Abstract
Introduction
Septic knee arthritis after elective arthroscopic procedures is a rare surgical emergency, with Pseudomonas aeruginosa even more rarely causing the infection. The treatment by arthroscopic debridement and lavage with diluted Povidone-Iodine has potential benefits that may be useful in improving the prognosis for patients. This case report discusses the potential benefits of using antiseptics like Povidone-Iodine in the washout of the affected joint.
Presentation of case
We present a patient with post arthroscopic septic knee arthritis caused by P. aeruginosa treated successfully by arthroscopic synovectomy and washout with normal saline and diluted povidone‑iodine, and prolonged antimicrobial therapy.
Discussion
Preceding reports of P. aeruginosa suggest intraoperative factors, postoperative factors, and host factors that may lead to this uncommon infection. There is controversy over the optimal management regarding arthroscopic versus open debridement, and the choice of the irrigating fluid.
Conclusion
The use of antiseptics like Povidone-Iodine in the washout procedure may lead to improved outcomes if used for a short controlled period of time and followed by copious irrigation with saline. Further studies must be done to determine the efficacy and risk-to-benefit ratio of this method.
Abbreviations: ml, milliliters; L, Litres; AP view, anteroposterior view; P. aeruginosa, Pseudomonas aeruginosa
Keywords: Septic arthritis, Pseudomonas Aeruginosa, Arthroscopy, Povidone-iodine, Case report
Highlights
-
•
Pseudomonas aeruginosa causing septic arthritis without any risk factors are unusual.
-
•
Treatment approach for septic knee arthritis is controversial.
-
•
The type of irrigating fluid used in septic arthritis washout is not well defined by international guidelines
-
•
Use of 2.5% Povidine-Iodine in joint lavage for a short time is safe and effective in treating septic arthritis.
1. Introduction
Septic knee arthritis is a rare complication of arthroscopic procedures [1] that requires prompt and aggressive management to preserve the joint, function, and prevent disability. The most common causative microbes are Staphylococcus aureus and Coagulase-negative Staphylococcus epidermidis [2]. P. aeruginosa is an uncommon source of such infections that happens as a result of inadequate sterilization of surgical instruments or contamination of wounds from swimming pools or hot tubs [2]. Initially, empiric antibiotics switched later to culture sensitive antibiotics is reasonable and acceptable for most health practitioners [3]. However, controversy exists whether open versus arthroscopic washouts [4], [5], single versus multiple procedures, and the type and quantity of the irrigating fluid [6]. To our knowledge joint lavage using diluted povidone‑iodine has not been reported in treating septic knee arthritis caused by P. aeruginosa. In this case report, we describe a patient presented to our private hospital with postoperative septic knee arthritis caused by P. aeruginosa following arthroscopic partial meniscectomy and managed successfully with arthroscopic washout with diluted povidone‑iodine.
2. Case presentation
This case follows 2020 SCARE guidelines for reporting of cases in surgery [7]. We describe a 50-year-old Middle Eastern male with no relevant medical-surgical history, working as a security guard, who presented to our clinic complaining of left knee pain, swelling, and limping after a twisting knee injury at work. He was diagnosed with a medial meniscus bucket handle tear based on magnetic resonance imaging (MRI) findings. After 4-weeks of failed conservative management, he was taken to the operating room for an arthroscopic partial meniscectomy performed by the author (S.T.D). He had an uneventful postoperative recovery, removal of stitches 8-days after the surgery, and was instructed to do exercises at home. Two-weeks after surgery, the patient presented to the clinic with a hot, swollen knee and limping. He denied fever, chills, or night sweats. Physical examination revealed a moderate effusion, hotness, limitation of range of motion, tenderness to touch, and healed portal wounds. The knee was aspirated at the clinic, which revealed 30 mL of turbid synovial fluid, which was sent for culture and analysis, in addition to laboratory studies. The studies revealed elevated C- reactive protein (CRP) of 32 (ref range 0-5 mg/L), normal ESR of 4 mm/hr (ref range 0-15 mm/hr), elevated serum white blood count (WBC) of 15.08 × 10^3/μL with 87.2% segmented neutrophils, and markedly elevated synovial WBCs. A provisional diagnosis of purulent septic arthritis was made, and the patient was admitted to the hospital, and the infectious disease was consulted. On the same day, a left knee arthroscopic washout and synovectomy was done by same surgeon utilizing 10 L of normal saline, and intraoperative cultures were taken before starting empiric intravenous antibiotics (Cefepime and Vancomycin), and then a redivac drain was inserted through the anterolateral skin portal.
