more longitudinal studies to explore the potential harms of e-cigarette use in pregnancy.
Supplementary Material
ACKNOWLEDGMENTS
This research was supported by the National Heart, Lung, and Blood Institute of the NIH and the Food and Drug Administration Center for Tobacco Products under award numbers P50HL120163 and U54HL120163. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH, Food and Drug Administration, or American Heart Association.
APD has received research grants from the NIH, Astra Zeneca, Ionis Pharmaceuticals, and private donors. He is also a consultant for Radiometer America. EJB has received research grants from the NIH and American Heart Association under award numbers 18SFRN34110082 and 2U54HL120163. All other authors have no financial disclosures or conflicts of interest.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.McCubbin A, Fallin-Bennett A, Barnett J, Ashford K. Perceptions and use of electronic cigarettes in pregnancy. Health Educ Res. 2017;32(1):22‒32. 10.1093/her/cyw059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.McMillen RC, Gottlieb MA, Whitmore Shaefer RM, Winickoff JP, Klein JD. Trends in electronic cigarette use among U.S. adults: use is increasing in both smokers and nonsmokers. Nicotine Tob Res. 2015;17(10):1195‒1202. 10.1093/ntr/ntu213. [DOI] [PubMed] [Google Scholar]
- 3.Bao W, Xu G, Lu J, Snetselaar LG, Wallace RB. Changes in electronic cigarette use among adults in the United States, 2014‒2016. JAMA. 2018;319(19):2039‒2041. 10.1001/jama.2018.4658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mirbolouk M, Charkhchi P, Kianoush S, et al. Prevalence and distribution of e-cigarette use among U.S. adults: Behavioral Risk Factor Surveillance System, 2016. Ann Intern Med. 2018;169(7):429‒438. 10.7326/m17-3440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tong VT, England LJ, Dietz PM, Asare LA. Smoking patterns and use of cessation interventions during pregnancy. Am J Prev Med. 200835(8):327‒333. 10.1016/j.amepre.2008.06.033. [DOI] [PubMed] [Google Scholar]
- 6.England LJ, Tong VT, Koblitz A, Kish-Doto J, Lynch MM, Southwell BG. Perceptions of emerging tobacco products and nicotine replacement therapy among pregnant women and women planning a pregnancy. Prev Med Rep. 2016;4:481‒485. 10.1016/j.pmedr.2016.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Whittington JR, Simmons PM, Phillips AM, et al. The use of electronic cigarettes in pregnancy: a review of the literature. Obstet Gynecol Surv. 2018;73(9):544‒549. 10.1097/ogx.0000000000000595. [DOI] [PubMed] [Google Scholar]
- 8.Mark KS, Farquhar B, Chisolm MS, Coleman-Cowger VH, Terplan M. Knowledge, attitudes, and practice of electronic cigarette use among pregnant women. J Addict Med. 2015;9(4):266‒272. 10.1097/adm.0000000000000128. [DOI] [PubMed] [Google Scholar]
- 9.Wagner NJ, Camerota M, Propper C. Prevalence and perceptions of electronic cigarette use during pregnancy. Matern Child Health J. 2017;21(8):1655‒1661. 10.1007/s10995-016-2257-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hansen AR, Akomolafe TO, McGalliard Z, Belle-Isle L, Zhang J. Striving to meet Healthy People 2020 objectives: trend analysis of maternal smoking. Public Health Rep. 2018;133(6):644‒649. 10.1177/0033354918793120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kurti AN, Redner R, Bunn JY, et al. Examining the relationship between pregnancy and quitting use of tobacco products in a U.S. national sample of women of reproductive age. Prev Med. 2018;117:52‒60. 10.1016/j.ypmed.2018.08.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lopez AA, Redner R, Kurti AN, et al. Tobacco and nicotine delivery product use in a U.S. national sample of women of reproductive age. Prev Med. 2018;117:61‒68. 10.1016/j.ypmed.2018.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Liu B, Xu G, Rong S, et al. National estimates of e-cigarette use among pregnant and nonpregnant women of reproductive age in the United States, 2014‒2017. JAMA Pediatr. 2019;173(6):600‒602. 10.1001/jamapediatrics.2019.0658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kapaya M, D’angelo DV, Tong VT, et al. Use of electronic vapor products before, during, and after pregnancy among women with a recent live birth — Oklahoma and Texas, 2015. MMWR Morb Mortal Wkly Rep. 2019:68(8):189‒194. 10.15585/mmwr.mm6808a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Castles A, Adams EK, Melvin CL, Kelsch C, Boulton ML. Effects of smoking during pregnancy: five meta-analyses. Am J Prev Med. 1999;16(3):208‒215. 10.1016/s0749-3797(98)00089-0. [DOI] [PubMed] [Google Scholar]
- 16.Ioakeimidis N, Vlachopoulos C, Katsi V, Tousoulis D. Smoking cessation strategies in pregnancy: current concepts and controversies. Hellenic J Cardiol. 2019;60(1):11‒15. 10.1016/j.hjc.2018.09.001. [DOI] [PubMed] [Google Scholar]
- 17.HHS. The Health Consequences of Smoking - 50 Years of Progress: A Report of the Surgeon General. www.cdc.gov/tobacco. Accessed January 6, 2020.
