Abstract
Objective
During the COVID-19 pandemic, Radiology practices experienced marked reductions in outpatient imaging volumes. Our purpose was to evaluate the timing, rate, and degree of recovery of outpatient imaging during the first wave of the pandemic. We also sought to ascertain the relationship of outpatient imaging recovery to the incidence of COVID-19 cases.
Methods
Retrospective study of outpatient imaging volumes in a large healthcare system was performed from January 1, 2019-August 25, 2020. Dataset was split to compare Pre-COVID (weeks 1–9), Peak-COVID (weeks 10–15) and Recovery-COVID (weeks 16–34) periods. Chi-square and Independent-samples t-tests compared weekly outpatient imaging volumes in 2020 and 2019. Regression analyses assessed the rate of decline and recovery in Peak-COVID and Recovery-COVID periods, respectively.
Results
Total outpatient imaging volume in 2020 (weeks 1–34) was 327,738 exams, compared to 440,314 in 2019. The 2020 mean weekly imaging volumes were significantly decreased in Peak-COVID (p = 0.0148) and Recovery-COVID (p = 0.0003) periods. Mean weekly decline rate was −2580 exams/week and recovery rate was +617 exams/week. The 2020 Post-COVID (weeks 10–34) period had an average decrease of 36.5% (4813.4/13,178.6) imaging exams/week and total estimated decrease of 120,335 exams. Significant inverse correlation (−0.8338, p < 0.0001) was seen between positive-tested COVID-19 cases and imaging utilization with 1-week lag during Post-COVID (weeks 10–34) period.
Conclusion
Recovery of outpatient imaging volume during the first wave of COVID-19 pandemic showed a gradual return to pre-pandemic levels over the course of 3–4 months. The rate of imaging utilization was inversely associated with new positive-tested COVID-19 cases with a 1-week lag.
Keywords: Outpatient imaging, COVID-19 pandemic, Recovery
1. Introduction
The COVID-19 pandemic continues to have a devastating global impact on the health of the population with an increasing need for healthcare resources, while the demands for imaging services have drastically declined 1., 2., 3.. During the first wave of the COVID-19 pandemic, Radiology departments experienced marked reductions in imaging volumes across all patient service locations, with the greatest impact on outpatient imaging [1]. Many outpatient imaging centers rescheduled and/or canceled non-urgent imaging exams and procedures in response to the mandated public health policy and social distancing requirements during the peak period of the pandemic.
To guide Radiology practices through uncertainty, scenario models were developed to predict imaging volume recovery over the course of the COVID-19 pandemic [4]. However, prediction models have inherent limitations including assumptions that may not be generalizable in new scenarios. In particular, some recently proposed models were based on prior epidemics in other countries, natural disasters, and other economic downturns, none of which was truly comparable to the COVID-19 pandemic. Given these inherent limitations, actual data from Radiology practices in the U.S. during the COVID-19 pandemic is needed to assess the predictive value of these models. Documenting and analyzing new events where observed data differ from model predictions is important to provide information necessary to further refine the models and make them more accurate.
The purpose of this study was to evaluate the actual recovery rate and pattern of outpatient imaging utilization during the first wave of the COVID-19 pandemic using the observed data from a large healthcare institution. We also sought to ascertain the relationship of outpatient imaging recovery to the incidence of COVID-19 cases as a potential factor influencing the recovery rate.
2. Materials and methods
We performed a retrospective review of the outpatient imaging case volumes in a large integrated healthcare system, located in the New York city metropolitan area, to assess the recovery rate and pattern of outpatient imaging utilization during the first wave of the COVID-19 pandemic. For a comprehensive evaluation of outpatient imaging utilization across the healthcare system, we included both hospital-based and free-standing outpatient imaging centers in this study. The study period was defined from January 1 – August 25, 2020, which were assigned as weeks 1–34 based on consecutive 7-day periods starting January 1st. The comparison study period was the same weeks 1–34 in the prior year 2019 to account for monthly and seasonal variation. The 2020 and 2019 study periods were split into the following 3 time periods for statistical analysis based on the first-documented positive-tested COVID-19 case in our healthcare system on March 8, 2020 (week 10): (1) Pre-COVID – weeks 1–9, (2) Peak-COVID – weeks 10–15, and (3) Recovery-COVID – weeks 16–34. Week 16 represented the turning point when outpatient imaging volume began to increase after the decline period. Additional analyses were performed combining the Peak-COVID and Recovery-COVID periods into a single Post-COVID (weeks 10–34) time period in order to assess the cumulative effect on outpatient imaging utilization from the start of the COVID-19 pandemic.
