Abstract
There is growing interest for a communitarian approach to the governance of genomics and for genomics governance to be grounded in principles of justice, equity and solidarity. However, little conceptual work has been done to show how communitarian-based principles may inform, support or guide the governance of genomics research. Given that solidarity is a key principle in Ubuntu, an African communitarian ethic and theory of justice, there is emerging interest about the extent to which Ubuntu could offer guidance for the equitable governance of genomics in Africa. To this effect, we undertook a conceptual analysis of Ubuntu with the goal of identifying principles that could inform equity-oriented governance of genomics research in Africa. Solidarity, reciprocity, open sharing, accountability, mutual trust, deliberative decision-making and inclusivity were identified as core principles that speak directly to the macro-level justice issues in genomics research in Africa such as: the exploitation of study populations and African researchers, equitable access and use of genomics data, benefit sharing, the possibility of genomics to widen global health inequities and the fair distribution of resources such as intellectual property and patents. We use the identified the principles to develop ethical guidance for genomics governance in Africa.
Keywords: Ubuntu, genomics, governance, equity, justice, Africa, solidarity, reciprocity
Introduction
It is anticipated that in the near future, there will be widespread integration of genomics into almost all areas of biomedical research and mainstream medical and public-health practices (Green et al. 2020; Stark et al. 2019). On the other hand, genomics raises complex ethical questions relating to the nature and type of informed consent that is appropriate for data sharing (Mascalzoni et al. 2008; McGuire and Beskow 2010) and more recently to questions of justice linked to secondary uses of samples and data, the equitable distribution of the benefits and risk of genomics research; resource allocation, and the equity-oriented responsibilities of genomics stakeholders (Gottweis 2005; Smith et al. 2004; Dowdeswell et al. 2006; Munung and de Vries 2020). These ethical issues are complex for various reasons. Firstly, it is near impossible to provide genomics research participants with comprehensive information on downstream uses of their data including the associated risks or benefits to them, their families and/or their communities. Secondly, if genomics is to deliver on the promise of precision medicine, then genomic information will have to be transformed into tangible clinical interventions such as diagnostic and analytic tools. This will undoubtedly require academic partnerships with industry. Yet, the involvement of commercial entities in genomics research, or even speculation thereof, can erode public trust in science as well as create tension between research collaborators (Moodley and Kleinsmidt 2020; Critchley and Nicol 2009; Lee et al. 2019). Possibilities of commercialisation in genomics has recently brought to light the need to discuss upfront issues of benefit sharing and the ownership of patents and IP rights in genomics research in Africa (Munung and de Vries 2020; Andanda 2008). Finally, access to genomics medicine by populations in Africa; and the potential of genomics to aggravate the global health inequities remains a major concern (Green et al. 2020; Singer and Daar 2001).
The above ethical challenges have generated a need for an in-depth exploration, within the genomics research context, of how to equitably distribute power, knowledge and resources in ways that benefit all populations, especially those in low- and middle-income countries (LMICs). It has also led to calls for genomics governance that prioritises justice, solidarity and equity, instead of individual responsibility (Prainsack and Buyx 2013; Chen and Pang 2015; Gottweis 2005). Additionally, given the common good nature of genomics data, and that genomics research is unlikely to yield direct benefit to research participants, it has been suggested that principles such as solidarity and equity that emphasise peoples willingness to engage in activities for the common good, should be adopted as underlying moral principles for genomics governance (Chadwick and Berg 2001; Chadwick and Wilso 2004; Prainsack and Buyx 2013; HUGO Ethics Committee 2007; Hoedemaekers et al. 2007). This interest in solidarity, equity and collective risks and benefits is also seen as adopting a communitarian approach to genomics governance (Pálsson and Rabinow 2001; Chadwick 2011).
Solidarity is a key principle in Ubuntu (Mbiti 1968), an African communitarian ethic and theory of justice, raising interest about the extent to which Ubuntu could offer guidance for the governanceof global health research in general (Behrens 2013; Tangwa 1996) and genomics in particular (Pepper et al. 2018; Yakubu et al. 2018). In this paper, we present a conceptual analysis of how Ubuntu could inform genomics governance in Africa. We start by briefly introducing Ubuntu (and related African epistemologies) and its underlying principles. We then make suggestions for how the identified principles offer guidance for the governance of genomics research in Africa, by first, describing the macro-level ethical issues in genomics research in Africa and how each principle could be applied to derive guidance on addressing one or more of the ethical challenges. In doing so, we rely on our experiences within the H3Africa consortium (H3Africa Consortium 2014) both as bioethics researchers and as observers of how ethics and governance policies within the consortium have evolved. We conclude by presenting what we consider to be the limitations of Ubuntu as a moral skeleton for equity-oriented genomics governance in Africa.
Ubuntu and Related African Epistemologies and Ideologies
Ubuntu is a Bantu term for the philosophical approach by which many populations or ethnic in sub-Saharan Africa reflect and act towards each other (Sulamoyo 2010; Muwanga-Zake 2009). It is a moral theory for humanness (Metz 2007; Tutu 2012; Ramose 1999), a communitarian ethic (Biko 1987; Mbigi and Maree 1995; Mkhize 2008; Ramose 1999) and a theory of justice and fairness (Moeketsi 2014). Broadly, Ubuntu is an epistemology that begins with the community and then moves to the individual (Battle 2009; Callahan 2003; Du Toit 2005), and the individual though autonomous, is in a mediated relationship with their society (Ramose 1999; Dauda 2017) and has a responsibility to share resources with, and to support, other community members to achieve their full capacity (Nzimakwe 2014). While Ubuntu (a person is a person because of another person) is a term with origins in Southern African languages, the tenets of Ubuntu, which emphasise collective responsibility towards the common good and human flourishing, are expressed in other philosophies and ideologies (Fig 1) across sub-Saharan Africa (Rankopo and Diraditsile 2020; Mugumbate and Chereni 2019; Tosam 2014).
Fig 1.
