Abstract
Decreased femoral anteversion is an often overlooked factor in femoroacetabular impingement (FAI), with potential to exacerbate both cam and pincer type impingement, or itself be the primary cause. Femoral de-rotation osteotomy (FDO) is a surgical option for symptomatic patients with such underlying bony deformity. This study aimed to investigate outcomes of FDO for management of symptomatic FAI in the presence of decreased (<5°) femoral anteversion. Secondary aims were to describe the surgical technique and assess complications. This study included 33 cases (29 patients) with average pre-operative anteversion measuring –3.1° (true retroversion). At an average follow-up of 1.5 years (19.8 months), 97% reported significant improvement. The overall average post-operative International Hip Outcome Tool (iHOT-33) score of 70.6 points (r: 23–98) compared to the average pre-operative score of 42.8 points (r: 0–56) for the 11 patients with available pre-operative scores suggests an overall improvement. The minimal clinically important difference for the iHOT-33 is 6.1 points. Patients with both pre- and post-operative iHOT-33 scores available demonstrated a statistically and clinically significant improvement of 37.7 (r: 13–70) points. There were three cases (9%) of delayed union and two cases (6%) of non-union early in the series which prompted evolution of the technique. Locking screw removal was performed in 33% of patients for a resultant overall re-operation rate of 45%. The findings suggest improvement in patient-reported outcomes can be achieved with FDO for symptomatic FAI in the setting of decreased femoral anteversion (<5°).
INTRODUCTION
Hip preservation surgery is rapidly evolving as is the current understanding of pathologic conditions that can affect young adult hips. One increasingly recognized cause of hip pain in young adults is femoroacetabular impingement (FAI). Ganz and associates had described the classic types of FAI which include cam, pincer, or mixed impingement [1]. Compared to acetabular version and coverage as well as femoral cam lesions, femoral version is an often overlooked factor in FAI [2].
Femoral version is determined as the angle between the femoral neck axis and the distal femoral condyles, often referenced to the transepicondylar or posterior condylar axis [3]. Normal anteversion in adults ranges from 8° to 20° [4–9], with ‘retroversion’ defined as less than 5° of anteversion [9, 10]. Prior to the introduction of the concept that FAI can lead to hip osteoarthritis [4, 8, 11, 12], Tönnis and Heinecke [13] had described the ‘diminished antetorsion syndrome’ as a cause of hip pain and early osteoarthritis. In their study, patients presented with ‘marked decrease in internal rotation (IR) of the femur, and a doubling of external rotation (ER)’, with hip pain beginning as early as age 12 but most often before age 30. The authors concluded that only rotational osteotomies to increase anteversion are successful in such patients. This study, however, did not explain the mechanism of osteoarthritis in patients with retroverted femora. It has been shown that when the femoral neck is retroverted, the peak joint pressure increases in hip flexion due to less clearance and may act as a cause of FAI [3]. Numerous studies have further implicated decreased femoral version in FAI with the potential to exacerbate both cam and pincer type impingement, or itself be the primary cause of impingement [7–9, 12, 14, 15]. In a study of 256 hips with FAI, Moya et al. [12] identified femoral retroversion in 16.6% of cases and also correlated increased rates of osteoarthritis in this group.
Although hip arthroscopy has rapidly evolved and is often successful in the treatment of symptomatic patients with FAI, it has been reported that patients with decreased femoral version are expected to have less successful outcomes [9, 10, 14, 16]. Alternatively, an anteverting femoral de-rotation osteotomy (FDO) may better correct the underlying bony deformities and the complex mechanical interactions of the hip. However, minimal data exist regarding outcomes of this surgical option [9].
The primary aim of this study was to investigate patient outcomes after anteverting FDO performed for management of symptomatic FAI in the presence of decreased femoral anteversion. The secondary aims of the study were to describe our surgical technique as well as assess osteotomy union rates and complications.
MATERIALS AND METHODS
This retrospective case-series included prospectively collected data of adolescent and adult patients who underwent elective FDO by the senior author (KDJ) for symptomatic FAI in the presence of decreased femoral version at our institution during the 6-year period of May 2013 to October 2019. The study was approved by the Conjoint Health Research Ethics Board at the University of Calgary. The inclusion criteria were as follows: (i) any patient who presented with symptomatic FAI with limited IR with the hip flexed to 90° and a total arc of rotational motion greater that 60° (ii) had decreased femoral anteversion (less than 5°) on imaging; (iii) their symptoms failed to improve with non-operative treatment (minimum 3 months of targeted physiotherapy and activity modifications); (iv) subsequently underwent elective anteverting FDO; (v) has completed a minimum 6-month post-operative follow-up period and (vi) was minimum 16 years of age at the time of surgery.
