Abstract
Background
Digital mental health services (DMHS) provide highly accessible psychological supports and interventions that can supplement existing mental health services. Concerns about the mental health impact of the COVID-19 pandemic have been widespread and provide a unique impetus to examine the utility and responsivity of DMHS. This study examined the service utilisation and user characteristics of two DMHS (THIS WAY UP and Just a Thought) in Australia and New Zealand before and during the early pandemic period in these countries (March to June 2020).
Methods
Service use indices (website visits, course registrations and prescriptions, clinician registrations) were compared across different time periods before (12, 6 and 3 months) and during the pandemic in Australia and New Zealand. The demographic and clinical characteristics of course registrants (anxiety and depression symptom severity and psychological distress) were also compared across the pre- and during-COVID periods.
Results
Comparing pre-COVID to during-COVID time periods, we observed substantial increases across all service use indices in both DMHS (increases of >100% on the majority of service use indices). For example, in the 3 months prior to the pandemic, 2806 people registered for a THIS WAY UP course and 1907 people registered for a Just a Thought course, whereas 21,872 and 5442 registered for a THIS WAY UP and Just a Thought course, respectively, during the first 3 months of the COVID pandemic. Slight differences in the demographic and clinical profiles of course registrants were found between pre- and during-COVID time periods, with limited evidence of elevated anxiety and depression symptom severity in the COVID period.
Conclusions
Following the outbreak of COVID-19 in Australia and New Zealand, the volume of users accessing DMHS increased yet the demographic and clinical characteristics of course registrants remained stable. Results underscore how nimble and scalable DMHS can be during periods of high demand.
Keywords: COVID-19, Anxiety, Depression, Digital mental health service, Internet, Cognitive behaviour therapy
Highlights
-
•
Uptake of digital mental health services substantially increased during COVID-19.
-
•
Most users undertook self-guided courses for anxiety and depression symptoms.
-
•
Results highlight the utility and scalability of digital mental health services.
1. Introduction
The rapid spread of the Coronavirus disease-2019 (COVID-19) and the extensive measures undertaken to contain its transmission has produced profound effects. The impact on public health and global economies has been substantial (e.g., International Monetary Fund, 2020; Sachs et al., 2020). There have also been serious concerns about the impact on mental health and wellbeing (e.g., Holmes et al., 2020; Luo et al., 2020), with some studies indicating an increase in the prevalence of clinically significant symptoms of anxiety, depression, and psychological distress during the pandemic (Pierce et al., 2020; Rossell et al., 2021; Wu et al., 2020).
In response to the growing need for mental health interventions, governments and healthcare systems across the globe have sought to deliver services in more accessible and scalable ways via telehealth and digital mental health services (DMHS) (Fisk et al., 2020; Gratzer et al., 2020). The effectiveness of DMHS and their capacity for rapid dissemination has been explored over many years prior to the outbreak of COVID-19 (e.g., Andrews et al., 2018; Carlbring et al., 2018). With such large numbers of individuals possibly experiencing elevated psychological distress, DMHS represent one low-intensity, highly scalable option to support the wellbeing of communities and supplement existing face-to-face mental health services which may have difficulties meeting rising mental health needs (Andersson et al., 2020; Torous et al., 2020; Wind et al., 2020). Recent studies examining service utilisation in one DMHS (the MindSpot Clinic) in the early months of COVID-19 in Australia (March–June 2020), showed an 89% increase in website visits, 90% increase in telephone calls, and a 16.7% increase in mental health assessments compared to 2019 (Titov et al., 2020; Staples et al., 2020). Compared to individuals accessing the service prior to the pandemic, no significant increases in levels of depressive symptom severity, psychological distress or suicidal ideation were observed in users of the MindSpot Clinic during the COVID period, and the small, initial elevation in anxiety symptom severity did not persist (Staples et al., 2020; Titov et al., 2020). It is likely that the increased consumption of DMHS may be related to disruptions to existing face-to-face service provision as well as the increased promotion and funding of remotely-delivered mental health interventions during the pandemic (e.g., Jayawardana and Gannon, 2021). The COVID pandemic has provided an unprecedented impetus to implement and enhance DMHS capabilities, as well as explore their utility and responsivity at a crucial moment in time (Andersson et al., 2020; Poulton et al., 2020). It is essential to continue exploring patterns of DMHS utilisation as the consumption of these services may increase as global mental health needs increase.
Accordingly, this study examined service utilisation and user characteristics from two DMHS in the early months of the COVID-19 pandemic in Australia and New Zealand (March–June 2020). The Australian service was THIS WAY UP and the New Zealand service was Just a Thought. Consistent with the experience of other Australian DMHS (Staples et al., 2020), we expected to find significant increases in service utilisation associated with the spread of the pandemic in Australia and New Zealand, but we did not expect to observe meaningful differences in the demographic and clinical characteristics of course registrants between the pre- and during-COVID groups.
2. Material and methods
2.1. Settings
2.1.1. THIS WAY UP
THIS WAY UP delivers online psychological education and support to individuals experiencing symptoms of anxiety and depression (see thiswayup.org.au).1 The service is an initiative of St Vincent's Hospital, Sydney, and the University of New South Wales, and is funded by the Australian Department of Health. THIS WAY UP courses are based on cognitive behaviour therapy (CBT) and mindfulness techniques and include eight disorder-specific courses (specifically, for social anxiety disorder, obsessive compulsive disorder, depression, generalised anxiety disorder, panic disorder, health anxiety, post-traumatic stress and chronic pain) and five transdiagnostic courses (for mixed anxiety and depression). THIS WAY UP also provides four wellbeing courses that address sleep difficulties, life stress, mindfulness skills, and student wellbeing. Wellbeing courses are brief and teach general coping skills rather target symptoms of specific mental health disorders. Each THIS WAY UP course involves a series illustrated comic-style lessons that follow the story of a fictional character who is experiencing mental health challenges. During the course, each character learns about their symptoms, how they are maintained, and how they can be managed using CBT and mindfulness-based skills. A summary with homework exercises is provided at the end of every lesson in order to reinforce course content and to help course users practise the therapy skills in their everyday lives.