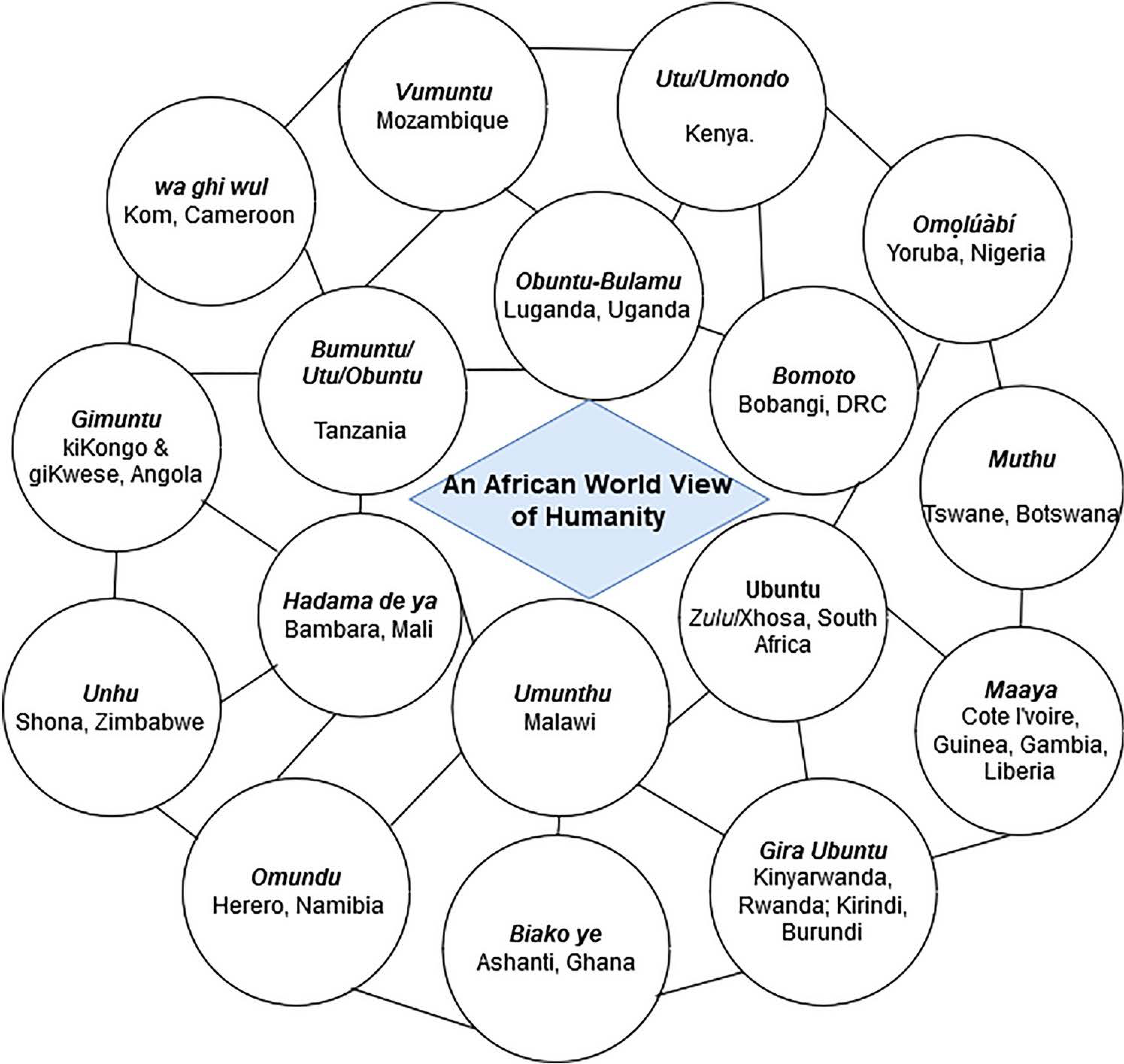
Ubuntu and related epistemologies across sub-Saharan Africa
Ubuntu: Principles, values and norms
The common principles, norms and values enshrined in the Ubuntu philosophy include: mutual caring, respect, solidarity, reciprocity, harmony, trust, shared responsibility, peer accountability, deliberative and consensus decision-making, inclusivity, dignity, generosity and compassion (Burgess 2017; Ramose 1999; Tavernaro-Haidarian 2018; Tutu 2012). Some of these principles/values suggest that Ubuntu could also broadly be categorised as the moral quality of a person (e.g. S/he has Ubuntu meaning s/he is friendly, generous, caring) or as a phenomenon–an ethic or philosophy (Gade 2012). It is the ethic, and its possible application to genomics governance, that will be the focus of this paper. As such, personal values such as caring, generosity, compassion and friendliness, while important, will not be discussed, although they arguably contribute to research ethics in general. Also, some of the personal values(in)directly contribute to the application of the Ubuntu ethics. Forexample, friendliness, empathy and harmony can be considered a demonstration of solidarity (Metz and Gaie 2010; Metz 2017). Figure 2 presents the principles of Ubuntu as identified in the literature(Burgess 2017; Ramose 1999; Tavernaro-Haidarian 2018; Tutu 2012). Whilst all these published accounts sometimes assign different names to the key principles, upon close reading we decided to capture the overarching principles of Ubuntu pertinent to governance in seven key principles and values, namely solidarity reciprocity, open sharing, inclusivity, deliberation and consensus, trust and accountability (see Fig 2). The principles of Ubuntu have also been adopted by some African ideologies of governance such as Ujamaa and Harambee. For example, in Ujamaa, Julius Nyerere imagines an African community that is based on deliberative governance (Nyerere 1968); while Harambee (Swahili for ‘let us pull together’) is a communal self-help ideology where the way of life is governed by norms of reciprocity, solidarity, equitable sharing of resources and mutual social obligations (Ng’ethe 1983). In the next section, we will highlight how these principles can inform genomics research governance.
Fig 2.

A representation of the principles and values espoused by Ubuntu and how they are centred on solidarity
Genomics governance through the lens of Ubuntu
Genomics governance requires navigating complex discussions around secondary uses of samples and data, benefit sharing, commercialisation, IPs and patents, equity in international research collaborations, and the contribution of genomics towards achieving global health equity. We briefly highlight how each Ubuntu principle (Figure 1) could contribute to the conceptualisation of genomics governance in Africa.
Solidarity
Solidarity is a key value in African communitarianism and is broadly construed as the realisation that one’s capability depends on others and that the common good should be pursued rather than the individual good (Wiredu 2000; Mbigi and Maree 1995). Group or communal solidarity is therefore a key aspect of Ubuntu and is central to the survival of a community (Mbigi and Maree 1995; Msila 2015). and is characterised by compassion, reciprocity, dignity, harmony and humanity to others (Nussbaum 2003) in ways that promote the flourishing of all members of a defined society, irrespective of their ideologies, viewpoints, responsibilities and personal values (Mbigi and Maree 1995; Nzimakwe 2014; Venter 2004). Applying the principle of solidarity to population genomics requires looking at what aspect or characteristic of ongoing genomics studies could prevent the health flourishing of one group over the other. For example, one of the end goals of genomics research is to foster precision medicine, be it at the population or personalised level, therefore, taking genomics variation across population groups into account, if genomics are limited to a specific population group, there is a chance that the outcome may not be translatable to other groups and this could in turn lead to a genomics divide between population groups or countries. Even so, within a given population group, there are concerns of access to the outcomes of genomics research and genomics medicine. The solidarity exemplified in Ubuntu is one that will require that global populations recognise these vulnerabilities and that it naturally motivates the scientific community to assume collective responsibility towards ensuring that genomics does not create a global health divide.
Oneof the majorfears in genomics hasbeenthat, ifpopulations insub-Saharan Africa arenot included in genomics research, they may not benefit from health innovations arising fromit (Popejoy and Fullerton 2016; H3Africa Consortium 2014). This observation sits alongside the possibility that being a hotspot for genetic diversity, the African continent offers a resource for advance genomics research and translation for the benefit of the global population. Solidarity will therefore demand global collective action to ensure representation of African populations in genomics studies so that they can benefit from precision medicine and other health advancements that may be the direct outcome of genomics. In practice, this will mean that global health funders should sponsor genomics studies in Africa (as an expression of solidarity) to ensure that the advances in genomics translate to health benefits for populations in Africa. On the other hand, populations in sub-Saharan Africa should be willing to consent to sample and data sharing for the common good.
There is also a parallel fear that representation of the African genome in the global genomics data pool is not sufficient for ensuring access to the benefits of genomics. Considering the high cost of genomics medicine, for example, there is a background concern that access to precision medicine will be a major challenge for populations in sub-Saharan Africa (Munung et al. 2018). Secondly, with limited capacity for genomics medicine in sub-Saharan Africa (Wonkam and Mayosi 2014), translating genetic research findings in the clinic may be a major challenge. Thirdly, some of major cases of morbidity and mortality in Sub-Saharan Africa are not mainly genetics related, but due to other social determinants of health raising questions of which health conditions or activities should be prioritised in genomics research in Africa (Munung et al. 2018; Wonkam and Mayosi 2014). Based on these concerns, one approach towards preventing a global genomics divide is to ensure that genomics studies in Africa 1) prioritise diseases that are major contributors to the disease burden in Africa;2) create an enabling environment for the clinical implementation of genomics medicine in Africa through supporting translational research for genomics medicine and 3) build capacity for genomics research and genomics medicine in Africa.