The outpatient imaging case volumes were provided as aggregate data for each day (Sunday – Saturday) in 2020 and 2019 for weeks 1–34 in the outpatient setting including all imaging modality types (X-ray, mammography, computed tomography [CT], magnetic resonance imaging [MRI], ultrasound, interventional radiology, nuclear medicine). Data was further aggregated into weekly case volumes for statistical analysis. Institutional Review Board (IRB) waived approval using retrospective aggregate data in the statistical analysis.
Since public health mandates and local institutional measures were instituted during the COVID-19 pandemic in order to lower the risk of exposure and transmission of disease, we acknowledge the following policy dates that may have an effect on outpatient imaging utilization: (a) March 17, 2020 (week 11) – Institution canceled routine cancer screening (breast and lung cancer) and issued guidelines that all non-urgent imaging should be avoided when possible in suspected or confirmed COVID-19 patients, (b) March 22, 2020 (week 12) – New York State on PAUSE Executive Order, (c) May 15, 2020 (week 20) – Institution reinstated routine cancer screening, (d) Reopening phases in our geographic region: Phase I on May 27, 2020 (week 22), Phase 2 on June 10, 2020 (week 24), Phase III on June 24, 2020 (week 26), and Phase IV on July 8, 2020 (week 28). Other factors that may have an effect on outpatient imaging utilization are the national holidays and power outages due to the tropical storm Isaias that occurred during the first wave of the COVID-19 pandemic. Holidays included Martin Luther King Day on January 20, 2020 (week 3), Presidents Day on February 17, 2020 (week 7), Memorial Day on May 25, 2020 (week 21), and Independence Day on July 4, 2020 (week 27). The tropical storm Isaias occurred on August 4, 2020 (week 31).
2.1. Statistical analysis
The aggregate sum data for the weekly imaging case volumes in the outpatient setting were plotted from weeks 1–34 to demonstrate the trend in outpatient imaging utilization in both 2020 and 2019 calendar years. The public health mandates, as well as the national holidays and tropical storm Isaias, were represented in the trend analysis. Separately, the aggregated data for the weekly positive-tested COVID-19 cases in our healthcare system were plotted with the weekly outpatient imaging case volumes from weeks 1–34 to demonstrate the trend in outpatient imaging utilization with newly diagnosed COVID-19 cases.
The outpatient imaging case volumes were aggregated for the Pre-COVID (weeks 1–9), Peak-COVID (weeks 10–15), Recovery-COVID (weeks 16–34), and total COVID (weeks 1–34) time periods in both 2020 and 2019. Chi-square tests were performed to assess statistically significant differences in the 2020 and 2019 outpatient imaging volumes during the Pre-COVID, Peak-COVID, and Recovery-COVID periods.
The mean weekly outpatient imaging volumes and standard deviation (SD) were calculated for the Pre-COVID (weeks 1–9), Peak-COVID (weeks 10–15), Recovery-COVID (weeks 16–34), Post-COVID (weeks 10–34), and total weeks 1–34 time periods in both 2020 and 2019. Independent samples t-tests were performed to assess statistically significant differences in the 2020 and 2019 mean weekly outpatient imaging volumes during each time period.
To evaluate the overall decline of outpatient imaging exams during the 2020 Post-COVID (weeks 10–34) period, the difference in the mean weekly outpatient imaging utilization was estimated using the Pre-COVID (weeks 1–9) period in the same year as the reference to account for the growth in outpatient imaging utilization from the prior year in 2019. Taking a conservative approach, without estimating further growth in outpatient imaging utilization during weeks 10–34 in 2020, the mean weekly volume would be expected to remain stable from the Pre-COVID period. The absolute difference and the percent difference in the mean weekly outpatient imaging volume were calculated during the 2020 Post-COVID period using the 2020 Pre-COVID period as the reference. The absolute total decline of outpatient imaging exams during the 2020 Post-COVID period was extrapolated from this data by multiplying the mean weekly decline of outpatient imaging volume by the total weeks (n = 25) in the Post-COVID period.
