Abstract
An encephalocele may be congenital or acquired and is characterized by the herniation of cranial contents through a skull bone defect. Most congenital encephaloceles occur in the occipital area, and temporal bone encephaloceles in children are rare. Congenital encephaloceles can be diagnosed either prenatally or after birth. We describe the case of a congenital temporal bone encephalocele in a 2-month-old boy that was diagnosed after birth. The patient presented with seizures and a bulging mass in the right neck that was detected by his mother during the second month after birth. The combined results from brain magnetic resonance imaging, computed tomography, and histological analysis confirmed the diagnosis of encephalocele. Although the surgical repair was offered, the family declined.
Keywords: Congenital encephalocele, Temporal bone, Bone defect, Neural tube defect
Introduction
An encephalocele is a herniation of the cranial contents outside of the skull, which is described as a meningocele when the herniation sac contains leptomeninges and cerebrospinal fluid (CSF) [1]. Congenital encephaloceles are a type of neural tube defect with an estimated incidence of 0.8–4 per 10,000 live births [2]. An acquired encephalocele occurs due to trauma, tumors, chronic otitis media, and postsurgery [3]. Genetic and environmental factors, including maternal infections; medications taken; or insufficient vitamin B12, folic acid, or mineral supplementation during the first trimester, are considered to be risk factors that contribute to encephalocele development [4]. This case report presents the imaging features of this rare congenital anomaly.
Case report
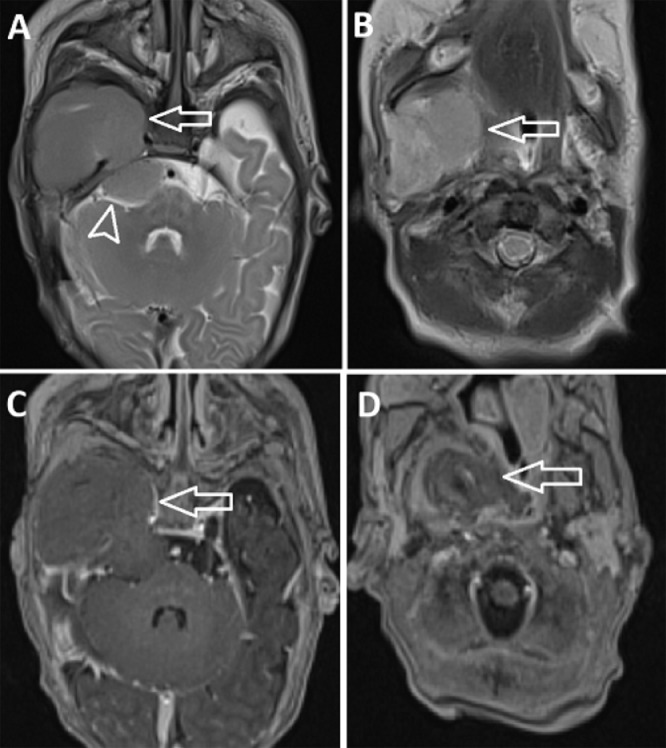
A 2-month-old male patient presented with seizures and a bulging mass in the right neck, which was detected by the patient's mother. The parents belong to an ethnic minority, and the mother did not attend medical check-ups during pregnancy. The pregnancy was full-term, with the patient born at 39 weeks of gestation. Physical examination showed early motor delays for the patient's age, no paralysis, and no epilepsy, and a soft mass in the right neck was identified, without skin color changes. Brain magnetic resonance imaging (MRI) showed a large mass in the right temporal lobe extending to the extracranial space, which caused a bulging mass in the right neck. We also detected that part of the tumor shifted downward into the posterior fossa (Fig. 1). The mass was hypointense on T1-weighted (T1W) images, intermediate intensity on T2-weighted (T2W) images, and not restricted on diffusion-weighted images. After a contrast agent was injected, the lesion enhanced heterogeneously, with central necrosis (Fig. 1).
Fig. 1.
A large mass in the right temporal lobe extended into the extracranial space, reaching the neck (A and B, arrows). Part of the tumor shifted downward into the posterior fossa (A, arrowhead). The lesion was intermediate on T2-weighted images and heterogeneously enhancing (C and D, arrows).
