Abstract
During the clinical care of hospitalized patients with COVID-19, diminished QRS amplitude on the surface electrocardiogram (ECG) was observed to precede clinical decompensation, culminating in death. This prompted investigation into the prognostic utility and specificity of low QRS complex amplitude (LoQRS) in COVID-19. We retrospectively analyzed consecutive adults admitted to a telemetry service with SARS-CoV-2 (n = 140) or influenza (n = 281) infection with a final disposition—death or discharge. LoQRS was defined as a composite of QRS amplitude <5 mm or <10 mm in the limb or precordial leads, respectively, or a ≥50% decrease in QRS amplitude on follow-up ECG during hospitalization. LoQRS was more prevalent in patients with COVID-19 than influenza (24.3% vs 11.7%, p = 0.001), and in patients who died than survived with either COVID-19 (48.1% vs 10.2%, p <0.001) or influenza (38.9% vs 9.9%, p <0.001). LoQRS was independently associated with mortality in patients with COVID-19 when adjusted for baseline clinical variables (odds ratio [OR] 11.5, 95% confidence interval [CI] 3.9 to 33.8, p <0.001), presenting and peak troponin, D-dimer, C-reactive protein, albumin, intubation, and vasopressor requirement (OR 13.8, 95% CI 1.3 to 145.5, p = 0.029). The median time to death in COVID-19 from the first ECG with LoQRS was 52 hours (interquartile range 18 to 130). Dynamic QRS amplitude diminution is a strong independent predictor of death over not only the course of COVID-19 infection, but also influenza infection. In conclusion, this finding may serve as a pragmatic prognostication tool reflecting evolving clinical changes during hospitalization, over a potentially actionable time interval for clinical reassessment.
In some patients infected with SARS-CoV-2, localized viral replication progresses to a systemic inflammatory syndrome.1, 2, 3 Myocardial injury has been reported in patients with COVID-19, yet the pathophysiologic mechanism has not been well defined.4, 5, 6 There has likewise been little reported evidence of direct myocardial damage on the 12-lead electrocardiogram (ECG) despite myocardial injury occurring in 33.7% of hospitalized patients.7 Low QRS amplitude (LoQRS) has been associated with both late gadolinium enhancement on magnetic resonance imaging and cardiac events in clinically suspected myocarditis.8 We noted QRS amplitude diminution on the 12-lead ECG to be coincident with worsening clinical status and death while caring for patients with COVID-19, prompting investigation into the significance of QRS amplitude in a consecutive series of admitted patients.9 Here, we expand the investigation to patients hospitalized with influenza to contextualize results and assess the specificity of any findings to COVID-19.
Methods
This single-center retrospective cohort study included consecutive adult patients (≥18 years old) with COVID-19 admitted to Mount Sinai Hospital (New York, NY) between March 7 and April 12, 2020 as part of a COVID-19 registry (NCT04358029). All patients had laboratory-confirmed COVID-19 based on a reverse transcriptase-polymerase chain reaction assay of nasal or pharyngeal swab specimens. Of 1,354 patients with COVID-19 screened using electronic medical records from March 7, 2020 to April 12, 2020, 800 patients were hospitalized. After exclusion of patients without telemetry data, retrievable ECGs, or a final disposition (death or discharge), 140 patients were analyzed. The comparison group included a cohort of 1,420 patients with laboratory-confirmed Influenza A or Influenza B admitted to Mount Sinai Hospital between January 2, 2017 and January 5, 2020. A total of 281 consecutive influenza patients with retrievable ECGs from the electronic medical record from September 2017 through February 2020 were analyzed to allow for a 2:1 comparison to COVID-19 patients.
We manually extracted demographics, laboratory findings, ECG data, treatments received, and clinical outcomes from admission through hospitalization from electronic medical records. For patients with COVID-19, laboratory assessment consisted of complete blood count, assessment of liver and renal function including serum electrolytes, coagulation profile, troponin-I, d-dimer, C-reactive protein, lactate dehydrogenase, fibrinogen, interleukin-6, brain natriuretic peptide, and procalcitonin. Data for patients with influenza were obtained through automated extraction from the electronic medical record and included demographic, laboratory testing, ECG data, treatments received, and clinical outcomes. Telemetry and ECG data were obtained with the GE CARESCAPE B850 V2.0.8.213 telemetry system. ECGs at baseline and before admission were obtained with the GE Mac 5500 ECG system. Acquisition by either system utilized electrodes placed in the standard 12-lead ECG configuration. Follow-up ECG acquisition was routine in patients on the telemetry service.
QRS complex amplitudes were measured individually to the nearest 0.5 mm and recorded as the sum of 2 peak-to-peak QRS complexes (peak of the R wave to the nadir of the Q or S wave, whichever was larger) in the limb leads (leads I, II, III, aVR, aVL, aVF) and for leads V1-V3 and V4-V6 which are reported respectively in aggregate such that the sum of the limb lead voltage is comprised of 12 QRS complexes and V1-V3 and V4-V6 each are comprised of 6 QRS complexes. If artifact precluded interpretation, 2 QRS complexes least impacted by the artifact in a given lead (e.g., V2) were reported. The sum of precordial QRS complex amplitude was obtained by adding the sum obtained for V1-V3 to that of leads V4-V6. To capture relative changes in QRS amplitude, the sum of the QRS amplitudes on the last available ECG were subtracted from the sum in the respective leads on the presenting (admission) ECG and the baseline ECG (ECG obtained within the past year). QRS amplitudes were considered to have met threshold cutoffs if all the QRS complexes in a given group were below the respective cutoff. Therefore, if the cutoff is <5 mm, then all leads to which that threshold applies must each individually demonstrate QRS amplitudes <5 mm.
LoQRS was defined by a composite of either: (1) QRS amplitude <5 mm in the limb leads odds ratio [OR] <10 mm in the precordial leads (a composite of V1-V3 and V4-V6), V1-V3 independently, or V4-V6 independently; (2) QRS amplitude decrease by ≥50% compared with the baseline or admission ECG in the limb leads or precordial leads; or (3) meeting the aforementioned criteria with a “limited interpretability” QRS morphology due to changes in rhythm origin or new bundle branch block. Stable QRS amplitude was defined by a failure to meet criteria for LoQRS. If a patient met the disposition outcome of death and met LoQRS criteria on the last available ECG, all ECGs were reviewed from the last available ECG until the first ECG with LoQRS identified. We recorded the interval from the day of presentation to the first ECG showing LoQRS, and calculated the time to death from the time stamp on the first ECG showing LoQRS until the clinically documented time of death. We likewise calculated the time interval from the last available ECG to the time of final disposition. Before data collection, the study was approved by the Institutional Review Board. The primary outcome was death. Secondary outcomes included the composite criteria of LoQRS and individual components of the composite.
