Abstract
The coronavirus disease 2019 (COVID-19) pandemic has had a profound effect on the delivery of vascular surgery to patients around the world. In order to conserve resources and reduce the risk of COVID-19 infection, many institutions have postponed or cancelled surgical procedures. In this scoping review, we aim to review current literature and recapitulate the significant changes in elective and emergency vascular surgery during the COVID-19 pandemic. We conducted this scoping review in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analysis extension for Scoping Reviews. We included all articles that had reported the effects of the COVID-19 pandemic on elective or emergency vascular surgery. A total of 28 articles were included in this scoping review. We identified eight distinct themes that were relevant to our study topic. We report global, regional, and local data on vascular surgical cases. We also discuss the adoption of vascular surgery triage systems, emergence of global collaborative vascular surgery research groups, increased use of endovascular techniques and locoregional anesthesia, delayed presentation of vascular surgery conditions, and poorer outcomes of patients with chronic limb threatening ischemia. This scoping review provides a snapshot of the impact of the COVID-19 pandemic on elective and emergency vascular surgery.
Keywords: COVID-19, SARS-CoV-2, Health Services Research, Pandemics, Elective Surgical Procedure, Emergencies
1. Introduction
According to the World Health Organization, an astounding 120 million cases of coronavirus disease 2019 (COVID-19) have been diagnosed as of March 2021. Since the start of the COVID-19 pandemic in December 2019, approximately 3 million people have died from complications from COVID-19 [1]. Despite global efforts in vaccination roll-out, the COVID-19 pandemic is expected to last beyond 2022 due to the emergence of more infectious variants [2]. The persistent onslaught of COVID-19 on our health care facilities has and will inevitably continue to profoundly impact the way we practice medicine around the world. The COVID-19 pandemic has strained our health care systems in multiple ways. The influx of patients with COVID-19 into our health care institutions has resulted in rising demands on hospital bed space, critical care resources, personal protective equipment, and staff [3]. To cope with the rising numbers of patient with COVID-19, many institutions have established multifaceted COVID-19 surge protocols or business continuity plans to protect and safeguard essential health care resources [4].
In addition to the deleterious effects of COVID-19 itself on global health, surgical practice itself has been particularly affected as a result of the refocus of medical priority towards preserving resources and caring for patients infected with COVID-19 [5]. Early in the COVID-19 pandemic, in March 2020, the American College of Surgeons (ACS) recommended that each health care institution review, minimize, or postpone scheduled elective surgery with a view to preserve crucial health care infrastructure [4]. They suggested using a tiered triage system based on surgical acuity to decide on the postponement of elective surgery. In the United Kingdom, hospitals in the National Health Service have been advised to suspend elective surgery procedures for at least 3 months starting from March 2020 to expand the capacity to care for patients with COVID-19. Similarly, multiple health care institutions around the world affected by the COVID-19 pandemic have also implemented plans to postpone elective surgery. Aside from the conservation of critical health care resources, deferment of nonurgent elective surgery can also reduce unnecessary patient-hospital exposure, and enable the repurposing of operating suites or recovery areas to care areas for patients with patients with COVID-19 [6]. Despite the widespread postponement of elective surgery, most institutions allowed the continuation of emergency or lifesaving surgery. However, in some regions overwhelmed by the COVID-19 pandemic, even patients requiring emergency surgery might have been turned down due to extremely scarce resources [7,8].
Vascular surgeons manage and operate on a large spectrum of surgical cases, ranging from elective cases, such as varicose veins, to semi-urgent cases, such as chronic limb threatening ischemia (CLTI), and emergent cases, such as ruptured aortic aneurysms. A large proportion of vascular surgery (VS) cases, although classified as elective, are actually time-sensitive in nature. Due to the COVID-19 pandemic, many of these cases have been deferred, possibly leading to detrimental outcomes. In order to explore the effects of the COVID-19 pandemic on elective and emergency VS, we chose to undertake a scoping review to map available literature in a systematic and transparent way [9].
2. Methods
This scoping review was conducted in accordance to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis extension for Scoping Reviews [9]. Unlike systematic reviews, scoping reviews do not need to have a protocol registered [10]. A systematic review is usually performed with a predefined question about a specific condition or intervention, and a scoping review is exploratory in nature and involves a broad literature review to identify the key concepts and themes of literature relevant to the topic of interest. A scoping review was chosen over a systematic review, as evidence relating to the effects of COVID-19 on VS provision is extremely diverse and heterogeneous. A scoping review is, therefore, more suitable in this instance as it remains relatively unclear what specific questions should be asked and valuably addressed by a more precise systematic review and meta-analysis [10], [11], [12].
2.1. Search strategy
A search string was developed to identify original studies reporting the effects of COVID-19 on elective and emergency VS. The search terms comprised synonyms of the following three key concepts: COVID-19, elective VS, and emergency VS. The search was applied to the following two electronic databases: Ovid MEDLINE and Embase. Searches were performed for each database on March 14, 2021. No limits were applied. Our complete search strategy is available in Supplementary Tables 1 and 2.
2.2. Research question
Outcome variables were not predefined in this study, due to the exploratory rather than hypothesis-led nature of this study. We explored the literature intending to address the effects of the COVID-19 pandemic on the conduct of VS cases globally.
2.3. Study selection and reliability
Articles were selected for inclusion in the review if they were published in a peer-reviewed journal in any language and had relevance to how COVID-19 altered the conduct of VS cases. Due to the nature of COVID-19 research, and because this scoping review aimed to broadly capture available evidence, we included original research and research letters, as these could potentially contain sufficient detail to evaluate the effects of COVID-19 on the provision of elective and emergency VS during the pandemic.
All titles and abstracts were screened independently by two reviewers (K.S.L. and S.R.) using the aforementioned inclusion criteria. Potentially eligible studies were selected for full-text analysis. To ensure literature saturation, the reference lists of the included studies were scanned. Due to the exploratory of this scoping review, the exclusion criteria were kept lenient—studies that did not report the effects of COVID-19 on VS provision were excluded. Disagreements were resolved by consensus or appeal to a third senior reviewer (J.J.N.).
2.4. Risk of bias assessment
Because this review did not aim to synthesize data about intervention effectiveness, it was not necessary to carry out an assessment of the risk of bias.