Linear regression models of weekly volume (dependent variable) and week (independent variable) were performed to assess the rate of decline and recovery in the Peak-COVID and Recovery-COVID periods, respectively. Linear regression models and correlation analysis of the weekly volume (dependent variable) and new positive-tested COVID-19 cases (independent variable) in our healthcare system (including one and two-week time-lags) were performed to assess their possible association. Statistical significance was considered for p-values <0.05. All statistical analyses were performed using SAS v9.4 (SAS, North Carolina).
3. Results
The total outpatient imaging case volume performed at our institution in year 2020 from weeks 1–34 was 327,738 exams, compared to 440,314 exams in year 2019 during the same time period (weeks 1–34). Table 1 displays the outpatient imaging case volumes for the Pre-COVID (weeks 1–9), Peak-COVID (weeks 10–15), and Recovery-COVID (weeks 16–34) time periods in years 2020 and 2019. Compared to 2019, there was a statistically significant difference in the proportion of outpatient imaging volume in 2020 (p < 0.0001), with 7.6% increased imaging volume in the Pre-COVID, 56.6% decreased imaging volume in the Peak-COVID, and 30.1% decreased imaging volume in the Recovery-COVID periods. Fig. 1 demonstrates the trend in the outpatient imaging case volumes in year 2020 across weeks 1–34, compared to 2019. The public health mandates, as well as the national holidays and tropical storm Isaias, are superimposed on the 2020 outpatient imaging utilization trend during the first wave of the COVID-19 pandemic.
Table 1.
Outpatient imaging case volumes for the pre-COVID, peak-COVID and recovery-COVID time periods in years 2020 and 2019.
| COVID time periods | 2020 | 2019 | P-value |
|---|---|---|---|
| Pre-COVID (weeks 1–9) | 118,607 | 110,263 | <0.0001 |
| Peak-COVID (weeks 10–15) | 35,482 | 81,774 | |
| Recovery-COVID (weeks 16–34) | 173,649 | 248,277 | |
| TOTAL (weeks 1–34) | 327,738 | 440,314 |
Fig. 1.
2020 and 2019 total outpatient imaging utilization trend data from weeks 1–34. The first COVID-19 patient was confirmed in our healthcare system on March 8, 2020 (week 10). The COVID time periods are represented as Pre-COVID (weeks 1–9), Peak-COVID (weeks 10–15), and Recovery-COVID (weeks 16–34). The reopening phases for non-essential businesses in our geographic region were Phase 1 on May 27, 2020 (week 22), Phase 2 on June 10, 2020 (week 24), Phase 3 on June 24, 2020 (week 26) and Phase 4 on July 8, 2020 (week 28). The 2020 and 2019 dips in outpatient imaging utilization correspond to the following national holidays numbered as 1 – Martin Luther King Day on January 20, 2020 (week 3), 2 – Presidents Day on February 17, 2020 (week 7), 3 – Memorial Day on May 25, 2020 (week 21), and 4 – Independence Day on July 4, 2020 (week 27). The tropical storm Isaias occurred on August 4, 2020 (week 31) corresponding to the last dip (5) in the 2020 outpatient imaging utilization. The X-axis represents the weeks and the Y-axis represents the number of outpatient imaging exams.
Table 2 compares the 2020 and 2019 mean weekly imaging volume performed in the outpatient setting for the Pre-COVID (weeks 1–9), Peak-COVID (weeks 10–15), and Recovery-COVID (weeks 16–34) time periods. In the Pre-COVID period, the 2020 mean weekly outpatient imaging volume was not statistically different compared to 2019 (p < 0.1428). However, the mean weekly outpatient imaging volumes were statistically decreased in the Peak-COVID (p = 0.0148) and Recovery-COVID (p = 0.0003) periods, as well as the total time period including all weeks from 1 to 34 (p≤0.0001).
