Abstract
In adult patients with dental phobia, dental treatment may be difficult, or may not be possible. Depending on the level of fear or anxiety, non-pharmacological or pharmacological behavior management techniques are used in the dental treatment of such patients. Among the pharmacological behavior management techniques, minimal sedation, that is, the lowest depth of sedation, can be easily obtained in adult patients using oral sedatives, does not require special equipment or tools, and does not affect ventilatory and cardiovascular function. Diazepam is an anxiolytic drug belonging to the benzodiazepine family that, in addition to relieving anxiety, produces muscle relaxation, and is a representative drug used in adult patients with fear of dental treatment. Herein, we report the case of a 50-year-old woman with severe dental fear who successfully underwent long-term dental treatment in approximately 20 visits with minimal sedation using oral diazepam. In addition, we reviewed the considerations for the use of benzodiazepines for minimal sedation.
Keywords: Benzodiazepine, Dental Phobia, Diazepam, Minimal Sedation, Oral Sedative
INTRODUCTION
A significant proportion of the adult population (approximately 30%–40%) has severe dental fear. Patients with dental fear or anxiety may have difficulty in undergoing dental treatment [1]. It has been reported that causes of dental fear include negative experiences of previous dental treatment, pain during local anesthesia, handpiece noise or vibration, fear of sharp instruments, loss of the ability to control the situation during treatment, passive personality or psychological factors, and negative perception of the dental practitioner [1].
Non-pharmacological behavior management techniques, pharmacological sedation, or a combination of both can be used in the dental treatment of adult patients with dental fear [2]. Non-pharmacological behavior management techniques include psychological approaches using the Tell-Show-Do technique or listening to music to divert the attention and relieve tension [1]. Pharmacological management is divided into minimal sedation, conscious sedation, deep sedation, and general anesthesia, depending on the depth of sedation [2].
Minimal sedation has the lowest depth of sedation [2,3]. It does not affect airway maintenance, ventilatory function, and cardiovascular function, and communication with the clinician is possible [2,3]. Patients categorized as Class I or Class II according to the patient classification of the American Society of Anesthesiologists (ASA), that is, healthy patients with no organic, physiological, biochemical, or mental disorders, and patients with mild systemic diseases or disorders, respectively, are indicated for minimal sedation [3]. It is recommended that patients categorized as Class III or Class IV are referred to a better equipped hospital and managed under medical supervision [3,4].
Minimal sedation is performed via the oral route or by inhalation of nitrous oxide [3]. Oral sedation is simple and familiar for adult patients, does not cause pain, requires no complicated equipment, and is less expensive than inhalation sedation [3,4]. Many studies related to these techniques have been reported in pediatric patients [4]. However, there are relatively few studies on oral sedation in adult patients, and there have been few investigations on adult sedation in Korea. In most studies, limited short-term cases have been reported [4].
As the first choice in patients with anxiety disorders, benzodiazepines are the most used anti-anxiety drugs and are also effectively used to reduce anxiety during dental treatment [4]. They have a wider safety margin than barbiturates, and their effect can be reversed by the antagonist flumazenil [4]. There are various types of benzodiazepines, such as alprazolam, clonazepam, diazepam, lorazepam, midazolam, and triazolam. Drugs can be selected considering the onset, half-life, action time, metabolic pathway, and presence of active metabolites [4].
We report a case of an adult patient with severe dental fear who successfully underwent long-term dental treatment over multiple visits under minimal sedation using oral diazepam. In addition, we reviewed the considerations for the use of benzodiazepines for minimal sedation.
CASE REPORT
A 50-year-old woman (weight, 52 kg) with severe dental fear visited the Department of Advanced General Dentistry at our hospital in 2019 for dental treatment under sedation. She had anxiety disorders, hypertension, hyperlipidemia, and osteoporosis. Regarding anxiety disorders, she had been taking an anti-anxiety drug prescribed by a private clinic very occasionally when she was very anxious. Medications related to hypertension, hyperlipidemia, and osteoporosis were taken daily. According to the past dental history, during treatment at a private dental clinic three years ago, dyspnea occurred due to severe anxiety and fear, and the dental treatment was interrupted. After that, she had not been able to visit the dentist until now. Following oral and radiographic examination, she was diagnosed with loss of multiple teeth, chronic periodontitis, and dental caries of the remaining teeth (Fig. 1). Complicated treatment including surgical, endodontic, and prosthodontic treatment was planned and was expected to take more than 1 year.