Two days later, both cultures taken at clinic and in theatre revealed growth of P. aeruginosa. Physical examination revealed stable vital signs, but a hot and tender joint, and the patient had one spike of fever (38.7 C). The drain had collected 150 mL of purulent fluid suggesting ongoing infection. Infectious disease had switched the antibiotics according to culture susceptibilities to Levofloxacin and Ceftazidime, and a second arthroscopic washout was planned on the next day.
In the second operation, which was performed by the same surgeon. First, we have performed an arthroscopic washout with 5 L of normal saline. Second, we opted to irrigate the joint manually with 1 L of 5% povidone‑iodine and normal saline at a ratio of (1:1) using 60 mL syringes through alternating portals in the sequence of three syringes of diluted Povidone Iodine followed by three syringes of normal saline, limiting continuous cartilage exposure to this diluted 2.5% Povidone-Iodine to less than 45-seconds. Finally, we did a second arthroscopic washout utilizing another 5 L of normal saline, and then a redivac drain was inserted through the anterolateral portal [Fig. 1].
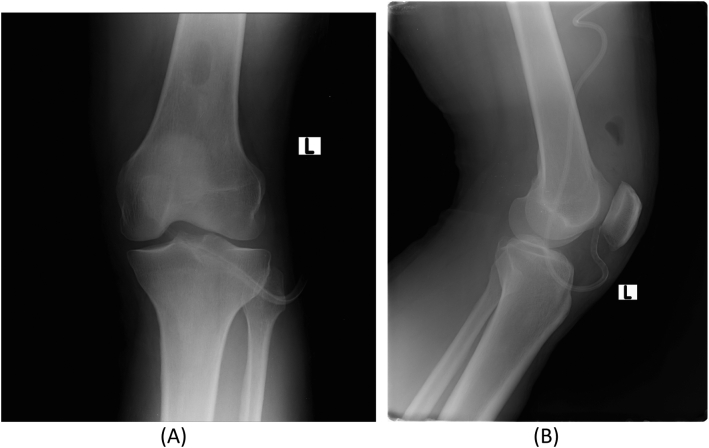
Fig. 1.
A) AP view of the left knee immediately after the second arthroscopic washout and debridement procedure, B) lateral view of the left knee immediately after the second arthroscopic washout and debridement procedure.
Thankfully, the patient improved after the second procedure as there were no pain, swelling, or other symptoms, and the drain was removed 24-hours later as there was no significant collection. Two-days postoperatively, immediate open chain knee exercises were initiated with the knee kept non-weight bearing for 1-week. One-week later, CRP level had normalized, and partial weight bearing started using crutches, and the patient was discharged home after 16-days of intravenous antibiotics on a 6-week course of oral levofloxacin with weekly repeat CRP test for 4-weeks, and then bi-weekly for another month which all were within normal levels. After 3-weeks, the patient was able to ambulate independently without crutches. The patient had full recovery at 6-weeks and was very satisfied. The patient was followed for 3-years clinically and radiographically which showed full recovery without any joint stiffness, pain, swelling, or signs of progressive degenerative arthritis [Fig. 2].
