Abstract
Objectives
The aim of this study was to estimate how well the excess mortality reflected the burden of coronavirus disease 2019 (COVID-19)-related deaths during the March–May 2020 COVID-19 outbreak in Stockholm, Sweden, and whether the excess mortality during the outbreak might have resulted in a compensatory reduced mortality after the outbreak.
Methods
Using previous 10-year or 5-year average mortality rates as a baseline, the excess mortality estimates before, during, and after the COVID-19 outbreak in March–May 2020 in Stockholm were compared.
Results
Weekly death estimates revealed that the immediate pre-outbreak and post-outbreak all-cause mortality did not exceed to excess mortality regardless of whether previous 10-year or 5-year average mortality was used. Forty-three days after the start of the outbreak, 74.4% of the total excess mortality was reportedly explained by known COVID-19-related deaths, and the present study reports an update, showing that 15 weeks after the start of the outbreak, the reported COVID-19-related deaths explained >99% of the total excess mortality.
Conclusions
An exceptional outbreak feature of rapid excess mortality was observed. However, no excess but similarly low mortality was observed immediately prior to the outbreak and post-outbreak, thus emphasizing the severity of the first wave of the COVID-19 outbreak in Stockholm.
KEYWORDS: Mortality; SARS-CoV-2; COVID-19; Outbreak, Public health
1. Introduction
Excess all-cause mortality is increasingly being used to monitor the timing and severity of COVID outbreaks; however the COVID-attributable fraction of the all-cause mortality is not always clear (www.euromomo.eu). When calculating weekly excess mortality, fluctuations in mortality rates by calendar year are minimized by calculating a baseline mortality over several years (Ledberg, 2020). As there are also temporal trends in mortality (increased life expectancy), the average mortality estimation cannot use too many years (Ledberg, 2020). The aim of this study was first to assess how well the excess mortality reflected the burden of COVID-19-related deaths during the March–May 2020 COVID-19 outbreak in Stockholm, Sweden, and then to investigate whether the excess mortality during the outbreak might have resulted in a compensatory reduced mortality after the outbreak.
2. Methods
Weekly estimates of mortality in Stockholm for the past 10 years and for the year 2020 were retrieved from EuroStat (https://appsso.eurostat.ec.europa.eu). A 10-year and 5-year average weekly baseline of all-cause mortality was calculated, as described previously (Pimenoff et al., 2020). In addition, reported COVID-19-related weekly deaths were retrieved from the most up-to-date public repository of the Swedish Public Health Agency (www.folkhalsomyndigheten.se).
3. Results
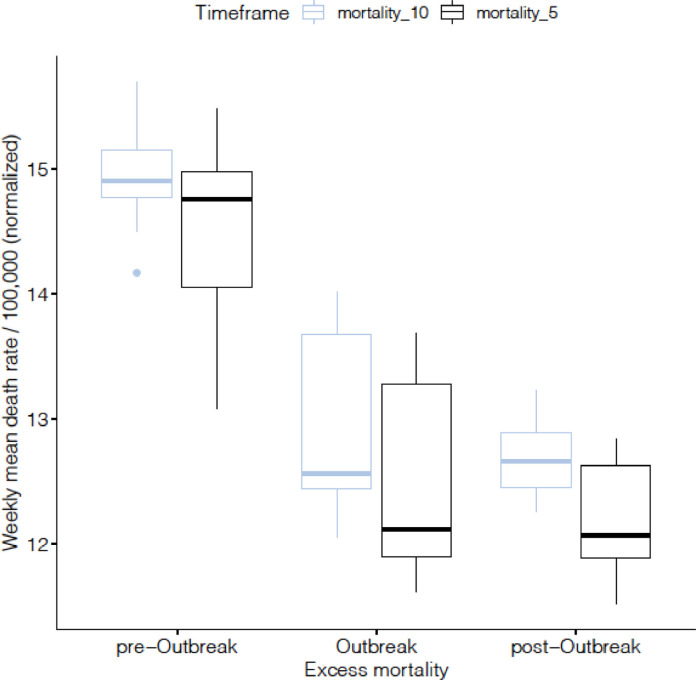
First, an investigation was performed to determine whether the results would be sensitive to whether the previous 5 years or the previous 10 years were used to calculate the average weekly mortality estimates (Figure 1 ). The 10-year averages were slightly but not significantly higher, and a clear seasonal trend was observed. Figure 2 shows the stratified 10-year average all-cause weekly mortality rates per 100 000 inhabitants during three time periods: pre-outbreak (weeks 1–11), outbreak (weeks 12–26), and post-outbreak (weeks 27–42).