Table 2.
Mean weekly outpatient imaging volumes for the pre-COVID, peak-COVID and recovery-COVID time periods in years 2020 and 2019.
| COVID time periods | 2020 |
2019 |
P-value |
||
|---|---|---|---|---|---|
| Mean | 95% CI | Mean | 95% CI | *<0.05 | |
| Pre-COVID (weeks 1–9) | 13,178.6 | 12,151.5–14,205.6 | 12,251.4 | 11,318.8–13,184.1 | 0.1428 |
| Peak-COVID (weeks 10–15) | 5913.7 | 477.2–11,350.2 | 13,629.0 | 13,499.3–13,758.7 | 0.0148* |
| Recovery-COVID (weeks 16–34) | 9139.4 | 7305.8–10,973.0 | 13,067.2 | 12,614.1–13,520.3 | 0.0003* |
| TOTAL (weeks 1–34) | 9639.4 | 8139.6–11,139.2 | 12,950.4 | 12,590.2–13,310.7 | <0.0001* |
Additional analyses were performed combining the Peak-COVID (weeks 10–15) and Recovery-COVID (weeks 16–34) periods into a single Post-COVID (weeks 10–34) period. A statistically significant decrease in the 2020 mean weekly outpatient imaging volume [95% CI] was seen in the Post-COVID period (8365.2 [6593.5 - 10,136.9]) compared to the Pre-COVID (13,178.6 [12,151.5-14,205.6]) period (p < 0.0001). There was also a statistically significant decrease in the mean weekly outpatient imaging volume [95% CI] in the 2020 Post-COVID (8365.2 [6593.5-10,136.9]) compared to the 2019 Post-COVID (13,202.0 [12,850.4-13,553.7]) period (p < 0.0001). Furthermore, the regression analysis reveals the mean weekly decline rate during the 2020 Peak-COVID (weeks 10–15) period was −2580 outpatient imaging exams per week. The mean weekly recovery rate during the 2020 Recovery-COVID (weeks 16–34) period was +617 outpatient imaging exams per week. Overall, this finding indicates a slower rate of recovery in weekly outpatient imaging volumes in the Recovery-COVID (weeks 16–34) period than the rate of decline in the Peak-COVID (weeks 10–15) period.
To evaluate the overall decline of outpatient imaging exams during the 2020 Post-COVID (weeks 10–34) period, the difference in the mean weekly outpatient imaging utilization was estimated compared to the Pre-COVID period in the same year to account for the annual growth in outpatient imaging utilization from the prior year. Taking a conservative approach, without estimating further growth in outpatient imaging utilization during weeks 10–34 in 2020, the mean weekly volume would be expected to remain stable as 13,178.6 exams per week, as observed in the 2020 Pre-COVID (weeks 1–9) period. However, the Post-COVID (weeks 10–34) period had a mean weekly volume of 8365.2 exams per week, indicating that on average a decrease of 36.5% (4813.4/13,178.6) outpatient imaging exams per week. When accounting for the 25 weeks in the 2020 Post-COVID (weeks 10–34) period, the total decrease of 120,335 outpatient imaging exams is estimated.