2.5. Data charting
The data extraction process in a scoping review is known as “data charting.” Key variables were screened and extracted from the articles into a data charting form. This was continuously updated in an iterative process, as the heterogeneity of data and reported outcomes often meant noncontiguous data points. In general, we extracted data pertaining to study design, country, participants, effects on elective and emergency VS, and other relevant findings. Two reviewers independently (K.S.L. and S.R.) charted data from each eligible article. Disagreements were resolved through discussion or further adjudication by a third reviewer (J.J.N.).
2.6. Synthesis of results
A narrative synthesis of data, with descriptive analyses where appropriate was undertaken to enable the analysis of the relationships within and between studies, as well as assessing gaps in the literature. An analytical framework of a quantitative and thematic approach was used to generate various clinically relevant themes that emerged from the existing data.
3. Results
3.1. Characteristics of included studies and themes
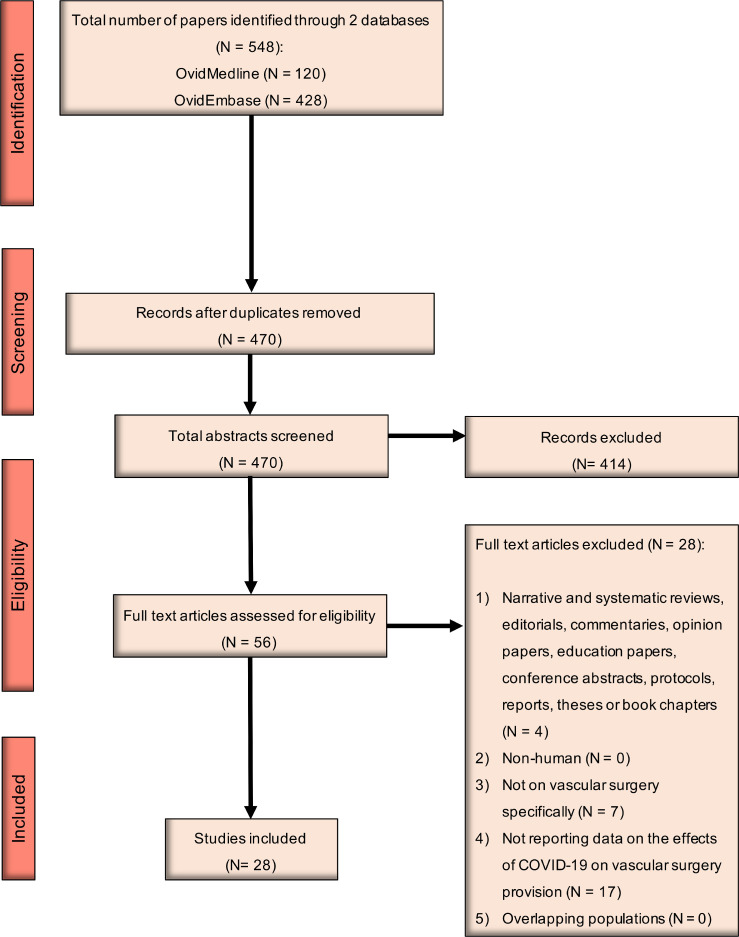
A total of 548 citations were identified from searching the two electronic databases. A thorough review of titles and abstracts and full text and reference lists retrieved 28 articles eligible for inclusion. From our literature search and scoping review, we identified eight distinct themes that related closely to the COVID-19 pandemic and the conduct of VS cases. The eight distinct themes were:
-
1.
VS case triage system
-
2.
Emergence of global collaborative VS research groups
-
3.
Global surveys on VS practice
-
4.
Regional surveys on VS practice
-
5.
Institutional changes in VS practice
-
6.
Use of endovascular techniques and locoregional anesthesia
-
7.
Delayed presentation of VS conditions
-
8.
Outcomes in patients with VS conditions
A summary of the included studies and their relevant themes are provided in Table 1 .
Table 1.
Summary of included studies and themes.
| Author | Study location | Study period | Study type | Key findings | Themesa |
|---|---|---|---|---|---|
| VASCC [15] | Global | Ongoing | Global registry | Elucidate the effect of the deferment of vascular cases Global registry of thrombotic complications of COVID-19 |
2 |
| Ng [7] | Global | March 2020 | Survey | 90.9% deferred of elective VS cases 92.2% still performing emergency surgery |
3 |
| COVER Tier 1 study [8] | Global | March to May 2020 | Survey, global registry | Stricter case selection for carotid intervention Increased threshold for aortic aneurysm repair |
2, 3, 6 |
| COVER Tier 2 study [40] | Global | March to May 2020 | Global observational study | Elevated in-hospital mortality across aortic, carotid and lower extremity interventions despite low COVID-19 infection rate | 8 |
| Aziz [16] | US | April 2020 | Survey | Deferment of elective cases Reduced emergency department consults for VS conditions |
4, 7 |
| Latz [17] | US | April 2020 | Survey | 80.5% performing urgent and emergent cases only 15.3% performing emergent cases only |
4 |
| Mouawad [18] | US | April 2020 | Survey | 91.7% cancelled elective cases | 4 |
| Mahentiran [19] | US | May 2020 | Survey | 74% performing urgent and emergent cases only Venous registry volumes reduced fivefold |
4 |
| Natarajan [20] | US | May 2020 | Survey | Arterial registry volumes reduced sevenfold | 4 |
| Mirza [21] | US | March to April 2020 | Institutional review | 93% of electives deferred Performed urgent and emergent cases |
5 |
| Sarfati [22] | US | March to April 2020 | Institutional review | Adhered to ACS guidelines Performed tier 2b and tier 3 cases Deferred tier 1, tier 2a, and some tier 2b cases |
5 |
| Boschetti [23] | Italy | March to April 2020 | Institutional review | 37.1% reduction on operative case volume Reduction in emergency room visits Increased presentation of patients with decompensated CLTI |
5, 7, 8 |
| Chisci [24] | Italy | March to April 2020 | Institutional review | Deferment of nonurgent elective cases Endovascular treatment of CLTI preferred |
5, 6 |
| Chiesa [25] | Italy | March to April 2020 | Institutional review | Deferment of varicose vein surgery Only symptomatic, urgent or emergent cases performed |
5 |
| Piazza [26] | Italy | March to April 2020 | Institutional review | Deferment of nonurgent elective cases Performed urgent and emergent cases Higher major amputation rate for CLTI patients |
5, 8 |
| Mascia [27] | Italy | March to April 2020 | Institutional review | Increased urgent and emergent cases due to referral system Higher proportion of late presentation of limb ischemia 50% reduction in ruptured or symptomatic AAA |
5, 7, 8 |
| Pini [28] | Italy | March to April 2020 | Institutional review | Priority criteria for elective cases adopted Performed urgent and emergency cases |
5 |
| Duarte [29] | Portugal | February to June 2020 | Institutional review | 17.8% reduction in operative case volume 54% reduction in patients admitted from the ED Significant increase in endovascular procedures Significant increase in use of locoregional anesthesia |
5, 6, 7 |
| Gouveia E Melo [30] | Portugal | March 2020 | Institutional review | Performed urgent and emergent cases only Decrease in urgent and emergent cases Endovascular approach and locoregional anesthesia preferred |
5, 6 |
| Correia [35] | Portugal | March to June 2020 | Institutional review | Fewer patients presented to ED compared to 2019 Patients required more urgent surgery compared to 2019 |
7 |
| Ben Abdallah [31] | France | March to April 2020 | Institutional review | Performed only urgent or emergent cases only Endovascular approach favored over open repair Increased number of patients with acute arterial events Significant decrease in overall vascular referrals |
5, 6, 7 |
| Connolly [32] | Ireland | March to April 2020 | Institutional review | Deferment of nonurgent elective cases Endovascular approach preferred |
5, 6 |
| Metelmann [33] | Germany | March to April 2020 | Institutional review | Deferment of nonurgent elective cases Performed urgent or emergent cases, ie, high-risk AAA |
5 |