- 18.Sekhon HS, Keller JA, Benowitz NL, Spindel ER. Prenatal nicotine exposure alters pulmonary function in newborn rhesus monkeys. Am J Respir Crit Care Med. 2001;164(6):989‒994. 10.1164/ajrccm.164.6.2011097. [DOI] [PubMed] [Google Scholar]
- 19.Banderali G, Martelli A, Landi M, et al. Short and long term health effects of parental tobacco smoking during pregnancy and lactation: a descriptive review. J Transl Med. 2015;13:327. 10.1186/s12967-015-0690-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Li G, Saad S, Oliver BG, Chen H. Heat or burn? Impacts of intrauterine tobacco smoke and e-cigarette vapor exposure on the offspring’s health outcome. Toxics. 2018;6(3):43. 10.3390/toxics6030043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pauly JR, Slotkin TA. Maternal tobacco smoking, nicotine replacement and neurobehavioural development. Acta Paediatr. 2008;97(10):1331‒1337. 10.1111/j.1651-2227.2008.00852.x. [DOI] [PubMed] [Google Scholar]
- 22.Spindel ER, McEvoy CT. The role of nicotine in the effects of maternal smoking during pregnancy on lung development and childhood respiratory disease: implications for dangers of e-cigarettes. Am J Respir Crit Care Med. 2016;193(5):486‒494. 10.1164/rccm.201510-2013pp. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jackler RK, Ramamurthi D. Nicotine arms race: JUUL and the high-nicotine product market. Tob Control. 2019;28(6):623‒628. 10.1136/tobaccocontrol-2018-054796. [DOI] [PubMed] [Google Scholar]
- 24.Cohn A, Villanti A, Richardson A, et al. The association between alcohol, marijuana use, and new and emerging tobacco products in a young adult population. Addict Behav. 2015;48:79‒88. 10.1016/j.addbeh.2015.02.005. [DOI] [PubMed] [Google Scholar]
- 25.Case KR, Harrell MB, Pérez A, et al. The relationships between sensation seeking and a spectrum of e-cigarette use behaviors: cross-sectional and longitudinal analyses specific to Texas adolescents. Addict Behav. 2017;73:151‒157. 10.1016/j.addbeh.2017.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Silveira ML, Conway KP, Green VR, et al. Longitudinal associations between youth tobacco and substance use in waves 1 and 2 of the Population Assessment of Tobacco and Health (PATH) Study. Drug Alcohol Depend. 2018;191:25‒36. 10.1016/j.drugalcdep.2018.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.CDC. BRFSS. www.cdc.gov/brfss/index.html. Accessed September 30, 2019.
- 28.CDC. Weighting the BRFSS Data. www.cdc.gov/brfss/annual_data/2017/pdf/weighting-2017-508.pdf. Accessed September 18, 2019.
- 29.Martin JA, Hamilton BE, Osterman MJK, Driscoll AK, Drake P. Births: final data for 2017. Natl Vital Stat Rep. 2018;67(8):1‒50. www.cdc.gov/nchs/data/nvsr/nvsr67/nvsr67_08-508.pdf. Accessed November 4, 2019. [PubMed] [Google Scholar]
- 30.Ashford K, Wiggins A, Butler K, Ickes M, Rayens MK, Hahn E. E-cigarette use and perceived harm among women of childbearing age who reported tobacco use during the past year. Nurs Res. 2016;65(5):408‒414. 10.1097/nnr.0000000000000176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bao W, Liu B, Du Y, Snetselaar LG, Wallace RB. Electronic cigarette use among young, middle-aged, and older adults in the United States in 2017 and 2018. JAMA Intern Med. 2020;180(2):313‒314. 10.1001/jamainternmed.2019.4957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Greene RM, Pisano MM. Developmental toxicity of e‐cigarette aerosols. Birth Defects Res. 2019;111(17):1294‒1301. 10.1002/bdr2.1571. [DOI] [PubMed] [Google Scholar]
- 33.Rom O, Pecorelli A, Valacchi G, Reznick AZ. Are e-cigarettes a safe and good alternative to cigarette smoking? Ann N Y Acad Sci. 2015;1340(1):65‒74. 10.1111/nyas.12609. [DOI] [PubMed] [Google Scholar]
- 34.Olmedo P, Goessler W, Tanda S, et al. Metal concentrations in e-cigarette liquid and aerosol samples: the contribution of metallic coils. Environ Health Perspect. 2018;126(2):027010. 10.1289/ehp2175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.HHS. E-Cigarette Use Among Youth and Young Adults: A Report of the Surgeon General. Atlanta, GA: HHS, CDC, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2016. www.cdc.gov/tobacco/data_statistics/sgr/e-cigarettes/index.htm. Accessed March 18, 2020. [Google Scholar]