Continuous variables are reported as the median and interquartile range (IQR), and were compared using the Wilcoxon rank-sum test. Categorical variables are reported as percentages and were compared using the chi-square test. Multivariable logistic regression models were performed to evaluate the association between LoQRS and in-hospital mortality for patients hospitalized with Covid-19 or Influenza. Model 1 accounted for baseline demographic and clinical characteristics that differed significantly between the COVID-19 and influenza groups and included the following covariates: age, body mass index, current/former smoking, and history of chronic kidney disease, liver disease, and hypertension. Model 2 included the same covariates as Model 1, with the addition of LoQRS. Using the same covariates as in Model 2, we performed formal interaction testing to determine how the type of viral infection, COVID-19 versus influenza, influenced the association of LoQRS with in-hospital mortality. Model 3, performed only in the COVID-19 group, additionally controlled for significant laboratory differences in admission troponin, peak troponin, peak D-dimer, C-reactive protein, and last available albumin levels. Lastly, Model 4 additionally controlled for patients who required intubation or inotropic or vasopressor medications.
We assessed discrimination of the predictive models by receiver operating characteristic analysis for each model. Improvement in model discrimination was assessed by calculating the integrated discrimination improvement index (IDI) of adding LoQRS to the baseline clinical variables adjusted for in Model 1. All analyses were performed with the use of Stata software version 14.2. A 2-sided p value <0.05 was deemed statistically significant.
Results
The study population included 140 patients hospitalized with COVID-19 and 281 patients hospitalized with influenza A or B. Clinical characteristics at baseline among COVID-19 patients are shown in Table 1 . Additional characteristics specific to COVID-19 patients are listed in the Appendix (Tables S1 through S7). Compared with patients with influenza, the patients with COVID-19 were younger and had a higher prevalence of diabetes, hypertension, sleep apnea, and female sex (Table 2 ). Patients admitted with COVID-19 had higher levels of C-reactive protein and lower levels of brain natriuretic peptide.
Table 1.
Patient demographics, clinical, and laboratory characteristics in patients with COVID-19
| Variable | Full cohort | Death | Discharge | p value |
| (n = 140) | (n = 52) | (n = 88) | ||
| Median age in years (IQR) | 61 (48.5-74) | 71 (59-78) | 58 (45-71) | <0.01 |
| Women | 38/140 (27%) | 14/52 (27%) | 24/88 (27%) | 0.96 |
| Race | 0.69 | |||
| White | 47/140 (34%) | 20/52 (39%) | 27/88 (31%) | |
| Black | 21/140 (15%) | 8/52 (15%) | 13/88 (15%) | |
| Hispanic | 32/140 (23%) | 12/52 (23%) | 20/88 (23%) | |
| Asian | 0/140 (0%) | 0/52 (0%) | 0/88 (0%) | |
| Other/unknown | 40/140 (29%) | 12/52 (23%) | 28/88 (32%) | |
| Weight (kg) | 84 (69-95) | 85 (73-96) | 82 (67-94) | 0.45 |
| Body mass index in kg/m2 (IQR) | 28 (25-33) | 30 (27-35) | 28 (25-32) | 0.08 |
| Comorbidities of interest | ||||
| Diabetes mellitus | 54/140 (39%) | 21/52 (40%) | 33/88 (38%) | 0.74 |
| Heart failure | 22/140 (16%) | 11/52 (21%) | 11/88 (13%) | 0.17 |
| Hypertension | 86/140 (61%) | 35/52 (67%) | 51/88 (58) | 0.27 |
| Asthma | 18/140 (13%) | 8/52 (15%) | 10/88 (11%) | 0.49 |
| Chronic kidney disease | 20/140 (14%) | 12/52 (23%) | 8/88 (9%) | 0.02 |
| Liver disease | 5/140 (4%) | 4/52 (8%) | 1/88 (1%) | 0.04 |
| HIV | 8/140 (6%) | 2/52 (4%) | 6/88 (7%) | 0.46 |
| Obesity | 52/140 (37%) | 25/52 (48%) | 27/88 (31%) | 0.04 |
| Smoker | 32/124 (26%) | 16/42 (38%) | 16/82 (20%) | 0.03 |
| Alcohol abuse | 8/140 (6%) | 4/52 (8%) | 4/88 (5%) | 0.44 |
| Sleep apnea | 18/140 (13%) | 9/52 (17%) | 9/88 (10%) | 0.23 |
| Coronary artery disease | 35/140 (25%) | 13/52 (25%) | 22/88 (25%) | 0.99 |
| Prior revascularization | 27/140 (19%) | 10/52 (19%) | 17/88 (19%) | 0.99 |
| PTCA/PCI | 21/27 (78%) | 8/10 (80%) | 13/17 (77%) | 0.83 |
| CABG | 4/27 (15%) | 1/10 (10%) | 3/17 (18%) | 0.59 |
| Atrial fibrillation or flutter | 19/140 (14%) | 8/52 (15%) | 11/88 (13%) | 0.37 |
| Prior ventricular arrhythmias | 3/140 (2%) | 1/52 (2%) | 1/88 (1%) | 0.69 |
| Ischemic stroke | 6/140 (4%) | 2/52 (4%) | 4/88 (5%) | 0.84 |
| Laboratory characteristics (IQR) | ||||
| White blood cell count (×103/uL) | 6.7 (4.9-10.2) | 8.1 (5.1-10.2) | 6.3 (4.9-9.8) | 0.4 |
| Neutrophil count (×103/uL) | 5.0 (3.4-8.0) | 6.2 (3.4-8.0) | 4.6 (3.4-8.1) | 0.43 |
