Abstract
Introduction and importance
The parathyroid cancer is sometime only diagnosed after a pathological fracture has occurred, and pathology fracture is often misdiagnosed as a malignancy tumor. The treatment for pathology fracture and multiple bone lesions is not defined.
Case presentation
We report a 41-year-old case of parathyroid carcinoma in which pathological femoral fracture and brown tumors are the first clinical signs of the disease and that masqueraded as a malignancy tumor. The treatment for the patient was parathyroidectomy and then surgical treatment of the right femur with a locking plate osteosynthesis. Four months post-operative, the patient reported no pain and became capable of walking without a crutch. X-rays showed full bone union at fracture site of right femur, and brown tumors regression seen to be taking place in the upper limb, lower limbs and pelvis.
Clinical discussion
A brown tumor was diagnosed by a high concentration of blood parathyroid hormone and serum calcium. Despite the lack of clinical guidelines, most authors agreed that parathyroidectomy was the first choice of treatment then orthopaedic treatment. The principles of osteosynthesis of fracture were based on stable osteosynthesis. It was reported that osteolytic lesions caused by brown tumor were recovered when hyperparathyroidism had been treated.
Conclusion
Brown tumor needs to be considered in the differential diagnosis when there are osteolytic lesions and high serum calcium. It is advisable to have a parathyroidectomy and then orthopaedic treatment. Brown tumor with Mirels' score less than 7 scores should be applied a conservative treatment.
Keywords: Brown tumor, Parathyroid cancer, Hyperparathyroidism, Pathology fracture
Highlights
-
•
Pathology fracture sometime is the first sign of parathyroid cancer and often misdiagnosed with bone malignant tumor.
-
•
Parathyroidectomy is the first choice.
-
•
The principles of osteosynthesis of pathology fracture are based on stable osteosynthesis.
-
•
Brown tumor with Mirels' score less than 7 scores should be applied a conservative treatment.
1. Introduction and importance
Brown tumor involves unifocal or multifocal bone lesions, is a rare bony benign lesion, which represent a terminal stage of hyperparathyroidism-dependent bone pathology. Parathyroid cancer is one of the rarest causes of primary hyperparathyroidism and tends to present with severe symptoms of hypercalcemia. However, in some cases the hyperparathyroidism is only diagnosed after a pathological fracture has occurred and that are mentioned as the first sign of a malignant tumor. Pathology fracture and multiple bony lesions of brown tumors are often misdiagnosed as metastatic carcinoma, bone cysts, osteosarcoma, or giant-cell tumors [1], [2], [3]. Parathyroidectomy is the first choice of treatment; however, the treatment for pathology fracture and multiple bone lesions is not defined. We report a 41-year-old case of primary hyperparathyroidism due to parathyroid carcinoma in which pathological femoral fracture is the first clinical sign of the disease and that masqueraded as a malignancy due to presence of multiple large osteolytic lesions. Our case was treated by parathyroidectomy, internal fixation of femur by locking plate and bone grafting.
2. Case presentation
This case follows 2020 SCARE guidelines for reporting of cases in surgery [4]. A 41-year-old woman was transferred from a local hospital to our hospital with a diagnosis as a pathological peritrochanteric fracture of the right femur due to multiple myeloma. The patient was in a good state overall. She reported a history of severe pain in the right hip that prevented active movement, mild swelling of the right thigh due to low energy fall one day ago. There was no compromising of blood flow, sensation or motor-nerve function. X-rays showed a pathological peritrochanteric fracture of right femur and multiple osteolytic lesions in the iliac bone (Fig. 1). The patient had never been in inpatient medical treatment and had no history of weight loss, fever or a family history for any tumors, any relevant genetic information, and psychosocial history or disorders of serum calcium and relevant pre-existing illnesses.
Fig. 1.