Figure 1.
All-cause mortality estimated using 10-year (2010–2019) and 5-year (2015–2019) weekly average mortality estimates. Average all-cause mortality in the previous 10 years (mortality_10: 2010–2019) and previous 5 years (mortality_5: 2015–2019), further split into the following timeframes: pre-outbreak (weeks 1–12); outbreak (weeks 13–27); post-outbreak (weeks 28–42). The point-estimates using the 10-year baseline are somewhat higher (although not statistically significant) than those using the 5-year baseline, but the variability is much less when the 10-year average is used.
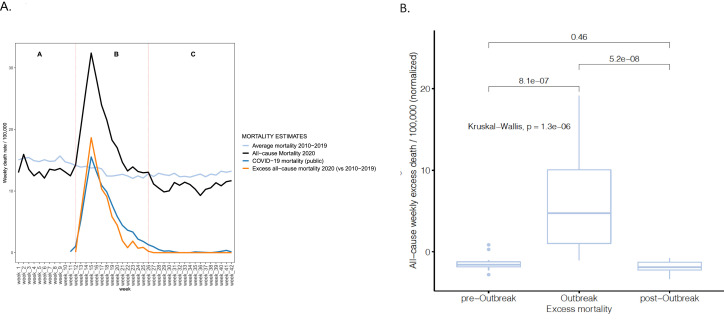
Figure 2.
Mortality during the COVID-19 outbreak, March–May 2020, in Stockholm, Sweden. (A) All-cause, excess, and COVID-19-attributable mortality in weeks 1–42 of 2020 in Stockholm. All-cause mortality in 2020 compared to the average all-cause mortality in the previous 10 years (2010–2019), split into ‘A’ pre-outbreak, ‘B’ outbreak, and ‘C’ post-outbreak timeframes. The 2020 total all-cause mortality exceeds the average of the previous 10 years and becomes excess mortality at the same time as reporting of COVID-19-related deaths started emerging in week 12 and declines below the 10-year average in week 27 (dashed vertical red lines). Excess all-cause mortality is estimated along with the reported COVID-19-related mortality. (B) Total excess mortality differences before (pre-outbreak), during (outbreak), and after (post-outbreak) a major outbreak of COVID-19, using the mean mortality of the last 10 years as a baseline.
The year 2020 weekly all-cause mortality per 100 000 inhabitants in the Stockholm region before the outbreak was slightly lower than the 10-year average mortality, but at the onset of the outbreak in week 12, the reduced mortality was turned into excess mortality at the same time as reporting of COVID-19-related deaths started (Figure 2A). After peaking in week 15 (mortality rate 32.9/100 000 inhabitants), all-cause mortality declined below the 10-year average in week 27 (Figure 2A). The 2020 accumulated weekly all-cause mortality during the outbreak (between weeks 12 and 26) was 46% higher than the 10-year average all-cause mortality for the same timeframe (Figure 2A). Moreover, the number of COVID-19-related deaths (2355 COVID deaths), including the updates notified later in the outbreak, explained more than 99% of the cumulative weekly excess mortality in week 27. To further understand the seasonal trends, estimated excess mortality was compared before, during, and after the March–May 2020 outbreak of COVID-19 in Stockholm, Sweden (Figure 2B). Stratified weekly mortality revealed that the immediate pre-outbreak and post-outbreak all-cause mortality were significantly similar and did not exceed to excess mortality.
4. Discussion
We and others have previously reported that the excess mortality estimates tend to exceed the COVID-19-attributable mortality data (Felix-Cardoso et al., 2020; Woolf et al., 2020), with only 74.4% of the excess mortality being attributable to COVID-related deaths in Stockholm when including the reports that had arrived up to 43 days after the start of the local outbreak (Pimenoff et al., 2020). However, 15 weeks after the start of the outbreak, the reports of COVID-related deaths during the first wave had increased and now explained more than 99% of the excess mortality. This implies that, in agreement with other studies (Ledberg, 2021; Woolf et al., 2020), excess all-cause mortality can give a more timely picture of the burden of outbreaks associated with a substantial increase in mortality rates, such as COVID-19, compared with early reporting of COVID-19-attributable deaths.