| Ünal [34] | Turkey | April 2020 | Institutional review | Triaged vascular cases according to “level of priority” Deferred nonurgent elective cases Endovascular approach preferred |
5, 6 |
| Leong Tan [36] | Singapore | March to April 2020 | Institutional review | Deferred nonurgent elective cases Performed urgent or emergent cases only |
5 |
| Ng [37] | Singapore | February to March 2020 | Institutional review | Deferred nonurgent elective cases Performed urgent or emergent cases only Increase in major amputation rate |
5, 8 |
| Wang [39] | China | April 2020 | Institutional review | Deferred nonurgent elective cases Performed urgent or emergent cases only Endovascular approach preferred |
5, 6 |
| Bashar [38] | Bangladesh | March to June 2020 | Institutional review | Deferred nonurgent elective cases Performed urgent or emergent cases only Higher rates of limb loss in CLTI patients |
5, 8 |
Abbreviations: AAA, abdominal aortic aneurysm; ACS, American College of Surgeons; CLTI, chronic limb threatening ischemia; COVER, COVID-19 Vascular Service Study; COVID-19, coronavirus disease 2019; ED, emergency department; US, United States; VASCC Vascular Surgery COVID-19 Collaborative; VS, vascular surgery.
Themes: (1) VS case triage system; (2) emergence of global collaborative VS research groups; (3) global surveys on VS practice; (4) regional surveys on VS practice; (5) institutional changes in VS practice; (6) use of endovascular techniques and locoregional anesthesia; (7) delayed presentation of VS conditions; and (8) outcomes in patients with VS conditions.
3.2. VS case triage system
Three case triage systems were identified while conducting a full-text review. Although these case triage systems were published on websites and not in medical journals, we thought it was important to include them in this scoping review, as they were vital to VS case triage during the COVID-19 pandemic. The Vascular Society of Great Britain and Ireland (VSGBI) first published their recommendations on the conduct of emergency and elective VS cases on March 20, 2020 [13]. VSGBI guidelines recommend using endovascular methods to manage emergency VS cases, such as ruptured abdominal aortic aneurysms (AAAs) or CLTI. They also recommend increasing the size threshold of asymptomatic AAAs and the deferment of elective VS cases, such as asymptomatic carotid artery stenosis and revascularization for claudication. On March 23, 2020, the Vascular and Endovascular Society (VESS) published similar recommendations to defer elective VS cases, such as asymptomatic AAAs, asymptomatic peripheral or visceral aneurysms, nonurgent hemodialysis access creation, revascularization for patients without tissue loss or patients with claudication, asymptomatic CAS, and varicose vein procedures [14]. Subsequently, the ACS published triage guidelines for an exhaustive list of VS cases [4]. The ACS guidelines classified various VS cases into different tier classes based on the acuity and urgency of the condition. For example, ruptured AAAs were classified as tier 3 (do not postpone), asymptomatic AAAs > 6.5 cm were classified as tier 2b (postpone if possible), and asymptomatic AAAs of < 6.5 cm in maximal diameter were classified as tier 1 (postpone).
3.3. Emergence of global collaborative research groups
Since the COVID-19 pandemic started, two global registries have been established to evaluate the impact of COVID-19 on VS cases. The Vascular and Endovascular Research Network (VERN) initiated the international COVID-19 Vascular Service (COVER) study to elucidate the change and outcomes of VS during the COVID-19 pandemic. The COVER study is divided into three distinct tiers. Tier 1 aimed to report changes to vascular unit level clinical processes, tier 2 aimed to report outcomes of vascular interventions performed during the COVID-19 pandemic, and tier 3 aimed to elucidate changes in management of urgent and acute vascular cases. Besides VERN and the COVER study, the Vascular Surgery COVID-19 Collaborative (VASCC) was also incepted early in the COVID-19 pandemic. Founded by two vascular surgeons in the United States, VASCC serves to collect prospective international data on the impact of COVID-19 on scheduled vascular operations, as well as the thrombotic complications of COVID-19 [15]. Published data from the VASCC are eagerly awaited.
3.4. Global surveys on VS practice
Two articles were identified that provided a global perspective on the effect of the COVID-19 pandemic on VS cases [7,8]. Ng et al [7] first reported the global impact of COVID-19 on VS cases via an online survey of vascular surgeons in March 2020. A total of 77 respondents from varying countries participated in the online survey. Ng et al reported that 90.9% of respondents had deferred at least some, if not all, elective VS cases, such as varicose vein surgery, revascularization for claudication, small or asymptomatic aortic aneurysms, dialysis access creation, and asymptomatic carotid stenoses. However, 92.2% of respondents were still performing emergency VS cases [7]. As mentioned previously, since the early publication by Ng et al, two global registries have been established to evaluate the impact of COVID-19 on VS cases. The COVER study collaborative conducted an online survey from March to May 2020, which garnered a total of 465 respondents from 249 VS units in 53 countries across six continents [8]. Tier 1 of the COVER study reported significant changes in VS practice relating to carotid surgery, aortic aneurysm treatment, and lower limb revascularization. Globally, there was a reduction in carotid surgery, with 17.7% of units offering carotid intervention for crescendo transient ischemic attacks only and 43.5% of units offering intervention on a case-by-case basis only. For AAAs, the threshold size for aneurysm repair was increased in some VS units. Some units only offered intervention if AAA size was > 6.5 cm, or if the AAA was symptomatic or ruptured. In the management of lower limb peripheral arterial disease, VS units seemed to only offer revascularization to patients with rest pain or tissue loss, adopt more endovascular means of revascularization, and offer upfront major amputation or palliation in patients presenting with severe tissue loss.