Open Sharing
Genomics research continues to advance policies that promote open science and research participants are often requested to consent to sample and data sharing. Broad consent – defined as consent for future unspecified use with process and content restrictions (Grady et al. 2015)– and tiered consent (Nembaware et al. 2019) allow for the re-use of samples and data in a way that promotes open science (Tindana and de Vries 2016). Data sharing has the advantage of expediting genetic research and innovation, and in some instances may substantially reduce the cost of research. While there is a scientific and ethical imperative to share genomic data generated as part of research, it must be done in ways that are non-exploitative, and of reciprocal benefits to all stakeholders. This is important as hesitancy to data sharing in Africa is marked by fears of exploitation of study populations and African researchers in global health research (Smith 2018; Munung et al. 2017). This is further compounded by limited capacity of African institutions, compared to their collaborators in high income countries (HICs), to fully and expeditiously analyse and translate genomics data (Helmy et al. 2016).
The African ethic of Ubuntu reflects a universal bond of open sharing (Broodryk 2002; Nzimakwe 2014) and to say that someone has Ubuntu is to refer to their selfless commitment to share what they have for the common good (Ramose 1999) and flourishing of all members in the community (Nussbaum 2003). Understood as such, the suggestion may be that Ubuntu’s principle of open sharing may broadly support principles of open science that the equitably sharing of resources such as data and samples.
Resources such as patents and intellectual property could impact on the even distribution of genomics innovation across nations (Cook-Deegan and Heaney 2010). Furthermore, current patent laws and market systems tend to favour bigger economies and where there the market/economy is weak, as is the case with most LMICs, the existing patent systems are unlikely to provide incentives for translation of genomics knowledge to products specific for use in those regions (Smith et al. 2004). This will mean that except there are intentional efforts to modify existing patents systems, health products that are an outcome of genomics may be largely accessible to persons living in HICs or to the privilege few in LMICs who can afford to pay for high cost genomics healthcare products or services. Solidarity and open sharing will require a global effort to adopt favourable licencing conditions that will facilitate low cost translation of genomics research.
Reciprocity
Reciprocity in African communitarianism is the awareness that human interactions are generally contingent upon mutual exchange whereby people continuously give and receive as part of daily life (Metz 2007). In Ubuntu ethics, reciprocity is seen as mutual aid whereby persons within a given community have an obligation to be responsive to the needs of others, not necessarily in terms of the exchange of goods but through one’s attitude to the community (Mkhize 2008; Metz 2007). In such societies, Reciprocity is forthrightly expressed in many African cultures as mutual aid where persons within a given community have the obligation to be responsive to the needs of others, not necessarily in terms of the exchange of goods but through one’s attitude to the community (Mkhize 2008). It is for this reason that many African cultures have an expression for the aphorism “the right arm washes the left arm and the left arm washes the right arm”. Julius Nyerere, for example, Captures reciprocity as such “In our traditional African society, we were individual within a community. We took care of the community, and the community took care of us. We neither needed nor wished to exploit our fellow men” (Nyerere 1968). Reciprocity, in the African worldview, is therefore about an obligation to act against social injustices such as exploitation.
Three types of relationships in genomics research therefore raise expectations of reciprocity, namely that between 1) researchers and study communities; 2) African researchers and their HIC collaborators and 3) African researchers and secondary users of samples and genetic data from Africa. In all three cases, expectations of reciprocity have been anchored in concerns around exploitation of African researchers and study populations (de Vries et al. 2015; Munung et al. 2017; Nienaber 2011).
Those who bear the risk of participating in genomics studies in Africa, appear to do so on the grounds that their samples and data will be used to find new solutions to diseases thataffect them. The principle of reciprocity will therefore require that these communities are provided access to the benefits of genomics studies, including access to genomic medicine and interventions. Equally, one of the factors that opens room for exploitation of Africa scientist is the limited capacity in most African institutions for the upstream use of samples and data, either for secondary analysis or for innovation purposes. This includes both human and infrastructural capacity as well as limited access to funding. Therefore when stakeholders with relatively more resources (infrastructural, human and financial) engage in a joint genomics research activity with African researchers, they have an obligation to ensure that as African researchers contribute towards ensuring that the African genetic diversity is captured for the benefit of all, they are equally supported with the needed resources to answer research questions of pertinence to them and their study populations. A third contention that pertains to exploitation is the sharing of benefits with study populations, either in terms of access to new interventions arising from genomics studies in Africa or financial benefits (where applicable). In as much as understanding human genetic diversity is important for advancing medicine and science, it is also important to highlight that genetic/genomic research is also commercially valuable. Therefore, issues of profits, patents, licensing and intellectual property will undoubtedly come to the fore especially at the discovery and translation stage. A communitarian perspective to the principle of reciprocity will support a collective approach to intellectual property/patents so as to enable equitable access to the outcome (innovation, services, profits) of genetic research in Africa. This is similar to arguments for benefit sharing ingrained in the idea that genetic information is both a common heritage and resource and therefore should be used for the benefit humankind irrespective of whether there are is existing optimal infrastructure and/or resources to support it use (HUGO Ethics Committee 2000; UNESCO 1997). In practice, this calls for detailing benefit sharing mechanisms in genomics projects in Africa.
Inclusivity
One of the most contested issues in genomics is how samples and data will be accessed for uses that are different from the original study including who makes decisions on access to data and samples (Langlois 2006; Upshur et al. 2007; Parker et al. 2009). Generally, the limited involvement of African researchers in decision making in global health research collaborations often create a sense of exploitation and lack of respect for African scientists, sometimes leading to a breakdown of trust between research collaborators (Munung et al. 2017; Tangwa 2017; Okeke 2016). Furthermore, there is the perception that decision-making processes in global health research collaborations can be unfair processes without and oftentimes HIC stakeholders tend to get the outcome they want at expense of LMIC stake holders or consensus with collaborators (Gautier et al. 2018). Researchers, however, are not the only stakeholders that should be included in decision making on secondary uses of samples and data or research priorities. Research participants, for example, should ideally be involved in decision-making on the uses of their samples and data (Upshur et al. 2007; Emerson et al. 2011) and journal editors sometimes request that authors provide information on where the data reported in publications could be accessed by other interested parties.
An Ubuntu approach to governance would ensure that the voices of sample and data providers, journal editors, researchers, funders, and other affected stakeholder groups are represented in decision-making on secondary uses of samples and data. This is because, in Ubuntu societies, inclusivity is considered to embody key aspects of good governance such as: trust, transparency, accountability and equality (Burgess 2017; Nzimakwe 2014; Shanyanana and Waghid 2016; Khomba et al. 2013). Two forms of inclusivity will be considered indispensable: representation of all affected stakeholder groups-formal representation); and the representation of the will of all stakeholder groups-substantive representation (Wiredu 2000; Shanyanana and Waghid 2016). Substantive representation is what is considered the critical component of legitimate decision-making in traditional African governance systems (Osabu-Kle 2000; Wiredu 2000; Horne 2004; Ramose 1999). The rationale is to minimise the effect of one group having a disproportionate influence on decision-making (Sesay 2014; Tavernaro-Haidarian 2018). However, this assumes that all stakeholders have equal powers (politically and resourcewise) in decision making structures. At a more global level, the decision-making field in genomics research is not level and many genomics research initiatives have struggled to balance the representation of different stakeholders in decision-making (Fusi et al. 2018; Lemke and Harris-Wai 2015).
