1.0. INTRODUCTION
The World Health Organization defined burnout as a syndrome resulting from chronic workplace stressors which have not been managed.1 Over the last two decades, researchers have found that burnout is prevalent among clinicians and negatively impacts quality of care and patient outcomes within the acute care setting.2,3 In a recent study, 44% of cardiologists and 50% of neurologist experience burnout.4 The high prevalence of burnout is concerning because burnt-out clinicians are more likely to report job stress and dissatisfaction, fatigue, and irritability.5,6 Furthermore, clinician burnout negatively affects patients as it is related with urinary tract and surgical site infections,7 poor quality of care,8 and medical errors thereby, compromising patient safety.2
Despite the adverse outcomes related to burnout, most studies that currently exist are focused on clinicians in the acute care settings.7,9,10 This is a limitation because a significant portion of health care is delivered in primary care settings by primary care providers (PCPs) who are physicians, physician assistants, and nurse practitioners (NPs),11 and so studies conducted in the acute care setting cannot be generalized to primary care. Of the studies investigating burnout among PCPs, most explore physician burnout.5,12,13 Some of these researchers found that 37% of primary care physicians were burnt-out,12 which is concerning since burnt-out physicians are also more likely to deliver suboptimal patient care.14 However, no study author has reported the prevalence and outcomes related to primary care NP burnout which is a limitation because compared to all NPs, 69% of NPs currently deliver primary care services to patients.15
A dearth of research exists on the relationship between primary care NP burnout and the practice environment. Poor practice environments are a major contributor to burnout in the primary care setting,16 and researchers have reported challenges within the practice environment that are unique to NPs.17,18 For example, NPs in poor environments have inadequate support from administrators, suboptimal communication with staff, limited autonomy,18 and such organizational challenges may predispose NPs to burnout and impact the quality of care they deliver to patients. In another study, 46.1% of NPs were working in a poor practice environment19 which is concerning because working in poor practice environments can lead to burnout5,20 and poor patient outcomes.20,21 However, NPs working in a good environment were more likely to incorporate patient preferences into care delivery compared to NPs in either mixed or poor environments.19 Since the environment where clinicians