X-rays and CT Scans pre-operative. A,B, X rays of femur and pelvis. C,D,E, CT Scans of pelvis. F, X rays of right tibia and fibula. G,H,I, X-rays of bilateral forearm and Rt arm. J, Post-operative X rays of right femur. K, parathyroid scintigraphy showed increased radiotracer uptake in the lower pole of the right thyroid lobe with 04 mCi TcO4 parathyroid scintigraphy. L, Abdominal ultrasound identified bilateral kidney stones.
Initially, the fracture was stabilized with a long leg cast and the patient was referred to our orthopaedic center for further treatment and diagnostic findings. Due to the pathological fracture, a haemato-oncological consultation was performed. A computed tomography (CT) scan of the abdomen, chest and neck; neck ultrasound; bone marrow biopsy and parathyroid scintigraphy were performed. Neck ultrasound showed an 18 × 34 mm hypoechoic parathyroid mass next to the lower pole of the right thyroid lobe. X-rays and CT scan showed a pathological peritrochanteric fracture of right femur. At the level of the pathological fracture, a large osteolytic lesion was observed. There were multiple osteolytic lesions were found at the middle third of right femur, pelvis bone and left femur, bilateral tibia, bilateral humerus and bilateral forearm (Fig. 1). Abdominal ultrasound and CT scan identified bilateral kidney stones. There was an increased radiotracer uptake in the lower pole of the right thyroid lobe with 04 mCi TcO4 parathyroid scintigraphy. The result of bone marrow biopsy was normal. No primary thoracic or abdominal malignancy was evident.
Laboratory test showed hypercalcemia (Table 1). Total serum calcium was highly elevated at 3.43 mmol/l (normal range: 2.2–2.6 mmol/l) and serum phosphorus was 1.08 mmol/l (normal range: 0.81–1.45 mmol/l). Intact PTH was 2481.7 pg/ml (normal range: 15–68.3 pg/ml) and phosphorus was 1.08 mmol/l (normal range, 0.8–1.5 mmol/l). Serum urea was 21.29 mmol/l (normal range, 2.5–6.7 mmol/l), serum creatinine was 143 μmol/l (normal range, 50–98 μmol/l). FT3, FT4, FSH and liver function tests were within normal limits.
Table 1.
Gradual variation of serum calcium, phosphorus, parathyroid hormone, urea, creatinine.
| Variable | Normal range | Pre-op | 1 day post-op | 2 days post-op | 4 days post-op | 7 days post-op | 4 months post-op |
|---|---|---|---|---|---|---|---|
| Calcium(mmol/l) | 2.2–2.6 | 3.43 | 2.61 | 1.9 | 2.0 | 1.9 | 2.2 |
| Phosphorus (mmol/l) | 0.8–1.5 | 1.08 | 0.93 | ||||
| PTH (pmol/l) | 1.6–6.9 | 1381 | 65.08 | ||||
| PTH (pg/ml) | 15.0–68.3 | 2481.7 | 269.5 | ||||
| Urea | 21.29 | 8.63 | |||||
| Creatinine | 143 | 150 |
The patient was presented to the interdisciplinary orthopaedic-oncological board and was diagnosed as a parathyroid carcinoma with pathology peritrochanteric fracture of right femur and multiple brown tumors. The decision was made for a parathyroidectomy and then surgical treatment of the right femur with a locking plate osteosynthesis (Fig. 1). Calcium carbonate and vitamin D were substituted. The patient consented to undergo the proposed operation. The lower portion of the right lobe of the thyroid gland, including the parathyroid gland, was then resected. The calcium became normalized and parathyroid hormone decreased to 65.08 pmol/l after the surgery. The pathological results of the parathyroid suggested the parathyroid carcinoma (Fig. 2). Immunohistochemically, tumor cells were negative for thyroid transcription factor-1 (TTF-1), negative for thyroglobulin, negative for S100 and CD 56, positive for Chrommogranin. Two days post-operative, our patient displayed the hungry bone syndrome with numbness and tingling sensations in her fingers and toes and serum calcium was at 1.9 mmol/l. The patient was treated with calcium gluconate intravenous infusion. These symptoms gradually stabilized soon. On the 4 days post-operative, the patient was scheduled for surgical treatment of the right femoral fracture. Surgery was performed by the authors (G.N.N., L.N.V.) The fracture was reduced and fixed with a proximal femoral locking plate (Mikromed, Poland) and bone grafting. The histopathology results of the right femur fracture confirmed the presence of a brown tumor. After discharge, she was received high amounts of calcium carbonate and vitamin D3 for four months. Patient was permitted partial weight-bearing activities until 10 weeks after operation. Monthly follow-ups were conducted by us and an endocrinologist.
