Abstract
Chronic tophaceous gout is a common disease but rarely found in the head and neck region. Here we report a case of a middle aged male who presented with a mass over the right side of the nasal bridge. CT of the paranasal sinuses revealed a tophi lesion in the right nasal bridge with erosion of the underlying nasal bone. The mass was excised and histologically confirmed to be a gouty tophus. This case report illustrates how a common disease presented in an uncommon location could pose a diagnostic challenge.
Keywords: Gout, Head and neck, Computed tomography
Case report
A 62 year old male presented with a mass over the right side of the nasal bridge for 2 months. The mass was associated with mild pain. There was no history of trauma and the patient was asymptomatic otherwise. The patient has a past medical history of hypertension and gout. He has been diagnosed with gout in bilateral ankles for years which was treated with allopurinol and colchicine. Despite diet control and compliance with medications, the patient has persistent hyperuricemia(Urate level: 0.62 mmol/L). On physical examination, there was a 2 cm non–tender mass over the right side of the nasal bridge which was firm in texture and appeared separated from the skin. Apart from skin erythematous, there was no sign of active inflammation. Bilateral nostrils were patent.
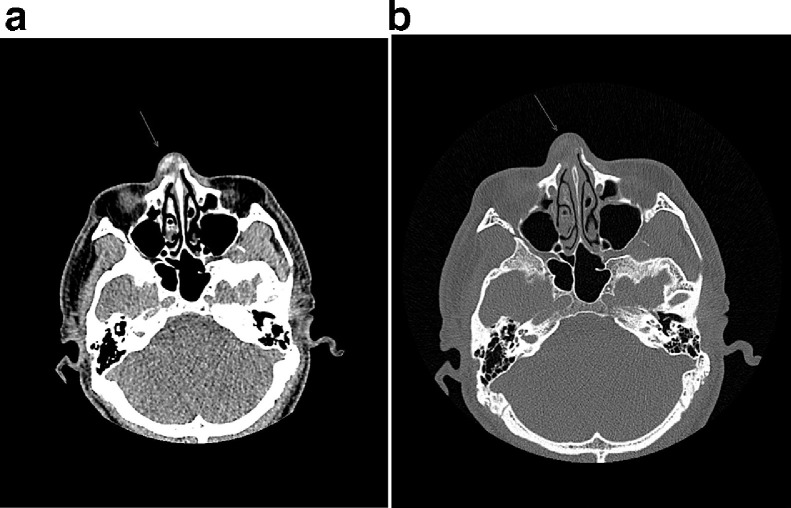
CT examination of the paranasal sinuses were obtained and are presented in Figs. 1 and 2.
Fig. 1.
(A,B) Axial plane CT paranasal sinuses show a 1.6 cm lesion containing hyperdensities. The lesion eroded and partially replaced the right nasal bone underneath.
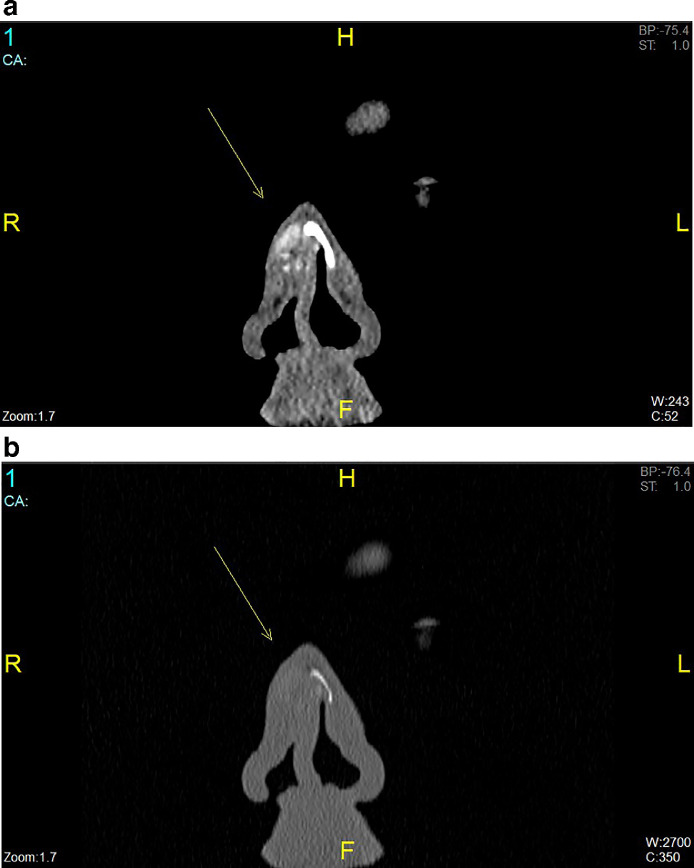
Fig. 2.