3.5. Regional surveys on VS practice
Five articles reported the changes in VS practice in North America via the conduct of online surveys or questionnaires [16], [17], [18], [19], [20]. Aziz et al [16] conducted an online survey from April 14 to 17, 2020 for members of the VESS to identify and report changes in VS surgical practice. Of the 206 respondents, an overwhelming majority (> 80%) would postpone lower limb revascularization for claudication, asymptomatic carotid artery disease, asymptomatic AAA < 6.5 cm, and patients with end-stage renal disease requiring nonurgent dialysis access. A lower proportion, but still more than one-half of the respondents would postpone procedures, such as revascularization for rest pain, chronic mesenteric ischemia, or patients requiring early (< 3 months) dialysis access. Conversely, only a smaller proportion of respondents (≤ 50%) would defer procedures such as revascularization for tissue loss, large asymptomatic AAA or TAA, or treatment of dysfunctional dialysis access.
Similarly, Latz et al [17] conducted an online survey for vascular surgeons from April 14 to 21, 2020 with a total of 121 eventual respondents. In general, they found that 80.5% of respondents were delaying elective cases and only performing urgent and emergent cases. Cases such as asymptomatic AAA, revascularization for claudication, amputation for nonacute disease, chronic mesenteric ischemia, asymptomatic carotid disease, thoracic outlet syndrome, varicose veins, venous ulceration, inferior vena cava filter removal, and anterior spine exposure were delayed. Cases such as symptomatic or ruptured AAA, aortic dissection with malperfusion, revascularization for CLTI, acute limb ischemia, amputation for wet gangrene or ascending cellulitis, acute mesenteric ischemia, and symptomatic carotid disease were continued. Likewise, Mouawad et al [18] conducted a cross-sectional survey from April 14 to 24, 2020 and obtained the responses of 535 vascular surgeons from 45 states in the United States. More than 90% of respondents had reported cancellation of elective VS procedures, regardless of whether the institution was a teaching or nonteaching hospital. Most of the respondents (86%) also reported institutional adherence to the Society for Vascular Surgery or ACS guidelines for elective VS case triage.
Lastly, Mahenthiran et al [19] and Natarajan et al [20] both surveyed more than 100 Vascular Quality Initiative physicians and the majority (74%) reported operating on urgent and emergent cases only. Approximately one-half of the respondents still operated on time-sensitive elective cases, such as dialysis access creation, intervention for dysfunctional dialysis access, and asymptomatic aortic aneurysms, as well as interventions for threatened bypass grafts. A small proportion (14%) of respondents reported operating on purely emergency cases only. Similar to other studies, revascularization for claudicants was performed rarely. With regard to threshold size for asymptomatic AAA repair, 26% and 21% of respondents had altered their operative size threshold to > 6 cm and 7 cm in male patients and > 5.5 cm and 6.5 cm in female patients, respectively. Mahenthiran et al and Natarajan et al also reported a fivefold reduction in venous registry case volumes and sevenfold reduction in arterial registry case volumes, respectively, during the COVID-19 study period compared with 2019.
3.6. Institutional changes in VS practice
A total of 19 articles had reported changes in the conduct of emergency and elective VS cases in respective institutions [21], [22], [23], [24], [25], [26], [27], [28], [29], [30], [31], [32], [33], [34], [35], [36], [37], [38], [39]. In summary, all of the articles reported continuation of emergency VS cases, such as ruptured AAAs, and deferment of nonurgent elective VS cases, such as revascularization for claudicants and varicose veins. There was some inter-institutional variation between the type of VS cases that proceeded or were deferred.
In North America, two articles retrospectively reviewed the type of cases performed during the COVID-19 study period [21,22]. Mirza et al [21] reported adherence to the ACS guidelines, with cancellation of 93% of all scheduled elective cases, such as outpatient vein procedures, revascularization for claudicants, asymptomatic AAA or carotid stenoses, and low-risk CLI patients in their study period (March 23 to April 8, 2020). Conversely, the authors continued to perform urgent cases, such as ruptured AAAs and symptomatic carotid stenoses. Similarly, Sarfati et al [22] also reported adherence to the ACS guidelines during the COVID-19 pandemic. During their study period (March 14 to April 14, 2020), Sarfati et al reported that 69 VS cases were performed, of which 47 (68%) cases were considered to be tier 3 and the remaining 22 (32%) to be tier 2b. The authors postponed all tier 2a or tier 1 cases.
A total of 13 articles that originated from Europe described the change in provision of VS surgical services during the COVID-19 pandemic [23], [24], [25], [26], [27], [28], [29], [30], [31], [32], [33], [34], [35]. Six articles were from Italy, three articles were from Portugal, and four articles were from France, Ireland, Turkey, and Germany, respectively. All six articles from Italy described continuation of emergency VS cases and only selected time-sensitive elective cases in March through April 2020, which corresponded to a lockdown period [23], [24], [25], [26], [27], [28]. Boschetti et al [23] retrospectively reviewed their surgical activity during their study period (March 1 to April 30, 2020) and reported a 37.1% reduction in operative caseload compared with before the pandemic started. Emergency VS cases, such as ruptured AAA, were still performed. Elective VS cases were screened and only time-sensitive cases, such as AAA ≥ 6 cm, TAA ≥ 7 cm, symptomatic CAS, asymptomatic CAS with high-grade stenosis and unstable plaque, and CLTI were continued. Chisci et al [24] also reported a 34% reduction in elective VS cases in March to April 2020 compared with a corresponding period in 2019. Similar findings were also reported by Chiesa et al [25], who reported deferment of all nonurgent elective VS cases, such as varicose vein surgery, and operating on emergent or urgent cases only. Piazza et al [26] reported a significant 50% reduction in elective VS cases. Contrary to the aforementioned articles, Pini et al [28] and Mascia et al [27] did not report a decrease in VS cases. Mascia et al reported an increase of urgent or emergent VS cases performed in March to April 2020 compared with 2019 due to increased referrals from spoke hospitals and more frequent presentation of thrombotic acute limb ischemia associated with COVID-19 infection. Pini et al reported no change in the total volume of emergency or elective cases, although they had also adopted a screening protocol to prioritize elective cases.