Fig. 2.
Pathologic examination suggested a parathyroid carcinoma (H.E. ×100, ×400).
Four months post-operative, the union of the fracture of right femur was confirmed (Fig. 3). The calcium and phosphate became normalized and parathyroid hormone was 269.5 pg/l. FT3, FT4, FSH, liver function and kidney function tests were within normal limits. The patient reported no pain and became capable of walking without a crutch (Fig. 3). X-rays showed full bone union at fracture site of right femur, without secondary displacement, and brown tumor regression seen to be taking place in the upper limb, lower limbs and pelvis (Fig. 3). She is now checked regularly monthly by the authors and an endocrinologist. The patient reports being very satisfied with the overall results.
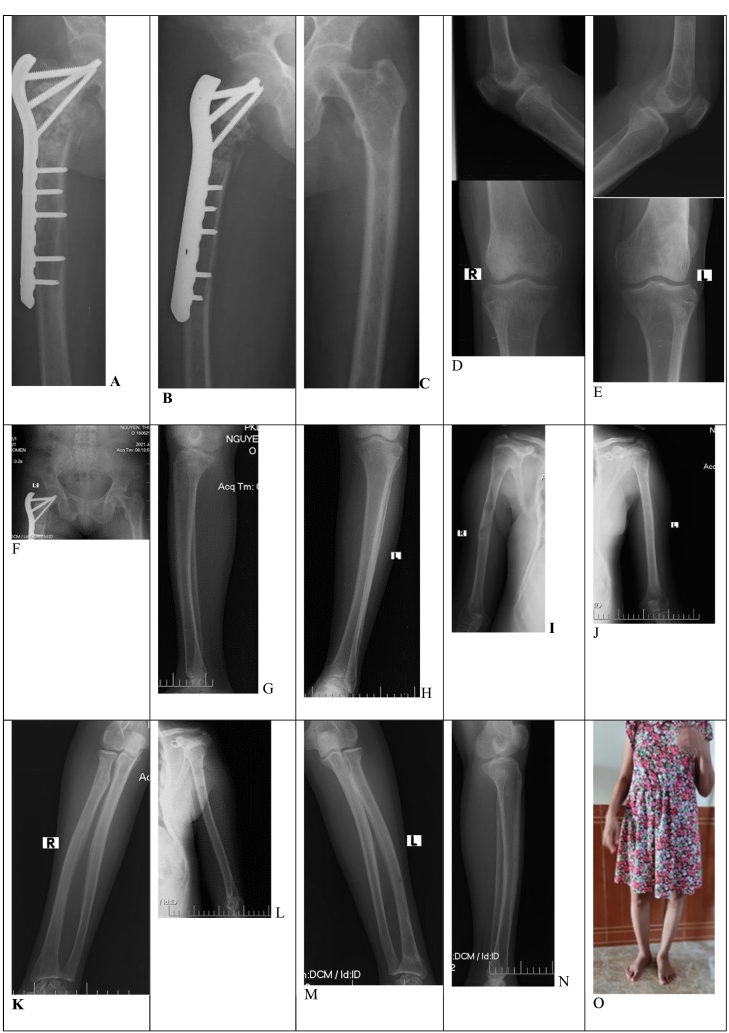
Fig. 3.
Four months post-operative, X-rays and clinical outcomes. A,B, X-rays showed bone union at fracture site of right femur, with no secondary displacement. C,D,E,F,G,H,I,K,L,M,N, brown tumor regression seen to be taking place in the upper limb, lower limbs and pelvis. O, 4 months post-operative clinical outcomes, the patient reported no pain and became capable of walking without a crutch.