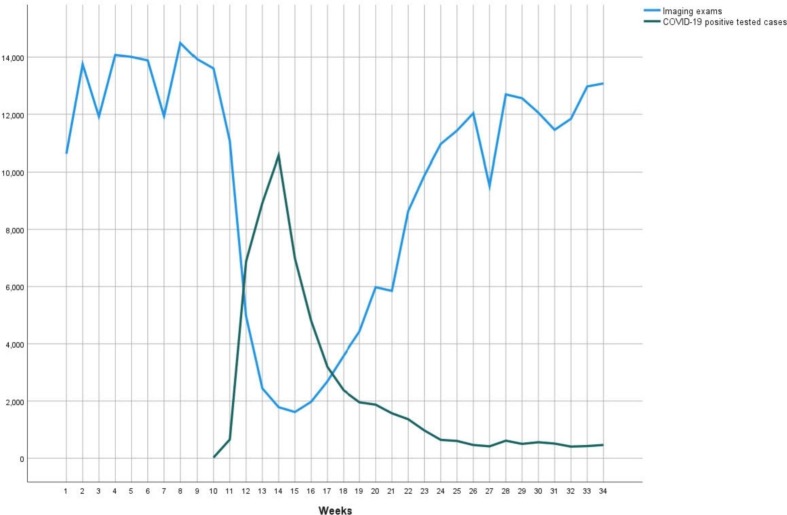
Additional analyses were performed to assess the correlation of new positive-tested COVID-19 cases with outpatient imaging utilization. Fig. 2 displays the weekly new positive-tested COVID-19 cases in our healthcare system superimposed on the 2020 outpatient imaging utilization trend data. The first positive-tested COVID-19 case in our healthcare system was confirmed on March 8, 2020 (week 10). Regression analysis revealed a statistically significant inverse correlation (−0.8338, p < 0.0001) between the positive-tested COVID cases and outpatient imaging utilization during the Post-COVID (weeks 10–34) period with a 1-week lag. The adjusted-R2 is 0.6814 and parameter = −1.1833, representing a medium-strong inverse correlation. These results can be interpreted as for every 1 new positive-tested COVID-19 case, there will be a decrease of approximately 1.2 outpatient imaging exams with the lag of 1 week.
Fig. 2.
2020 outpatient imaging utilization trend data across weeks 1–34 (blue line). The trend for the new COVID-19 positive-tested cases at our institution are shown (green line) with the first positive-tested case on March 8, 2020 (week 10). Regression analysis revealed a statistically significant medium-strong inverse correlation (−0.8338, p < 0.0001) between the new positive-tested COVID-19 cases and outpatient imaging utilization 1 week later during the Post-COVID (weeks 10–34) period. (For interpretation of the references to color in this figure legend, the reader is referred to the web version of this article.)
4. Discussion
The COVID-19 pandemic has brought significant uncertainty to Radiology practices, not only regarding the unprecedented imaging volume reduction during the peak of the pandemic, but importantly what to expect during the recovery period. In order to appropriately plan for the post-pandemic imaging needs of the population, understanding the rate, duration and pattern of imaging recovery would be instrumental in directing healthcare resources. This study reveals that during the first wave of the pandemic, there was a statistically significant decline in outpatient imaging volume, compared to the same time-periods in 2019. Although these findings are similar to previous reports in the literature 1., 2., 3., this study demonstrates that outpatient imaging volumes remained significantly reduced even during the recovery phase when reopening of non-essential businesses occurred. The regression analysis reveals a mean weekly decline rate during the 2020 Peak-COVID (weeks 10–15) period of −2580 outpatient imaging exams per week, while the mean weekly recovery rate during the 2020 Recovery-COVID (weeks 16–34) period was only +617 outpatient imaging exams per week, with imaging volumes gradually returning to the pre-pandemic baseline over the course of 3–4 months. In other words, the recovery was slow and prolonged relative to the steep peak-pandemic decline. This resulted in an estimated total decrease of 120,335 outpatient imaging exams during the first wave of the pandemic.
Based on historical events, Guitron et al. proposed a model with three potential scenarios for long-term volume recovery in the COVID-19 pandemic [4]. These included a swift recovery scenario, a gradual recovery scenario, and a muted recovery scenario [4]. The data from our study most closely resembles the “gradual” scenario model in terms of the shape and duration of the recovery curve. Our data differs from the prediction model in that we experienced a complete return to pre-pandemic baseline volume per week as opposed to the prediction of a return to 80–90% of prior volume in 3–4 months. Another difference from the model concerns the timing of the recovery. More specifically, the return in outpatient imaging occurred prior to the implementation of the national vaccination program and without a known cure for COVID-19 infection, which were both suggested to be necessary for recovery to begin.