| Lymphocyte count (×103/uL) | 0.9 (0.6-1.2) | 0.9 (0.5-1.3) | 0.9 (0.6-1.2) | 0.45 |
| Hemoglobin (g/dl) | 13.1 (11.0-14.0) | 12.1 (9.6-14.0) | 13.5 (12.3-14.7) | <0.01 |
| Platelets (×103/dl) | 199 (161-256) | 187 (132-245) | 219 (170-257) | 0.03 |
| Creatinine (mg/dl) | 1.1 (0.8-1.5) | 1.5 (1.0-2.7) | 1.0 (0.8-1.3) | <0.01 |
| Aspartate aminotransferase (AST) (U/L) | 38 (27-56) | 46 (27-69) | 36 (27-50) | 0.06 |
| Alanine transaminase (ALT) (U/L) | 28 (17-46) | 30 (17-48) | 28 (17-44) | 0.68 |
| Albumin (g/dl) | 3.3 (2.9-3.6) | 3.1 (2.7-3.5) | 3.3 (3.0-3.6) | 0.02 |
| D-Dimer (ug/ml) | 1.4 (0.6-3.1) | 2.3 (0.9-4.1) | 1.1 (0.5-2.3) | 0.01 |
| International normalized ratio (INR) | 1.1 (1.0-1.3) | 1.2 (1.1-1.4) | 1.1 (1.0-1.2) | <0.01 |
| Troponin-I (ng/ml) | 0.02 (0.01-0.07) | 0.03 (0.01-0.20) | 0.01 (0.01-0.04) | <0.01 |
| Lactate dehydrogenase (LDH) (U/L) | 400 (296-544) | 481 (331-835) | 369 (292-494) | <0.01 |
| Brain natriuretic peptide (pg/ml) | 48 (10-205) | 71 (15-579) | 34 (10-167) | 0.12 |
| Erythrocyte sedimentation rate (mm/h) | 59 (24-85) | 67 (33-101) | 51 (18-77) | 0.25 |
| C-reactive protein (mg/L) | 105 (46-185) | 146 (62-219) | 87 (31-143) | <0.01 |
| Fibrinogen (mg/dl) | 556 (438-685) | 558 (420-685) | 554 (453-667) | 0.82 |
| Interleukin-6 (pg/ml) | 111 (42-234) | 160 (85-327) | 55 (26-148) | <0.01 |
| Lactate (mmol/L) | 1.5 (1.1-2.0) | 1.5 (1.0-2.1) | 1.6 (1.2-2.0) | 0.37 |
| Procalcitonin (ng/ml) | 0.17 (0.08-0.61) | 0.51 (0.13-1.39) | 0.12 (0.06-0.30) | <0.01 |
| Baseline medications | ||||
| ACE inhibitor | 28/140 (20%) | 9/52 (17%) | 19/88 (22%) | 0.54 |
| Angiotensin receptor blocker | 21/140 (15%) | 8/52 (15%) | 13/88 (15%) | 0.92 |
| Aspirin | 41/140 (29%) | 14/52 (27%) | 27/88 (31%) | 0.64 |
| Anticoagulant | 21/140 (15%) | 10/52 (19%) | 11/88 (13%) | 0.28 |
| Warfarin | 7/21 (33%) | 2/10 (20%) | 5/11 (46%) | 0.22 |
| DOAC | 14/21 (67%) | 8/10 (80%) | 6/11 (55%) | 0.22 |
| Antiarrhythmic | 6/140 (4%) | 4/52 (8%) | 2/88 (2%) | 0.13 |
Table 2.
Patient demographics, clinical, and laboratory characteristics in patients with COVID-19 or influenza
| Characteristic | COVID-19 (n = 140) | Influenza (n = 281) | p value |
|---|---|---|---|
| Median age in years (IQR) | 61 (49-74) | 69 (57-80) | <0.01 |
| Women | 38 (27%) | 157 (56%) | <0.01 |
| Race | <0.01 | ||
| White | 47 (34%) | 77 (28%) | |
| Black | 21 (15%) | 79 (28%) | |
| Hispanic | 32(23%) | 89 (32%) | |
| Asian | 0 (0%) | 8 (3%) | |
| Other/unknown | 40 (29%) | 27 (10%) | |
| Median body mass index in kg/m2 (IQR) | 28 (25-33) | 27 (23-32) | 0.01 |
| Comorbidities of interest | |||
| Diabetes mellitus | 54 (39%) | 64 (23%) | 0.01 |
| Heart failure | 22 (16%) | 61 (22%) | 0.15 |
| Hypertension | 86 (61%) | 121 (43%) | <0.01 |
| Asthma | 18 (13%) | 45 (16%) | 0.39 |
| Chronic kidney disease | 20 (14%) | 59 (18%) | 0.36 |
| Liver disease | 5 (4%) | 11 (4%) | 0.86 |
| HIV | 8 (6%) | 15 (5%) | 0.87 |
| Obesity | 52 (37%) | 97 (35%) | 0.60 |
| Smoker | 32 (26%) | 129 (46%) | <0.01 |
| Sleep apnea | 18 (13%) | 14 (5%) | <0.01 |
| Ischemic stroke | 6 (4%) | 13 (5%) | 0.87 |
| Baseline laboratory characteristics | |||
| White blood cell count (×103/uL) | 6.7 (4.9-10.2) | 7.9 (5.9-10.7) | 0.03 |
| Neutrophil count (×103/uL) | 5.0 (3.4-8.0) | 6.0 (4.2-8.6) | 0.04 |
| Lymphocyte count (×103/uL) | 0.9 (0.6-1.2) | 0.9 (0.6-1.1) | 0.45 |
| Hemoglobin (g/dl) | 13.1 (11.0-14.4) | 12.3 (10.8-14.0) | 0.05 |
| Platelets (×103/dl) | 199 (161-256) | 195 (147-246) | 0.34 |
| Creatinine (mg/dl) | 1.1 (0.8-1.5) | 1.0 (0.8-1.5) | 0.14 |
| Aspartate aminotransferase (AST) (U/L) | 38 (27-56) | 34 (22-53) | 0.09 |
| Alanine transaminase (ALT) (U/L) | 28 (17-46) | 22 (15-38) | 0.03 |
| Albumin (g/dl) | 3.3 (2.9-3.6) | 3.5 (2.9-3.8) | 0.02 |
| D-Dimer (ug/ml) | 1.4 (0.6-3.1) | 0.9 (0.5-4.0) | 0.91 |
| International normalized ratio (INR) | 1.1 (1.0-1.3) | N/A | N/A |
| Troponin-I (ng/ml) | 0.02 (0.01-0.07) | 0.03 (0.01-0.06) | 0.32 |
| Lactate dehydrogenase (LDH) (U/L) | 400 (296-544) | 353 (260-530) | 0.30 |
| Brain natriuretic peptide (pg/ml) | 48 (10-205) | 188 (51-812) | <0.01 |
| Erythrocyte sedimentation rate (mm/h) | 59 (24-85) | 42 (28-70) | 0.54 |
| C-reactive protein (mg/L) | 105 (46-185) | 49 (11-106) | 0.04 |
| Fibrinogen (mg/dl) | 556 (438-685) | N/A | N/A |
| Interleukin-6 (pg/ml) | 111 (42-234) | N/A | N/A |
| Lactate (mmol/L) | 1.5 (1.1-2.0) | N/A | N/A |
| Procalcitonin (ng/ml) | 0.2 (0.1-0.6) | 0.6 (0.1-3.7) | <0.01 |
| Baseline medications no. (%) | |||
| ACE inhibitor | 28 (20%) | 47 (17%) | 0.43 |
| Angiotensin receptor blocker | 21 (15%) | 41 (15%) | 0.92 |
| Aspirin | 41 (29%) | 89 (32%) | 0.60 |
N/A = not available.