(A,B) Coronal plane of nasal bone in soft tissue and bone windows demonstrate the gouty tophus and nasal bone erosion.
It showed a well-defined mildly hyperdense roundish lesion centered over the right side of the nasal bridge with associated erosion in the right nasal bone. There was no intralesional calcification or cavitation. No similar lesion is seen elsewhere in the scanned region. The patient later underwent rhinoplasty and histology confirmed a diagnosis of gouty tophus. The histologic findings are presented in Fig. 3A and E.
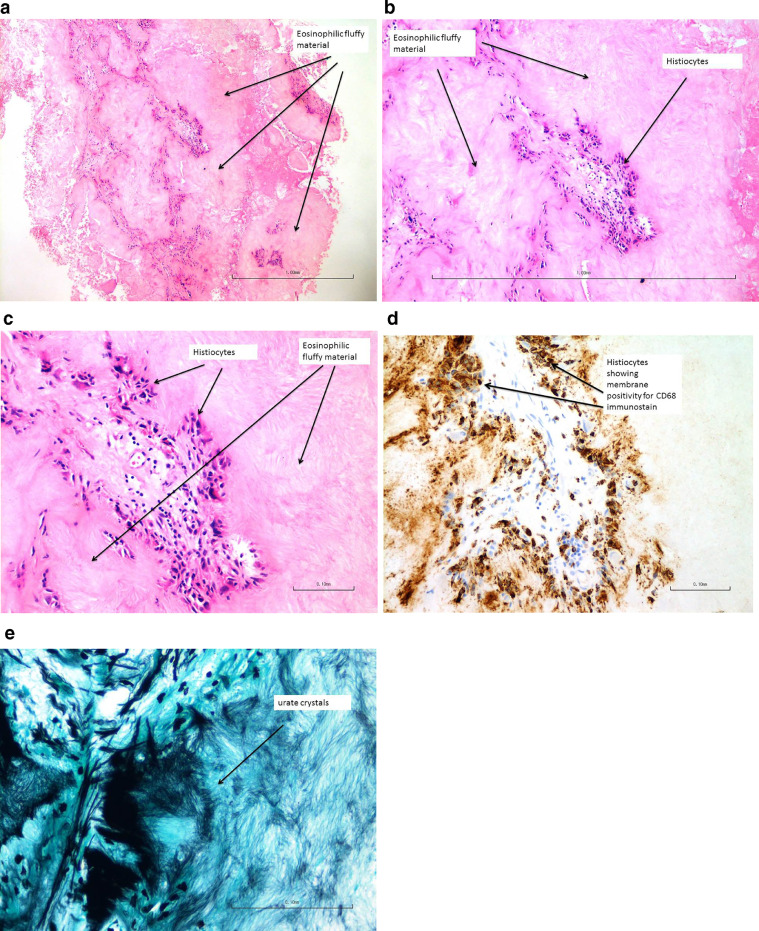
Fig. 3.
(A,B,C) H&E (hematoxylin and eosin) sections show multiple pieces of eosinophilic fluffy material surrounded by histiocytes, neutrophils and multinucleated giant cells. Features are consistent with foreign body reaction developed around gouty tophaceous deposits. (D) There is no evidence of malignancy. The histiocytes are highlighted by CD68 immunostaining. (E) Urate stain (silver impregnation) showed a small amount of urate crystals.
Discussion
Despite gout being the most common inflammatory arthritis [2], diagnosis of gout can be clinically challenging, especially if it presents in an atypical location. The gold standard in diagnosing gout is by demonstrating negatively birefringent, needle shaped monosodium crystal in tissue or synovial fluid by polarized microscopy [3]. However, histologic diagnosis is not always feasible and imaging is very helpful to establish a diagnosis. Furthermore, imaging has an important role in assessing the extent of disease and monitoring treatment response [3]. During the acute phase of the disease, only soft tissue swelling around the affected joint may be demonstrated on imaging. The typical radiographic finding in chronic gout includes well defined “punched-out” erosions with overhanging and sclerotic edges, radiodense soft tissue nodules (tophi) with or without calcifications and asymmetrical involvement [3]. The erosions are typically juxta-articular in location, but may be intraarticular, extra-articular, or intraosseous in location. The joint space is usually preserved until late in the disease [3].