deliver care has long been shown to affect provider outcomes and patient care,5,20 it is plausible that working in a poor practice environment may lead to NP burnout and perceptions of lower care quality, however, further investigation is needed. Thus, in this study, we (Aim 1) seek to determine whether NPs experiencing burnout will be less likely to perceive delivering high quality of care compared to NPs not experiencing burnout, and (Aim 2) we investigate whether the practice environment moderates the relationship between burnout and perceptions of care quality.
2.0. METHODOLGY
2.1. Conceptual frameworks
Aim 1 of our study was informed by the Clinician Well-Being and Resilience model which exemplifies the relationship between factors contributing to clinician burnout and outcomes of burnout such as compromised clinician well-being, clinician-patient relationships, and patient well-being.22 We adapted the conceptual model to display the relationship between NP demographics, practice characteristics (i.e., hours of operation, practice size, and type of practice), burnout, and perceptions of care quality (Figure 1). For Aim 1, we hypothesized that NPs experiencing burnout will be less likely to perceive delivering high quality of care compared to NPs not experiencing burnout.
Figure 1.
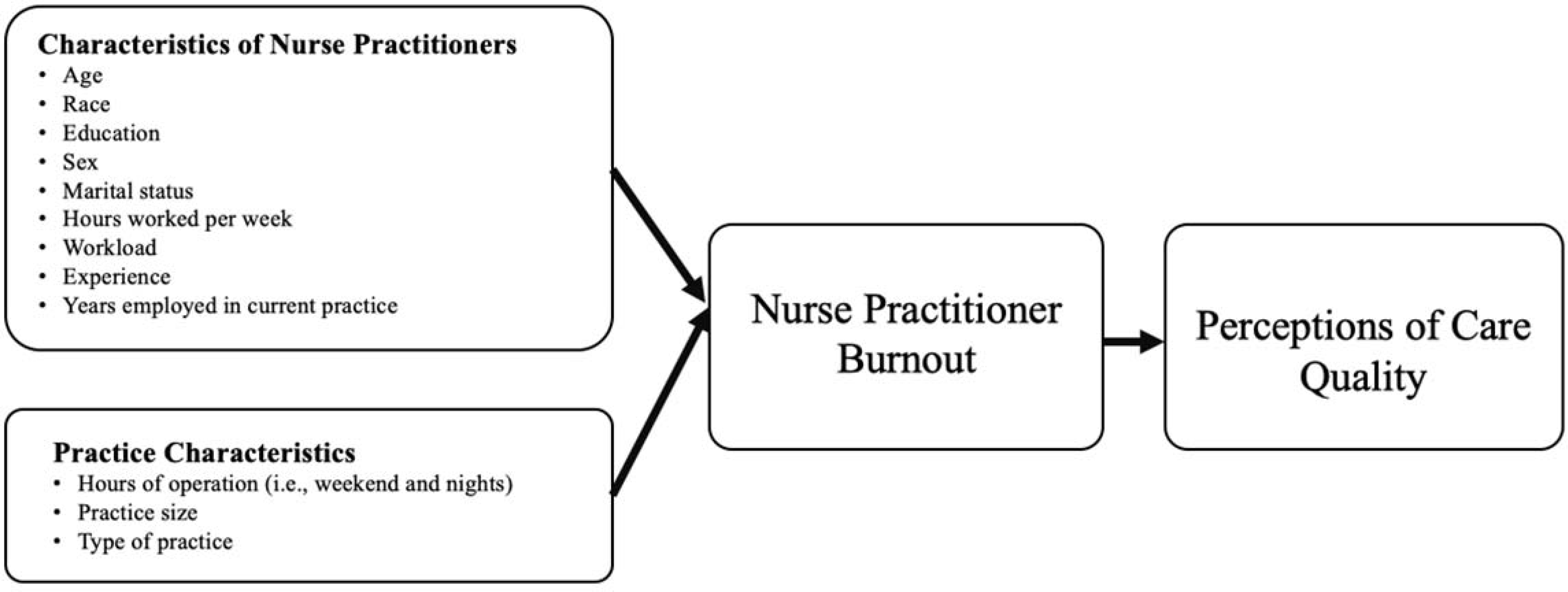
Adapted Clinician Well-Being and Resilience model
Aim 2 of our study was guided by the Baron and Kenny moderation model, which illustrate three causal paths that may lead to the outcome variable.23 A Baron and Kenny moderation analysis was conducted to assess if each of the four practice environment subscales (i.e., Professional Visibility, NP-Administration Relations, NP-Physician Relations, and Independent Practice and Support) moderates the relationship between burnout and quality of care. Figure 2 illustrates a path diagram representing the moderation model. As shown in Figure 2, there are three paths that can influence the outcome variable which is perceptions of care quality. Path A tests the impact of NP burnout on perceptions of care quality. Path B tests the impact of the moderator variable (i.e., the four practice environment subscales) on perceptions of care quality. Lastly, path C tests the impact of the interaction term on perceptions of care quality. For Aim 2, we hypothesized that each practice environment subscale (collectively considered the “practice environment”) might moderate the relationship between burnout and perceptions of care quality.
Figure 2.
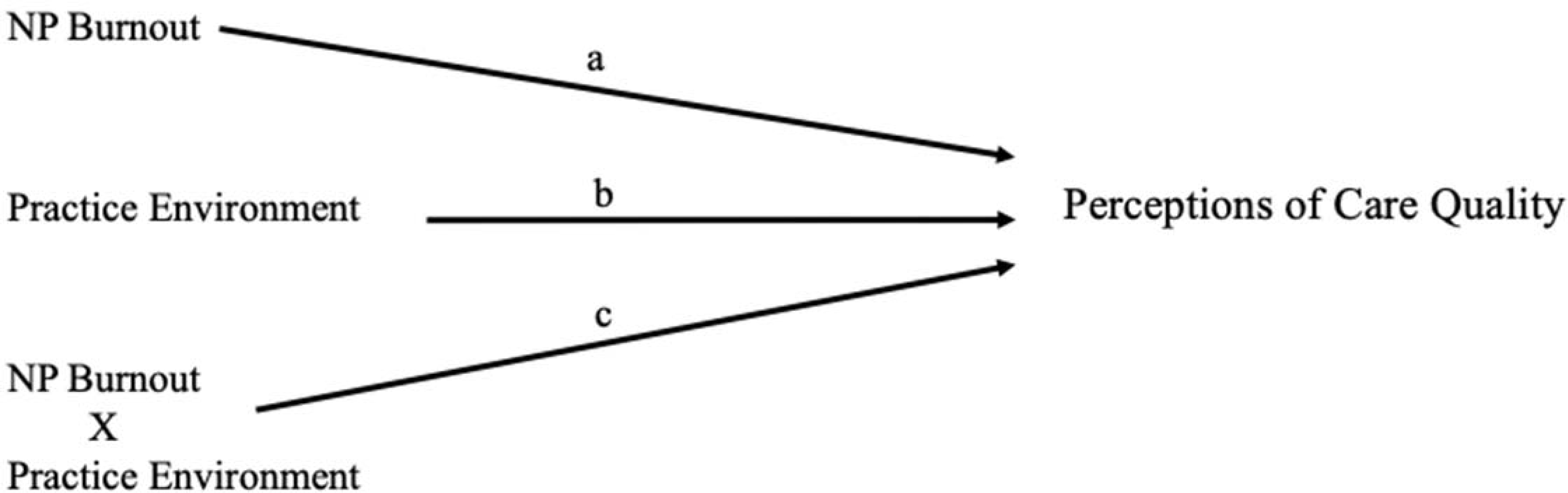
Adapted moderation model
Note. NP = Nurse Practitioner; Each practice environment subscale has a separate moderation model.