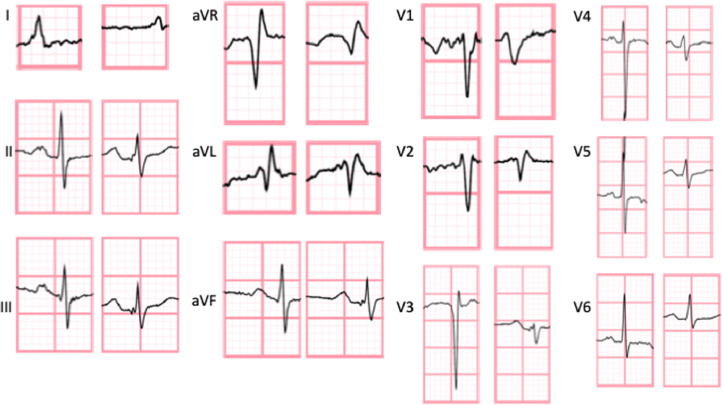
QRS amplitudes in the limb leads, composite precordial leads, leads V1-V3, and leads V4-V6 were all significantly lower on the last available ECG in patients who died compared with those surviving to hospital discharge (Table 3 ). There were no significant differences in QRS amplitude measurements between the baseline and admission ECGs. A representative ECG demonstrating LoQRS is shown in Figure 1 .
Table 3.
Quantitative QRS amplitude characteristics by patient disposition in COVID-19 patients
| Median voltage in mm (IQR) | Full cohort (n = 140) | Death (n = 52) | Discharge (n = 88) | p value |
|---|---|---|---|---|
| Baseline QRS amplitude | ||||
| Sum of all leads | 258 (208-292) | 240 (209-294) | 259 (202-291) | 0.95 |
| Sum of limb leads | 98 (80-129) | 104 (73-135) | 96 (81-115) | 0.27 |
| Sum of precordial leads | 149 (115-179) | 133 (112-175) | 164 (119-180) | 0.36 |
| Sum of V1-V3 | 75 (52-88) | 72 (52-89) | 76 (53-87) | 0.52 |
| Sum of V4-V6 | 73 (50-97) | 70 (50-96) | 74 (50-98) | 0.72 |
| Admission QRS amplitude | ||||
| Sum of all leads | 242 (205-303) | 249 (208-294) | 241 (203-307) | 0.61 |
| Sum of limb leads | 100 (80-128) | 99 (75-126) | 100 (82-131) | 0.48 |
| Sum of precordial leads | 141 (116-177) | 138 (110-176) | 143 (117-181) | 0.49 |
| Sum of V1-V3 | 73 (57-89) | 70 (57-86) | 74 (58-89) | 0.42 |
| Sum of V4-V6 | 69 (53-93) | 69 (45-94) | 69 (56-93) | 0.44 |
| Last available QRS amplitude | ||||
| Sum of all leads | 224 (174-287) | 200 (151-274) | 231 (192-297) | <0.01 |
| Sum of limb leads | 95 (70-124) | 86 (63-124) | 98 (81-129) | 0.02 |
| Sum of precordial leads | 129 (94-166) | 107 (78-157) | 140 (106-176) | <0.01 |
| Sum of V1-V3 | 67 (48-90) | 58 (40-79) | 73 (54-96) | <0.01 |
| Sum of V4-V6 | 58 (42-85) | 52 (34-82) | 62 (46-86) | 0.03 |
QRS complex amplitudes reflect the sum of 2 peak-to-peak QRS complexes per lead presented in aggregate.
Figure 1.
Precordial electrocardiographic QRS diminution. QRS amplitudes are demonstrated meeting criteria for precordial LoQRS. From left to right in each column, an ECG QRS complex on admission is compared with an ECG QRS complex on the last available ECG.
The composite endpoint of LoQRS occurred in 24.3% of COVID-19 patients (Table 4 ). LoQRS occurred more frequently in patients who died compared with those who survived to hospital discharge (48.1% vs 10.2%, p <0.001). A ≥50% decrease in QRS amplitude occurred in 17.1% of patients (36.5% in the mortality group vs 5.7% in the discharged group, p <0.001). QRS amplitude met a threshold <5 mm in the limb leads or <10 mm in the precordial leads in 15.7% of patients and was more prevalent in those who died (28.9% vs 8.0%, p = 0.001). Estimates of survival by LoQRS are demonstrated in the Appendix (Figure S1).
Table 4.
Categorical electrocardiographic QRS amplitude changes in COVID-19 by patient disposition
| Voltage characteristic no. (%) | Death (n = 52) | Discharge (n = 88) | p value |
|---|---|---|---|
| Composite low QRS amplitude (LoQRS)* | 25 (48.1) | 9 (10.2) | <0.01 |
| QRS amplitude <5 mm in limb leads AND <10 mm in precordial leads | 0 (0.0) | 0 (0.0) | 0.99 |
| ≥50% decrease in QRS amplitude | 19 (36.5) | 5 (5.7) | <0.01 |
| QRS amplitude <5 mm limb OR <10 mm precordial in precordial leads | 15 (28.9) | 7 (8.0) | 0.001 |
| LoQRS in limb leads | 7 (13.5) | 3 (3.4) | 0.026 |
| LoQRS in precordial leads | 18 (34.6) | 6 (6.8) | <0.01 |
| LoQRS in leads V1-V3 | 10 (19.2) | 5 (5.7) | 0.01 |
| LoQRS in leads V4-V6 | 14 (26.9) | 4 (4.6) | <0.01 |
| LoQRS with LIQRS morphology† | 5 (9.6) | 2 (2.3) | 0.05 |
| Any QRS amplitude increase (baseline to admission ECG) | 8 (15.4) | 8 (9.1) | 0.26 |
| Any QRS amplitude increase (baseline to last ECG) | 4 (7.7) | 11 (12.5) | 0.37 |
| Any QRS amplitude increase (admission to last ECG) | 4 (7.7) | 12 (13.6) | 0.29 |
Low QRS amplitude (LoQRS) is a composite of relative QRS amplitude reduction by ≥50% from baseline or admission ECG or meeting a threshold of QRS amplitude <5 mm in the limb leads or <10 mm in the precordial leads or in V1-V3 or V4-V6.
Limited interpretablity QRS morphology due to change from sinus rhythm, new bundle branch block, or pacing.