Patient demographic data, including age, gender and symptomatic side, as well as the implants utilized and occurrence of intra- or post-operative complications, were collected from patients’ medical records.
Clinical exam
Pre-operatively, a comprehensive physical exam was performed and recorded by the principle investigator (PI) KDJ. Diagnosis of FAI was made clinically based on patient history as well as suggestive physical exam findings such as reduced IR with the hip flexed, and positive provocative anterior impingement with hip flexion, adduction and IR. Passive hip range of motion (ROM) was evaluated with the patient supine and the hip at 90°, and the degree of IR and ER was clearly documented.
Imaging
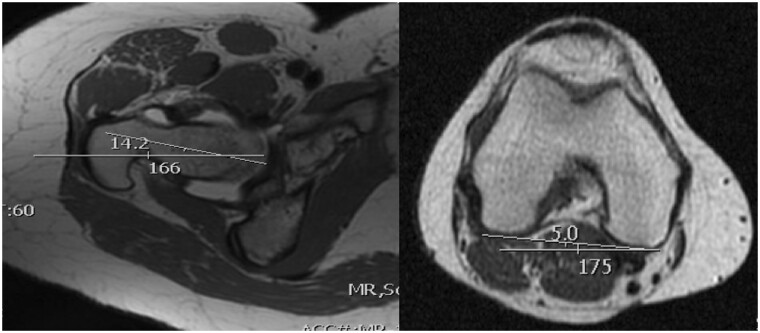
All patients had standardized supine pelvic anteroposterior (AP) and Dunn’s lateral plain radiographs of the affected hip. Signs of chondrosis were documented based on Tonnis classification [17], and the lateral center-edge angle (LCEA) and alpha angle were measured in a standardized fashion. Magnetic resonance imaging (MRI) or magnetic resonance arthrogram of the affected hip was acquired for all patients to assess for intra-articular hip pathology. Femoral version angle was determined in all cases via advanced imaging involving both the hip and knee. If the initial MRI did not include this ‘femoral torsional protocol’ then versional information was subsequently acquired by low dose computed tomography (CT) scan at the hip and knee due to improved availability compared to MRI, or via an EOS imaging system. On MRI and CT imaging the femoral version was calculated as the angle between the femoral neck axis and the posterior condylar axis of the femur (Fig. 1). The technique described by Weiner et al. was used to determine the most true axis of the femoral neck with a line drawn between three points equidistant between the superior and inferior cortical neck [5]. Post-operative plain radiographs of the affected hip and ipsilateral femur (AP and lateral views) were obtained at 6 weeks, 3 months, 6 months and 1 year.
Fig. 1.
Select images of a pre-operative MRI demonstrating measurement of the femoral version angle of –9.2°. The femoral neck is 14.2° retroverted to the horizontal line while the distal femur is 5° internally rotated. 73 × 31 mm (300 × 300 DPI).
Outcome measures
Clinical outcomes were assessed utilizing the International Hip Outcome Tool (iHOT-33) [18]. iHOT-33 scores were not routinely collected until 2016 and therefore pre-operative scores were unavailable for 22 cases. The patient’s subjective perception of improvement post-operatively was also recorded throughout clinical follow-up visits. Resolution or ongoing presence of a positive anterior impingement sign was identified, as was post-operative hip ROM at 6–12 months post-operatively. Rates and timing of osteotomy union as well as intra- and post-operative complications were assessed.