2.2. Study design and data source
This current study is a secondary analysis of cross-sectional survey data obtained from the parent study,24 which investigated ways to reduce health disparities in outcomes for older adults receiving primary care services from NPs. A description of the study methodology is described below.25
2.2.1. Description of the parent study
Primary care NPs were recruited from the SK&A OneKey primary care practice database which is a comprehensive database containing information on health care providers in the U.S.26 Three different types of primary care practices employing NPs were included: 1) an independent practice with a physician who has a primary care specialization and no less than one NP employed in that practice, 2) a medical group practice that delivers primary care and employs no less than one NP in the practice, or 3) a medical group practice containing one or more physician, at-least half of the physicians have a primary care specialization, and no less than one NP employed in that practice.25 As there were more NPs in geographically larger states than in smaller states, a random sampling of NPs was conducted.25
From 2018–2019, primary care NPs completed surveys containing valid measures of burnout, quality of care, practice environment, demographics, and characteristics of their main practice site. Researchers from the parent study collected survey data using a modified Dillman approach for mixed-mode surveys.25,27 Overall, there were three rounds of mailed surveys sent to NPs and two rounds of reminder postcards which were sent two weeks after the first and second survey mailings.25 To maximize the overall response rate, follow-up phone calls to non-responding NPs were also conducted. During some of these calls, researchers could not confirm whether the NPs were truly eligible (e.g., actually worked in that practice) and so these NPs were labeled as “unknown,” non-responding NPs.25 In total, 1,244 NPs across six states completed the survey. The most conservative response rate, 22.2%, was one in which we assumed that all non-responding NPs were eligible. However, we also calculated a response rate, 31.8%, based on a scenario where all non-responding NPs were ineligible. Therefore, we anticipate the real response rate to be in a range from 22.2% to 31.8%.25
2.2.2. Current study
Our final sample contained 396 primary care NPs practicing in New Jersey or Pennsylvania. These two states were selected because NPs working in these states would be practicing in related health care markets since New Jersey and Pennsylvania have comparable rankings for access to care28 and quality of care.29 Given that our study used multi-level modeling, a power analysis was conducted and it was found that 280 NPs was the minimal sample size needed for this study.25
2.3. Ethical consideration
We obtained approval from the institutional review board of a large university located in the East Coast of the United States prior to conducting this study.
2.4. Measures
Burnout:
Primary care NP burnout was measured using a non-proprietary, single-item measure which has been validated using a national sample of primary care clinicians.30 For this present study, NPs reported their experience of burnout from one (I enjoy my work. I have no symptoms of burnout) to five (I feel completely burned-out and often wonder if I can go on), with higher scores indicating greater burnout.30 Consistent with prior studies,31,32 burnout responses were dichotomized by combining scores three to five to indicate “burnout,” and scores one to two to indicate “no burnout.”
Practice Environment:
The practice environment was measured using the Nurse Practitioner Primary Care Organizational Climate Questionnaire (NP-PCOCQ), which is a 29-item survey containing the following four subscales: Professional Visibility (PV) (4 items), NP-Physician Relations (NP-PR) (7 items), NP-Administration Relations (NP-AR) (9 items), and Independent Practice and Support (IPS) (9 items).33 The NP-PR subscale measured the level of collegiality and teamwork between physicians and NPs, the PV subscale measured how well NP role is understood within the organization, the NP-AR subscale measured NP perceptions of their relations with organization administrators, and the IPS subscale measured the presence of organizational support and resources available to NPs.33 The NP-PCOCQ has strong psychometric properties including construct, structural, and predictive validity, and high internal consistency reliability.33 Since each NP-PCOCQ subscale represents a different dimension of the practice environment, we did not combine scores across the four subscales to generate one practice environment score. Using a sample of 396 primary care NPs from New Jersey and Pennsylvania, the Cronbach’s alpha for the PV subscale was 0.85, the NP-AR subscale was 0.94, the IPS subscale was 0.87, and the NP-PR subscale was 0.88.
Responses for each NP-PCOCQ survey item ranged from “strongly agree” to “strongly disagree.”33 Scores for the individual NP-PCOCQ subscales ranged from one to four, with higher subscale scores indicating better practice environments for NPs. Practice-level scores for each NP-PCOCQ subscale were generated by aggregating the individual subscale scores of NPs in the same practice. Each practice-level NP-PCOCQ subscale score was centered to have a mean of zero before being included in the moderation analysis, because this can reduce the possibility of high multicollinearity,34,35 and researchers recommend that continuous variables be centered to avoid problems that can inflate the standard errors.36
Perceptions of quality of care:
Perceptions of organizational care quality was measured by asking NPs “how would you rate the quality of care your organization delivers as a whole?” Response options are on a 5-point Likert scale, ranging from “poor” to “excellent,” with higher scores indicating better perceptions of care quality. Nurse-perceived quality of care is a consistent indicator of the quality of patient care in outcomes such as failure to rescue, mortality, and patient satisfaction.37 Furthermore, various researchers have used nurse-perceived quality of care as an outcome measure and have produced valuable, clinically significant results.8,38,39 Thus, NP perceptions of quality of care may provide valuable information on the quality of care delivered to patients within their organizations.
Provider and Practice-level covariates:
We selected variables measuring the demographic characteristics of NPs (i.e., age, sex, race, marital status, highest educational degree, years employed in current practice, number of hours worked per week, workload, and years of NP experience), practice characteristics (i.e., size, hours of operation, and the type of primary care practice), and state. These covariates were selected because they were identified as factors within the Clinician Well-Being and Resilience model and reported in the literature as contributing to burnout and outcomes of burnout.14,22
2.5. Statistical analysis
The dataset was cleaned and variables were coded in SPSS version 25.40 The distribution of scores for continuous variables and potential outlier scores were identified using boxplots within SPSS. Eight outlier values were removed from the dataset, but no participants were removed. To determine if multicollinearity was present, we used variance inflation factor (VIF) statistics. A VIF value less than five suggested no multicollinearity.41
Multiple Imputation:
We used multiple imputation analyses because some covariates in our study had up to 12% of missing data and multiple imputation allows researchers to obtain accurate results, prevent a potential loss in statistical power, and generate valid variance estimates when there is missing data.42,43 Given these benefits, we conducted multiple imputation analyses by creating 10 simulated versions of the dataset which was ascertained from the percentage of missing data.44 The results from the 10 complete datasets were combined and adjusted for obtained coefficients and standard errors for missing data.42,43 All multi-level analyses were conducted using the pooled estimates from the multiple imputation analyses.