Recovery of outpatient imaging may be accelerated by public outreach and national campaigns demonstrating that imaging centers are safe and urging patients not to delay healthcare any longer. A temporal relationship between the imaging volume trend and public health announcements as well as COVID-19 cases has been reported in the literature [5]. In our study, the recovery of outpatient imaging volume did not appear to be closely related to the local legislative policies for reopening of non-essential businesses. In particular, outpatient imaging utilization began to increase at week 16, with over 50% return, prior to reopening phase 1 (week 22). However, this study found a medium-strong inverse correlation between outpatient imaging volume and the daily number of new positive-tested COVID-19 cases in our region. The correlation analyses revealed that there was a 1-week lag between the positive-tested COVID-19 cases and outpatient imaging volume. For example, for every 1 new positive-tested COVID-19 case, there were 1.2 fewer outpatient imaging exams 1 week later. Although this analysis does not imply causation, it does shed light on another possible contributing factor affecting outpatient imaging utilization during the pandemic.
Due to the inherent limitations of retrospective study designs, our data collection and analyses could not assess causation of the recovery rate observed with outpatient imaging volume. Furthermore, detailed analyses exploring the specific types of imaging services with the fastest and slowest recovery rates were not evaluated. Thus, it should not be assumed that the different imaging services recover at the same rate. Specifically, CT volume has been reported with faster rates of recovery while mammography recovered at a slower rate [5]. Additionally, our statistical analyses comparing the 2020 and 2019 outpatient imaging volume did not account for the expected growth rate in 2020 Post-COVID period (weeks 10–34) had the COVID-19 pandemic not occurred, thus possibly underestimating the difference in outpatient imaging decline in both the Peak-COVID and Recovery-COVID time periods. Lastly, it's important to recognize that our institution was located in the epicenter of the first wave of the COVID-19 pandemic, potentially limiting the generalizability of these results. However, as the nationwide spread of COVID-19 continues to affect many Radiology practices across the country, these findings may be useful in generating predictive models of recovery.
In summary, this study reveals that the recovery of outpatient imaging volume during the first wave of the COVID-19 pandemic was a gradual and steady return to pre-pandemic levels over the course of 3–4 months. Unlike prior prediction models that expected outpatient imaging recovery to be linked to health policy changes and/or national vaccination programs, our study showed that outpatient imaging volume had over 50% return prior to reopening Phase I when a vaccine was not yet available to the public. Instead, the return of outpatient imaging utilization was associated with the new positive-tested COVID-19 weekly cases. These findings may help inform Radiology practices regarding other contributing factors influencing outpatient imaging utilization during the recovery period.
Author's employment status, leadership positions, roles on this study and disclosure statements
Jason J. Naidich, MD, MBA, academic affiliation non-partnership track employee, Chair, Department of Radiology, Donald and Barbara Zucker School of Medicine at Hofstra/Northwell.
Senior Vice President/Regional Executive Director, Northwell Health
-
-
Substantially contributed to the conception and design of the study
-
-
Substantially contributed to the data supervision
-
-
Substantially contributed to the writing and revision of the manuscript
-
-
Approved the final version of the manuscript
-
-
Accountable for the manuscript's contents
Disclosure statement: Dr. Naidich has nothing to disclose.
Artem Boltyenkov, PhD, MBA, academic affiliation non-partnership track employee, Visiting Scholar at the Feinstein Institutes for Medical Research
-
-
Substantially contributed to the conception and design of the study
-
-
Substantially contributed to the data curation and organization
-
-
Substantially contributed to the statistical analyses
-
-
Substantially contributed to the writing and revision of the manuscript
-
-
Approved the final version of the manuscript
-
-
Accountable for the manuscript's contents
Disclosure statement: Dr. Boltyenkov reports personal fees from Siemens Medical Solutions USA, Inc., outside the submitted work, and is a shareholder of Siemens Healthineers.
Jason J. Wang, PhD, academic affiliation non-partnership track employee
-
-
Substantially contributed to the design of the study
-
-
Substantially contributed to the data curation and organization
-
-
Substantially contributed to the statistical analyses
-
-
Substantially contributed to the revision of the manuscript
-
-
Approved the final version of the manuscript
-
-
Accountable for the manuscript's contents
Disclosure statement: Dr. Wang has nothing to disclose.