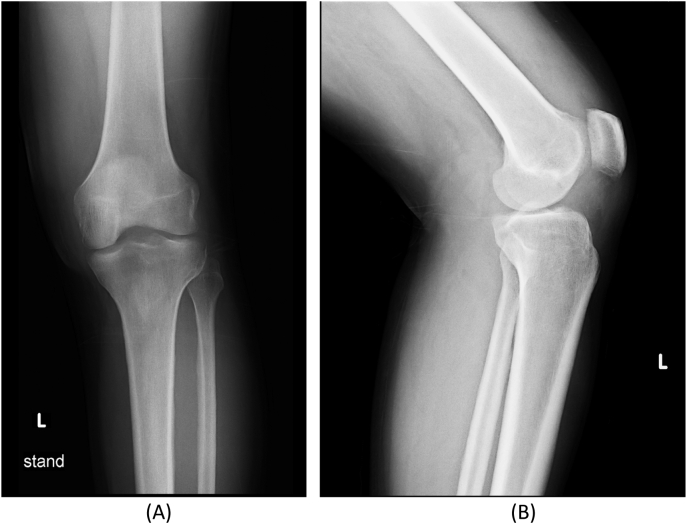
Fig. 2.
A) AP view of the left knee 3 years after surgery, B) lateral view of the left knee 3 years after surgery.
3. Discussion
Knee septic arthritis is an uncommon, but devastating complication of arthroscopic knee surgery [1], and its treatment is not defined clearly by any guidelines, which means surgeons are not instructed on how they should manage these cases [8]. The amount of normal saline used in arthroscopic washout isn't clearly defined, and the use of antiseptics in the washout hasn't been tested thoroughly to determine the toxic effects on native cartilage [9], [10]. These antiseptics have many advantages, including their ability to eradicate multi-drug resistant bacteria and the lack of resistance mechanisms by bacteria towards these antiseptics like Povidone Iodine [11], [12].
In our patient's case, the fact that he had an unusual microorganism (Pseudomonas aeruginosa) without any risk factors, that predispose patients to develop such infection (Old age, Immunocompromised status, Diabetes Mellitus, and IV drug abuse) [13], [14], and the failure of the first arthroscopic washout and debridement procedure, as well as the ineffective empirical antibiotic regimen that is directed at more commonly involved bacteria [2], [3]. This all lead to our decision, to use diluted Povidone-Iodine for less than 45-seconds [9] in the second arthroscopic lavage, since it is effective against orthopedic infections, cheap, available, and has no reported adverse effects [15], followed by copious irrigation with normal saline.
Previous studies confirmed the safety and efficacy of Povidine-Iodine lavage in treating various orthopedic and periprosthetic Joint infections [15], [16], however, there is paucity of literature on treating septic arthritis in native joints utilizing lavage with antiseptics. We believe that there must be further studies that explore the use of disinfectants like Povidone-Iodine in the treatment of knee septic arthritis with completely native cartilage.
4. Conclusion
Septic arthritis of the native knee post arthroscopy is a condition that requires definitive management in a timely manner, which could be achieved by a combination of treatments that include antibiotics, and open or arthroscopic washout and debridement. We believe that the use of antiseptics like diluted Povidone-Iodine in the washout procedure is safe, and will lead to improved outcomes, if used for a controlled period of time, followed by copious irrigation with saline. Further studies must be done to determine the efficacy and risk-to-benefit ratio of this method, in order to guide physicians to a better approach to the treatment of septic arthritis, which may lead to improved outcomes, and lessen the number of washouts required to eradicate such infections.
Funding
Not applicable.
Ethical approval
Ethical approval for this case report has been exempted by our institution.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Registration of research studies
Not applicable.
Guarantor
Dr. Salah Tewfik Daradkeh.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Registration of research studies
N/A.
CRediT authorship contribution statement
Salah Tewfik Daradkeh: study design, data collection, data analysis, conceptualization, and writing the paper.
Mohammad Jamal Abunasser: data analysis, conceptualization, and writing the paper.
Yazan Tawfiq Daradkeh: writing the paper.
Mohammad Suleiman Olimat: writing the paper.
Waleed F Dabbas: writing the paper.
Alaa Akel: reviewing the paper.
Declaration of competing interest
We report no conflicts of interest.
Contributor Information
Salah Tewfik Daradkeh, Email: salah.daradkeh@yu.edu.jo.
Waleed F. Dabbas, Email: waleed.dabbas@bau.edu.jo.
Alaa Akel, Email: alaakel@mutah.edu.jo.