3. Discussion
3.1. Diagnosis
Brown tumor is a benign bone lesion due to hyperparathyroidism. An increase of blood parathyroid hormone concentration activates the osteoclast. Due to the rapid bone loss, haemorrhage, granulation tissue and fibrous tissue replace the bone marrow; the brownish due to haemosiderin deposition, that are referred as brown tumor [5], [6], [7], [8]. It can cause pain and fracture. In developing countries, hyperparathyroidism is mostly diagnosed lately due to lack of routine screening of serum calcium and parathyroid hormone, so pathology fracture is the first sign suggesting the disease and our case is an example. In radiological aspects, which has an osteolytic lesion at the fracture site and multiple osteolytic lesions so it is often misdiagnosed as malignant tumors, such as metastatic carcinoma, osteosarcoma, Ewing sarcoma, lymphoma and multiple myeloma [3], [7], [9], [10]. In our case, there was not only a large osteolytic lesion in the right femoral peritrochanteric fracture but also multiple osteolytic lesions in the left femur, at the middle third of right femur, in the pubis, tibia, humerus and forearm. She was misdiagnosed as a multiple myeloma by another hospital. Brown tumor needs to be considered in the differential diagnosis when there are osteolytic lesions and high serum calcium.
In our cases, the difference of radiological aspects of brown tumor was that it does not invade adjacent tissues and did not induce changes around the periosteum. In contrast, a periosteal reaction is frequently observed in cases of metastatic tumor. A brown tumor due to hyperparathyroidism was diagnosed by a high concentration of blood parathyroid hormone and serum calcium. Neck ultrasound, CT scan and parathyroid scintigraphy should be done to identify and localize the parathyroid tumor.
Some patients present with symptoms involving the urinary system [6]. Ultrasound and CT scans of abdomen should be done to identify urinary stone. When the concentration of calcium ions and phosphorus ions exceeds the renal threshold and these ions enter the urine, causing stone of urinary system and secondary symptoms. Abdominal ultrasound and CT scan of our case identified bilateral kidney stone, serum urea and serum creatinine were highly elevated.
The main causes of hyperparathyroidism are parathyroid adenoma, accounting for 85%, parathyroid hyperplasia, accounting for 10–15%, and carcinoma, accounting for 1–5% [11]. While there is definitely an overlap between the symptomatology of them, the following characteristics are more likely to reflect parathyroid carcinoma: A higher frequency of symptomatic hypercalcemia; very high serum PTH concentrations (over 5–10× upper limit of normal range); serum calcium levels >14 mg/dl; presence of a parathyroid crisis; presence of a palpable neck mass [5]. In our case, total serum calcium was 3.43 mmol/l and intact PTH was 2481.7 pg/ml (normal range: 15–68.3 pg/ml), that reflected the parathyroid carcinoma. Neck ultrasound, CT scans and parathyroid scintigraphy were helpful to identify a parathyroid tumor at the lower right glands and relationship to surrounding soft tissue structures. Fine needle aspiration biopsies were not done in our case because that are discouraged since histology does not differentiate between benign and malignant disease, and there is always a risk of seeding the biopsy tract [5].
3.2. Treatment
Proper treatment of pathological fractures due to brown tumor requires a multidisciplinary approach, focused on the achievement of appropriate bone union of pathological fracture and osteolytic lesions and parathyroid tumor management. In patient with severe hyperparathyroidism, parathyroidectomy is the first choice of treatment then orthopaedic treatment. The best chance for cure is with a complete en bloc resection, especially when the diagnosis of parathyroid carcinoma is suspected preoperatively. In our case, the total serum calcium and PTH reflected the parathyroid carcinoma, so the lower portion of the right lobe of the thyroid gland including the parathyroid gland was resected. Pathological results confirmed parathyroid carcinoma. The calcium and parathyroid hormone became reduced sharply post-operative. Postoperative, the patients are required to close monitoring both clinical and laboratory since most of these patients are highly susceptible to hungry bone syndrome [6]. This may be exaggerated in patients who received preoperative bisphosphonates for treatment of a hypercalcemic crisis [5]. In our case, the calcium became normalized and parathyroid hormone decreased to 65.08 pmol/l after the surgery. Two days post-operative, our patient displayed the hungry bone syndrome with serum calcium was at 1.9 mmol/l. The patient was treated with calcium gluconate intravenous infusion. These symptoms gradually stabilized soon. So, we recommended osteosynthesis at the three or four day post-operative parathyroidectomy.