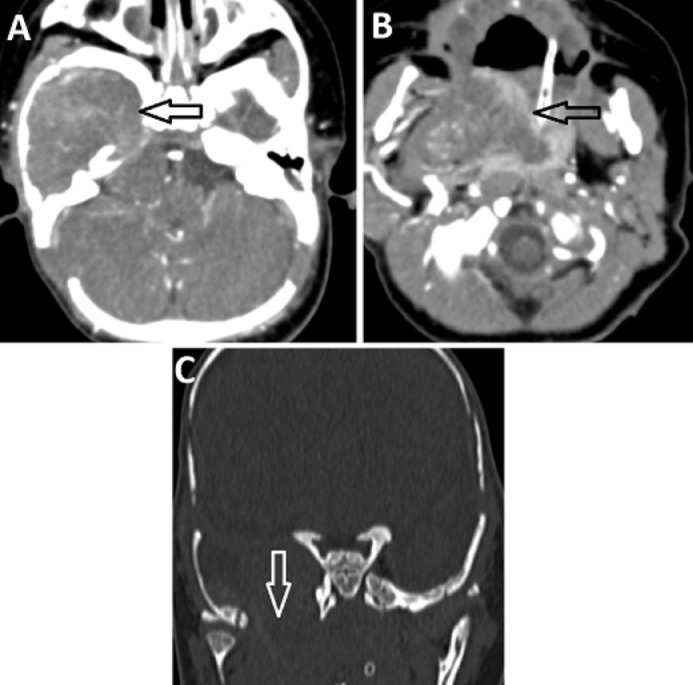
Brain computed tomography (CT) scan showed the mass was isodense compared with the normal brain parenchyma, heterogeneously enhancing, and the blood supply for the lesion originated from the middle cranial artery (Fig. 2). A large bone defect was detected in the right temporal bone, and the intracranial herniation of the brain tissues occurred through this defect (Fig. 2). Based on the MRI and CT results, we suspected the mass was an encephalocele. However, the lesion was heterogeneous and presented with central necrosis, which required the exclusion of a tumor in the sac hernia. The patient underwent a biopsy of the cervical lesion. Histopathology analysis revealed normal brain parenchyma without tumor cells. After multidisciplinary consultation, the patient was recommended to undergo surgery to remove the sac herniation and repair the bone defect. However, the family declined treatment.
Fig. 2.
The lesion was isodense with the normal brain parenchyma and heterogeneously enhancing on computed tomography (CT) scan (A and B, arrows). The right temporal bone defect can be observed on the CT bone window (C, arrow).
Discussion
Encephaloceles can be classified according to the location of the skull defect, involving the occipital, anterior, parietal, temporal, or vertex regions of the skull [2,5]. Most encephaloceles have been reported to occur in the occipital region [6]. Encephalocele may coincide with other anomalies, such as hydrocephalus, seizures, microcephaly, corpus callosal abnormalities, heterotopias, and cerebral dysgenesis [2]. A male predominance has also been noted for the occurrence of encephaloceles [4,6]. The two primary theories that have been proposed to describe the etiology of encephaloceles are weakness in the ossifying bone and delay in neural tube closure [1].
The clinical presentation depends on the encephalocele location, the size of the herniated sac, and the presence of other anomalies. Some symptoms associated with encephaloceles located at the anterior cranial base include nasal obstruction, CSF rhinorrhea, meningitis, hypertelorism, failure to thrive, feeding difficulties, facial deformities, polyuria, polydipsia, respiratory distress, and epilepsy [7]. Temporal lobe encephaloceles are often associated with seizures, otorrhea, rhinorrhea, hearing loss, and meningitis [8]. Occipital encephaloceles can present with developmental delays and mental disorders, seizures, and neurological deficits [9].
CT scans can be useful for detecting bony integrity and identifying the defect site [8]. Lesions in the hernia sac can appear with the same density as normal brain tissue [10]. A diagnosis of inflammation and tumor originating from the brain should also be considered [10]. On MRI, the herniated sac is indicated by the presence of brain tissue herniated through the bone defect, appears enhanced, and the lesion is typically bordered by high-signal CSF on T2W [3].
Surgery is the mainstay of treatment, with the aim of repairing the bone defect, ensuring the watertight closure of the dura, and removing nonfunctional brain tissue [11]. Surgery can be performed as open or endoscopic procedures and should be performed as soon as possible [1,11].