We extracted and imported the pooled data into STATA statistical software45 version 14 to conduct all multi-level analyses. For Aim 1, we conducted a multi-level proportional odds cumulative logit model containing variables measuring burnout, perceptions of care quality, and characteristics of NPs within level one of the model and variables measuring characteristics of the practice within level two of the model. Since NPs had the option of completing either mail or online surveys, we controlled for survey modality within our multi-level models. State was included as a fixed effects variable.
Moderation analysis:
To test for moderation, we ran two separate models for each of the practice-level PV, IPS, NP-PR, and NP-AR subscales after centering these subscale scores to a mean of zero. In the first multi-level proportional odds cumulative logit model, perception of care quality was the outcome variable, and the two independent variables were burnout and the centered practice-level practice environment subscale (i.e., either PV, IPS, NP-PR, or NP-AR). In the second model, the only newly added variable was the centered interaction term which was created by multiplying burnout with the centered practice-level practice environment subscale. A cross-level interaction term was created because we had variables within level one (NP level) and level two (practice level) of the multi-level model. If the interaction variable was statistically significant, it was reported that the practice environment subscale moderates the relationship between burnout and quality of care. Among all models, significance values less than 0.05 were deemed statistically significant.
3.0. RESULTS
There were 396 NPs included in the study with nearly 73% of NPs from Pennsylvania (Table 1). Most NPs were female (90.4%), White (89.4%), had a Master’s degree (87.6%), and had an average of 11.4 years of NP experience (Standard Deviation [SD] = 8.9 years). None of the NPs perceived delivering poor quality of care, 4.3% perceived fair, 14.9% perceived good, 43.4% perceived very good, and 37.4% perceived delivering excellent quality of care. Nearly 25% of NPs reported burnout. No multicollinearity was detected in the final model, since the VIF was 1.69. In the multi-level model, NP burnout was a significant predictor of quality of care. The odds of perceiving higher quality of care was 85% less for NPs experiencing burnout, as compared to NPs not experiencing burnout (Cumulative Odds Ratio [COR] = 0.15, 95% CI = 0.09 to 0.24, p = .000), after controlling for NP and practice level covariates (Table 2).
Table 1.
Characteristics of Primary Care Nurse Practitioners (N = 396)
| N (%) | Mean (SD) | |
|---|---|---|
| Age | 49.5 years (12.0) | |
| Female | 358 (90.4) | |
| Highest Educational Degree- Master’s degree | 347 (87.6) | |
| Race- White | 354 (89.4) | |
| Marital status- Married | 315 (79.5) | |
| Years of NP experience | 11.4 years (8.9) | |
| Years employed in current practice | 6.4 years (6.3) | |
| Average hours worked per week | 38.9 hours (11.2) | |
| NP workload | ||
| Providing direct patient care | 31.1 hours (10.1) | |
| Coordinating patient care | 5.6 hours (6.0) | |
| Providing care management services | 2.0 hours (3.3) | |
| Performing quality assurance and improvement activities |
1.6 hours (3.5) | |
| Conducting administrative activities/leadership | 1.7 hours (3.9) | |
| Survey Format | ||
| 309 (78.0) | ||
| Online | 87 (22.0) | |
| Burnout | 100 (25.3) | |
| Perceptions of Organizational Care Quality | ||
| Poor | 0 (0.0) | |
| Fair | 17 (4.3) | |
| Good | 59 (14.9) | |
| Very good | 172 (43.4) | |
| Excellent | 148 (37.4) | |
| Characteristics of Primary Care Practices | ||
| Practice Location | ||
| New Jersey | 109 (27.5) | |
| Pennsylvania | 287 (72.5) | |
| Main practice site | ||
| Physician practice | 239 (60.4) | |
| Community health center | 51 (12.9) | |
| Hospital based clinic | 37 (9.3) | |
| Retail-based clinic | 8 (2.0) | |
| Urgent care clinic | 12 (3.0) | |
| Nurse managed clinic | 4 (1.0) | |
| Other | 45 (11.4) | |
| Practice Open on Weekends | 141 (35.6) | |
| Practice Open at Night | ||
| None | 127 (32.1) | |
| Once a week | 78 (19.7) | |
| Twice a week | 82 (20.7) | |
| Three times a week | 24 (6.1) | |
| Four or more times a week | 85 (21.5) | |
| Practice Environment Subscale Scores | ||
| Professional Visibility | 3.11 (0.65) | |
| NP-Administration Relations | 2.82 (0.71) | |
| NP-Physician Relations | 3.33 (0.52) | |
| Independent Practice and Support | 3.42 (0.48) | |
Note. SD = Standard Deviation; NP = Nurse Practitioners
Table 2.