A stakeholder group that has, in our view, been traditionally left out of genomics governance in Africa is the sample and data providers. By this we mean the research participants or biobank donors. In countries in the global north, there is growing consensus that sample providers group should be involved in decision making on access and secondary uses of samples and data (O’Doherty and Burgess 2009; Burgess 2014), and in some cases this has been either through representation of sample and data providers in data and biospecimen access committees or through public deliberations aimed at informing genomics policy. What Ubuntu contributes to the methodological challenges of representation of stakeholder groups in decision making, especially study communities, is its approach to inclusiveness, where the emphasis is not only on physical representation, albeit important, but on substantive representation - that is including the voices of study participants and this could be through public/patient consultation that is bidirectional in nature, similar to what occurs in community meetings e.g. Indaba ( Zulus, South Africa), Ama-ala (Igbo, Nigeria) and Durbar (Northern Ghana), allowing for participants not only to be recipients of expert information but as agents of change capable to contributing to discussions on emerging ethical or moral issues in genomics. This has been described as participatory consensus (Ayittey 2010) and has the power to build trust and strengthen the communal spirit (solidarity) within a society (Msila 2015).
Deliberative and consensus decision-making
Arguably, the ethical issues in genomics are likely to generate a plurality of views from the different genomics research stakeholders, depending on how each stakeholder group may be affected by a policy, action, or research practice. For example, while some studies have demonstrated that study participants are often willing to consent to future uses of samples and data, both for altruistic reasons (Mweemba et al. 2019) and when there is a plan for benefit sharing (Moodley et al. 2014), other studies have found reluctance by African researchers to share data and samples with other researchers (Bangani and Moyo 2019; Bezuidenhout 2019). If Ubuntu is used as a framework to support governance, then it will require that genomics initiatives openly invite these diverse opinions through deliberative and consensus-driven dialogue (Osabu-Kle 2000; Wiredu 2000, 2002). This is because “every person is regarded as a fountain of knowledge who has valuable things to contribute to society as a whole” (Blankenberg 1999).
In practice, this requires having open and deliberative discussions on the science and ethics of genomics to enable each stakeholder group to, at some point, acknowledge that while there may be disagreement on how certain ethical issues are perceived and should be addressed, there is some degree of awareness on the risk that it involves and there is consensus on how to approach each ethical concern. Such an approach allows for willing suspension of disagreement (Wiredu 2000), that is, though we differ in our views, we choose to unite for the good of the community. In this way, consensus is seen as an expression of solidarity. One of the pitfalls for deliberative processes however is that the tend to be more effective if the stakeholder groups involved all have some basic awareness of concepts in genomics and the risk and benefits thereof. Currently, there is limited genomic literacy amongst study participants, the general public and healthcare practitioners in Africa (Traore et al. 2015; Mboowa and Sserwadda 2019; Wonkam et al. 2006), suggesting that engaging the public and health care workers through deliberative processes will first require setting up initiatives that will improve their genetic literacy levels. More so, researchers will have to be transparent in discussing risks and benefits when they engage and provide information to stakeholder group with limited background knowledge of genomics and its potential risks and benefits. Secondly there is need to imagine and develop models of facilitating these deliberative processes to ensure that the diverse voices of all participants are captured and to identify when consensus has been reached on a policy or topic of interest.
Accountability
Data from genomics projects could be used for purposes different from that of the primary studies. At the time of enrolment into genomics studies, research participants are typically informed that no direct benefit will accrue to them as a result of their participation in the study but that by participating in the study they will be contributing to the advancement of science and medicine (Munung et al. 2016). In some cases, participants are informed that they could receive some individual results. Consent forms for genomics studies used in H3Africa, an African genomics research initiative for instance also tend to state conditions for which samples may or may not be used (Munung et al. 2016). Downstream, and in the interest of trust, it is important that participants are informed of how their samples and data have been used to advance the common good.
Accountability in Ubuntu places emphasis on engaging relevant stakeholders, not just as key informants but also as agents of change who are capable of addressing concerns and issues that affect their community (Burgess 2017; Ayittey 2010). This constitutes social accountability would require, for example, that scientists inform study communities of research outcomes, including how samples and data are being used to address the health needs of study communities, benefit sharing mechanisms, what research results (general or individual) mean and what study communities could do with the results. In the process, study participants should be able to share their views on how genomics studies could be strengthen or re-aligned to serve their health and research-related needs.
Mutual trust between collaborators and stakeholders
Generally, genomics research thrives on collaborative research networks and the sharing of samples and data. This is partly due statistical requirements for large sample sizes and diverse scientific expertise needed in genomics research (Kaye et al. 2009; Green et al. 2015). Therefore, samples and data from one project will often be shared with other researchers or institutions who may not have been involved in the collection of the samples. Therefore, the success of any genomics research and biobanking project in Africa will depend not only on the quality of samples collected or the researchers and institutions involved, but to a large extent on building and maintaining the trust and support of all stakeholders (Parker and Kwiatkowski 2016). For example, there are broad perceptions that the expertise and contributions of African partners involved in international collaborations are not recognised and that HIC partners are seen as self-sufficient collaborators (Parker and Kingori 2016). This is a call to recognise the interdependence of all stakeholders within a research collaboration and an acknowledgement that each is making a significant contribution to the success of the project (Munung et al. 2017), without which there may be a breakdown of trust, leading to refusal to participate in studies or to share samples and data. This could have severe implications for the sustainability of genomics studies in Africa.
Ubuntu is characterised by a system of mutual trust and respect and is thought of as a feature of a relation that is built over time, and enshrined in solidarity, reciprocity, and accountability (Venter 2004). Trust is gained when: 1) there is recognition of the contribution of all members of the community; 2) individuals demonstrate their commitment towards contributing to the flourishing of their community; 3) a person does not act opportunistically at the detriment of other members of their community (Mbigi and Maree 1995). This is usually achievable through long-term consistency in words and actions (Ting-Toomey, 2012). It calls for genomics research projects to recognise the interdependence of all stakeholders within a research collaboration and to acknowledge that each is making a significant contribution to the success of the project. It requires keeping promises made either to collaborators or to research participants during the consent process and public engagement activities. It also implies having procedures for recognising contributions of all participating researchers, such as shared authorship, joint ownership of patents and recognising the expertise of each researcher.
Potential objections to Ubuntu as a moral compass for genomics governance in Africa
Ubuntu is a moral theory or communitarian ethic that has its origins in Bantu cultures in southern Africa(Metz 2007). As such, we felt it made sense to explore how its application could inform the governance of genomics research in Africa. However, it could be asserted that Ubuntu is specific to sub-Saharan Africa and thus less relevant outside Bantu communities. As a result, some global health and genomics stakeholders may not subscribe to some of the principles espoused in Ubuntu. While acknowledging that different African moral philosophies exist (Kagame 1976; Verharen 2008; Wiredu 2006) and that the term Ubuntu is used predominantly in South Africa, there are equivalent philosophies or concepts (Fig 1) across a range of sub-Saharan African communities (Dauda 2017; Metz 2007; Oppenheim 2012; Ramose 1999; Tosam 2014). Also, Ubuntu principles/values are shared by population groups across and beyond sub-Saharan Africa (Fig 1). It is therefore a value system that is, arguably, globalisable (Tangwa 2019; Etieyibo 2017). At a minimum,, where there are diverse views on the foundational theories and principles that should inform the governance of genomics research, exploration of each and dialogue should be encouraged (Chimakonam 2017).