The prognosis of encephaloceles depends on the degree of brain herniation, such as the size of the hernia, the amount of brain tissue contained in the hernia sac, the association with other congenital anomalies, and the application of effective treatment [5]. Patients who present with encephaloceles may lack normal development, which can present with varying levels of severity, or they can present with normal development, depending on the size and location of the encephalocele [2].
The patient, in this case, was a boy who presented with early motor delays for his age. Due to the large temporal bone defect, the brain tissue herniation was large and manifested as a tumor. The brain tissue in the herniated sac was necrotic and nonfunctioning. On imaging, we were unable to recognize any normal structures of the brain parenchyma in the herniated sac. MRI and CT imaging provided useful findings that contributed to the diagnosis.
Conclusion
Congenital encephalocele describes the herniation of brain tissues through a defect in the cranium. CT and MRI scans are effective imaging modalities that can be used to identify the cause of herniation and exclude a tumor diagnosis. CT may also be used to assess the bone anomaly. Regular check-ups during pregnancy are necessary for the early diagnosis, planning, and management of congenital encephaloceles.
Ethical Statement
Appropriate written informed consent was obtained for the publication of this case report and accompanying images.
Author contributions
D-V.N. and N.M.D. contributed equally to this article as co-first authors. All authors have read the manuscript and agree to the contents.
Informed Consent
Informed consent for patient information to be published in this article was obtained.
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
Funding: Self-financed.
References
- 1.Gump WC. Endoscopic endonasal repair of congenital defects of the anterior skull base: developmental considerations and surgical outcomes. J Neurol Surg B Skull Base. 2015;76(4):291–295. doi: 10.1055/s-0034-1544120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lo BWY, Kulkarni AV, Rutka JT, Jea A, Drake JM, Lamberti-Pasculli M. Clinical predictors of developmental outcome in patients with cephaloceles. J Neurosurg Pediatr. 2008;2(4):254–257. doi: 10.3171/PED.2008.2.10.254. [DOI] [PubMed] [Google Scholar]
- 3.Papanikolaou V, Bibas A, Ferekidis E, Anagnostopoulou S, Xenellis J. Idiopathic temporal bone encephalocele. Skull Base. 2007;17(5):311-316. doi: 10.1055/s-2007-986429. [DOI] [PMC free article] [PubMed]
- 4.Yucetas SC, Uçler N. A retrospective analysis of neonatal encephalocele predisposing factors and outcomes. Pediatr Neurosurg. 2017;52(2):73–76. doi: 10.1159/000452805. [DOI] [PubMed] [Google Scholar]
- 5.Ghritlaharey RK. A brief review of giant occipital encephalocele. J Neurosci Rural Pract. 2018;9(4):455–456. doi: 10.4103/jnrp.jnrp_189_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ramdurg S, Sukanya M, Maitra J. Pediatric encephaloceles: a series of 20 cases over a period of 3 years. J Pediatr Neurosci. 2015;10(4):317. doi: 10.4103/1817-1745.174462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Thompson HM, Schlosser RJ, McCarty Walsh E. Current management of congenital anterior cranial base encephaloceles. Int J Pediatr Otorhinolaryngol. 2020;131 doi: 10.1016/j.ijporl.2020.109868. [DOI] [PubMed] [Google Scholar]
- 8.Morone PJ, Sweeney AD, Carlson ML. Temporal lobe encephaloceles: a potentially curable cause of seizures. Otol Neurotol. 2015;36(8):1439–1442. doi: 10.1097/MAO.0000000000000825. [DOI] [PubMed] [Google Scholar]
- 9.Rehman L, Farooq G, Bukhari I. Neurosurgical interventions for occipital encephalocele. Asian J Neurosurg. 2018;13(2):233–237. doi: 10.4103/1793-5482.228549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Agladioglu K, Ardic FN, Tumkaya F, Bir F. MRI and CT imaging of an intrasphenoidal encephalocele: a case report. Pol J Radiol. 2014;79:360–362. doi: 10.12659/PJR.890795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Velho V, Naik H, Survashe P. Management strategies of cranial encephaloceles: a neurosurgical challenge. Asian J Neurosurg. 2019;14(3):718–724. doi: 10.4103/ajns.AJNS_139_17. [DOI] [PMC free article] [PubMed] [Google Scholar]