Eric Cruzen, MD, MBA, academic affiliation non-partnership track employee,
Chief Medical Informatics Officer, Northwell Health
-
-
Substantially contributed to the data collection
-
-
Substantially contributed to the revision of the manuscript
-
-
Approved the final version of the manuscript
-
-
Accountable for the manuscript's contents
Disclosure statement: Dr. Cruzen has nothing to disclose.
Jesse Chusid, MD, MBA, academic affiliation non-partnership track employee,
Senior Vice President of Imaging Services, Northwell Health
-
-
Substantially contributed to the design of the study
-
-
Substantially contributed to the data supervision
-
-
Substantially contributed to the revision of the manuscript
-
-
Approved the final version of the manuscript
-
-
Accountable for the manuscript's contents
Disclosure statement: Dr. Chusid has nothing to disclose.
Elizabeth Rula, PhD, non-partnership track employee, Executive Director of the Harvey L. Neiman Health Policy Institute
-
-
Substantially contributed to the conception and design of the study
-
-
Substantially contributed to the revision of the manuscript
-
-
Approved the final version of the manuscript
-
-
Accountable for the manuscript's contents
Disclosure statement: Dr. Rula reports employment at the Harvey L. Neiman Health Policy Institute.
Pina C. Sanelli, MD, MPH, FACR, academic affiliation non-partnership track employee, Vice Chair of Research, Department of Radiology, Donald and Barbara Zucker School of Medicine at Hofstra/Northwell
-
-
Substantially contributed to the conception and design of the study
-
-
Substantially contributed to the data curation and organization
-
-
Substantially contributed to the statistical analyses
-
-
Substantially contributed to the writing and revision of the manuscript
-
-
Approved the final version of the manuscript
-
-
Accountable for the manuscript's contents
Disclosure statement: Dr. Sanelli reports grants from Harvey L. Neiman Health Policy Institute, during the conduct of the study; grants and non-financial support from Siemens Healthineers, Inc., outside the submitted work.
Statement of data access and integrity
The authors declare that they had full access to all of the data in this study and the authors take complete responsibility for the integrity of the data and the accuracy of the data analysis.
Sources of support
Funding support received from the Harvey L. Neiman Health Policy Institute through a research partnership.
Acknowledgments
We would like to acknowledge Frank Rizzo, Morgan O'Hare and Chen (Shirley) Liu from the finance department at our institution for contributing the aggregated data used in the analyses in this study.
We would like to acknowledge the Northwell Health COVID-19 Research Consortium.
References
- 1.Naidich J.J., Boltyenkov A., Wang J.J., Chusid J., Hughes D., Sanelli P.C. Impact of the coronavirus disease 2019 (COVID-19) pandemic on imaging case volumes. J Am Coll Radiol. 2020 Jul;17(7):865–872. doi: 10.1016/j.jacr.2020.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.For the RSNA COVID-19 Task Force. Sharpe R.E., Kuszyk B.S., Mossa-Basha M. Special report of the RSNA COVID-19 task force: the short- and long-term financial impact of the COVID-19 pandemic on private radiology practices. Radiology. Jan 2021;298(1) doi: 10.1148/radiol.2020202517. PubMed PMID: 32677874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Parikh K.D., Ramaiya N.H., Kikano E.G., Tirumani S.H., Pandya H., Stovicek B., Sunshine J.L., Plecha D.M. COVID-19 pandemic impact on decreased imaging utilization: a single institutional experience. Acad Radiol. 2020 Sep;27(9):1204–1213. doi: 10.1016/j.acra.2020.06.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Guitron S., Pianykh O.S., Succi M.D., Lang M., Brink J. COVID-19: recovery models for radiology departments. J Am Coll Radiol. Nov 2020;17(11):1460–1468. doi: 10.1016/j.jacr.2020.09.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lang M., Yeung T., Mendoza D.P., Flores E.J., Som A., Lang A.L., Pianykh O.S., Lee S.I., Saini S., Little B.P., Succi M.D. Imaging volume trends and recovery during the COVID-19 pandemic: a comparative analysis between a large urban academic hospital and its affiliated imaging centers. Acad Radiol. Oct 2020;27(10):1353–1362. doi: 10.1016/j.acra.2020.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]