AUTHORS PREFERRED SURGICAL TECHNIQUE
All procedures were performed by the senior author (KDJ). The procedure evolved over time and the refined technique that is routinely used is presented here. Patients receive either general or spinal anesthesia along with intravenous antibiotic prophylaxis. Patients are positioned supine on a fracture table with a perineal post to facilitate intra-operative fluoroscopic imaging. Both hips are examined under anesthesia and the pre-operative ROM documented. The operative leg is freely draped while the non-operative leg is positioned in a leg holder flexed and abducted. A piriformis fossa entry is obtained to optimize a colinear trajectory with the intramedullary canal to facilitate rotational correction. Sequential reaming of the femoral canal is performed until optimal cortical contact is obtained and the size of the final reamer is 1 mm greater than the desired nail diameter. Preferably, a nail with diameter of 12 mm or larger is used as smaller nail diameters were used in the early cases where non-union occurred. All intramedullary reamings are collected to be used as bone graft. In order to prevent varus mal-alignment of the proximal femur, the osteotomy level is planned with fluoroscopy to allow the nail to provide a minimum two cortical diameters endosteal contact in the proximal femoral segment. The guidewire is retracted proximal to the osteotomy location. A 4–5 cm sub-vastus lateral approach is performed with minimal periosteal disruption, and a Bennett retractor inserted over the anterior femur. The lateral cortex is scored longitudinally using an oscillating surgical saw (Fig. 2A) to assess rotational correction. A transverse osteotomy is performed with the oscillating saw. Copious irrigation and meticulous maintenance of a clean saw blade with no bone debris clogging the teeth are used to minimize thermal necrosis of bone. The minimal soft-tissue dissection at the osteotomy site maintains sufficient stability of the proximal and distal fragments such that no displacement typically occurs, and no temporary reduction and stabilization is required. Once the osteotomy is complete, the guidewire is re-introduced and a T2 Stryker nail inserted. One partially threaded locking screw is inserted into the proximal dynamic hole. The nail handle is removed to facilitate hip ROM assessment. Rotational correction is performed by flexing the hip to 90° and internally rotating until a point of impingement is encountered, at which point the distal fragment is then further internally rotated to achieve a minimum 20° of IR (Fig. 3). It is our anecdotal belief that patients generally require at least 15° of IR with the hip flexed to 90° to function regularly without impingement, therefore this maneuver directly improves the femoroacetabular conflict. The leg is then carefully extended without allowing further rotation, and a supplementary assessment of correction performed based on the angular change of the score mark at the osteotomy site (Fig. 2B), along with overall rotational alignment of the limb. A single static locking screw is then inserted distally and the hip is again flexed to 90°, with IR and ER assessed and documented ensuring a more balanced arc of rotation. In the extended position, the leg is checked to ensure the patella is forward facing and foot progression angle is less externally rotated (Fig. 4). A compression screw is inserted through the proximal end of the nail to contact the smooth portion of the partially threaded proximal locking screw and compress the osteotomy (Fig. 5). The osteotomy site is then grafted with the intramedullary reamings to enhance bone healing. The proximal wound is thoroughly irrigated to minimize formation of heterotopic ossification (HO).
Fig. 2.
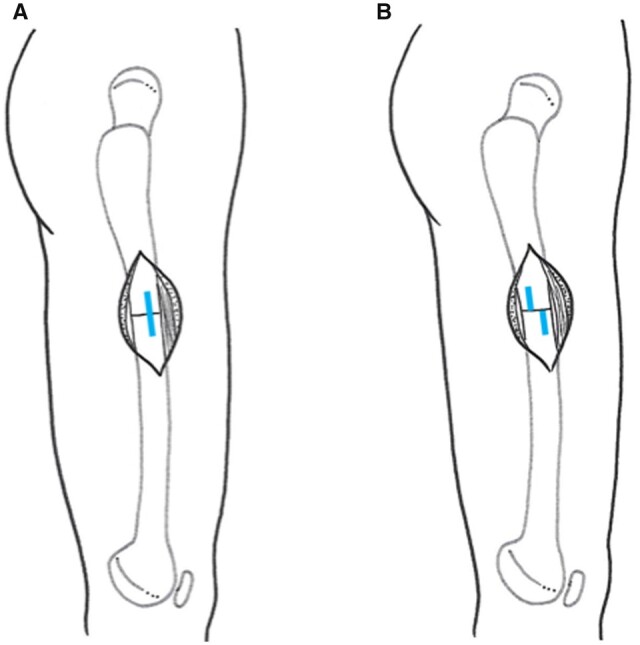
(A) The lateral femoral cortex is marked with a longitudinal 3 cm scratch mark using a power surgical saw and a transverse osteotomy is performed. (B) Shows the achieved correction of the femoral version after femoral de-rotation. (i) 8 × 18 mm (300 × 300 DPI) and (ii) 7 × 18 mm (300 × 300 DPI).
Fig. 3.

Following insertion of the proximal locking screw, the hip is flexed to 90° and internally rotated until a point of impingement is encountered, then the distal fragment is further internally rotated to achieve a minimum 20° of IR. 11 × 23 mm (300 × 300 DPI).