Mortality occurred in 37.1% of the COVID-19 cohort, but was 73.5% in patients with LoQRS compared with 25.5% of patients without LoQRS (p <0.001). There was no significant difference in the median length of stay between groups (7 days, IQR 4 to 10, p = 0.89). More patients with LoQRS required both intubation (61.8% vs 30.2%, p = 0.001) and administration of inotropic or vasopressor medications (58.8% vs 25.5%, p <0.001). Among patients who died, the median time to the first ECG with LoQRS was 5.3 days (IQR 2.1 to 11.1), and the median time to death from the first ECG with LoQRS was 52 hours (IQR 18 to 130). No significant difference in timing from the last available ECG to disposition between LoQRS and stable QRS amplitude groups was noted (Supplement, Table S15).
When adjusted for baseline clinical variables, LoQRS was independently associated with mortality (OR 11.5, 95% confidence interval [CI] 3.9 to 33.8, p <0.001) and improved discrimination of the logistic regression model (Table 5 ). The area under the receiver operating characteristic curve increased from 0.79 to 0.87 when LoQRS was added to the multivariable model and the IDI was 0.15, with a p value of <0.001, indicating that the mean difference of predicted risk between patients who died or survived increased by 15%.
Table 5.
Multivariable sensitivity analysis in COVID-19
| Significant covariates | Odds ratio (95% CI) | p value | AUC |
|---|---|---|---|
| Model 1: Baseline characteristics without LoQRS | 0.79 | ||
| Age | 1.07 (1.04-1.11) | <0.01 | |
| BMI | 1.10 (1.03-1.18) | <0.01 | |
| Liver disease | 12.01 (1.09-132.76) | 0.04 | |
| Model 2: Baseline characteristics and LoQRS | 0.87 | ||
| LoQRS | 11.51 (3.92-33.81) | <0.01 | |
| Age | 1.08 (1.04-1.12) | <0.01 | |
| BMI | 1.13 (1.05-1.22) | 0.01 | |
| Model 3: Baseline characteristics, labs, and LoQRS | 0.91 | ||
| LoQRS | 6.01 (1.31-27.63) | 0.02 | |
| Age | 1.07 (1.01-1.13) | 0.03 | |
| BMI | 1.16 (1.05-1.29) | <0.01 | |
| Peak D-dimer | 1.14 (1.02-1.28) | 0.02 | |
| Last available albumin | 0.12 (0.02-0.62) | 0.01 | |
| Model 4: Baseline characteristics, labs, LoQRS, and need for inotropes, vasopressors, or mechanical ventilation | 0.98 | ||
| LoQRS | 13.78 (1.31-145.46) | 0.03 | |
| Age | 1.08 (1.00-1.16) | 0.04 | |
| Mechanical ventilation | 90.32 (2.82-2893.11) | 0.01 |
Model 1 included the following covariates: Age, BMI, CKD, smoker (current or former), liver disease, HTN. Model 2 included the covariates in Model 1, in addition to low QRS amplitude (LoQRS). Model 3 included the covariates of Model 2, presenting and peak troponin, peak d-dimer, presenting C-reactive protein, and last available albumin. Model 4 included all covariates in Model 3, need for mechanical ventilation, and need for inotropes or vasopressors. AUC = area under the receiver operating characteristic curve.
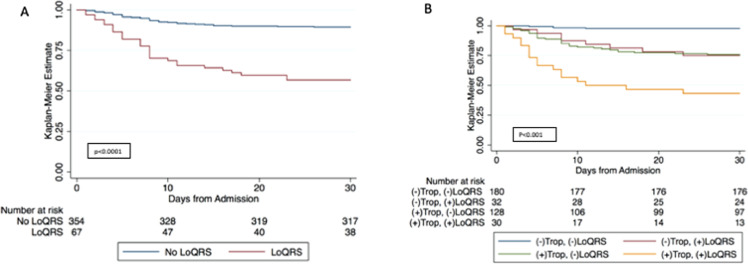
The strong association between LoQRS and mortality (Figure 2 ) persisted after adjustment for presenting troponin, peak troponin, peak d-dimer, C-reactive protein, and last available albumin in addition to baseline clinical covariates [OR 6.0 (95% CI 1.3 to 27.6), p = 0.021] with an area under the receiver operating characteristic curve of 0.91 and when intubation and inotrope or vasopressor requirement were added to the model (OR 13.78 (1.31 to 145.46), p = 0.029). No interaction between myocardial injury (troponin level >0.03 ng/ml) and LoQRS was demonstrated by multivariable analysis (p interaction 0.179). When mortality was stratified by LoQRS and presence of myocardial injury, there was a significant trend towards increased mortality not only in those who exhibited LoQRS without myocardial injury but even more so in patients with both LoQRS and concomitant myocardial injury (Figure 2).
Figure 2.
In-hospital survival in COVID-19 and influenza. (A) In-hospital survival by presence of LoQRS. In this Kaplan-Meier analysis, patients discharged from the hospital were considered to have survived (not censored). (B) In-hospital survival by presence of LoQRS and troponin positivity. Trop = troponin level. A positive troponin level (+) is demarcated by a troponin-I level by the Abbot architect methodology exceeding 0.03 ng/ml.
Compared with Covid-19, LoQRS occurred less frequently in the influenza cohort (11.0% vs 24.3%, p = 0.001). Among influenza patients, LoQRS was more prevalent in those who died than in those who survived to discharge (38.9% vs 9.1%, p <0.001; Supplement, Table S13). QRS amplitude met a threshold of <5 mm in limb leads AND <10 mm in the precordial leads in 5.2% of patients, which was significantly more common in patients who died (22.2% vs 4.0%, p = 0.001). QRS amplitudes that decreased by at least 50% from baseline or admission ECG occurred in 5.3% of the influenza cohort and were also more frequent in patients who died (27.8% vs 3.8%, p <0.001). Similarly, QRS amplitudes that met a threshold of <5 mm in the limb leads OR <10 mm in the precordial leads were noted in 7.8% of the influenza group and were significantly more prevalent in patients who died (27.8% vs 6.5%, p = 0.001).
Mortality was lower in patients with influenza than in those with COVID-19 (6.4% vs 37.1%, p <0.01) and the length of hospital stay was shorter with influenza (5 days vs 7 days, p = 0.002). However, length of stay among those who died was shorter in COVID-19 patients (7 days [IQR 4 to 11]) than in those who succumbed to influenza (9.5 days [IQR 7 to 26], p = 0.01). For influenza patients with LoQRS who died, the median time to death from the first ECG meeting LoQRS criteria was 144 hours (IQR 48 to 144). The median time from admission to the first ECG that met LoQRS criteria was 55 days (IQR 11 to 65). LoQRS was also an independent predictor of mortality in influenza when adjusted for baseline clinical variables (OR 10.71, 95% CI 3.01 to 38.16, p <0.001; Table 6 ). The IDI was 0.09 (p = 0.03). A significant interaction between LoQRS and type of viral infection (i.e., SARS-CoV-2 or Influenza) on mortality was noted (p = 0.038).