Conclusion
Genomics research in Africa is animated by questions of justice and governance, most of which are linked to differences in research and economic power between stakeholder groups; a history of exploitation of African researchers and study populations; and access to the promises of genomics medicine by populations in Africa. Ubuntu is an both an ethic and a theory of justice that represents an African understanding of equity. It emphasises a way of being that is grounded in principles of solidarity, reciprocity, open sharing, mutual trust and accountability. These different principles are key in addressing macro-level justice concerns in genomics research, not just in Africa but globally. We are of the opinion that some of these principles can easily be transferable to the governance of global health in general. More conceptual and empirical research on these different principles is required to provide in-depth clarity on how they may be actualised in global health research and genomics research.
In this conceptual study, we identified seven Ubuntu principle that speak to equity and fairness and have applied them to generate a framework for an inclusive, forward-looking and ethical governance of genomics research in Africa (Table 1). The framework sees study communities as key partners and contributors to decision-making on the use of their samples and data. It also promotes a genomics governance model that is rooted in solidarity and where no stakeholder group should hoard genetic resources (data, samples etc) or products (IPs, patents, publications etc) for their personal gain at the expense of others. The framework recognises the interdependence of all stakeholder groups and acknowledge that each is making a significant contribution to preventing a global genomics divide.
Table 1.
Summary of Ubuntu Principles and how the apply to genomics governance in Africa
| Principle | Description/Definition | Potential Application in Genomics Research |
|---|---|---|
| Solidarity | Recognition of the interdependence of members involved in a joint activity. | Global collective action to ensure that African populations are represented in genomics studies and that these studies 1) prioritise health conditions that contribute to the disease burden in Africa and 2) build capacity for genomics and genomics medicine Populations in Africa should contribute samples and data for global genomics studies by consenting for data sharing All stakeholders should share experiences, knowledge, and resources for the common good |
| Open Sharing | Ubuntu embodies the philosophical concept of an open society whereby community members demonstrate a selfless commitment to share what they have for the benefit of their community | No stakeholder group should hoard genetic resources (data, samples) or products (IPs, patents, publications etc) for their personal gain at the expense of others Genomics projects should share samples and data with other researchers in ways that allow for maximum use of samples and data towards improving health of populations in Africa IPs and patent arising from the use of genomic data in Africa should not create access barriers to precision medicine by populations in Africa African researchers should share research data for the advancement of science and this contribution should be acknowledged by secondary users of the data for example in research publications, patents, and the development of new tools |
| Reciprocity | Human interactions are contingent upon mutual exchange Persons within a community have an obligation to be responsive to the needs of others |
Genomics initiatives should define a benefit sharing plan that recognises the collective action of all stakeholder groups. communities should be provided access to the benefits of genomics studies including access to genomic health care interventions developed using data from the communities. African researchers should be supported to make maximum use of the samples and genetic data from Africa |
| Inclusivity | Inclusivity is consciously encouraged in decision-making processes. Two forms of inclusivity are considered indispensable: representation of all stakeholder groups (formal representation); and the representation of the will of all stakeholder groups (substantive representation). | The voices of all stakeholders should be included in decision-making mechanisms. Efforts should be made to include vulnerable populations and stakeholder groups that may be affected by a decision but typically left out in decision-making processes (sample provid ers, African researchers, junior researchers) |
| Deliberative and consensus decision-making | Participatory decision-making characterised by, consensus, substantive representation, and willing suspension of disagreement. | Decision making processes should be structured in such a way that no stakeholder group affected is able to disproportionately influence the final decision (attention should be paid to the motivations of ethics experts; funders, researchers and other powerful stakeholders) and final outcome should be by consensus Public/patient engagement activities that adopt deliberative processes are required when developing ethics policies for genomics projects in Africa |
| Accountability | Engaging with relevant stakeholders, not just as key informants but also as agents of change capable of addressing concerns and issues that affect their community. | Researchers have an obligation to feedback the outcome of research projects to study communities, including how samples and data have been, or are being, used to address the health needs of study communities. Study communities and research participants should be informed of how their samples and data have been used and this should be done in ways that allow research participants or study communities to provide feedback to researchers |
| Mutual Trust | Trust is fostered through respect and recognition of the contribution of all members of the community and can be achieved through demonstration of long-term consistency in words and actions | Genomics projects should recognise the interdependence of all stakeholders and acknowledge that each is making a significant contribution to the success of the project through for example shared authorship, joint ownership of patents and recognising the expertise of each researcher. All stakeholders should keep to promises made either to other stakeholders or to research participants during the consent process/ public engagement activities. |
Acknowledgements
Nchangwi S. Munung received a studentship from the “Stigma in African Genomics” study funded by the NIH(U01HG008226; PI: Jantina de Vries) to conduct this study and is currently supported by the Sickle Africa Data Coordinating Centre (N.I.H. grant no: U24HL135600). Jantina de Vries is currently supported by the IFGENERA Centre, which receives funding from the National Human Genome Research Institute of the National Institutes of Health under Award Number U54HG009790. Bridget Pratt is currently supported by a University of Melbourne R Douglas Wright Research Fellowship and a Faculty of Medicine Dentistry and Health Sciences Bridging Fellowship.