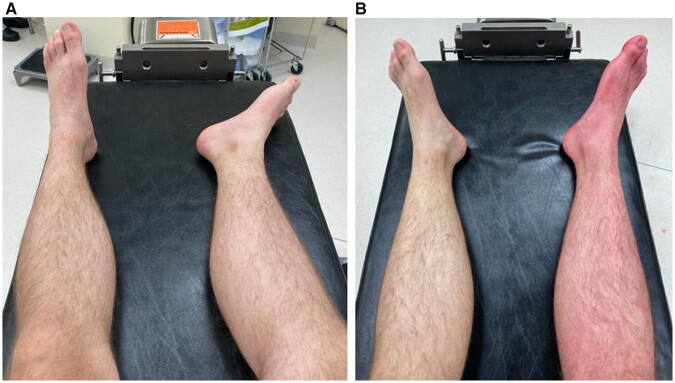
Fig. 4.
Pre-operative (A) and immediate post-operative (B) images demonstrating decreased external foot position following a right anteverting de-rotational femoral osteotomy. (i) 36 × 38 mm (300 × 300 DPI) and (ii) 33 × 39 mm (300 × 300 DPI).
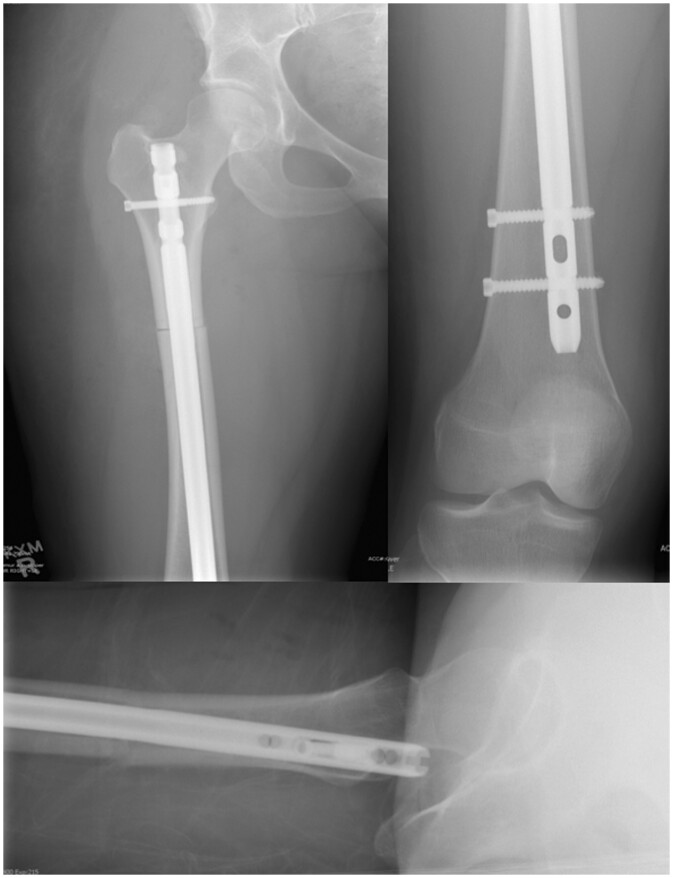
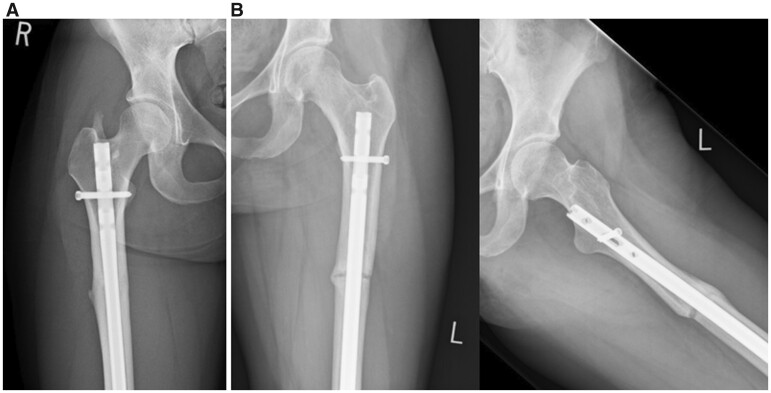
Fig. 5.
Immediate post-operative AP and lateral plain radiographs of the same patient shown in Fig. 1, demonstrating fixation of the FDO with an intramedullary nail. 49 × 65 mm (300 × 300 DPI).
Post-operative protocol
Patients are allowed to fully weight bear with crutches. Thromboprophylaxis is given for 28 days. The surgical wounds are reviewed at 10–14 days post-operatively. Follow-up at 6, 12 and 24 weeks, and 1 year post-operatively includes clinical and radiographic assessment.