The principles of osteosynthesis of pathology fracture due to brown tumor are based on stable osteosynthesis with preservation of proper length, axis and rotation of the bone. Intramedullary nailing remains the preferred stabilization technique for shaft fracture of femur and tibia [10]. Intramedullary nailing or DHS or locking plate can be used for osteosynthesis at the femoral peritrochanteric region. In our case, 4 days post-operative, the patient was scheduled for surgical treatment of the right femoral fracture. The fracture was open reduced and fixed with a locking plate and bone grafting. 4 month post-operative, X-rays showed bone union at fracture site of right femur, with no secondary displacement.
It was reported that osteolytic lesions caused by brown tumor are recovered when hyperparathyroidism is treated. However, there is no clearly defined treatment for lesions that can induce pathological fractures developing in lower extremities. We agree with Park [10] that it is necessary to actively do the preventive fixation for brown tumor with Mirels' score with score ≥ 9. Mirels' score ≥ 9 indicates high risk of fracture and primary stabilizing should be recommended, ≤7: low risk of fracture. Mirels score is based on 4 categories: site (upper limb: 1 score, lower limb: 2 scores, peritrochanteric: 3 scores), pain (mild: 1 score, moderate: 2 scores, functional: 3 scores), lesion (blastic: 1, mixed: 2 scores, lytic: 3 scores), size (<1/3: 1 score, 1/3–2/3: 2 scores, >2/3: 3 scores) [12]. In our case, all brown tumors except right femoral peritrochanteric region had Mirels' score less than 7 scores that were applied a conservative treatment and their regression seen to be taking place in the upper limb, lower limbs and pelvis 4 months post-operative.
4. Conclusion
Brown tumor due to parathyroid carcinoma needs to be considered in the differential diagnosis when there are osteolytic lesions and high serum calcium. It is advisable to have a parathyroidectomy and then orthopaedic treatment. The principles of osteosynthesis of pathology fracture are based on stable osteosynthesis with or without bone graft. Brown tumor without pathological with Mirels' score less than 7 scores should be applied a conservative treatment. It is necessary to actively do the preventive fixation for brown tumor with Mirels' score ≥ 9.
Ethical approval
All procedures were approved by the 108 Central Military Hospital's Institutional Review Board, Hanoi, Viet Nam.
Funding
No financial support was received for the completion of this study.
CRediT authorship contribution statement
Dr. Gioi Nguyen Nang: Conceptualization, Surgery, Writing - Review & Editing, Supervision
Dr. Luong Nguyen Van: Conceptualization, Surgery, Writing - Review & Editing, Supervision.
Guarantor
Dr. Luong Nguyen Van.
Registration of research studies
Not applicable.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Availability of data and materials
The data used to support the findings of this study are available from the corresponding author upon request.
Declaration of competing interest
The authors declare that they have no conflicts of interest.
Acknowledgments
The authors would like to acknowledge with gratitude the precious help of colleagues and the health staff of the Institute of Trauma and Orthopaedics at the 108 Military Central Hospital for the time required to prepare and implement this study.
Contributor Information
Gioi Nang Nguyen, Email: nanggioi108@gmail.com.
Luong Van Nguyen, Email: luongbv108@yahoo.com.vn, luongnv108@gmail.com.