Multi-level proportional-odds cumulative logit models assessing the effect of burnout on perceptions of care quality while controlling for provider and practice level covariates (N = 396)
| Cumulative Odds Ratio | P > |z| | 95% Confidence Interval | ||
|---|---|---|---|---|
| Burnout | 0.15 | 0.00 | 0.09 | 0.24 |
| Average hours worked/week | 0.99 | 0.61 | 0.97 | 1.02 |
| Age | 1.00 | 0.89 | 0.98 | 1.02 |
| Female | 0.96 | 0.90 | 0.48 | 1.91 |
| Marital Status- Married | 0.78 | 0.31 | 0.48 | 1.27 |
| Education | ||||
| Master’s Degree | 1.12 | 0.86 | 0.33 | 3.80 |
| Doctorate of Nursing Practice | 1.64 | 0.49 | 0.41 | 6.56 |
| Other Degree | 0.66 | 0.65 | 0.11 | 3.95 |
| Race- White | 1.21 | 0.58 | 0.62 | 2.35 |
| Years of Experience as an NP | 1.02 | 0.13 | 0.99 | 1.05 |
| Workload^ | ||||
| Providing patient care | 1.02 | 0.12 | 0.99 | 1.05 |
| Coordinating patient care | 0.98 | 0.27 | 0.94 | 1.02 |
| Providing care management services | 1.02 | 0.70 | 0.94 | 1.10 |
| Performing quality improvement | 1.07 | 0.10 | 0.99 | 1.16 |
| Practice leadership and administrative tasks | 1.00 | 0.92 | 0.94 | 1.06 |
| Type of practice - Physician practice | 1.28 | 0.24 | 0.85 | 1.93 |
| Open during the Weekends | 1.08 | 0.74 | 0.68 | 1.73 |
| Open at Night | 1.09 | 0.20 | 0.96 | 1.24 |
| Practice Size | 1.03 | 0.05 | 1.00 | 1.06 |
| Survey type | 0.88 | 0.60 | 0.55 | 1.42 |
| State | 0.46 | 0.00 | 0.29 | 0.74 |
Note. NP = Nurse Practitioner; Workload^ = Measured as hours per week performing the following tasks
3.1. Moderation analysis
Tables 3 and 4 (and in the supplementary file Figures 3–6) display the results from the two multi-level proportional-odds cumulative logit models for each practice environment subscale.
Table 3.
Multi-level proportional-odds cumulative logit models assessing the effect of burnout and practice environment with quality of care (N = 396)
| Cumulative Odds Ratio | P > |z| | 95% Confidence Interval | ||
|---|---|---|---|---|
| Model 1 for Professional Visibility Subscale = | ||||
| Burnout | 0.23 | 0.00 | 0.14 | 0.36 |
| Professional Visibility | 4.39 | 0.00 | 3.10 | 6.20 |
| Model 1 for Independent Practice and Support Subscale = | ||||
| Burnout | 0.21 | 0.00 | 0.13 | 0.34 |
| Independent Practice and Support | 7.57 | 0.00 | 4.77 | 12.03 |
| Model 1 for NP-Physician Relations Subscale = | ||||
| Burnout | 0.21 | 0.00 | 0.13 | 0.34 |
| NP-Physician Relations | 4.76 | 0.00 | 3.15 | 7.20 |
| Model 1 for NP-Administration Relations Subscale = | ||||
| Burnout | 0.27 | 0.00 | 0.16 | 0.43 |
| NP-Administration Relations | 3.83 | 0.00 | 2.76 | 5.30 |
Note. NP = Nurse Practitioner
Table 4.
Multi-level proportional-odds cumulative logit models testing whether the practice environment moderates the relationship between burnout and quality of care (N = 396)
| Beta Coefficient | P > |z| | 95% Confidence Interval | ||
|---|---|---|---|---|
| Model 2 for Professional Visibility Subscale = | ||||
| Burnout | −1.51 | 0.00 | −2.00 | −1.02 |
| Professional Visibility | 1.51 | 0.00 | 1.10 | 1.93 |
| Interaction Term (Burnout*Professional Visibility) | −0.10 | 0.77 | −0.80 | 0.59 |
| Model 2 for Independent Practice and Support Subscale = | ||||
| Burnout | −1.54 | 0.00 | −2.03 | −1.06 |
| Independent Practice and Support | 2.03 | 0.00 | 1.48 | 2.57 |
| Interaction Term (Burnout*Independent Practice and Support) | −0.005 | 0.99 | −0.92 | 0.91 |
| Model 2 for NP-Physician Relations Subscale = | ||||
| Burnout | −1.58 | 0.00 | −2.07 | −1.10 |
| NP-Physician Relations | 1.63 | 0.00 | 1.12 | 2.14 |
| Interaction Term (Burnout*NP-Physician Relations) | −0.20 | 0.63 | −1.02 | 0.62 |
| Model 2 for NP-Administration Relations Subscale = | ||||
| Burnout | −1.39 | 0.00 | −1.90 | −0.88 |
| NP-Administration Relations | 1.42 | 0.00 | 1.04 | 1.81 |
| Interaction Term (Burnout*NP-Administration Relations) | −0.27 | 0.43 | −0.93 | 0.40 |
Note. NP = Nurse Practitioner
Professional Visibility:
Burnout and the PV subscale score were both significantly related to perceptions of care quality (p < .00). With a one unit increase in the PV subscale, the odds of perceiving higher quality of care increased 4.39 times (COR = 4.39, 95% CI = 3.10 to 6.20, p = .000). In the second model, the cross-level interaction variable between burnout and the PV subscale score was not significant (Beta Coefficient = −0.10, p = .77).
Independent Practice and Support:
Similar to the PV subscale, the cross-level interaction variable between burnout and the IPS subscale score was not significant (Beta Coefficient = −0.005, p = .99). However, without the interaction term, burnout and the IPS subscale score were significantly related to perceptions of care quality (p < .00). With a one unit increase in the IPS subscale, the odds of perceiving higher quality of care increased 7.57 times (COR = 7.57, 95% CI = 4.77 to 12.03, p = .000).