References
- 1.Balato G. Knee septic arthritis after arthroscopy: incidence, risk factors, functional outcome, and infection eradication rate. Joints. 2017;5(2):107. doi: 10.1055/s-0037-1603901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shirtliff Mark E., Mader Jon T. Acute septic arthritis. Clin. Microbiol. Rev. 2002;15(4):527–544. doi: 10.1128/CMR.15.4.527-544.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ascione T. Post-arthroscopic septic arthritis of the knee. analysis of the outcome after treatment in a case series and systematic literature review. Eur. Rev. Med. Pharmacol. Sci. 2019;23(2 Suppl):76–85. doi: 10.26355/eurrev_201904_17477. [DOI] [PubMed] [Google Scholar]
- 4.Johns Brenton P., Loewenthal Mark R., Dewar David C. Open compared with arthroscopic treatment of acute septic arthritis of the native knee. JBJS. 2017;99(6):499–505. doi: 10.2106/JBJS.16.00110. [DOI] [PubMed] [Google Scholar]
- 5.Acosta-Olivo Carlos. Comparison of open arthrotomy versus arthroscopic surgery for the treatment of septic arthritis in adults: a systematic review and meta-analysis. Int. Orthop. 2021:1–13. doi: 10.1007/s00264-021-05056-8. [DOI] [PubMed] [Google Scholar]
- 6.Liu Cheryl L.S., Hall Andrew C. Optimizing the composition of irrigation fluid to reduce the potency of Staphylococcus aureus a-toxin: potential role in the treatment of septic arthritis. Cartilage. 2020;11(4):500–511. doi: 10.1177/1947603518798888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Agha R.A., Sohrabi C., Mathew G., Franchi T., Kerwan A., O’Neill N. The PROCESS 2020 guideline: updating consensus Preferred Reporting Of CasESeries in Surgery (PROCESS) guidelines. Int. J. Surg. 2020;84(4):231–235. doi: 10.1016/j.ijsu.2020.11.005. [DOI] [PubMed] [Google Scholar]
- 8.Cho Hyung J., Burke Leah A., Lee Mikyung. Septic arthritis. Hosp. Med. Clin. 2014;3.4:494–503. [Google Scholar]
- 9.von Keudell Arvind, Canseco Jose A., Gomoll Andreas H. Deleterious effects of diluted povidone–iodine on articular cartilage. J. Arthroplast. 2013;28(6):918–921. doi: 10.1016/j.arth.2013.02.018. [DOI] [PubMed] [Google Scholar]
- 10.Kataoka Masashi. Toxic effects of povidone–iodine on synovial cell and articular cartilage. Clin. Rheumatol. 2006;25(5):632–638. doi: 10.1007/s10067-005-0133-x. [DOI] [PubMed] [Google Scholar]
- 11.Lepelletier Didier. Povidone iodine: properties, mechanisms of action, and role in infection control and Staphylococcus aureus decolonization. Antimicrob. Agents Chemother. 2020;64:9. doi: 10.1128/AAC.00682-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lachapelle Jean-Marie. Antiseptics in the era of bacterial resistance: a focus on povidone iodine. Clin. Pract. 2013;10.5:579. [Google Scholar]
- 13.Keynes Stuart A., Due Steven L., Paul Biju. Pseudomonas arthropathy in an older patient. Age Ageing. 2009;38(2):245. doi: 10.1093/ageing/afn300. [DOI] [PubMed] [Google Scholar]
- 14.Wang Ching-Chun. Pseudomonas aeruginosa costovertebral arthritis in association with spontaneous cervical spondylodiscitis and epidural abscesses in the elderly. J. Clin. Gerontol. Geriatr. 2012;3(2):82–86. [Google Scholar]
- 15.Ruder J.A., Springer B.D. Treatment of periprosthetic joint infection using antimicrobials: dilute povidone-iodine lavage. J. Bone Joint Infect. 2017;2:10–14. doi: 10.7150/jbji.16448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Goswami K., Austin M.S. Intraoperative povidone-iodine irrigation for infection prevention. Arthroplasty Today. 2019;5(3):306–308. doi: 10.1016/j.artd.2019.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]