Fig. 1. Initial panoramic radiograph.
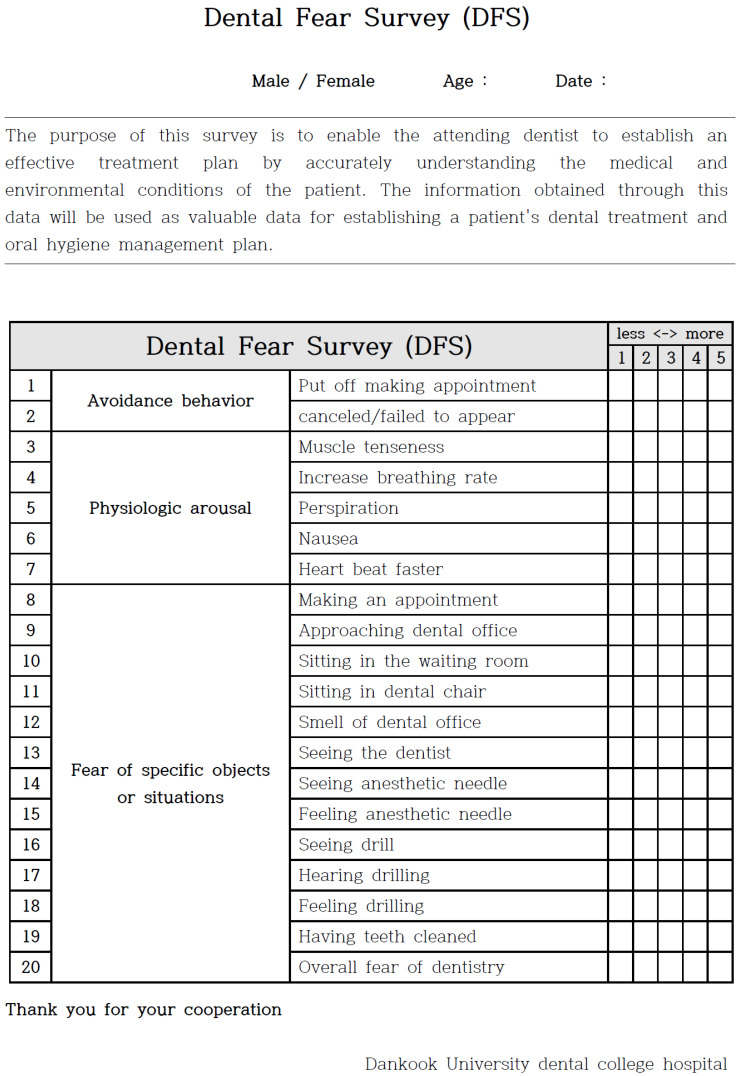
We decided to perform pharmacological sedation according to the patient's request with the lowest depth of sedation, that is, minimal sedation. The drug used for minimal sedation was diazepam (Valium®, Roche), which has been previously used for anxiolytic effects. We planned to switch to deep sedation or general anesthesia if minimal sedation was insufficient to relieve anxiety. (Fig. 2). The patient was informed that the dose of diazepam should not exceed 5–10 mg and should be taken 1 h before treatment. To measure the dental fear, we used Kleintnecht's Dental Fear Survey (DFS) at every visit. The patient arrived at the dental office 1 h before the scheduled appointment with a guardian and took 10 mg of diazepam. A dental fear survey was completed during the waiting time immediately after taking diazepam. (Fig. 3) [5]. The dental care team comprised up of an operator with a current certificate of Basic Life Support Instructor, and an assistant certified as a Basic Life Support Provider. Vital signs, such as blood pressure and pulse rate, were monitored during the pre- and post-operative periods at every visit. In addition, we confirmed that the patient was able to respond to verbal commands appropriately during treatment.
Fig. 2. Treatment flow for minimal sedation.
Fig. 3. Kleintnecht's dental fear survey [5].
In order to evaluate the anxiolytic effect of minimal sedation, we decided to perform simple treatment initially and gradually increase the difficulty of the procedure (Fig. 2). During the test treatment, a simple extraction of the right maxillary first molar with mobility was planned. The initial DFS index was 97. One hour after taking diazepam, the patient still showed restlessness and fear. The operator achieved behavior control by communicating with the patient in a calm tone and encouraging the patient. The patient was sedated, and local anesthesia for tooth extraction was successfully performed. No events occurred during the local anesthesia. During treatment, the patient was instructed to practice deep breathing to relieve her tension. The treatment time was 15 min. The preoperative and postoperative blood pressure and pulse rate were 136/92 mmHg and 90 bpm, and 125/87 mmHg and 81 bpm, respectively. The patient remained conscious and responded normally. After the discharge criteria were met, the patient was sent to her guardian (Table 1) [2].