Footnotes
Publisher's Disclaimer: This Author Accepted Manuscript is a PDF file of an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
References
- Andanda PA 2008. Human-Tissue-Related Inventions: Ownership and Intellectual Property Rights in International Collaborative Research in Developing Countries. Journal of Medical Ethics 34 (3):171–179. [DOI] [PubMed] [Google Scholar]
- George Ayittey B. N. 2010. Traditional Institutions and the State of Accountability in Africa. Social Research 77 (4):1183–1210. [Google Scholar]
- Bangani Siviwe, and Moyo Mathew. 2019. Data Sharing Practices among Researchers at South African Universities. Data Science Journal 18 (1). [Google Scholar]
- Battle M 2009. Ubuntu: I in You and You in Me. New York: Seabury Books. [Google Scholar]
- Behrens KG 2013. Towards an indigenous African bioethics. South African Journal of Bioethics and Law 6:32+. [Google Scholar]
- Louise Bezuidenhout. 2019. To share or not to share: Incentivizing data sharing in life science communities. Developing World Bioethics 19 (1):18–24. doi: 10.1111/dewb.12183. [DOI] [PubMed] [Google Scholar]
- Biko S 1987. Some African Cultural Concepts. In I Write what I Like: A Selection of His Writings, ed. Stubbs A, 40–47. Heinemann. [Google Scholar]
- Ngaire Blankenberg. 1999. In search of a real freedom: Ubuntu and the media. Critical Arts 13 (2):42–65. doi: 10.1080/02560049985310121. [DOI] [Google Scholar]
- Broodryk J 2002. Ubuntu: Life Lessons from Africa. South Africa: Ubuntu School of Philosophy. [Google Scholar]
- Burgess Gloria J. 2017. Unpacking Inclusivity: Lessons from Ubuntu Leadership. In Breaking the Zero-Sum Game (Building Leadership Bridges), 379–394. Building Leadership Bridges: Emerald Publishing Limited. [Google Scholar]
- Burgess MM 2014. From ťrust us’ to participa tory governance: Deliberative publics and science policy. Public Underst Sci 23 (1):48–52. doi: 10.1177/0963662512472160. [DOI] [PubMed] [Google Scholar]
- Callahan D 2003. Individual good and common good: a communitarian approach to bioethics. Perspect Biol Med 46 (4):496–507. [DOI] [PubMed] [Google Scholar]
- Chadwick R, and Berg K 2001. Solidarity and equity: new ethical frameworks for genetic databases. Nat Rev Genet 2(4):318–321. doi: 10.1038/35066094. [DOI] [PubMed] [Google Scholar]
- Chadwick R, and Wilso S 2004. Genomic databases as global public goods? Res Publica 10 (2):123–134. [DOI] [PubMed] [Google Scholar]
- Chadwick Ruth. 2011. The communitarian turn: myth or reality? Cambridge Q. Healthcare Ethics 20:546. [DOI] [PubMed] [Google Scholar]
- Haidan Chen, and Pang Tikki. 2015. A call for global governance of biobanks. Bull World Health Organ 93 (2):113–117. doi: 10.2471/BLT.14.138420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chimakonam Jonathan O. 2017. African philosophy and global epistemic injustice. Journal of Global Ethics 13 (2):120–137. doi: 10.1080/17449626.2017.1364660. [DOI] [Google Scholar]
- Robert Cook-Deegan, and Heaney Christopher. 2010. Patents in genomics and human genetics. Annu Rev Genomics Hum Genet 11:383–425. doi: 10.1146/annurev-genom-082509-141811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Critchley Christine R., and Nicol Dianne. 2009. Understanding the impact of commercialization on public support for scientific research: Is it about the funding source or the organization conducting the research? Public Understanding of Science 20 (3):347–366. doi: 10.1177/0963662509346910. [DOI] [PubMed] [Google Scholar]
- Dauda Bola. 2017. African humanism and Ethics: The cases of Ubuntu and Omoluwabi. In The Palgrave Handbook of African Philosophy, eds. Afolayan A, and Falola T, 475–491. USA: Palgrave Macmillan [Google Scholar]
- de Vries J, Tindana P, Littler K, Ramsay M, Rotimi C, Abayomi A, Mulder N, and Mayosi BM 2015. The H3Africa policy framework: negotiating fairness in genomics. Trends Genet 31 (3):117–119. doi: 10.1016/j.tig.2014.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dowdeswell Elizabeth, Daar Abdallah S., Acharya Tara, and Singer Peter A. 2006. Realising the promise of genomics: exploring governance. International Journal of Biotechnology 8 (1–2):132–141. doi: 10.1504/IJBT.2006.008969. [DOI] [Google Scholar]
- Du Toit C 2005. Technoscience and the Integrity of Personhood in Africa and the West: Facing our Technoscientific Environment. HTS 61 (3):829–860. [Google Scholar]
- Emerson Claudia I., Singer Peter A., and Upshur Ross E. G. 2011. Access and use of human tissues from the developing world: ethical challenges and a way forward using a tissue trust. BMC Medical Ethics 12 (1):2. doi: 10.1186/1472-6939-12-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwin Etieyibo. 2017. Ubuntu, Cosmopolitanism, and Distribution of Natural Resources. Philosophical Papers 46 (1):139–162. doi: 10.1080/05568641.2017.1295616. [DOI] [Google Scholar]
- Fusi F, Manzella D, Louafi S, and Welch E 2018. Building Global Genomics Initiatives and Enabling Data Sharing: Insights from Multiple Case Studies. Omics 22 (4):237–247. doi: 10.1089/omi.2017.0214. [DOI] [PubMed] [Google Scholar]
- Gade Christian B. N. 2012. What is Ubuntu,? Different Interpretations among South Africans of African Descent. South African Journal of Philosophy 31 (3):484–503. doi: 10.1080/02580136.2012.10751789. [DOI] [Google Scholar]
- Lara Gautier, Sieleunou Isidore, and Kalolo Albino. 2018. Deconstructing the notion of “global health research partnerships” across Northern and African contexts. BMC Medical Ethics 19 (1):49. doi: 10.1186/s12910-018-0280-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gottweis H 2005. Governing genomics in the 21st century: between risk and uncertainty. New Genet Soc 24 (2):175–193. doi: 10.1080/14636770500184818. [DOI] [PubMed] [Google Scholar]
- Grady C, Eckstein L, Berkman B, Brock D, Cook-Deegan R, Fullerton SM, Greely H et al. 2015. Broad Consent for Research With Biological Samples: Workshop Conclusions. Am J Bioeth 15 (9):34–42. doi: 10.1080/15265161.2015.1062162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green AK, Reeder-Hayes KE, Corty RW, Basch E, Milowsky MI, Dusetzina SB, Bennett AV, and Wood WA 2015. The project data sphere initiative: accelerating cancer research by sharing data. Oncologist 20 (5):464–e420. doi: 10.1634/theoncologist.2014-0431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green Eric D., Gunter Chris, Biesecker Leslie G., Valentina Di Francesco Carla L. Easter, Feingold Elise A., Felsenfeld Adam L. et al. 2020. Strategic vision for improving human health at The Forefront of Genomics. Nature 586 (7831):683–692. doi: 10.1038/s41586-020-2817-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- H3Africa Consortium. 2014. Enabling the genomic revolution in Africa. Science 344 (6190):1346–1348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohamed Helmy, Awad Mohamed, and Mosa Kareem A. 2016. Limited resources of genome sequencing in developing countries: Challenges and solutions. Applied & Translational Genomics 9:15–19. doi: 10.1016/j.atg.2016.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogeer Hoedemaekers, Gordijn Bert, and Pijnenburg Martien. 2007. Solidarity and Justice as Guiding Principles in Genomic Research. Bioethics 21 (6):342–350. doi: 10.1111/j.1467-8519.2007.00562.x. [DOI] [PubMed] [Google Scholar]
- Horne DL 2004. Meeting Ma’at: The African Centered Handbook for Conducting Meetings. Bloomington, Indiana: AuthorHouse. [Google Scholar]
- HUGO Ethics Committee. 2000. HUGO urges genetic benefit-sharing. Community Genet 3 (2):88–92. doi: 10.1159/000051110. [DOI] [PubMed] [Google Scholar]