NP-Physician Relations:
In the multi-level proportional-odds cumulative logit model, the cross-level interaction variable between burnout and the NP-PR subscale score was not significant (Beta Coefficient = −0.20, p = .63). When the interaction term is removed, with a one unit increase in the NP-PR subscale, the odds of perceiving higher quality of care increased 4.76 times (COR = 4.76, 95% CI = 3.15 to 7.20, p = .000).
NP-Administration Relations:
The cross-level interaction variable between burnout and the NP-AR subscale score was not significant (Beta Coefficient = −0.27, p = .43). Nevertheless, with a one unit increase in the NP-AR subscale, the odds of perceiving higher quality of care increased 3.83 times (COR = 3.83, 95% CI = 2.76 to 5.30, p = .000).
4.0. DISCUSSION
In this study, we examine whether a relationship exists between NP burnout and perceptions of care quality in primary care practices and whether NP practice environment moderates the relationship between burnout and perceptions of care quality. We found that nearly 25% of NPs report burnout and that NP burnout is a significant predictor of lower perceptions of care quality, since the odds of NPs perceiving higher quality of care was 85% less for NPs experiencing burnout, as compared to NPs not experiencing burnout. Furthermore, we found that the practice environment did not moderate the relationship between burnout and perceptions of care quality. This finding is important because it suggests that, specifically within our sample of primary care NPs, the practice environment does not explain the link between NP burnout and quality of care. Although there is no moderating effect, we did find that the practice environment is independently related to perceptions of care quality. Increased scores on any of the four practice environment subscales (i.e., PV, IPS, NP-PR, and NP-AR) were associated with higher odds of NPs perceiving the delivery of higher quality of care. This implies that working environments where administrators and staff members have a good understanding of the NP role, NPs are allowed to provide care within their scope of practice, and NPs have positive relations with physicians and practice administrators all contribute to NPs’ perceptions of delivering higher quality of care. As such, fostering a healthy practice environment for an NP may be an important mechanism to improving patient care delivery.
Our findings are consistent with researchers who also report that nurse burnout is related to lower perceptions of care quality.8,46 One researcher found that for every unit increase in the emotional exhaustion score for nurses, there was a 2.53 times increase in nurses perceiving fair or poor quality of patient care,8 which shows that burnout in nurses can influence nurse perceptions of care quality. Moreover, our findings are also consistent with the larger body of evidence showing that when nurses practice in favorable environments, perceptions of care quality may also improve.20,21,47 For example, in better practice environments, nurses were 66% less likely to perceive fair or poor quality of care compared to nurses in poor environments.21 As a result, one may infer that improvements made to the NP practice environment (e.g., organizational support for NPs, adequate supply of resources to provide care, optimal relationships with physicians and administrators, and professional visibility within their practice) may help to subsequently improve NP perceptions of care quality. In a systematic review on interventions to reduce physician burnout, researchers report that improving the practice environment by reducing workload, improving work processes, and team communication can reduce burnout.48 Therefore, it may be possible that such improvements made to the NP practice environment may also reduce NP burnout.
4.1. Implications
Clinicians and practice administrators can view the independent relationships between the practice environment and perceptions of care quality as evidence showing how working in favorable practice environments is related to perceptions of delivering higher quality of patient care. As a result, organizational changes designed to improve the practice environment and reduce NP burnout may also improve perceptions of care quality. To ensure that patients receive the highest quality of care in primary care practices, future research should involve all PCPs to see how the practice environment for NPs, physicians, and physician assistants can be modified to reduce provider burnout and optimize care quality for patients. With high provider workloads having the potential to impact care quality, future research should investigate whether workload moderates the relationship between burnout and care quality.
4.2. Limitations
Since this study uses cross-sectional survey data, it is not possible to determine whether burnout causes lower NP perceptions of care quality. Additionally, another limitation is the subjective nature of the collected data, since NP perceptions of care quality may be different from patient reported quality of care. Objective data regarding quality of care are needed. However, researchers have successfully measured perceptions of care quality among primary care physicians,49 and provider perceptions of quality of care has been shown to be a reliable indicator for quality of care delivered to patients.37 The overall response rate is low which may suggest that the NPs who completed the survey are different from NPs nationally. However, NPs in our study were fairly akin in race (89.4% White vs. 87% White nationally), age (49.5 years vs. 49 years nationally), and sex (90.4% female vs. 91.7% female nationally) to NPs nationally.50 Moreover, since this study investigates burnout among primary care NPs in New Jersey and Pennsylvania, the generalizability of our findings is limited.
5.0. CONCLUSION
This study examined the relationship between primary care NP burnout and perceptions of care quality in practices located in New Jersey and Pennsylvania. We found a relationship between NP burnout and lower perceptions of delivering higher quality of care. Similarly, favorable primary care NP practice environments were related to higher perceptions of care quality, but the practice environment did not moderate the relationship between burnout and perceptions of care quality. Results from our study provide valuable insight for practice administrators to prioritize reducing NP burnout and create favorable practice environments for NPs, which may contribute to the delivery of high quality patient care.
Supplementary Material
Acknowledgements:
We thank all the nurse practitioners who completed the survey.
Funding:
This study was supported by grant number R36HS027290 from the Agency for Healthcare Research and Quality, as well as from the Robert Wood Johnson Foundation, the Jonas Center for Nursing and Veterans Healthcare, and the National Institute on Minority Health and Health Disparities (R01MD011514). The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality, the Robert Wood Johnson Foundation, the Jonas Center for Nursing and Veterans Healthcare, nor the National Institute on Minority Health and Health Disparities.