Table 1. Discharge criteria [2].
| Vitals | Normalization |
| Airway | No potential for obstruction |
| Consciousness | Fully responsive and alert / Verbalize appropriately |
| Companion | Responsible companion for transportation |
| Postoperative instructions | Provide written instructions |
At the second visit after one week, the DFS index was 89; the patient received the same dose of diazepam one hour before the treatment. To reinforce the positive experience of dental treatment, the left mandibular second premolar with mobility was extracted and suturing of the extraction site was performed, which was a simple treatment. The treatment lasted for 63 min. The preoperative and postoperative blood pressure and pulse rate were 127/83 mmHg and 85 bpm, and 125/82 mmHg and 83 bpm, respectively.
At the third visit one week later, the same dose of diazepam was administered with the same regimen. The patient appeared to be stable. The DFS index decreased to 74. Following removal of the sutures at the extraction site, the mandibular anterior teeth were prepared and provisional restorations were fabricated. The differences between simple extractions and tooth preparation were explained to the patient before treatment. The treatment time was 150 min. Blood pressure and pulse rate were stable in the pre- and postoperative periods.
Thereafter, the patient visited the hospital every 2 to 3 weeks, and complicated prosthetic treatments, endodontic treatments, tooth extractions, and implant surgery with bone graft were performed under minimal sedation using 10 mg of diazepam. The treatment was uneventful. Oral rehabilitation with dental implants and fixed dental prostheses was performed (Fig. 4). The total treatment duration was 17 months. There were 20 visits, out of which, minimal sedation was administered in 16 (Table 2). Four simple and short procedures, such as suture removal were performed without sedation. The interval between visits was at least 1 week. The mean interval between visits was 25.5 days. The DFS index was 97 at the first visit, but it decreased continuously as the number of visits increased, and was 43 at the 20th visit (Fig. 5). At every visit, the pre- and postoperative blood pressure and pulse rate were within the normal range. The patient complied with the dosage and administration of diazepam. No adverse effects were observed. The patient stated that she was taking diazepam only during dental treatment. No tendency for drug abuse or dependence was observed.
Fig. 4. Clinical findings after 17 months of dental treatment under minimal sedation (A) Intraoral photograph, (B) Panoramic radiograph.
Table 2. Dental procedures and dental fear level of patients at each dental visit.
| Visit number | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
|---|---|---|---|---|---|---|---|---|---|---|
| Dental procedures | ext | ext | pros | ext pros | s/o | pros rct | pros | imp | s/o pros | imp |
| Diazepam dosage (mg) | 10 | 10 | 10 | 10 | 0 | 10 | 0 | 10 | 10 | 10 |
| Dental fear survey | 97 | 89 | 74 | 70 | 70 | 70 | 70 | 65 | 65 | 68 |
| Treatment time (min) | 15 | 63 | 150 | 97 | 4 | 44 | 43 | 140 | 52 | 99 |
*ext, tooth extraction; pros, prosthodontic treatment; s/o, stitch out; rct, root canal treatment; imp, implant surgery.
Fig. 5. Dental fear survey index, evaluated using Kleintnecht's dental fear survey.
DISCUSSION
Our patient was classified as ASA II with mild systemic disease and no drug allergy. Considering that it was a complicated case that required multiple visits and a long treatment period, deep sedation or general anesthesia were considered. However, repetitive general anesthesia has disadvantages such as postoperative discomfort, high anesthesia cost, and no communication between the patient and clinician during dental treatment. Therefore, minimal sedation was preferentially planned. The patient exhibited a very high dental fear at the first visit, but as the treatment progressed, the fear index decreased. This indicates that minimal sedation can be effective in adult patients with anxiety and dental phobia.
The oral sedative used in this case was diazepam, which is a long-acting benzodiazepine. It has a lesser sedative effect than midazolam, but has strong anti-anxiety and muscle relaxation effects. It is used effectively in patients with dental anxiety [4]. As it has strong lipid solubility, it is rapidly absorbed from the gastrointestinal tract, and the highest plasma concentration is reached after 1–2 h [6]. Typically, the dosage of diazepam for anxiolytic effects in adults is 5–10 mg. In this case, the generally recommended dosage according to the in-office sedation guidelines of the American Dental Association on diazepam was used, and no additional dose was required [7]. Diazepam has a long half-life of 20–80 h due to the activity of metabolites such as desmethyldiazepam and oxazepam [8]. If additional dosage is taken before metabolites are eliminated, complications of oversedation may occur. [8] The interval between visits for this patient was at least 7 days, with an average of 25.5 days to achieve complete excretion of metabolites.