However, for a comprehensive view of a local COVID-19 outbreak, an excess mortality measure may be affected by seasonal mortality fluctuations and warrants careful investigation. Indeed, a decrease in the magnitude of mortality fluctuations in Sweden in the 20th century has been associated with significantly high life expectancy in the population (Ledberg, 2020). Hence, the issue of whether the COVID-19-related excess mortality is followed by a compensatory mortality deficit when many frail and elderly in the Swedish population have died is also essential for our understanding of the impact of the pandemic (Woolf et al., 2020). That is, previous reporting estimated that the elderly living in care homes in Stockholm had at least a four-fold increased risk of COVID-19 mortality during the first wave of COVID-19 between March and May 2020 (Brandén et al., 2020). Similarly, the pooled weekly total number of deaths estimated during the first wave of COVID-19 in Sweden showed a more than three-fold higher excess mortality for over 65-year-olds compared to 45–65-year-olds (www.euromomo.eu).
Here, we show that the immediate post-outbreak mortality was similarly as low as the pre-existing, pre-outbreak mortality in Stockholm in 2020 and that this conclusion is not sensitive to the exact methods of calculating the baseline average mortality (Figure 2B). We suggest that these results may also be partly explained by the disappearance of other relevant respiratory infections after March 2020 due to social distancing and increased hygiene measures implemented at the beginning of the pandemic. Moreover, a recent report characterizing the 15 most severe all-cause mortality outbreaks in Sweden since the 19th century – including COVID-19 – showed that the influenza A virus outbreak in 1918 and the COVID-19 outbreak have been exceptional compared to any other severe outbreak observed in Sweden: excess mortality increased rapidly to a high magnitude in both outbreaks and eventually both sustained longer than 3 months (Ledberg, 2021). Comparing the excess mortality estimates of the outbreaks showed that mortality during the 1918 ‘Spanish flu’ influenza A outbreak was likely at least 13-fold higher than that during COVID-19 (Ledberg, 2021). However, improved medical treatments and better hygiene, particularly since the early 20th century, make it difficult to directly compare the severity of the two outbreaks.
In summary, excess mortality was compared before, during, and after the March–May 2020 outbreak of COVID-19 in Stockholm, Sweden. The immediate post-outbreak low mortality was similar to the pre-existing, pre-outbreak low mortality in 2020, thus emphasizing the severity of the COVID-19 outbreak. Furthermore, excess all-cause mortality represents a timely measure of the death burden of the COVID-19 outbreak, which may not always be available solely from direct disease-attributable death reports.
Declarations
Funding: This research was financially supported by an unrestricted donation from Creades. The funder did not have any role in the interpretation of the results, or in the preparation of this manuscript.
Ethical approval: Ethical approval was not needed, as only publicly available mortality and COVID-19-related data from www.folkhalsomyndigheten.se and https://appsso.eurostat.ec.europa.eu were used.
Conflict of interest: The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- Brandén M, Aradhya S, Kolk M, Härkönen J, Drefahl S, Malmberg B, et al. Residential context and COVID-19 mortality among adults aged 70 years and older in Stockholm: a population-based, observational study using individual-level data. Lancet Heal Longev. 2020;1:e80–e88. doi: 10.1016/S2666-7568(20)30016-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Felix-Cardoso J, Vasconcelos H, Rodrigues P, Cruz-Correia R. Excess mortality during COVID-19 in five European countries and a critique of mortality analysis data. MedRxiv. 2020 doi: 10.1101/2020.04.28.20083147. 2020.04.28.20083147. [DOI] [Google Scholar]
- Ledberg A. Mortality of the COVID-19 Outbreak in Sweden in Relation to Previous Severe Disease Outbreaks. Front Public Heal. 2021;9 doi: 10.3389/fpubh.2021.579948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ledberg A. A large decrease in the magnitude of seasonal fluctuations in mortality among elderly explains part of the increase in longevity in Sweden during 20th century. BMC Public Health. 2020;20:1674. doi: 10.1186/s12889-020-09749-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pimenoff VN, Elfström M, Baussano I, Björnstedt M, Dillner J. Estimating total excess mortality during a COVID-19 outbreak in Stockholm, Sweden. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa1593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woolf SH, Chapman DA, Sabo RT, Weinberger DM, Hill L. Excess Deaths From COVID-19 and Other Causes, March-April 2020. JAMA. 2020 doi: 10.1001/jama.2020.11787. [DOI] [PMC free article] [PubMed] [Google Scholar]