Footnotes
Conflicts of Interest: The authors declare no conflicts of interest.
Contributor Information
Cilgy M. Abraham, Columbia University School of Nursing, 560 West 168th Street-Mail Code 6, New York, NY 10032.
Katherine Zheng, Columbia University School of Nursing, 560 West 168th Street-Mail Code 6, New York, NY, 10032.
Allison A. Norful, Columbia University School of Nursing, 630 West 168th Street-Mail Code 6, New York, NY 10032.
Affan Ghaffari, Columbia University School of Nursing, 516 W. 168th Street, 2nd Floor; New York, NY 10032.
Jianfang Liu, Columbia University School of Nursing, 560 W. 168th Street, New York, NY 10032.
Lusine Poghosyan, 630 W. 168th Street, mail code 6; New York, NY 10032.
References
- 1.World Health Organization. Burn-out an “occupational phenomenon:” international classification of diseases. 2019. Retrieved from https://www.who.int/mental_health/evidence/burn-out/en/
- 2.West CP, Dyrbye LN, Shanafelt TD. Physician burnout: contributors, consequences and solutions. J Intern Med. 2018;283(6):516–529. [DOI] [PubMed] [Google Scholar]
- 3.Panagioti M, Geraghty K, Johnson J, et al. Association Between Physician Burnout and Patient Safety, Professionalism, and Patient Satisfaction: A Systematic Review and Meta-analysis. JAMA Intern Med. 2018;178(10):1317–1330. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 4.Kane L Medscape national physician burnout and suicide report 2020: The generational divide. 2020. https://www.medscape.com/slideshow/2020-lifestyle-burnout-6012460. Accessed March 15, 2020.
- 5.Rabatin J, Williams E, Manwell LB, et al. Predictors and Outcomes of Burnout in Primary Care Physicians. J Prim Care Community Health. 2016;7(1):41–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Abdulla L, Al-Qahtani DM, Al-Kuwari MG. Prevalence and determinants of burnout syndrome among primary healthcare physicians in Qatar. S Afr Fam Pract. 2011;53(4):380–383. [Google Scholar]
- 7.Cimiotti JP, Aiken LH, Sloane DM, et al. Nurse staffing, burnout, and health care-associated infection. Am J Infect Control. 2012;40(6):486–490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nantsupawat A, Nantsupawat R, Kunaviktikul W, et al. Nurse Burnout, Nurse-Reported Quality of Care, and Patient Outcomes in Thai Hospitals. J Nurs Scholarsh. 2016;48(1):83–90. [DOI] [PubMed] [Google Scholar]
- 9.Tourigny L, Baba VV, Monserrat SI, et al. Burnout and absence among hospital nurses: an empirical study of the role of context in Argentina. European Journal of International Management. 2019;13(2):198–223. [Google Scholar]
- 10.Wen J, Cheng Y, Hu X, et al. Workload, burnout, and medical mistakes among physicians in China: A cross-sectional study. Biosci Trends. 2016;10(1):27–33.doi: 10.5582/bst.2015.01175 [DOI] [PubMed] [Google Scholar]
- 11.Petterson S, McNellis R, Klink K, et al. The State of Primary Care in the United States: A Chartbook of Facts and Statistics. 2018. https://www.graham-center.org/content/dam/rgc/documents/publications-reports/reports/PrimaryCareChartbook.pdf. Accessed March 18, 2020.
- 12.Robertson SL, Robinson MD, Reid A. Electronic Health Record Effects on Work-Life Balance and Burnout Within the I3 Population Collaborative. J Grad Med Educ. 2017;9(4):479–484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Babbott S, Manwell LB, Brown R, et al. Electronic medical records and physician stress in primary care: results from the MEMO Study. J Am Med Inform Assoc. 2014;21(e1):e100–e106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dewa CS, Loong D, Bonato S, et al. The relationship between physician burnout and quality of healthcare in terms of safety and acceptability: a systematic review. BMJ Open. 2017;7(6):e015141. 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.AANP. NP Fact Sheet. 2020. https://www.aanp.org/about/all-about-nps/np-fact-sheet. Accessed June 20, 2020.
- 16.Abraham CM, Zheng K, Poghosyan L. Predictors and outcomes of burnout among primary care providers in the United States: A systematic review. Med Care Res Rev. 2020;77(5):387–401. [DOI] [PubMed] [Google Scholar]
- 17.Poghosyan L, Aiken LH. Maximizing nurse practitioners’ contributions to primary care through organizational changes. J Ambul Care Manage. 2015;38(2):109–117. [DOI] [PubMed] [Google Scholar]
- 18.Poghosyan L, Nannini A, Stone PW, et al. Nurse practitioner organizational climate in primary care settings: implications for professional practice. J Prof Nurs. 2013;29(6):338–349. [DOI] [PubMed] [Google Scholar]
- 19.Carthon JMB, Brom H, Poghosyan L, et al. Supportive Clinical Practice Environments Associated With Patient-Centered Care. J Nurse Pract. 2020;16(4):294–298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lake ET, Sanders J, Duan R, et al. A Meta-Analysis of the Associations Between the Nurse Work Environment in Hospitals and 4 Sets of Outcomes. Med Care. 2019;57(5):353–361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lake ET, Hallowell SG, Kutney-Lee A, et al. Higher Quality of Care and Patient Safety Associated With Better NICU Work Environments. J Nurs Care Qual. 2016;31(1):24–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Brigham T, Barden C, Dopp AL, et al. A journey to construct an all-encompassing conceptual model of factors affecting clinician well-being and resilience. NAM Perspectives. 2018; 1–8. [Google Scholar]
- 23.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51(6):1173–1182. [DOI] [PubMed] [Google Scholar]
- 24.Poghosyan L, Ghaffari A, Liu J, et al. Primary care nurse practitioners’ roles and work environment in six states with variable scope of practice regulations. Unpublished Manuscript. 2020. [Google Scholar]
- 25.Abraham CM, Zheng K, Norful AN, et al. Primary care practice environment and burnout among nurse practitioners. J Nurse Pract. 2021;17(2):157–162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.DesRoches CM, Barrett KA, Harvey BE, et al. The results are only as good as the sample: assessing three national physician sampling frames. J Gen Intern Med. 2015;30:S595–S601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dillman DA, Smyth JD, Christian LM . Internet, Mail, and Mixed-Mode Surveys: The Tailored Design Method. John Wiley & Sons; 2014. [Google Scholar]
- 28.U.S. News and World Reports. Health care access rankings. 2019. https://www.usnews.com/news/best-states/rankings/health-care/healthcare-access. Accessed April 9, 2019.