In oral sedation, it is relatively difficult to predict the effect of the drug, as it depends on the conditions of the gastrointestinal tract and hepatic metabolism [6]. Therefore, the effect of the drug on each patient must be determined through a test appointment [3]. In this case, the first visit for treatment was a test appointment. The operator can assess whether the patient is sufficiently relieved through a simple dental procedure. To avoid the risk of oversedation, additional doses are not considered at the level of minimal sedation. If minimal sedation is insufficient, conversion to deep sedation and general anesthesia should be considered.
In this case of multi-visit and long-term dental treatment under minimal sedation, we were concerned about the effect of the patient's systemic disease, the drug interactions of benzodiazepines, and the possibility of drug dependence.
The patient had cardiovascular diseases such as hypertension and hyperlipidemia. As benzodiazepines are effective in reducing pain and anxiety, they may prevent angina in patients with cardiovascular disease [4]. However, in patients with impaired liver function, benzodiazepines should be used at the lowest possible dose, as most benzodiazepines are metabolized by cytochrome P (CYP) 450 enzymes and glucuronide conjugation [6]. Lorazepam, which is metabolized by glucuronyl transferase in peripheral tissues rather than liver microsomal enzymes, is preferentially recommended [6]. In patients with renal disease, high doses increase central nervous system side effects, and lowering the dose is recommended.
Benzodiazepines are known to cause clinically significant drug interactions when combined with inhibitors and inducers of CYP3A4 or 2C19, which are enzymes of CYP 450 [9]. Drugs in this category include carbamazepine, cimetidine, clarithromycin, and erythromycin. Oxazepam and lorazepam, which have different metabolic pathways, can be used in combination with these drugs [10]. Prior to selecting a drug for minimal sedation, the patient's medication must be identified in advance, and a careful evaluation of drug interactions is required. Our patient did not take any drugs which could potentially result in drug interactions.
The third consideration is the possibility of drug dependence caused by diazepam used > 20 times over a long period. The recommended dosage of diazepam for anxiolysis is 2–10 mg, 2–4 times per day in adults under the age of 64, and 2.0–2.5 mg, 1–2 times per day in patients with systemic weakness [11]. For those > 65 years old, it is recommended to avoid the prescription of drugs, but if there is no alternative treatment, the dose should be reduced by 50% [8,11]. The initial dose should not exceed 40 mg. Long-term use is defined as continuous daily administration for > 2 weeks and can cause dependence or withdrawal symptoms [12]. For long-term use, gradual tapering is performed to prevent tolerance, dependence, and withdrawal symptoms [12]. The half-life of diazepam is 20–40 h, and the wash-out period increases to 80–100 h in people > 60 years old or in patients with hepatic disease [8]. In the present case of a 50-year-old patient, the dose was 10 mg, and the interval between visits was at least 7 days with an average of 25.5 days. Thus, an adequate wash-out period was allowed to achieve complete excretion of metabolites of the drug, and the possibility of drug dependence could be ruled out. For follow-up visits, an attempt to treat with a non-pharmacological behavioral control technique needs to be attempted. Therefore, in visits for simple treatments of < 10 minutes, such as suture removal (5th, 7th, 13th, and 15th visits), we explained the patient that she could come to the clinic without taking sedatives. This attempt was also necessary to prevent drug abuse and dependence.
In this case, diazepam was used as a sedative. Midazolam and triazolam are also known to have excellent anxiolytic effects and are used for sedation in dental treatment [3,13]. However, midazolam is produced as a premixed syrup or by diluting the intravenous formulation [3]. It has no advantages in adult patients who can take tablets. Triazolam has been reported to induce significant amnesia for intraoperative events in some patients [13]. As it is a sleep inducer, the patient can fall asleep during treatment that requires patient response and communication. It is necessary to evaluate the adequacy of the drug through a test appointment and select the drug that suits the procedure.