Two articles originated from Portugal. Duarte et al [29] retrospectively reviewed VS cases from February to June 2020 and found that, compared with a similar period in 2018, the VS team performed 17.8% fewer procedures. Similar to most institutions, Gouveia E Melo et al [30] reported deferment of all nonurgent elective cases and continuation of time-sensitive cases, such as CLTI, symptomatic CAS, or AAA > 5.5 cm.
The remaining four articles were from France, Ireland, Turkey, and Germany. According to Ben Abdallah et al [31], VS units in Paris adopted recommendations from the French Society for Vascular Surgery and limited surgical activity to more urgent cases, such as acute aortic syndromes, acute limb ischemia, CLTI, symptomatic CAS, mesenteric ischemia, and vascular access for hemodialysis. In the United Kingdom, Connolly et al [32] also reported the postponement of nonurgent elective surgery. Similarly, Metelmann et al [33] also reported deferment of nonurgent elective VS cases in Germany, and the treatment of emergency cases only, such as large aneurysms with immediate risk of rupture from March to April 2020. Lastly, Ünal et al [34] described the adaptation of a level of priority case triage system in Turkey to prioritize VS cases. For example, cases such as revascularization for intermittent claudication were considered as level of priority 1 and deferred. On the contrary, cases such as ruptured AAA or acute limb ischemia are considered level of priority 3 and should be prioritized.
Outside of North America and Europe, four articles described the change in conduct of VS cases. Two articles were from Singapore and the remaining two articles were from Bangladesh and China. Both Leong Tan et al [36] and Ng et al [37] described institutional and VS unit changes early in the COVID-19 pandemic in Singapore. Both authors described deferment of elective nonurgent VS cases, and only continuation of more urgent elective cases, such as revascularization for CLTI patients. Bashar et al [38] provided insight into the conduct of VS cases during the COVID-19 pandemic. Lastly, Wang et al [39] also reported the deferment of nonurgent elective VS cases in China, but did not provide additional data.
3.7. Use of endovascular techniques and locoregional anesthesia
Several articles had reported an increase in the adoption of endovascular techniques and locoregional anesthesia for treatment of VS cases during the COVID-19 pandemic. The COVER study reported an overall 18.2% increase in the use of endovascular management for lower limb pathology [8]. Sarfati et al [22] compared VS activity before and during the COVID-19 pandemic and found a significant increase in endovascular cases from 41% to 58%. Similarly, Duarte et al [29] also reported a significant rise in the use of an endovascular approach from 15.2% and 17% in 2018 and 2019, respectively, to 22.6% in 2020 during the COVID-19 pandemic. Duarte et al also reported a 27.1% increase in the use of local anesthesia only during the COVID-19 pandemic. Gouveia E Melo et al [30], Ben Abdallah et al [31], Connolly et al [32], and Ünal et al [34] have also recommended the use of more endovascular techniques and locoregional anesthesia, although they did not provide any descriptive data.
3.8. Delayed presentation of VS conditions
To examine how COVID-19 had impacted VS patients presenting via the emergency department, Correia et al [35] conducted a retrospective study and found that although there were fewer patients presenting to the emergency department for VS conditions during their study period (March to June 2020) compared with a similar prepandemic period, more patients required urgent surgery. In a survey of VESS members, most participants also reported reduction in emergency department consults for acute and chronic VS conditions [10]. Similarly, Duarte et al [29] and Boschetti et al [23] reported 54% and 40.5% reductions in patients presenting via the emergency department, respectively. Ben Abdallah et al [31] also reported an overall decrease in vascular referrals. Lastly, specific to CLTI, Mascia et al [27] reported a 50% reduction in patients presenting with ruptured or symptomatic AAAs, suggesting a possible delay or lack of presentation for aortic conditions.
3.9. Outcomes in patients with VS conditions
One theme that had emerged from our scoping review is possible poorer outcomes for patients presenting with VS conditions during the COVID-19 pandemic. The COVER tier 2 study was a global multicenter observational study that aimed to elucidate outcomes after open and endovascular interventions performed for VS conditions during the early phases of the COVID-19 pandemic (April to June 2020). Results from this study indicated an unsurprisingly high mortality associated with aortic surgery, carotid surgery, lower limb interventions, and amputations, despite a low incidence of suspected or confirmed COVID-19 cases [40]. Several other authors also described poorer outcomes in patients with CLTI during the COVID-19 pandemic. Piazza et al [26] reported a higher major amputation rate for patients presenting with CLTI compared with a corresponding period before the COVID-19 pandemic (10% v 4%). Ng et al [37] had also reported an increase in major amputation rates from 2.5% of all VS cases performed in November and December 2019 combined, to 4.2% of all VS cases performed in January to March 2020 combined. Boschetti et al [23] and Mascia et al [27] both reported more patients presenting late with limb ischemia. Lastly, Bashar et al [38] similarly reported a decrease in limb salvage rate from 83.6% to 72.4% for patients presenting with CLTI during the COVID-19 pandemic compared with a prepandemic period.
4. Discussion
This scoping review attempts to comprehensively review the effects of the COVID-19 pandemic on elective and emergency VS cases performed worldwide. It provides a snapshot of how VS cases were conducted during the early periods of the COVID-19 pandemic, as most studies were conducted during the first half of 2020. It is also important to note that most of the included articles were published by groups or institutions from North America and Europe, and hence this scoping review might not accurately depict the conduct of VS cases in other regions of the world, such as in South America, Africa, the Indian subcontinent, and Australasia.
The COVID-19 pandemic has certainly spurred the rapid establishment of global multi-institutional collaborative studies, such as the COVER study and the VASCC study [8,15]. Aside from these new collaborative studies, the COVID-19 pandemic has also had an effect on current pre-existing vascular registries, such as member registries of VASCUNET and the Society for Vascular Surgery Vascular Quality Initiative. Some of these registries have expanded their data forms to capture COVID-19 specific data. The newer collaborative studies and pre-existing registries both play important roles in collecting and assimilating worldwide data pertaining to the effects of COVID-19 on vascular surgical practice [41].