Conventional CT are sensitive in detecting bony erosions and hyperdense tophi. However, these findings are non–specific. Dual energy CT is a relatively recent development in the imaging of gouty arthritis. The fundamental principle behind the use of dual energy CT is to image the lesion with 2 different energy levels and differentiate the lesion based on its relative absorption of X ray at different photon energy levels. In the cases of gout, dual energy CT can help differentiate urate and non–urate deposition with high sensitivity and specificity. This is particularly useful when joint aspirate is not feasible or in cases of extra-articular gout, where the monosodium urate deposits in the extra-articular tissues, such as tendons and bursae, may result in false negative results on joint aspirations [6].
The use of MRI in the evaluation of gout has not been studied extensively. Tophi appears on MRI as a predominantly intermediate signal mass on T1 weighted images, with variable signal on T2-weighting, depending on the calcium concentration, and fairly homogeneous enhancement. However, these findings are again not specific for gout [6].
The most common site affected by gout is the first metatarsal phalangeal joint, followed by the fifth MTP joint, mid foot and hand and wrist. Presentation of gout in the head and neck region is rare. According to a literature review, there were 7 documented cases of gouty tophus in the nasal bridge from 1978 to 2018 in English literature [5]. Other atypical locations of gout include sclera, nose, ears, heart valves, abdominal striae, and gouty panniculitis [4].
For mass presented in the nasal region, more common differential diagnosis includes skin cancer (squamous cell carcinoma, basal cell carcinoma, melanoma) and chondroid lesions. The high densities of gouty tophi in radiography and/or CT can sometimes be mistaken as chondroid matrix in chondroid lesion. Given the rarity of such presentations, many clinicians may not be comfortably making this diagnosis based on the clinical and imaging features and histopathological confirmation may be needed. In this case, our patient underwent rhinoplasty and excision of the nasal mass, from which the definitive diagnosis was made. Ultrasound guided fine needle aspiration cytology is a cosmetically less destructive alternative [5].
Management of gout is usually taken by lifestyle changes and urate lowering drugs [1]. Surgical excision of tophi is indicated if the lesion is limiting joint mobility, causing structural damage and for cosmetic reasons [4]. For nasal tophi, management options for reconstructing the nasal bone is dependent on the extent of the defect and patient's preference [4].
Conclusion
Gouty arthritis is the most common inflammatory arthritis. Prompt and accurate diagnosis are essential in controlling the disease and preventing further destruction. Chronic tophaceous gout can present a diagnostic challenge if it presents in an atypical location.
In such cases, it is crucial to keep a wide list of differential diagnosis and a diagnosis of gout should be considered in any patients with a background history of hyperuricemia.
Patient consent
All patient data has been removed and no informed consent is required to participate.
Footnotes
Competing Interests: The authors declare that they have no conflict of interests.
References
- 1.Ragab G, Elshahaly M, Bardinc T. Gout: An old disease in new perspective – A review. J Adv Res. 2017;8(5):495–511. doi: 10.1016/j.jare.2017.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dehlin M., Jacobsson L., Roddy E. Global epidemiology of gout: prevalence, incidence, treatment patterns and risk factors. Nat Rev Rheumatol. 2020;16:380–390. doi: 10.1038/s41584-020-0441-1. [DOI] [PubMed] [Google Scholar]
- 3.Chowalloor P, Siew T, Keen H. Imaging in gout: A review of the recent developments. Ther Adv Musculoskelet Dis. 2014;6(4):131–143. doi: 10.1177/1759720X14542960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chung-HanWu J, Pang-Yun C, Chih-Hao C. Nasal gouty tophus: Report a rare case presenting as a nasal hump with nasal obstruction. Biomed J. 2016;39(4):295–297. doi: 10.1016/j.bj.2016.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chen S, Chen J, Yang S. Painless gouty tophus in the nasal bridge. Case Rep Lit Rev Med. 2019;98(11):e14850. doi: 10.1097/MD.0000000000014850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chou H, Chin T, Peh Wilfred C. Dual-energy CT in gout – A review of current concepts and applications. J Med Radiat Sci. 2017;64(1):41–51. doi: 10.1002/jmrs.223. [DOI] [PMC free article] [PubMed] [Google Scholar]