References
- 1.Keiler A., Dammerer D., Liebensteiner M., Schmitz K., Kaiser P., Wurm A. Pathological fracture of the tibia as a first sign of hyperparathyroidism - a case report and systematic review of the current literature. Anticancer Res. 2021;41(6):3083–3089. doi: 10.21873/anticanres.15092. Epub 2021/06/05. [DOI] [PubMed] [Google Scholar]
- 2.Garla V.V., Akhtar I., Salim S., Subauste A. Osteitis fibrosa cystica masquerading as bone neoplasm. BMJ Case Rep. 2018;2018 doi: 10.1136/bcr-2018-224546. Epub 2018/05/08. PubMed PMID: 29735505; PubMed Central PMCID: PMCPMC5950634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ngo Q.X., Ngo D.Q., Tran T.D., Le DT Hoang G.N., Le Q.V. Multiple brown tumors with primary hyperparathyroidism mimicking bone metastases [ ] Int. J. Surg. Case Rep. 2021;79:375–378. doi: 10.1016/j.ijscr.2021.01.002. Epub 2021/01/31. PubMed PMID: 33516054; PubMed Central PMCID: PMCPMC7847817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Agha R.A., Franchi T., Sohrabi C., Mathew G., Kerwan A., Group S The SCARE 2020 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. Epub 2020/11/13. [DOI] [PubMed] [Google Scholar]
- 5.Machado N.N., Wilhelm S.M. Parathyroid cancer: a review. Cancers (Basel) 2019;(11) doi: 10.3390/cancers11111676. Epub 2019/10/31. PubMed PMID: 31661917; PubMed Central PMCID: PMCPMC6896123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Xu W., Qu Y., Shi W., Ma B., Jiang H., Wang Y. Multiple bone brown tumor secondary to primary hyperparathyroidism: a case report and literature review. Gland Surg. 2019;8:810–816. doi: 10.21037/gs.2019.11.14. Epub 2020/02/12. PubMed PMID: 32042691; PubMed Central PMCID: PMCPMC6989901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rueda D.A., Nazionale B.A., Espinal Jimenez A.M., Carrozza D.A., Finocchietto P., Di Fonzo H. Tibial brown tumor as a presentation of primary hyperparathyroidism. Rev. Fac. Cien. Med. Univ. Nac. Cordoba. 2021;78(2):207–209. doi: 10.31053/1853.0605.v78.n2.30679. Epub 2021/06/29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Steadman H.E., Jernigan H.W. Parathyroid adenoma with fibrocystic skeletal changes resulting in pathologic fracture of the femur. J. Int. Coll. Surg. 1954;21(1 1):30–41. Epub 1954/01/01. PubMed PMID: 13118222. [PubMed] [Google Scholar]
- 9.Nasser M.L., Medawar S., Younan T., Abboud H., Trak-Smayra V. Osteitis fibrosa cystica mimicking bone tumor, a case report. BMC Musculoskelet. Disord. 2021;22(1):479. doi: 10.1186/s12891-021-04374-7. Epub 2021/05/27. PubMed PMID: 34034731; PubMed Central PMCID: PMCPMC8152144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Park S.H., Kong G.M., Kwon Y.U., Park J.H. Pathologic fracture of the femur in brown tumor induced in parathyroid carcinoma: a case report. Hip Pelvis. 2016;28(3):173–177. doi: 10.5371/hp.2016.28.3.173. Epub 2016/10/26. PubMed PMID: 27777921; PubMed Central PMCID: PMCPMC5067395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wieneke J.A., Smith A. Parathyroid adenoma. Head Neck Pathol. 2008;2(4):305–308. doi: 10.1007/s12105-008-0088-8. Epub 2008/12/01. PubMed PMID: 20614300; PubMed Central PMCID: PMCPMC2807581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jawad M.U., Scully S.P. In brief: classifications in brief: Mirels' classification: metastatic disease in long bones and impending pathologic fracture. Clin. Orthop. Relat. Res. 2010;468(10):2825–2827. doi: 10.1007/s11999-010-1326-4. Epub 2010/03/31. PubMed PMID: 20352387; PubMed Central PMCID: PMCPMC3049613. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data used to support the findings of this study are available from the corresponding author upon request.