The development of societal guidelines is extremely important during a pandemic to guide the VS community. The VSGBI, VESS, and ACS had rapidly published recommendations on VS practice in March 2020, which corresponded to a period of COVID-19 surge in North America and Europe. Based on our scoping review, we found that most institutions had adhered, with some variation, to these VS case triage guidelines. All of the articles that had described their VS practice during the COVID-19 pandemic had reported continuation in the management of emergency VS cases, such as ruptured AAA, vascular trauma, and acute limb ischemia. These are cases that have an immediate threat to life, limb, or viscus if not treated emergently. For elective cases that are more urgent, such as large AAA, symptomatic CAS, or CLTI, most units still continued to offer surgical management. However, all units had reported deferring nonurgent VS cases, such as varicose vein procedures, revascularization for claudicants, and pre-emptive arteriovenous access creation. This resource-conservation practice is reflected in multiple other surgical specialties as well, such as surgical oncology, where low-risk cases such as carcinoma in situ or premalignant lesions were deferred, and high-risk cases, such as locally advanced tumors, were continued. During the height of the COVID-19 pandemic, this resource-conserving practice of elective case triaging has several benefits. First, it reduces the need for these patients to come to the hospital where there might be a higher risk of COVID-19 exposure. Second, it allows preservation of essential personal protection equipment, such as surgical masks and gloves, and allows them to be reallocated to areas of the hospitals that might need it more. Third, it allows the repurposing of operating theaters or anesthetic bays into critical care units for the management of patients with COVID-19. Lastly, it allows crucial staff, such as anesthetists and nurses, to be redeployed for care of patients with COVID-19.
Aside from the postponement and stricter triage of elective and semi-elective VS cases, the COVID-19 pandemic also affected outpatient services. In a cross-sectional survey conducted in April 2020 by Mouawad et al [18], 71% of vascular surgeons reduced the operating hours of outpatient clinics and 81.1% cited the adoption of telehealth. Close to half of the respondents still operated an office-based laboratory, which mainly performed urgent cases such as dialysis access salvage. Similarly, in a global survey performed by Ng et al [7], 86.9% of vascular surgeons reported closure or downscaling of outpatient services in the early phases of the pandemic. In Italy, outpatient activities were also significantly reduced from January to April 2020. However, from May 2020 onwards, as the COVID-19 situation improved, outpatient activities were restored to prepandemic levels [23]. The initial reduction in outpatient-based services during the early phase of the pandemic can be attributed to factors such as staff conservation and reduction of nonurgent patient contact to limit COVID-19 spread. As the COVID-19 situation improves, we must make preparations to manage a possible surge in outpatient load.
In this scoping review, several articles had reported an increase in endovascular management of VS conditions during the COVID-19 pandemic compared with prepandemic times [26,40]. Endovascular procedures generally have a shorter recovery period after the procedure. Therefore, patients can be discharged earlier, reducing the possibility of transmission of COVID-19 and also increasing vital resources, such as bed space. The increased use of endovascular procedures can also conserve critical care resources, such as intensive care unit or high-dependency bed space. Nevertheless, although the increased adoption of endovascular management has its benefits during the COVID-19 pandemic, vascular surgeons still have to decide on an individualized basis in consideration of the patient's disease factor, as well as the outcomes of endovascular versus open surgery.
We also reported the increased use of locoregional anesthesia compared with general anesthesia for VS cases. This is likely to be related to the increased use of percutaneous and endovascular management. Even so, the use of locoregional anesthesia, if possible, during the COVID-19 pandemic can also help conserve critical care resources, such as ventilators, drugs such as neuromuscular blockade agents, general ward bed space, and intensive care bed space. The use of locoregional anesthesia in VS cases has been shown to reduce hospital length of stay and intensive care requirements.
Unfortunately, we also found that VS patients were less likely to seek treatment in the emergency department during the COVID-19 pandemic, which can potentially lead to delays in treatment and poorer outcomes. This phenomenon has also been reported in other non–VS-related articles. Nourazari et al [42] reported a 32% decrease in all emergency department admissions from 12 hospitals in Massachusetts. The reduction in emergency department presentation might be due to several factors, such as fear of COVID-19 transmission resulting in avoidance of hospital facilities. We must be cognizant of the detrimental effects of this phenomenon. The impact of the COVID-19 pandemic on the health-seeking behavior of the general population has not been fully elucidated. Patients with acute cardiovascular emergencies, such as leaking or ruptured AAAs, cerebrovascular accidents, or acute myocardial infarctions, might die at home due to reluctance or delay in seeking appropriate medical help. In these patients, their exact cause of mortality might not be determined, and overall mortality rates of the respective abovementioned cardiovascular emergencies might therefore be underreported.
Our scoping review also found an increase in in-hospital mortality for patients admitted for cardiovascular conditions during the early phases of the COVID-19 pandemic. The increase in in-hospital mortality can be attributed to direct and indirect effects of COVID-19 infection. An international study conducted by the COVIDSurg collaborative reported an elevated 30-day mortality rate of 23.8% in COVID-19–positive patients who underwent a diverse range of elective and emergency surgery [43]. Similar findings were also reported by a German study that analyzed health insurance claims data, which observed a higher mortality in patients with COVID-19 admitted for cardiovascular conditions, such as acute stroke, acute limb ischemia, and transient ischemic attacks [44]. On the contrary, the COVER tier 2 study demonstrated a elevated in-hospital mortality risk across patients who underwent aortic, carotid, or lower limb procedures, despite a low (4%) COVID-19 infection rate [40]. The authors of the COVER tier 2 study attributed the increase of in-hospital mortality to indirect effects of the COVID-19 pandemic, such as delayed presentation, case postponement, increased size threshold for aortic aneurysm repair, and infrastructure change.
A recurrent theme that we noticed in our scoping review was poorer outcomes in patients presenting with CLTI. Boschetti et al [23] had reported an increase in the proportion of patients presenting with decompensated CLTI. Several articles had also reported an increase in major amputation rates during the COVID-19 pandemic [26,27,37,38]. This occurrence could be a result of delayed case presentation as discussed earlier, or can be due to a change in surgical practice. Limb salvage can be a resource-intensive process involving long hospitalizations coupled with multiple re-interventions. For some patients who present with extensive tissue loss, some vascular surgeons might offer upfront major amputation in order to conserve resources during the COVID-19 pandemic.