RESULTS
A total of 33 femoral de-rotation osteotomies performed in 29 patients met the inclusion criteria. Pre-operative patient demographics and findings are demonstrated in Table I. Average age at time of surgery was 29 (r: 17–45) years and average femoral anteversion –3.1 (r: –21–4) degrees. Mean duration of follow-up was 19.8 (r: 6–48) months.
Table I.
Pre-operative patient demographics along with associated clinical and imaging findings (IR = Internal Rotation; ER = External Rotation; CEA = Lateral Center-Edge Angle)
| Patient demographics | Age at surgery (years) | 29 (r : 17–45) |
| Gender | 5 male (17%) | |
| 24 female (83%) | ||
| Laterality | 18 right; | |
| 7 left; | ||
| 4 bilateral | ||
| Femoral anteversion angle (degrees) | –3.1 (r: –21 to 4) | |
| Previous hip arthroscopy | 3/33 cases | |
| Pre-operative clinical findings | Positive hip impingement sign | 33/33 cases |
| Hip IR (degrees) | 6.7 (r: 0–15) | |
| Hip ER (degrees) | 70.6 (r: 45–90) | |
| Pre-operative X-ray | Tonnis grade 0 | 33/33 cases |
| CEA (degrees) | Mean 31.8 (r: 18–47); | |
| 1 patient (2 hip cases) <25 | ||
| Alpha angle (degrees) | Mean 50.6 (r: 38–72); | |
| 14/33 cases ≥ 50 | ||
| Pre-operative MRI | Presence of labral pathology | 25/33 hips (76%) |
| Articular degeneration | Mild: 6 hips (18%); | |
| Moderate: 1 hip |
The median diameter of femoral nail inserted was 12 mm (r: 9–13 mm). A uni-cortical fixed locking compression plate (LCP) was employed to control rotation in 6/33 cases early in the case-series although the technique evolved with time ultimately eliminating this step for the remainder of cases.
Post-operatively, 97% of patients reported overall subjective improvement in pain and satisfaction by final assessment. One patient with hypermobility, suspected Ehlers–Danlos syndrome and a poor pain response had persistent residual symptoms which correlated with an iHOT-33 score of only 23 at over 2 years post-operatively. Pre-operative iHOT-33 scores were available for only 11 cases with an average score of 42.8 (r: 0–56). Post-operative iHOT-33 scores were obtained for 29/33 (88%) of cases. The average post-operative iHOT-33 score was 70.6 (r: 23–98) at a mean follow-up of 16.5 months. For those with both pre- and post-operative iHOT-33 scores, the average improvement was 37.7 points (r: 13-70, P-values < 0.001). Mean change in hip IR was 23° increase (P < 0.001) and ER 27° decrease (P < 0.001) (Table II). Seven cases (21%) continued to have a mildly positive anterior hip impingement sign at 6–12 months following surgery, although all of these patients had progressive improvement of symptoms with non-operative treatment and continued follow-up.
Table II.
Mean pre- and post-operative hip IR and ER along with average improvement following FDO
| Pre-operative | Post-operative | Improvement | |
|---|---|---|---|
| IR (degrees) | 6.7 (r: 0–15) | 29.7 (r: 15–45) | 23 (P < 0.001) |
| ER (degrees) | 70.6 (r: 45–90) | 43.4 (R: 30–70) | 27° (P < 0.001) |
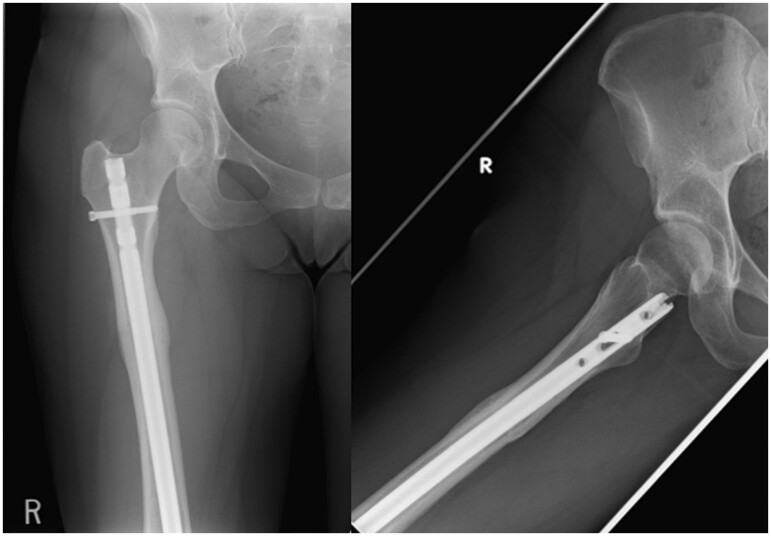
Union was achieved in 27/33 (82%) cases (Fig. 6) by 6 months as determined clinically and radiographically (bridging callus on three of four cortices).