- HUGO Ethics Committee. 2007. HUGO Statement on Pharmacogenomics (PGx): Solidarity, Equity and Governance. Genomics, society, and policy 3 (1):44. doi: 10.1186/1746-5354-3-1-44. [DOI] [Google Scholar]
- Alexis Kagame. 1976. La philosophie bantu comparée. Paris: Présence Africaine. [Google Scholar]
- Kaye J, Heeney C, Hawkins N, de Vries J, and Boddington P 2009. Data sharing in genomics--re-shaping scientific practice. Nat Rev Genet 10 (5):331–335. doi: 10.1038/nrg2573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kamwachale Khomba James, Bakuwa Rhoda C, and Cindy Kangaude-Ulaya Ella. 2013. Shaping business ethics and corporate governance: An inclusive African Ubuntu Philosophy. Global Journal of Management And Business Research 13 (5):30–42. [Google Scholar]
- Adèle Langlois. 2006. The governance of genomic information: will it come of age? Genomics, society, and policy 2 (3):49–63. doi: 10.1186/1746-5354-2-3-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandra Lee S. J., Cho Mildred K., Kraft Stephanie A., Varsava Nina, Gillespie Katie, Ormond Kelly E., Wilfond Benjamin S., and Magnus David. 2019. “I don’t want to be Henrietta Lacks”: diverse patient perspectives on donating biospecimens for precision medicine research. Genetics in Medicine 21 (1):107–113. doi: 10.1038/s41436-018-0032-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lemke Amy A., and Harris-Wai Julie N. 2015. Stakeholder engagement in policy development: challenges and opportunities for human genomics. Genet Med 17 (12):949–957. doi: 10.1038/gim.2015.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deborah Mascalzoni, Hicks Andrew, Pramstaller Peter, and Wjst Matthias. 2008. Informed Consent in the Genomics Era. PLoS Medicine 5 (9):e192. doi: 10.1371/journal.pmed.0050192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mbigi L, and Maree J 1995. Ubuntu, the spirit of African transformation management. California: Knowledge Resources. [Google Scholar]
- Mbiti John S. 1968. African Religions and Philosophy. London: Heinemann. [Google Scholar]
- Gerald Mboowa, and Sserwadda Ivan. 2019. Role of genomics literacy in reducing the burden of common genetic diseases in Africa. Molecular genetics & genomic medicine 7 (7):e00776–e00776. doi: 10.1002/mgg3.776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGuire Amy L., and Beskow Laura M. 2010. Informed consent in genomics and genetic research. Annu Rev Genomics Hum Genet 11:361–381. doi: 10.1146/annurev-genom-082509-141711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thaddeus Metz. 2007. Toward an African Moral Theory. Journal of Political Philosophy 15 (3):321–341. doi: 10.1111/j.1467-9760.2007.00280.x. [DOI] [Google Scholar]
- Thaddeus Metz. 2017. Replacing Development: An Afro-Communal Approach to Global Justice. Philosophical Papers 46 (1):111–137. doi: 10.1080/05568641.2017.1295627. [DOI] [Google Scholar]
- Metz Thaddeus, and Gaie Joseph B. R. 2010. The African ethic of Ubuntu/Botho: implications for research on morality. Journal of Moral Education 39 (3):273–290. doi: 10.1080/03057240.2010.497609. [DOI] [Google Scholar]
- Nhlanhla Mkhize. 2008. Ubuntu and harmony: an African approach to morality and ethics. In Persons in Community: African Ethics in a Global Culture, ed. Nicolson Ronald, 25–44. Pietermaritzburg: University of Kwazulu-Natal Press. [Google Scholar]
- Letseka Moeketsi. 2014. Ubuntu and Justice as Fairness. Mediterranean Journal of Social Sciences 5 (9). [Google Scholar]
- Keymanthri Moodley, and Kleinsmidt Anita. 2020. Allegations of misuse of African DNA in the UK: Will data protection legislation in South Africa be sufficient to prevent a recurrence? Developing World Bioethics n/a (n/a). doi: 10.1111/dewb.12277. [DOI] [PubMed] [Google Scholar]
- Moodley Keymanthri, Sibanda Nomathemba, February Kelsey, and Rossouw Theresa. 2014. “It’s my blood”: ethical complexities in theuse, storage and export of biological samples: perspectives from South African research participants. BMC Medical Ethics 15 (1):4. doi: 10.1186/1472-6939-15-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vuyusile Msila. 2015. UBUNTU: Shaping the current workplace with (African) wisdom. Randburg, South Africa: Knowres Publishing. [Google Scholar]
- Mugumbate J, and Chereni A 2019. Using African ubuntu theory in social work with children in Zimbabwe.
- Munung NS, Mayosi BM, and de Vries J 2018. Genomics research in Africa and its impact on global health: insights from African researchers. Global Health, Epidemiology and Genomics 3:e12. doi: 10.1017/gheg.2018.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Syntia Munung Nchangwi, and de Vries Jantina. 2020. Benefit Sharing for Human Genomics Research: Awareness and Expectations of Genomics Researchers in Sub-Saharan Africa. Ethics & Human Research 42 (6):14–20. doi: 10.1002/eahr.500069. [DOI] [PubMed] [Google Scholar]
- Nchangwi Syntia Munung, Marshall Patricia, Campbell Megan, Littler Katherine, Masiye Francis, Ouwe-Missi-Oukem-Boyer Odile, Seeley Janet, Stein DJ, Tindana Paulina, and de Vries Jantina. 2016. Obtaining informed consent for genomics research in Africa: analysis of H3Africa consent documents. Journal of Medical Ethics 42 (2):132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Syntia Munung Nchangwi, Mayosi Bongani M., and de Vries Jantina. 2017. Equity in international health research collaborations in Africa: Perceptions and expectations of African researchers. PLoS ONE 12 (10):e0186237. doi: 10.1371/journal.pone.0186237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muwanga-Zake JWF 2009. Building bridges across knowledge systems: Ubuntu and participative research paradigms in Bantu communities. Discourse: Studies in the Cultural Politics of Education 30 (4):413–426. doi: 10.1080/01596300903237198. [DOI] [Google Scholar]
- Oliver Mweemba, Musuku John, Mayosi Bongani M., Parker Michael, Rutakumwa Rwamahe, Seeley Janet, Tindana Paulina, and De Vries Jantina. 2019. Use of broad consent and related procedures in genomics research: Perspectives from research participants in the Genetics of Rheumatic Heart Disease (RHDGen) studyina University Teaching Hospital in Zambia. Global Bioethics:1–16. doi: 10.1080/11287462.2019.1592868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nembaware V, Johnston K, Diallo AA, Kotze MJ, Matimba A, Moodley K, Tangwa GB, Torrorey-Sawe R, and Tiffin N 2019. A framework for tiered informed consent for health genomic research in Africa. Nat Genet 51 (11):1566–1571. doi: 10.1038/s41588-019-0520-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Njuguna Ng’ethe. 1983. Politics, Ideology and the Underprivileged: The Origins and Nature of the Harambee Phenomenon in Kenya. Journal of Eastern African Research & Development 13:150–170. [Google Scholar]
- Annelize Nienaber. 2011. Consent to and authorisation of the export and use of human biological specimens for future research — perspectives from three African countries. The Comparative and International Law Journal of Southern Africa 44 (2):225–254. [Google Scholar]
- Nussbaum Barbara. 2003. Ubuntu: Reflections of a South African on our common humanity. Reflections: The SoL Journal 4 (4):21–26. [Google Scholar]
- Nyerere JK 1968. Ujamaa [engl.] Essays on socialism. Oxford University Press. [Google Scholar]
- Nzimakwe. 2014. Practising Ubuntu and leadership for good governance: the South African and continental dialogue. African Journal of Public Affairs 7 (4):30–41. [Google Scholar]
- O’Doherty KC, and Burgess MM 2009. Engaging the public on biobanks: outcomes of the BC biobank deliberation. Public Health Genomics 12 (4):203–215. doi: 10.1159/000167801. [DOI] [PubMed] [Google Scholar]