Table 6.
Multivariable sensitivity analysis in influenza
| Significant covariates | OR (95% CI) | p value | AUC |
|---|---|---|---|
| Model 1: Baseline characteristics without LoQRS | 0.78 | ||
| Hypertension | 0.13 (0.03-0.63) | 0.01 | |
| Model 2: Baseline characteristics with LoQRS | 0.85 | ||
| LoQRS | 10.71 (3.01-38.16) | <0.01 | |
| BMI | 0.89 (0.81-0.98) | 0.02 | |
| Hypertension | 0.10 (0.02-0.53) | <0.01 | |
Model 1 included the following covariates: Age, BMI, CKD, smoker (current or former), liver disease, HTN. Model 2 included the covariates in Model 1, in addition to low QRS amplitude (LoQRS).
Discussion
This study demonstrates that LoQRS is an independent predictor of mortality in hospitalized patients with either COVID-19 or influenza. QRS amplitude diminution is dynamic during the course of illness and underscores the utility of both a relative reduction in QRS amplitude of at least 50% or meeting a threshold in QRS amplitude.
Low QRS complex amplitude on the ECG has been described in conditions that decrease net myocardial action potential generation or attenuate recorded surface voltage.10, 11, 12, 13, 14, 15, 16, 17, 18 In a variety of disease processes, low ECG voltage portends adverse outcomes.12 , 13 , 19 , 20 A recent multicenter analysis noted low QRS voltage in only 5% of COVID-19 patients, highlighting the potential importance of dynamic QRS amplitude diminution during the course of illness. A median time of 52 hours from the first ECG with LoQRS until death in COVID-19 may provide an opportunity to focus clinical reassessment such as escalating the level of care or medical therapy when LoQRS is identified.
The absence of imaging and autopsy data limits definitive conclusions regarding the mechanism of LoQRS. Recovered COVID-19 patients who underwent cardiac MRI exhibited myocardial edema in 54% to 60% of cases with 31% demonstrating late gadolinium enhancement.21 , 22 This parallels findings in patients with myocarditis and ECG abnormalities.8 LoQRS tracks with the incidence of influenza-associated myocarditis, which has been reported in over 10% of patients and was prevalent in 11% of patients in our influenza cohort.23 We found that inflammatory markers in the COVID-19 cohort were higher in those with LoQRS, suggesting inflammation-mediated myocardial edema as a plausible mechanism. Myocardial injury alone does not explain LoQRS as initial and peak troponin levels were not significant in the multivariable model, while patients with the highest mortality exhibited coincident myocardial injury and LoQRS (Figure 2).
Alternative mechanisms such as lung parenchymal disease can explain LoQRS by extracardiac voltage attenuation. Low voltage in leads V4-V6 has been attributed to the relative contribution of underlying lung parenchymal volume to those unipolar leads.24 This contrasts with our observation that all leads demonstrated significant decreases in QRS amplitude, suggesting a more diffuse process. Given that LoQRS remained independently predictive of mortality adjusted for intubation requirement, which would be expected to track with lung disease severity, this singular etiology is less likely but could plausibly contribute to the findings.
Echocardiographic data were not available to eliminate pericardial effusion as a contributing factor, but imaging studies have found pericardial effusion to be infrequent in patients with COVID-19.25 , 26 Barotrauma and pleural effusions have likewise been reported in only 15% and 5% of cases, respectively, and similarly cannot account for the observed prevalence of LoQRS in this study.27 , 28 Prone positioning was not standard practice in the absence of mechanical ventilation during the study period, which might entail posterior ECG lead placement. Mechanical ventilation does not appear to cause significant changes in QRS amplitude and LoQRS remained independently predictive even when adjusted for intubation.29 Telemetry electrodes were placed in a standard 12-lead configuration from which ECGs during admission were obtained, thus improving reliability between acquisitions. As LoQRS was predictive of mortality after adjusting for serum albumin levels and weight, it is unlikely that volume accumulation or body habitus explain the findings.
Treatment differences do not explain the association between LoQRS and mortality (Supplement, Table S7). More patients in the mortality group received glucocorticoids, which were reserved for the most critically ill patients during the study period and have subsequently demonstrated a mortality benefit in a randomized trial.30 LoQRS may ultimately reflect a spectrum of accumulated insults resulting in a cardiotoxic milieu, including edema, hypoxia, and metabolic disarray.
This study is limited by its retrospective design and lack of corroborating imaging or autopsy data. Inclusion of hospitalized patients on a telemetry service may compromise generalizability to other populations or raise potential for selection bias, possibly overestimating the magnitude of association between LoQRS and mortality. Alternatively, the data were manually extracted at a patient level—buttressing data quality. Lastly, this study did not include outpatient follow-up in survivors with LoQRS to assess long-term outcomes or QRS amplitude recovery.
LoQRS is a dynamic finding associated with mortality in patients with both COVID-19 and influenza infections, underscoring the importance of both a reduction in QRS amplitude below an absolute threshold and the prognostic utility of a relative reduction in QRS amplitude over time. Further studies should address the optimum intervals at which QRS amplitude should be assessed and whether intensification of therapy in individuals manifesting LoQRS would improve clinical outcomes.
Authors’ Contributions
Joshua Lampert: Data curation, conceptualization, data curation, methodology, writing, review, and editing. Michael Miller: Formal Analysis, methodology, writing. Jonathan L. Halperin: Methodology, writing conceptualization, supervision. Connor Oates: data acquisition. Gennaro Giustino: methodology, formal analysis. Kyle Nelson: data acquisition. Jason Feinman: data acquisition. Nikola Kocovic: data acquisition. Matthew Pulaski: data acquisition. Daniel Musikantow: review and editing, writing. Mohit K. Turagam: review and editing, writing, formal analysis. Aamir Sofi: review and editing, writing. Subbarao Choudry: review and editing, writing. Marie-Noelle Langan: review and editing, writing. Jacob S. Koruth: review and editing, writing. William Whang: review and editing, writing. Marc A. Miller: conceptualization, review and editing, writing. Srinivas R. Dukkipati: review and editing, writing, conceptualization. Adel Bassily-Marcus: data acquisition. Roopa Kohli-Seth: data acquisition. Martin E. Goldman: conceptualization, review and editing, supervision. Vivek Y. Reddy: conceptualization, review and editing, methodology, writing, supervision.