- 36.Behar RZ, Wang Y, Talbot P. Comparing the cytotoxicity of electronic cigarette fluids, aerosols and solvents. Tob Control. 2017;27(3):325‒333. 10.1136/tobaccocontrol-2016-053472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zhu SH, Gamst A, Lee M, Cummins S, Yin L, Zoref L. The use and perception of electronic cigarettes and snus among the U.S. population. PLoS One. 2013;8(10):e79332. 10.1371/journal.pone.0079332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ashford K, Rayens E, Wiggins AT, Rayens MK, Fallin A, Sayre MM. Advertising exposure and use of e-cigarettes among female current and former tobacco users of childbearing age. Public Health Nurs. 2017;34(5):430‒436. 10.1111/phn.12334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Fallin A, Miller A, Assef S, Ashford K. Perceptions of electronic cigarettes among Medicaid-eligible pregnant and postpartum women. J Obstet Gynecol Neonatal Nurs. 2016;45(3):320‒325. 10.1016/j.jogn.2016.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chiang SC, Abroms LC, Cleary SD, Pant I, Doherty L, Krishnan N. E-cigarettes and smoking cessation: a prospective study of a national sample of pregnant smokers. BMC Public Health. 2019;19:964. 10.1186/s12889-019-7299-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Dutra LM, Glantz SA. Electronic cigarettes and conventional cigarette use among US adolescents: a cross-sectional study. JAMA Pediatr. 2014;168(7):610‒617. 10.1001/jamapediatrics.2013.5488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bowker K, Orton S, Cooper S, et al. Views on and experiences of electronic cigarettes: a qualitative study of women who are pregnant or have recently given birth. BMC Pregnancy Childbirth. 2018;18:233. 10.1186/s12884-018-1856-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ashford KB, Chavan NR, Wiggins A, et al. 717: Prenatal electronic cigarette, dual use and nicotine dependency. Am J Obstet Gynecol. 2018;218(1 suppl):S431‒S432. 10.1016/j.ajog.2017.11.248. [DOI] [Google Scholar]
- 44.Clemens M, Cardenas V, Fischbach L, et al. Use of electronic nicotine delivery systems by pregnant women II: hair biomarkers for exposures to nicotine and tobacco-specific nitrosamines. Tob Induc Dis. 2019;17:50. 10.18332/tid/105387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Committee Opinion No. 721 Summary: Smoking Cessation During Pregnancy. Obstet Gynecol. 2017;130(4):929‒930. 10.1097/aog.0000000000002348. [DOI] [PubMed] [Google Scholar]
- 46.U.S. Preventive Services Task Force. Final recommendation statement: tobacco smoking cessation in adults, including pregnant women: behavioral and pharmacotherapy interventions. www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/tobacco-use-in-adults-and-pregnant-women-counseling-and-interventions1. Accessed January 6, 2020.
- 47.Gunn JKL, Rosales CB, Center KE, et al. Prenatal exposure to cannabis and maternal and child health outcomes: a systematic review and meta-analysis. BMJ Open. 2016;6(4):e009986. 10.1136/bmjopen-2015-009986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hayatbakhsh MR, Flenady VJ, Gibbons KS, et al. Birth outcomes associated with cannabis use before and during pregnancy. Pediatr Res. 2012;71(2):215‒219. 10.1038/pr.2011.25. [DOI] [PubMed] [Google Scholar]
- 49.Denny CH, Acero CS, Naimi TS, Kim SY. Consumption of alcohol beverages and binge drinking among pregnant women aged 18–44 years - United States, 2015‒2017. MMWR Morb Mortal Wkly Rep. 2019;68(16):365‒368. 10.15585/mmwr.mm6816a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ghosh TS, Tolliver R, Reidmohr A, Lynch M. Youth vaping and associated risk behaviors - a snapshot of Colorado. N Engl J Med. 2019;380(7):689‒690. 10.1056/nejmc1900830. [DOI] [PubMed] [Google Scholar]
- 51.Berg CJ, Stratton E, Schauer GL, et al. Perceived harm, addictiveness, and social acceptability of tobacco products and marijuana among young adults: marijuana, hookah, and electronic cigarettes win. Subst Use Misuse. 2015;50(1):79‒89. 10.3109/10826084.2014.958857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Oncken C, Ricci KA, Kuo C-L, Dornelas E, Kranzler HR, Sankey HZ. Correlates of electronic cigarettes use before and during pregnancy. Nicotine Tob Res. 2017;19(5):585‒590. 10.1093/ntr/ntw225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Demissie Z, Jones SE, Clayton HB, King BA. Adolescent risk behaviors and use of electronic vapor products and cigarettes. Pediatrics. 2017;139(2):e20162921. 10.1542/peds.2016-2921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Roberti JW. A review of behavioral and biological correlates of sensation seeking. J Res Pers. 2004;38(3):256‒279. 10.1016/S0092-6566(03)00067-9. [DOI] [Google Scholar]
- 55.Hanewinkel R, Isensee B. Risk factors for e-cigarette, conventional cigarette, and dual use in German adolescents: a cohort study. Prev Med. 2015;74:59‒62. 10.1016/j.ypmed.2015.03.006. [DOI] [PubMed] [Google Scholar]
- 56.U.S. Food and Drug Administration. Research Priorities. www.fda.gov/tobacco-products/research/research-priorities. Accessed February 19, 2020.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