It is difficult to predict an individual's response to oral sedatives. This patient reported a history of taking diazepam when necessary; the previous dose of was confirmed through a medical consultation, and side effects such as oversedation were not observed on administering the recommended dose. For patients with no history of drug use, it is recommended to administer a low dose first during a test appointment. In the event of oversedation, oxygen supply and equipment for maintaining the patient's airways should be available, and the antagonist flumazenil should be administered immediately. Effective suction equipment to remove foreign substances must be secured. According to the guidelines of the American Dental Association, dentists wishing to perform minimal sedation must complete regular or intensive training courses in sedation and general anesthesia and obtain a current certificate of basic life support for health care providers.
Compared to pediatric patients, studies and surveys of adult patients with dental fear are relatively insufficient. Considering that the proportion of adult patients with dental fear and the demand for sedation are gradually increasing, further studies are required. In addition, education on adult sedation for dental practitioners needs to be further expanded.
In conclusion, we can assume that multi-visit dental treatment using minimal sedation with adequate intervals can be effective in adult patients with anxiety and dental phobia based on careful patient selection.
ACKNOWLEDGMENTS
The authors received no funding.
Footnotes
- Seung-Rye Song: Conceptualization, Data curation, Writing — original draft.
- Tae Min You: Project administration, Supervision, Writing — review & editing.
CONFLICTS OF INTEREST: The authors declare no conflict of interest.
CONSENT: Informed consent was obtained from the patient in this case report. According to the policy of our Institutional Review Board, case reports are exempt from IRB approval.
References
- 1.Armfield JM, Heaton LJ. Management of fear and anxiety in the dental clinic: a review. Aust Dent J. 2013;58:390–407. doi: 10.1111/adj.12118. [DOI] [PubMed] [Google Scholar]
- 2.Goodchild JH, Dickinson SC. Anxiolysis in dental practice: a report of three cases. Gen Dent. 2004;52:264–268. [PubMed] [Google Scholar]
- 3.Donaldson M, Gizzarelli G, Chanpong B. Oral sedation: a primer on anxiolysis for the adult patient. Anesth Prog. 2007;54:118–128. doi: 10.2344/0003-3006(2007)54[118:OSAPOA]2.0.CO;2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bae CH, Kim H, Cho KA, Kim MS, Seo KS, Kim HJ. A survey of sedation practices in the Korean dentistry. J Korean Dent Soc Anesthesiol. 2014;14:29–39. [Google Scholar]
- 5.Kleinknecht RA, Klepac RK, Alexander LD. Origins and characteristics of fear of dentistry. J Am Dent Assoc. 1973;86:842–848. doi: 10.14219/jada.archive.1973.0165. [DOI] [PubMed] [Google Scholar]
- 6.Klotz U. Clinical pharmacokinetics of diazepam and its biologically active metabolites (author's transl) Klin Wochenschr. 1978;56:895–904. doi: 10.1007/BF01489215. [DOI] [PubMed] [Google Scholar]
- 7.American Dental Association. The use of conscious sedation, deep sedation and general anesthesia in dentistry. Available from http://www.ada.org/prof/resources/positions/statements/anesthesia_guidelines.pdf.
- 8.Flockhart DA. Drug Interactions: Cytochrome P450 Drug Interaction Table. Indiana University School of Medicine; 2007. [Google Scholar]
- 9.Ruffalo RL, Thompson JF, Segal JL. Diazepam-cimetidine drug interaction: a clinically significant effect. South Med J. 1981;74:1075–1078. doi: 10.1097/00007611-198109000-00016. [DOI] [PubMed] [Google Scholar]
- 10.Cogo K, Bergamaschi CC, Yatsuda R, Volpato MC, Andrade ED. Conscious sedation with benzodiazepines in dentistry. Rev Odontol. 2006;18:181–188. [Google Scholar]
- 11.Ashton H. Guidelines for the rational use of benzodiazepines. When and what to use. Drugs. 1994;48:25–40. doi: 10.2165/00003495-199448010-00004. [DOI] [PubMed] [Google Scholar]
- 12.Olkkola KT, Ahonen J. Midazolam and other benzodiazepines. Handb Exp Pharmacol. 2008;(182):335–360. doi: 10.1007/978-3-540-74806-9_16. [DOI] [PubMed] [Google Scholar]
- 13.Ehrich DG, Lundgren JP, Dionne RA, Nicoll BK, Hutter JW. Comparison of triazolam, diazepam, and placebo as outpatient oral premedication for endodontic patients. J Endod. 1997;23:181–184. doi: 10.1016/S0099-2399(97)80272-5. [DOI] [PubMed] [Google Scholar]