Disclosures
Gennaro Giustino reports a relation with Pfizer that includes: board membership. Srinivas Dukkipati reports a relation with Biosense Webster Inc that includes: board membership, equity or stocks, and funding grants. Srinivas Dukkipati also reports a relation with Farapulse Inc that includes: equity or stocks. Vivek Reddy reports a relation with Farapulse Inc that includes: equity or stocks. Vivek Reddy has also disclosures with other companies not related to this manuscript: Abbott (Consultant), Ablacon (Consultant, Equity), Acutus Medical (Consultant, Equity), Affera (Consultant, Equity), Apama Medical (Consultant, Equity), APN Health (Consultant, Equity), Aquaheart (Consultant, Equity), Atacor (Consultant, Equity), Autonomix (Consultant, Equity), Axon Therapeutics (Consultant, Equity), Backbeat (Consultant, Equity), BioSig (Consultant, Equity), Biosense-Webster (Consultant), BioTel Heart (Consultant), Biotronik (Consultant), Boston Scientific (Consultant), Cardiac Implants (Consultant, Equity), CardiaCare (Consultant, Equity), Cardiofocus (Consultant), Cardionomic (Consultant), CardioNXT/AFTx (Consultant, Equity), Circa Scientific (Consultant, Equity), Corvia Medical (Consultant, Equity), Dinova-Hangzhou Nuomao Medtech Co, Ltd (Consultant, Equity), East End Medical (Consultant, Equity), EBR (Consultant), EPD (Consultant, Equity), Epix Therapeutics (Consultant, Equity), EpiEP (Consultant, Equity), Eximo (Consultant, Equity), Farapulse (Consultant, Equity), Fire1 (Consultant), Gore & Associates (Consultant), HRT (Consultant, Equity), Impulse Dynamics (Consultant), Intershunt (Consultant, Equity), Javelin (Consultant, Equity), Kardium (Consultant, Equity), Keystone Heart (Consultant, Equity), LuxMed (Consultant, Equity), Manual Surgical Sciences (Equity), Medlumics (Consultant, Equity), Medtronic (Consultant), Middlepeak (Consultant, Equity), Newpace (Equity), Nuvera (Consultant, Equity), Philips (Consultant), Pulse Biosciences (Consultant), Sirona Medical (Consultant, Equity), Surecor (Equity), Thermedical (Consultant), Valcare (Consultant, Equity) and Vizaramed (Equity). Joshua Lampert, Michael Miller, Jonathan Halperin, Connor Oates, Kyle Nelson, Jason Feinman, Nikola Kocovic, Matthew Pulaski, Daniel Musikantow, Mohit Turagam, Aamir Sofi, Subbarao Choudry, Marie-Noelle Langan, Jacob Koruth, William Whang, Marc Miller, Adel Bassily-Marcus, Roopa Kohli-Seth, and Martin Goldman have no financial support to disclose.
Footnotes
Funding: This manuscript was internally funded.
Supplementary material associated with this article can be found in the online version at https://doi.org/10.1016/j.amjcard.2021.07.048.
Appendix. Supplementary materials
References
- 1.Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, Xiang J, Wang Y, Song B, Gu X, Guan L, Wei Y, Li H, Wu X, Xu J, Tu S, Zhang Y, Chen H, Cao B. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Siddiqi HK, Mehra MR. COVID-19 illness in native and immunosuppressed states: a clinical–therapeutic staging proposal. J Heart Lung Transpl. 2020;39:405. doi: 10.1016/j.healun.2020.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Agricola E, Beneduce A, Esposito A, Ingallina G, Palumbo D, Palmisano A, Ancona F, Baldetti L, Pagnesi M, Melisurgo G, Zangrillo A, De Cobelli F. Heart and lung multimodality imaging in COVID-19. JACC Cardiovasc Imaging. 2020;13:1792–1808. doi: 10.1016/j.jcmg.2020.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lala A, Johnson KW, Januzzi JL, Russak AJ, Paranjpe I, Richter F, Zhao S, Somani S, Van Vleck T, Vaid A, Chaudhry F, De Freitas JK, Fayad ZA, Pinney SP, Levin M, Charney A, Bagiella E, Narula J, Glicksberg BS, Nadkarni G, Mancini DM, Fuster V. Prevalence and impact of myocardial injury in patients hospitalized with COVID-19 infection. J Am Coll Cardiol. 2020;76:533–546. doi: 10.1016/j.jacc.2020.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ackermann M, Verleden SE, Kuehnel M, Haverich A, Welte T, Laenger F, Vanstapel A, Werlein C, Stark H, Tzankov A, Li WW, Li VW, Mentzer SJ, Jonigk D. Pulmonary vascular endothelialitis, thrombosis, and angiogenesis in Covid-19. N Engl J Med. 2020;383:120–128. doi: 10.1056/NEJMoa2015432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Basso C, Leone O, Rizzo S, De Gaspari M, van der Wal AC, MC Aubry, Bois MC, Lin PT, Maleszewski JJ, Stone JR. Pathological features of COVID-19-associated myocardial injury: a multicentre cardiovascular pathology study. Eur Heart J. 2020;41:3827–3835. doi: 10.1093/eurheartj/ehaa664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lala A, Johnson KW, Januzzi JL, Russak AJ, Paranjpe I, Richter F, Zhao S, Somani S, Van Vleck T, Vaid A, Chaudhry F, De Freitas JK, Fayad ZA, Pinney SP, Levin M, Charney A, Bagiella E, Narula J, Glicksberg BS, Nadkarni G, Mancini DM, Fuster V. Prevalence and impact of myocardial injury in patients hospitalized with COVID-19 infection. J Am Coll Cardiol. 2020;76:533–546. doi: 10.1016/j.jacc.2020.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fischer K, Marggraf M, Stark AW, Kaneko K, Aghayev A, Guensch DP, Huber AT, Steigner M, Blankstein R, Reichlin T, Windecker S, Kwong RY, Gräni C. Association of ECG parameters with late gadolinium enhancement and outcome in patients with clinical suspicion of acute or subacute myocarditis referred for CMR imaging. PLoS One. 2020;15 doi: 10.1371/journal.pone.0227134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lampert J, Miller M, Halperin JL, Oates C, Giustino G, Feinman J, Miller MA, Dukkipati SR, Goldman ME, Reddy VY. Prognostic value of electrocardiographic QRS diminution in patients with COVID-19. J Am Coll Cardiol. 2021;77:2258–2259. doi: 10.1016/j.jacc.2021.02.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bruch C, Schmermund A, Dagres N, Bartel T, Caspari G, Sack S, Erbel R. Changes in QRS voltage in cardiac tamponade and pericardial effusion: reversibility after pericardiocentesis and after anti-inflammatory drug treatment. J Am Coll Cardiol. 2001;38:219–226. doi: 10.1016/s0735-1097(01)01313-4. [DOI] [PubMed] [Google Scholar]