- Okeke Iruka N. 2016. African biomedical scientists and the promises of “big science”. Canadian Journal of African Studies / Revue canadienne des études africaines 50 (3):455–478. doi: 10.1080/00083968.2016.1266677. [DOI] [Google Scholar]
- Oppenheim E. Claire 2012. Nelson Mandela and the Power of Ubuntu. Religions 3 (2). doi: 10.3390/rel3020369. [DOI] [Google Scholar]
- Osabu-Kle T. Daniel 2000. Compatible Cultural Democracy:The Key to Development in Africa. University of Toronto Press. [Google Scholar]
- Gísli Pálsson, and Rabinow Paul. 2001. The Icelandic genome debate. Trends Biotechnol 19 (5):166–171. [DOI] [PubMed] [Google Scholar]
- Parker Michael, Bull Susan J., Jantina de Vries Tsiri Agbenyega, Doumbo Ogobara K., and Kwiatkowski Dominic P. 2009. Ethical Data Release in Genome-Wide Association Studies in Developing Countries. PLoS Medicine 6 (11):e1000143. doi: 10.1371/journal.pmed.1000143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parker Michael, and Kingori Patricia. 2016. Good and Bad Research Collaborations: Researchers’ Views on Science and Ethics in Global Health Research. PLOS ONE 11 (10):e0163579. doi: 10.1371/journal.pone.0163579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michael Parker, and Kwiatkowski Dominic P. 2016. The ethics of sustainable genomic research in Africa. Genome Biology 17 (1):44. doi: 10.1186/s13059-016-0914-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pepper Michael S., Dandara Collet, Jantina de Vries Amaboo Dhai, Labuschaigne Melodie, Mnyongani Freddy, Moodley Keymanthri et al. 2018. ASSAf consensus study on the ethical, legal and social implications of genetics and genomics in South Africa. South African Journalof Science 114 (11–12):1–3. doi:doi: 10.17159/sajs.2018/a0302. [DOI] [Google Scholar]
- Popejoy AB, and Fullerton SM 2016. Genomics is failing on diversity. Nature 538 (7624):161–164. doi: 10.1038/538161a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prainsack B, and Buyx A 2013. A solidarity-based approach to the governance of research biobanks. Med Law Rev 21 (1):71–91. doi: 10.1093/medlaw/fws040. [DOI] [PubMed] [Google Scholar]
- Ramose Mogobe B. 1999. African Philosophy Through Ubuntu. Indiana University: Mond Books. [Google Scholar]
- Rankopo J Morena, and Diraditsile Kabo. 2020. The interface between Botho and social work practice in Botswana: towards Afrocentric models. African Journal of Social Work 10 (1):1–4. [Google Scholar]
- Amadu Sesay. 2014. African Governance Systems in the Pre-and Post-Independence Periods: Enduring Lessons and Opportunities for Youth in Africa. Johannesburg: The Mandela Institute for Development Studies. [Google Scholar]
- Rachel Ndinelao Shanyanana, and Waghid Yusef. 2016. Reconceptualizing ubuntu as inclusion in African higher education: towards equalization of voice. Knowledge Cultures 4 (4):104–120. [Google Scholar]
- Singer Peter A., and Daar Abdallah S. 2001. Harnessing Genomics and Biotechnology to Improve Global Health Equity. Science 294 (5540):87. [DOI] [PubMed] [Google Scholar]
- James Smith. 2018. Parasitic and parachute research in global health. The Lancet Global Health 6 (8):e838. doi: 10.1016/S2214-109X(18)30315-2. [DOI] [PubMed] [Google Scholar]
- Smith RD, Thorsteinsdottir H, Daar AS, Gold ER, and Singers PA 2004. Genomics knowledge and equity: a global public goods perspective of the patent system. Bull World Health Organ 82 (5):385–389. [PMC free article] [PubMed] [Google Scholar]
- Stark Zornitza, Dolman Lena, Manolio Teri A., Ozenberger Brad, Hill Sue L., Caulfied Mark J., Levy Yves et al. 2019. Integrating Genomics into Healthcare: A Global Responsibility. The American Journal of Human Genetics 104 (1):13–20. doi: 10.1016/j.ajhg.2018.11.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dalitso Sulamoyo. 2010. "I Am Because We Are": Ubuntu as a Cultural Strategy for OD and Change in Sub-Saharan Africa. Organization Development Journal 28 (4):41–51. [Google Scholar]
- Tangwa GB. 2019. Bioethics and Ubuntu, The transformative global potential of an African concept. In The Tenacity of Truthfulness: Philosophical Essays in Honour of Mogobe Bernard Ramose, eds. Lauer Helen, and Yitah Helen, 239–249. Pretoria: EARS Publishing Company. [Google Scholar]
- Tangwa Godfrey B. 1996. Bioethics: An African Perspective. Bioethics 10 (3):183–200. doi: 10.1111/j.1467-8519.1996.tb00118.x. [DOI] [PubMed] [Google Scholar]
- Tangwa B. Godfrey 2017. Giving voice to African thought in medical research ethics. Theoretical Medicine and Bioethics 38 (2):101–110. doi: 10.1007/s11017-017-9402-3. [DOI] [PubMed] [Google Scholar]
- Tavernaro-Haidarian L 2018. A Relational Model of Public Discourse: The African Philosophy of Ubuntu. New York: Routledge. [Google Scholar]
- Tindana P, and de Vries J 2016. Broad Consent for Genomic Research and Biobanking: Perspectives from Low- and Middle-Income Countries. Annu Rev Genomics Hum Genet 17:375–393. doi: 10.1146/annurev-genom-083115-022456. [DOI] [PubMed] [Google Scholar]
- Tosam MJ 2014. The Relevance of Kom Ethics to African Development. International Journal of Philosophy. 2 (3):36–47. doi: 10.11648/j.ijp.20140203.12. [DOI] [Google Scholar]
- Traore K, Bull S, Niare A, Konate S, Thera MA, Kwiatkowski D, Parker M, and Doumbo OK 2015. Understandings of genomic research in developing countries: a qualitative study of the views of MalariaGEN participants in Mali. BMC Med Ethics 16:42. doi: 10.1186/s12910-015-0035-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Desmond Tutu. 2012. No future without forgiveness. Random House. [Google Scholar]
- UNESCO. 1997. Universal Declaration on the Human Genome and Human Rights United Nations Education and Scientific Council.
- Upshur Ross E. G., Lavery James V., and Tindana Paulina O. 2007. Taking tissue seriously means taking communities seriously. BMC Medical Ethics 8 (1):11. doi: 10.1186/1472-6939-8-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elza Venter. 2004. The Notion of Ubuntu and Communalism in African Educational Discourse. Studies in Philosophy and Education 23 (2):149–160. doi: 10.1023/B:SPED.0000024428.29295.03. [DOI] [Google Scholar]
- Charles Verharen. 2008. Comparing Oromo and ancient Egyptian philosophy. Journal of Oromo Studies 15 (2):1–32. [Google Scholar]
- Kwasi Wiredu. 2000. Democracy and Consensus in African Traditional Politics: A Plea for a Non-party Polity Polylog 2. [Google Scholar]
- Kwasi Wiredu. 2002. The moral foundations of an African culture. In Philosophy From Africa: A Text with Readings, eds. Coetzee PH, and Roux APJ, 287. Oxford University Press. [Google Scholar]
- Kwasi Wiredu. 2006. A Companion to African Philosophy. A Companion to African Philosophy. Oxford: Blackwell Publishing Limited. [Google Scholar]
- Wonkam A, Njamnshi AK, and Angwafo FF 3rd. 2006. Knowledge and attitudes concerning medical genetics amongst physicians and medical students in Cameroon (sub-Saharan Africa). Genet Med 8 (6):331–338. doi:10.109701.gim.0000223542.97262.21. [DOI] [PubMed] [Google Scholar]
- Ambroise Wonkam, and Mayosi Bongani M. 2014. Genomic medicine in Africa: promise, problems and prospects. Genome Medicine 6 (2):11. doi: 10.1186/gm528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yakubu A, Tindana P, Matimba A, Littler K, Munung NS, Madden E, Staunton C, and De Vries J. 2018. Model framework for governance of genomic research and biobanking in Africa - a content description [version 1; referees: awaiting peer review]. AAS Open Res 1 (13). [DOI] [PMC free article] [PubMed] [Google Scholar]