Fig. 6.
Six month post-operative plain radiographs of the previous patient shown in Figs. 1 and 5, demonstrating complete union of the FDO. 57 × 39 mm (300 × 300 DPI).
Complications
There were three intra-operative un-displaced fractures involving the osteotomy identified during surgery. All three were managed with elimination of the active compression step, and one with the addition of a cerclage wire. Two of these cases were still dynamically locked with post-operative partial weight bearing. One was statically locked and ultimately required dynamization at 5 months for persistent lateral cortical gapping. Three patients (9%) had delayed union (Fig. 7A). Two of these patients united by 12 months, one of which had experienced an intra-operative fracture with a partial weight bearing protocol post-operatively. The third patient with a delayed union declined an exchange intramedullary nailing procedure at 18 months and ultimately united by 2 years. Two patients (6%) had an oligotrophic non-union and underwent femoral exchange nailing with insertion of a proximal compression screw at 8 months post-operatively. Union was ultimately achieved at 13 and 17 months following the index procedures. It was noted that 1 patient with delayed union had received a size 11 intramedullary nail, and one patient with non-union had received a size 10 intramedullary nail with the addition of an LCP. HO was identified in three patients with one being asymptomatic, one with limited peri-trochanteric pain not warranting excision and the third patient with a large symptomatic prominence at the proximal nail insertion with an excision procedure planned (Fig. 7B). The HO prominence in this particular patient was impinging on the sciatic nerve as demonstrated on dynamic ultrasound, with the patient experiencing numbness with hip flexion. Two patients (6%) had post-operative trochanteric bursitis and responded to local steroid injections. One patient experienced a post-operative spinal headache and received an epidural blood patch procedure.
Fig. 7.
Post-operative X-ray images demonstrating (A) AP image of a patient with HO at the proximal nail insertion. (B) AP and lateral images of a delayed union at 6 months. The osteotomy had not been actively compressed during surgery in this particular case. (i) 19 × 32 mm (300 × 300 DPI) and (ii) 47 × 32 mm (300 × 300 DPI).
DISCUSSION
Previous studies have described FDO procedures for decreased femoral version and impingement through numerous techniques. These include sub-trochanteric osteotomies with LCP fixation, closed intramedullary de-rotation procedures, as well as procedures with adjuvant hip arthroscopy for eradication of secondary cam impingement arising from severe femoral retroversion [9, 19]. However, to our knowledge, no study has focused on patient-reported outcomes. In our study of 33 cases with an average follow-up of 1.5 years (19.8 months), 97% of patients reported overall subjective improvement in pain and satisfaction by final assessment. Further characterization of improvement was attempted with employment of a patient-reported outcome measure tool, the iHOT-33. The refined technique that is currently employed is described, although this procedure had evolved during this study.
The iHOT-33 score was designed as a self-administered outcome tool to measure health-related quality-of-life in young active patients with hip disorders, and specifically to be used as a primary outcome measure. Through evaluation of 4 key domains, a score of 0–100 is generated, with the latter representing the best possible quality-of-life [18]. In our study, the average post-operative iHOT-33 score of 70.6 points (r: 23–98) compared to the average pre-operative score of 42.8 points (r: 0–56) for the 11 patients with available pre-operative scores suggests an overall improvement. The minimal clinically important difference for the iHOT-33 is 6.1 points, and during the development and assessment of the tool, the mean scores in the responsiveness cohort with ‘much improvement’ were 32/100 at baseline and 65/100 at 6 months, with a mean change in score of 33 [18]. In the present study, the individual cases with both pre- and post-operative iHOT-33 scores completed demonstrated a statistically and clinically significant improvement of 37.7 (r: 13–70) points.