- 29.U.S. News and World Reports. Health care quality rankings. 2019. https://www.usnews.com/news/best-states/rankings/health-care/healthcare-quality. Accessed April 9, 2019.
- 30.Dolan ED, Mohr D, Lempa M, et al. Using a single item to measure burnout in primary care staff: a psychometric evaluation. J Gen Intern Med. 2015;30(5):582–587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Edwards ST, Marino M, Balasubramanian BA, et al. Burnout Among Physicians, Advanced Practice Clinicians and Staff in Smaller Primary Care Practices. J Gen Intern Med. 2018;33(12):2138–2146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Helfrich CD, Dolan ED, Simonetti J, et al. Elements of team-based care in a patient-centered medical home are associated with lower burnout among VA primary care employees. J Gen Intern Med. 2014;29 Suppl 2(Suppl 2):S659–S666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Poghosyan L, Nannini A, Finkelstein SR, et al. Development and psychometric testing of the Nurse Practitioner Primary Care Organizational Climate Questionnaire. Nurs Res. 2013;62(5):325–334. [DOI] [PubMed] [Google Scholar]
- 34.Shieh G Clarifying the role of mean centring in multicollinearity of interaction effects. Br J Math Stat Psychol. 2011;64(3):462–477. [DOI] [PubMed] [Google Scholar]
- 35.Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Thousand Oaks, CA: Sage; 1991. [Google Scholar]
- 36.Goldstein ND (2015). The why and when of centering continuous predictors in regression modeling. https://www.goldsteinepi.com/blog/thewhyandwhenofcenteringcontinuouspredictorsinregressionmodeling/index.html. Accessed March 16, 2021.
- 37.McHugh MD, Stimpfel AW. Nurse reported quality of care: a measure of hospital quality. Res Nurs Health. 2012;35(6):566–575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ball J, Day T, Murrells T, et al. Cross-sectional examination of the association between shift length and hospital nurses job satisfaction and nurse reported quality measures. BMC Nurs. 2017;16:26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Stalpers D, Kieft RAMM, van der Linden D, et al. Concordance between nurse-reported quality of care and quality of care as publicly reported by nurse-sensitive indicators. BMC Health Serv Res. 2016;16:120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.IBM Corp. IBM SPSS Statistics for Windows, Version 25.0. 2017; Armonk, NY. [Google Scholar]
- 41.Akinwande MO, Dikko HG, Samson A. Variance inflation factor: as a condition for the inclusion of suppressor variables in regression analysis. Open J Stat. 2015;5(7):754. [Google Scholar]
- 42.Murray JS. Multiple imputation: A review of practical and theoretical findings. Statistical Science. 2018;33(2): 142–159. [Google Scholar]
- 43.McCleary L Using multiple imputation for analysis of incomplete data in clinical research. Nurs Res. 2002;51(5):339–343. [DOI] [PubMed] [Google Scholar]
- 44.Bodner TE. What improves with increased missing data imputations? Struct Equ Modeling. 2008;15(4):651–675. [Google Scholar]
- 45.Stata Corp. STATA statistical software: Release 14. 2015; College Station, TX. [Google Scholar]
- 46.Poghosyan L, Clarke SP, Finlayson M, et al. Nurse burnout and quality of care: cross-national investigation in six countries. Res Nurs Health. 2010;33(4):288–298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kanai-Pak M, Aiken LH, Sloane DM, et al. Poor work environments and nurse inexperience are associated with burnout, job dissatisfaction and quality deficits in Japanese hospitals. J Clin Nurs. 2008;17(24):3324–3329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.West CP, Dyrbye LN, Erwin PJ, Shanafelt TD. Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. The Lancet. 2016;388(10057):2272–81. [DOI] [PubMed] [Google Scholar]
- 49.Pantell MS, De Marchis E, Bueno A, et al. Practice Capacity to Address Patients’ Social Needs and Physician Satisfaction and Perceived Quality of Care. Ann Fam Med. 2019;17(1):42–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.AANP. The state of the nurse practitioner profession: results from the national nurse practitioner sample survey. 2019. https://www.aanp.org/news-feed/nurse-practitioner-role-continues-to-grow-to-meet-primary-care-provider-shortages-and-patient-demands. Accessed March 28, 2020.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