- 11.Madias JE. Low QRS voltage and its causes. J Electrocardiol. 2008;41:498–500. doi: 10.1016/j.jelectrocard.2008.06.021. [DOI] [PubMed] [Google Scholar]
- 12.Kamath SA, Meo Neto Jde P, Canham RM, Uddin F, Toto KH, Nelson LL, Kaiser PA, de Lemos JA, Drazner MH. Low voltage on the electrocardiogram is a marker of disease severity and a risk factor for adverse outcomes in patients with heart failure due to systolic dysfunction. Am Heart J. 2006;152:355–361. doi: 10.1016/j.ahj.2005.12.021. [DOI] [PubMed] [Google Scholar]
- 13.Cyrille NB, Goldsmith J, Alvarez J, Maurer MS. Prevalence and prognostic significance of low QRS voltage among the three main types of cardiac amyloidosis. Am J Cardiol. 2014;114:1089–1093. doi: 10.1016/j.amjcard.2014.07.026. [DOI] [PubMed] [Google Scholar]
- 14.Dudley SC, Jr, Baumgarten CM, Ornato JP. Reversal of low voltage and infarction pattern on the surface electrocardiogram after renal hemodialysis for pulmonary edema. J Electrocardiol. 1990;23:341–345. doi: 10.1016/0022-0736(90)90124-k. [DOI] [PubMed] [Google Scholar]
- 15.Spodick DH. Electrocardiographic studies in pulmonary disease: I. Electrocardiographic abnormalities in diffuse lung disease. Circulation. 1959;20:1067–1072. doi: 10.1161/01.cir.20.6.1067. [DOI] [PubMed] [Google Scholar]
- 16.Oreto G, Luzza F, Donato A, Satullo G, Calabrò MP, Consolo A, Arrigo F. Electrocardiographic changes associated with haematocrit variations. Eur Heart J. 1992;13:634–637. doi: 10.1093/oxfordjournals.eurheartj.a060227. [DOI] [PubMed] [Google Scholar]
- 17.Madias JE. Low voltage ECG in myocarditis: peripheral edema as a plausible contributing mechanism. Pacing Clin Electrophysiol. 2007;30:448–452. doi: 10.1111/j.1540-8159.2007.00691.x. [DOI] [PubMed] [Google Scholar]
- 18.Schroeder JS, Popp RL, Stinson EB, Dong E, Jr, Shumway NE, Harrison DC. Acute rejection following cardiac transplantation. Phonocardiographic and ultrasound observations. Circulation. 1969;40:155–164. doi: 10.1161/01.cir.40.2.155. [DOI] [PubMed] [Google Scholar]
- 19.Fox KM, Tomlinson IW, Meek DR, Portal RW, Aber CP. Low voltage electrocardiogram after acute myocardial infarction. Br Heart J. 1975;37:748–751. doi: 10.1136/hrt.37.7.748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Roberts WC, Filardo G, Ko JM, Siegel RJ, Dollar AL, Ross EM, Shirani J. Comparison of total 12-lead QRS voltage in a variety of cardiac conditions and its usefulness in predicting increased cardiac mass. Am J Cardiol. 2013;112:904–909. doi: 10.1016/j.amjcard.2013.04.061. [DOI] [PubMed] [Google Scholar]
- 21.Huang L, Zhao P, Tang D, Zhu T, Han R, Zhan C, Liu W, Zeng H, Tao Q, Xia L. Cardiac involvement in patients recovered from COVID-2019 identified using magnetic resonance imaging. JACC Cardiovasc Imaging. 2020;13:2330–2339. doi: 10.1016/j.jcmg.2020.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Puntmann VO, Carerj ML, Wieters I, Fahim M, Arendt C, Hoffmann J, Shchendrygina A, Escher F, Vasa-Nicotera M, Zeiher AM, Vehreschild M, Nagel E. Outcomes of cardiovascular magnetic resonance imaging in patients recently recovered from coronavirus disease 2019 (COVID-19) JAMA Cardiol. 2020;5:1265–1273. doi: 10.1001/jamacardio.2020.3557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ukimura A, Satomi H, Ooi Y, Kanzaki Y. Myocarditis associated with influenza a H1N1pdm2009. Influenza Res Treat. 2012;2012 doi: 10.1155/2012/351979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wasserburger RH, Kelly JR, Rasmussen HK, Juhl JH. The electrocardiographic pentalogy of pulmonary emphysema. A correlation of roentgenographic findings and pulmonary function studies. Circulation. 1959;20:831–841. doi: 10.1161/01.cir.20.5.831. [DOI] [PubMed] [Google Scholar]
- 25.Bao C, Liu X, Zhang H, Li Y, Liu J. Coronavirus disease 2019 (COVID-19) CT findings: a systematic review and meta-analysis. J Am Coll Radiol. 2020;17:701–709. doi: 10.1016/j.jacr.2020.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Giustino G, Croft LB, Stefanini GG, Bragato R, Silbiger JJ, Vicenzi M, Danilov T, Kukar N, Shaban N, Kini A, Camaj A, Bienstock SW, Rashed ER, Rahman K, Oates CP, Buckley S, Elbaum LS, Arkonac D, Fiter R, Singh R, Li E, Razuk V, Robinson SE, Miller M, Bier B, Donghi V, Pisaniello M, Mantovani R, Pinto G, Rota I, Baggio S, Chiarito M, Fazzari F, Cusmano I, Curzi M, Ro R, Malick W, Kamran M, Kohli-Seth R, Bassily-Marcus AM, Neibart E, Serrao G, Perk G, Mancini D, Reddy VY, Pinney SP, Dangas G, Blasi F, Sharma SK, Mehran R, Condorelli G, Stone GW, Fuster V, Lerakis S, Goldman ME. Characterization of myocardial injury in patients with COVID-19. J Am Coll Cardiol. 2020;76:2043–2055. doi: 10.1016/j.jacc.2020.08.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.McGuinness G, Zhan C, Rosenberg N, Azour L, Wickstrom M, Mason DM, Thomas KM, Moore WH. Increased incidence of barotrauma in patients with COVID-19 on invasive mechanical ventilation. Radiology. 2020;297:e252–e262. doi: 10.1148/radiol.2020202352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shi H, Han X, Jiang N, Cao Y, Alwalid O, Gu J, Fan Y, Zheng C. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. Lancet Infect Dis. 2020;20:425–434. doi: 10.1016/S1473-3099(20)30086-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Elinoff J, Talmor D, Subramaniam B, Karmpaliotis D, Goldberger AL, Malhotra A. Effects of mechanical ventilation on the electrocardiogram in adults. Lung. 2008;186:219. doi: 10.1007/s00408-008-9094-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dexamethasone in hospitalized patients with Covid-19. N Engl J Med. 2020;384:693–704. doi: 10.1056/NEJMoa2021436. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.