Our scoping review primarily reported and discussed the changes in VS practice during the early phases of the COVID-19 pandemic due to paucity of individual institutional data on VS practice during the later phases of the pandemic [41]. The sharp decline in VS cases during the first two quarters of 2020 is corroborated by registry data, such as the UK National Vascular Registry and the US Vascular Quality Initiative. However, by the third quarter of 2020, elective VS cases such as carotid endarterectomies and AAA repairs, had rebounded to near prepandemic volumes due to easing of COVID-19 restrictions [41]. As discussed earlier, more long-term studies are required to fully elucidate the long-term effects of VS case delay and postponement.
Our scoping review included an extensive literature review and had included articles from around the world. Multiple clinically relevant themes were identified that provided a snapshot of how VS was conducted during the COVID-19 pandemic. However, there are still several limitations to this scoping review. A large majority of included articles were from North America or Europe, and this scoping review might misrepresent the situation in other parts of the world. In addition, most articles described VS services during the early phase of the COVID-19 pandemic. There is a paucity of articles that described the resumption of VS services as the pandemic situation evolved. Lastly, this scoping review focused on evaluating the changes in VS case mix due to the COVID-19 pandemic and did not evaluate other aspects of VS service, such as outpatient clinics, telemedicine, and vascular education (Fig. 1 ).
Fig. 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analysis flow diagram.
5. Conclusions
The impact of COVID-19 on the delivery of VS service has been far-reaching. Vascular surgeons around the world report a substantial impact on their practices: This scoping review provides insight on the conduct of VS cases during the COVID-19 pandemic. Moving ahead, we need actively plan for resumption of full VS services in the post-pandemic phase. We must also make contingencies for the future, if a similar pandemic affects us again.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1053/j.semvascsurg.2021.07.002.
Appendix. Supplementary materials
References
- 1.WHO Coronavirus COVID-19) dashboard. World Health Organization. Accessed. June 16, 2021 https://covid19.who.int/ Available at. [Google Scholar]
- 2.Charumilind S, Craven MC, Lamb J, et al. When will the COVID-19 pandemic end? Accessed June 16, 2021. Available at: https://www.mckinsey.com/industries/healthcare-systems-and-services/our-insights/when-will-the-covid-19-pandemic-end
- 3.Moghadas SM, Shoukat A, Fitzpatrick MC, et al. Projecting hospital utilization during the COVID-19 outbreaks in the United States. Proc Natl Acad Sci U S A. 2020;117:9122–9126. doi: 10.1073/pnas.2004064117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.COVID-19: recommendations for management of elective surgical procedures. American College of Surgeons. Accessed March 14, 2021. Available at: https://www.facs.org/about-acs/covid-19/information-for-surgeons/elective-surgery
- 5.Al-Jabir A, Kerwan A, Nicola M, et al. Impact of the coronavirus (COVID-19) pandemic on surgical practice-Part 2 (surgical prioritisation) Int J Surg. 2020;79:233–248. doi: 10.1016/j.ijsu.2020.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Collaborative COVIDSurg. Elective surgery cancellations due to the COVID-19 pandemic: global predictive modelling to inform surgical recovery plans. Br J Surg. 2020;107:1440–1449. doi: 10.1002/bjs.11746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ng JJ, Ho P, Dharmaraj RB, et al. The global impact of COVID-19 on vascular surgical services. J Vasc Surg. 2020;71:2182–2183. doi: 10.1016/j.jvs.2020.03.024. e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.The Vascular and Endovascular Research Network (VERN) COVER Study Collaborative Global impact of the first coronavirus disease 2019 (COVID-19) pandemic wave on vascular services. Br J Surg. 2020;107:1396–1400. doi: 10.1002/bjs.11961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tricco AC, Lillie E, Zarin W, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169:467–473. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- 10.Munn Z, Peters MDJ, Stern C, et al. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018:18. doi: 10.1186/s12874-018-0611-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lee KS, Zhang JJY, Alamri A, et al. Neurosurgery education in the medical school curriculum: a scoping review. World Neurosurg. 2020;144:e631–e642. doi: 10.1016/j.wneu.2020.09.015. [DOI] [PubMed] [Google Scholar]
- 12.Lee KS, Ng JJ, Choong AMTL. A scoping review of vascular surgery education in the medical school curriculum [published online ahead of print May 2, 2021]. J Vasc Surg doi:10.1016/j.jvs.2021.04.024 [DOI] [PubMed]
- 13.COVID-19 virus and vascular surgery. The Vascular Society for Great Britain and Ireland. Accessed June 9, 2021. Available at: https://www.vascularsociety.org.uk/professionals/news/113/covid19_virus_and_vascular_surgery
- 14.Vascular and Endovascular Surgery Society COVID-19 statement. Vascular and Endovascular Surgery Society. Accessed June 9, 2021. Available at: https://vesurgery.org/site/wp-content/uploads/2020/03/VESS-COVID-19-Statement.pdf
- 15.Mouawad NJ, Cuff RF, Hultgren R, et al. The Vascular Surgery COVID-19 Collaborative (VASCC) J Vasc Surg. 2020;72:379–380. doi: 10.1016/j.jvs.2020.04.463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Aziz F, Bath J, Smeds MR. Implications of the severe acute respiratory syndrome associated with the novel coronavirus-2 on vascular surgery practices. J Vasc Surg. 2021;73:4–11. doi: 10.1016/j.jvs.2020.08.118. e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Latz CA, Boitano LT, Png CYM, et al. Early vascular surgery response to the COVID-19 pandemic:results of a nationwide survey. J Vasc Surg. 2021;73:372–380. doi: 10.1016/j.jvs.2020.05.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mouawad NJ, Woo K, Malgor RD, et al. The impact of the COVID-19 pandemic on vascular surgery practice in the United States. J Vasc Surg. 2021;73:772–779. doi: 10.1016/j.jvs.2020.08.036. e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mahenthiran AK, Natarajan JP, Bertges DJ, et al. Impact of COVID-19 on the Society for Vascular Surgery Vascular Quality Initiative Venous Procedure Registries (varicose vein and inferior vena cava filter) J Vasc Surg Venous Lymphat Disord. 