It is interesting to note that no intra-articular surgery was performed in our cohort of patients as we wished to target the underlying mechanical pathology, to ideally provide the most significant amount of improvement with a single procedure. The importance of labral function and the necessity of labral repair or preservation on clinical outcomes has been stressed in the literature [2]. However, others have suggested that although labral pathology often co-exists in young patients with hip pain, it is usually morphological abnormalities that cause pain due to abnormal loading and impingement, with labral pathology occurring secondarily [16]. This concept that optimum treatment should address the underlying mechanical pathology provides support to our finding of improved clinical outcomes despite the presence of labral pathology in 25/33 hips (76%) that was not specifically addressed. Regarding femoral neck cam lesions, normal and pathological values for alpha angles remains somewhat controversial although most authors suggest a value of 50° or greater to be abnormal [2, 8, 20]. In our study, 14/33 cases (42%) had alpha angles above this threshold. The cam lesions of these patients were not addressed via osteochondroplasty yet decreased impingement and improved patient outcomes were achieved through anteverting FDO. Overall, it is unknown if our cohort of patients would have had different results with intra-articular procedures either in addition or in isolation, such as cam osteochondroplasty for cam or pincer impingement, or labral repair when indicated. However, three of the cases had previously undergone one or more hip arthroscopies for impingement with persistence of symptoms that improved after FDO. The authors therefore suspect that alpha angles should ultimately be interpreted in conjunction with femoral neck anteversion angles as increased femoral anteversion can provide an element of protection from anterior impingement, even in the presence of an anterosuperior cam lesion. However, further investigation is necessary to determine the most appropriate indications for FDO compared to hip arthroscopy for FAI in the setting of decreased femoral version.
Wyss et al. (2007) found a strong correlation between hip IR in 90° flexion and the measurable free space between particular bony contours on MRI. The authors suggested that the clinical range of IR is closely related to skeletal anatomy, and can be used as a non-invasive tool to predict the risk of impingement [21]. Several other studies have demonstrated similar correlation between femoral version and resultant ROM with decreased anteversion resulting in decreased internal hip rotation and an increase in ER [8, 9, 12, 16]. Our cohort of patients with decreased femoral anteversion (average –3.1°) reflected these clinical findings (Table II).
Any femoral osteotomy procedure carries significant risk for complications and consequently has an associated learning curve. As such, the DFO procedure presented had evolved over time and the issues of delayed- and non-union were in the first 10 cases performed with alternate techniques. In response to potential technical factors identified as a cause, a minimum nail size of 12 mm, a compression screw and no uni-cortical LCP is now routine. In cases of identified HO, only one case was associated with symptoms warranting an excision. There were 11 cases (33%) of patients who underwent removal of locking screws for mild soft-tissue irritation, however, this in addition to the three procedures for delayed- or non-union early in the series, along with the one planned excision of HO resulted in an overall re-operation rate of 45%.
Strengths of this study include the focus on the isolated effect of an FDO for patients with symptomatic hip impingement and decreased femoral anteversion, despite the significant presence of other pathologic findings including cam lesions, labral pathology and hip dysplasia that was not addressed. To our knowledge, this is the first study examining patient-reported outcomes for this particular procedure in this subset of patients. In addition, all surgical procedures were performed by a single surgeon (KDJ), minimizing variation in procedure and resultant outcome influence.
There are, however, limitations to our study. Although outcome data were collected prospectively, it was analysed retrospectively, which could potentially lead to selection bias. This risk was minimized with the use of specific inclusion criteria. The retrospective nature of this study also resulted in pre-operative iHOT-33 scores not being available for all patients. The PI now routinely collects iHOT-33 scores on all patients pre-operatively and at 6–12 months and 2 years post-operatively. This became a routine clinical practice part-way through this case-series. In addition, all clinical findings were documented solely by the treating surgeon, leaving the potential for bias. The mean follow-up duration of 20 months is another limitation as longer-term assessment can better reflect the impact of a procedure.
CONCLUSION
Improvement in both patient-reported outcomes as well as clinical findings can be achieved with FDO for symptomatic hip impingement in the setting of decreased femoral anteversion (less than 5°), despite the potential presence of other pathologic findings. Although literature focusing on hip preservation continues to rapidly expand, further study in this particular area is required to optimize surgical management of the challenging pathologies leading to FAI.
ACKNOWLEDGMENTS
Ms. Saboura Mahdavi, Ms. Sophie Piroozfar and Ms. Kate Boyd for their assistance with administering iHOT-33 scores, data collection and statistical analysis. Dr. Eva Gusnowski for artistic renderings.
CONFLICT OF INTEREST STATEMENT
None declared.
DATA AVAILABILITY
The data underlying this article will be shared on reasonable request to the corresponding author.