2021;9:1093–1098. doi: 10.1016/j.jvsv.2021.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Natarajan JP, Mahenthiran AK, Bertges DJ, et al. Impact of COVID-19 on the Society for Vascular Surgery Vascular Quality Initiative Arterial Procedure Registry. J Vasc Surg. 2021;73:1852–1857. doi: 10.1016/j.jvs.2020.12.087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mirza AK, Manunga J, Skeik N. Indirect casualties of COVID-19: perspectives from an American vascular surgery practice at a tertiary care centre. Br J Surg. 2020;107(8):e246. doi: 10.1002/bjs.11690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sarfati MR, Griffin CL, Kraiss LW, et al. Vascular surgery triage during the coronavirus disease 2019 pandemic. J Vasc Surg. 2021;73:1858–1868. doi: 10.1016/j.jvs.2020.11.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Boschetti GA, Di Gregorio S, Mena Vera JM, et al. COVID-19 impact on vascular surgery practice: experience from an Italian University Regional Hub Center for Vascular Pathology. Ann Vasc Surg. 2021;74:73–79. doi: 10.1016/j.avsg.2021.01.072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chisci E, Masciello F, Michelagnoli S. The Italian USL Toscana Centro model of a vascular hub responding to the COVID-19 emergency. J Vasc Surg. 2020;72:8–11. doi: 10.1016/j.jvs.2020.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chiesa R, Kahlberg A, Rinaldi E, et al. Emergency management of the COVID-19 pandemic in a vascular surgery department of a large metropolitan hospital in Italy. Preparation, escalation, de-escalation, and normal activity. J Card Surg. 2021;36:1632–1636. doi: 10.1111/jocs.14999. [DOI] [PubMed] [Google Scholar]
- 26.Piazza M, Xodo A, Squizzato F, et al. The challenge of maintaining necessary vascular and endovascular services at a referral center in Northern Italy during the COVID-19 outbreak. Vascular. 2021;29:477–485. doi: 10.1177/1708538120962964. [DOI] [PubMed] [Google Scholar]
- 27.Mascia D, Kahlberg A, Melloni A, et al. Single-center vascular hub experience after 7 weeks of COVID-19 Pandemic in Lombardy (Italy) Ann Vasc Surg. 2020;69:90–99. doi: 10.1016/j.avsg.2020.07.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pini R, Faggioli G, Vacirca A, et al. Is it possible to safely maintain a regular vascular practice during the COVID-19 pandemic? Eur J Vasc Endovasc Surg. 2020;60:127–134. doi: 10.1016/j.ejvs.2020.05.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Duarte A, Gouveia E Melo R, Lopes A, et al. Lessons learned from the impact of the COVID-19 pandemic in a vascular surgery department and preparation for future outbreaks. Ann Vasc Surg. 2021;73:97–106. doi: 10.1016/j.avsg.2021.01.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gouveia E Melo R, Pedro LM. Vascular surgery department adjustments in the era of the COVID-19 pandemic. J Vasc Surg. 2020;72:375–376. doi: 10.1016/j.jvs.2020.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ben Abdallah I. Early experience in Paris with the impact of the COVID-19 pandemic on vascular surgery. J Vasc Surg. 2020;72:373. doi: 10.1016/j.jvs.2020.04.467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Connolly MJ, Ahmed Z, Aly S, et al. The impact of COVID-19 on an Irish vascular unit's service. J Vasc Surg. 2021;73:347. doi: 10.1016/j.jvs.2020.07.082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Metelmann IB, Busemann A. Elective surgery in times of COVID-19: a two-centre analysis of postponed operations and disease-related morbidity and mortality. Z Evid Fortbild Qual Gesundhwes. 2020;158–159:62–65. doi: 10.1016/j.zefq.2020.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ünal EU, Mavioğlu HL, İscan HZ. Vascular surgery in the COVID-19 pandemic. J Vasc Surg. 2020;72:752–754. doi: 10.1016/j.jvs.2020.04.480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Correia M, Constâncio V, Silva JC, et al. Is there an impact of COVID-19 on admission of patients to the emergency department for vascular surgery? Ann Vasc Surg. 2020;69:100–104. doi: 10.1016/j.avsg.2020.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Leong Tan GW, Chandrasekar S, Lo ZJ, et al. Early experience in the COVID-19 pandemic from a vascular surgery unit in a Singapore tertiary hospital. J Vasc Surg. 2020;72:12–15. doi: 10.1016/j.jvs.2020.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ng JJ, Gan TRX, Niam JY, et al. Experience from a Singapore tertiary hospital with restructuring of a vascular surgery practice in response to national and institutional policies during the COVID-19 pandemic. J Vasc Surg. 2020;72:1166–1172. doi: 10.1016/j.jvs.2020.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bashar AHM, Hakim ME, Rahman MM, et al. Vascular surgery practice guidelines during COVID-19 pandemic in a setting of high work volume against limited resources: perspective of a developing country. Ann Vasc Surg. 2021;70:306–313. doi: 10.1016/j.avsg.2020.08.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wang J, Kuang M, Chen L, et al. Strategy for treating vascular emergencies during the COVID-19 pandemic in China. J Vasc Surg. 2020;72:1173–1177. doi: 10.1016/j.jvs.2020.05.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Benson RA, Nandhra S. The Vascular and Endovascular Research Network (VERN) COVID-19 Vascular Service (COVER) Tier 2 Study. Outcomes of vascular and endovascular interventions performed during the coronavirus disease 2019 (COVID-19 pandemic. Ann Surg. 2021;273:630–635. doi: 10.1097/SLA.0000000000004722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Aziz F, Behrendt CA, Sullivan K, et al. The impact of COVID-19 pandemic on vascular registries and clinical trials. Semin Vasc Surg. 2021;34:28–36. doi: 10.1053/j.semvascsurg.2021.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Nourazari S, Davis SR, Granovsky R, et al. Decreased hospital admissions through emergency departments during the COVID-19 pandemic. Am J Emerg Med. 2021;42:203–210. doi: 10.1016/j.ajem.2020.11.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.COVIDSurg Collaborative Mortality and pulmonary complications in patients undergoing surgery with perioperative SARS-CoV-2 infection: an international cohort study. Lancet. 2020;396(10243):27–38. doi: 10.1016/S0140-6736(20)31182-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Behrendt CA, Seiffert M, Gerloff C, et al. How does SARS-CoV-2 infection affect survival of emergency cardiovascular patients? A cohort study from a German insurance claims database. Eur J Vasc Endovasc Surg. 2021;62:119–125. doi: 10.1016/j.ejvs.2021.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.