REFERENCES
- 1. Myers SR, Eijer H, Ganz R. Anterior femoroacetabular impingement after periacetabular osteotomy. Clin Orthop Relat Res 1999; 363: 93–9. [PubMed] [Google Scholar]
- 2. Jackson TJ, Lindner D, El-Bitar YF et al. Effect of femoral anteversion on clinical outcomes after hip arthroscopy. Arthrosc–J Arthrosc Relat Surg 2015; 31: 35–41. [DOI] [PubMed] [Google Scholar]
- 3. Satpathy J, Kannan A, Owen JR et al. Hip contact stress and femoral neck retroversion: a biomechanical study to evaluate implication of femoroacetabular impingement. J Hip Preserv Surg 2015; 2: 287–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Reikeråls O, Bjerkreim I, Kolbenstvedt A. Anteversion of the acetabulum and femoral neck in normals and in patients with osteoarthritis of the hip. Acta Orthop 1983; 54: 18–23. [DOI] [PubMed] [Google Scholar]
- 5. Weiner DS, Cook AJ, Hoyt WA et al. Computed tomography in the measurement of femoral anteversion. Orthopedics 1978; 1: 299–306. [PubMed] [Google Scholar]
- 6. Sugano N, Noble PC, Kamaric E. A comparison of alternative methods of measuring femoral anteversion. J Comput Assist Tomogr 1998; 22: 610–4. [DOI] [PubMed] [Google Scholar]
- 7. Ito K, Minka-II M-A, Leunig M et al. Femoroacetabular impingement and the cam-effect. J Bone Joint Surg Br 2001; 83-B: 171–6. [DOI] [PubMed] [Google Scholar]
- 8. Ejnisman L, Philippon MJ, Lertwanich P et al. Relationship between femoral anteversion and findings in hips with femoroacetabular impingement. Orthopedics 2013; 36: e293–300. [DOI] [PubMed] [Google Scholar]
- 9. Matsuda DK, Gupta N, Martin HD. Closed Intramedullary derotational osteotomy and hip arthroscopy for cam femoroacetabular impingement from femoral retroversion. Arthrosc Tech 2014; 3: e83–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Fabricant PD, Fields KG, Taylor SA et al. The effect of femoral and acetabular version on clinical outcomes after arthroscopic femoroacetabular impingement surgery. J Bone Joint Surg Am 2015; 97: 537–43. [DOI] [PubMed] [Google Scholar]
- 11. Ganz R, Parvizi J, Beck M et al. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res 2003; 417: 112–20B. [DOI] [PubMed] [Google Scholar]
- 12. Moya L, Buly R, Henn F et al. Femoral retroversion in patients with femoroacetabular impingement: a cofactor in the development of hip osteoarthritis. Orthopaedic Proceedings 2010; 92–B:SUPP_IV, 526. [Google Scholar]
- 13. Tönnis D, Heinecke A. Diminished femoral antetorsion syndrome: a cause of pain and osteoarthritis. J Pediatr Orthop 1991; 11: 419–31. [DOI] [PubMed] [Google Scholar]
- 14. Kamath AF, Ganz R, Zhang H et al. Subtrochanteric osteotomy for femoral mal-torsion through a surgical dislocation approach. J Hip Preserv Surg 2015; 2: 65–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Bedi A, Dolan M, Hetsroni I et al. Surgical treatment of femoroacetabular impingement improves hip kinematics: a computer-assisted model. Am J Sports Med 2011; 39: 43–49S. [DOI] [PubMed] [Google Scholar]
- 16. Peters CL, Erickson J. The etiology and treatment of hip pain in the young adult. J Bone Joint Surg 2006; 88A: 20–6. [DOI] [PubMed] [Google Scholar]
- 17. Kovalenko B, Bremjit P, Fernando N. Classifications in brief: Tonnis classification of hip osteoarthritis. Clin Orthop Relat Res 2018; 476: 1680–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Mohtadi NGH, Griffin DR, Pedersen ME et al. , Multicenter Arthroscopy of the Hip Outcomes Research Network. The development and validation of a self-administered quality-of-life outcome measure for young, active patients with symptomatic hip disease: the International Hip Outcome Tool (iHOT-33). Arthrosc–J Arthrosc Relat Surg 2012; 28: 595–610 e1. [DOI] [PubMed] [Google Scholar]
- 19. Huber H, Haefeli M, Dierauer S et al. Treatment of reduced femoral antetorsion by subtrochanteric rotational osteotomy. Acta Orthop Belg 2009; 75: 490–6. [PubMed] [Google Scholar]
- 20. Barrientos C, Barahona M, Diaz J et al. Is there a pathological alpha angle for hip impingement? A diagnostic test study. J Hip Preserv Surg 2016; 3: 223–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Wyss TF, Clark JM, Weishaupt D et al. Correlation between internal rotation and bony anatomy in the hip. Clin Orthop Relat Res 2007; 460: 152–8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data underlying this article will be shared on reasonable request to the corresponding author.