THIS WAY UP courses are self-guided or guided by the user's clinician (although referral to the service is not required). Clinicians can ‘prescribe’ courses to their patients and integrate it within their routine care. Most courses are available as a free or low-cost service to Australian residents over the age of 18 years, with one course available for people as young as 12 years old (under adult supervision). Service users were advised that the THIS WAY UP courses may be less likely to be beneficial if users 1) were being treated with benzodiazepines or atypical anti-psychotics; 2) had an alcohol or substance use disorder; 3) had schizophrenia or bipolar affective disorder; or 4) were actively suicidal. However, adhering to these recommendations was at the discretion of the individual user and their clinician (i.e., these recommendations were not exclusion criteria). Over 30 randomized controlled trials have demonstrated the safety and effectiveness of THIS WAY UP courses (e.g., Kladnitski et al., 2020; Loughnan et al., 2019; Smith et al., 2019, and see crufad.org/our-research/). In response to the COVID-19 pandemic and with the support of the St Vincent's Hospital's Inclusive Health Foundation, all THIS WAY UP courses were free to access between 25th March 2020 and 30th June 2020.2 On 5th of April 2020, COVID-specific wellbeing resources were made available. A series of brief national media engagements promoted the service in April 2020 (and included one newspaper article, one television news story, and one radio interview).
2.1.2. Just A Thought
Just a Thought was launched in September 2019 and provides free access to online psychological education and support to New Zealanders (see www.justathought.co.nz). Just a Thought is a self-funded entity of the Wise Group, one of New Zealand's largest non-government mental health care providers. The service currently provides culturally-adapted versions of two THIS WAY UP courses: the generalised anxiety course and the depression course. Adaptations of the original courses did not alter CBT components but included tailoring of design features, character personas and language to the New Zealand context (e.g., incorporating national colloquiums, semantics, symbols, images, and environments [including those of Māori and Pasifika peoples]). Cultural adaptations are thought to support the acceptability, effectiveness, and appropriateness of mental health interventions (see Gearing et al., 2013; Spanhel et al., 2020). Courses are only available to New Zealand residents aged ≥16 years with both course available as self-guided or guided by the user's clinician in routine care settings. Just a Thought does not have additional exclusion criteria, however, makes recommendations that people who are experiencing severe distress and/or suicidal ideation, or are utilising medications with overly sedating side effects may not benefit or may require additional support from a clinician. No referral is required to access the courses. To encourage broad public utilisation of the service, Just a Thought undertook nation-wide marketing and promotional activities during its launch, including support and promotion by government. Secondary promotional efforts were directed towards healthcare workers and encouraged integration of courses into routine care. During the first COVID-19 lockdown in New Zealand in April 2020, the Ministry of Health partial funded the development of Just a Thought's specific COVID-19 course called ‘Staying on Track’. This course was included in New Zealand's initial psychosocial response to the pandemic which resulted in extensive national promotion of Just a Thought from April to September 2020 (specifically, direct-to-public promotion via print, television, online and/or radio media outlets, as well as marketing across a range of government and non-governmental public health organisations).
2.2. Study design
The purpose of this study was to examine changes in use of THIS WAY UP and Just a Thought associated with the early months of the COVID-19 pandemic. We compared service utilisation levels and user characteristics for the DMHS ‘during COVID’ (12th March 2020-11th June 2020, the 3 months following confirmation of the COVID-19 pandemic by the World Health Organisation, consistent with Staples et al., 2020 and Titov et al., 2020) to service utilisation levels and user characteristics in three ‘pre-COVID’ periods. These three ‘pre-COVID’ periods included: 1) 0–3 months prior to the COVID period (12th December 2019 to 11th March 2020); 2) 3–6 months prior to the pandemic period (12th September 2019 to 11th December 2019); and 3) 9–12 months prior to the pandemic period (12th March 2019 to 11th June 2019; i.e., the same 3-month period as the during-COVID period one year earlier). Note that this final comparator group was not available for Just a Thought as the service was launched in September 2019. We used multiple pre-COVID periods as comparisons for the during-COVID period because some instability in service use across time periods was expected due to the launch of Just a Thought in September 2019 and seasonal factors such as the extended summer/Christmas holiday period in both countries from December to February and the severe ‘Black Summer’ bushfires experienced across Australia in mid/late 2019 to early 2020.
2.3. Participants
Participants were THIS WAY UP and Just a Thought users who engaged with the services between 12 March 2019 and 11 June 2020. This study was conducted as part of the routine quality assurance activities of the DMHS. Prior to enrolment, THIS WAY UP users provided electronic informed consent that their pooled de-identified data would be collected, analysed and published for quality assurance and research purposes by agreeing to the Terms of Use and Privacy Policy of the service (St Vincent's Hospital Human Research Ethics Committee, 2020/ETH03027). Similarly, Just a Thought course users provided electronic informed consent that their aggregated, non-identifiable data would be collected, analysed and published for research purposes by agreeing to the Privacy Policy of Just a Thought (formal research ethics review was not required or sought by Just a Thought as the study fell within the quality assurance activities of the Wise Group).
2.4. Measures of service utilisation and user characteristics
2.4.1. Service utilisation
DMHS utilisation was estimated via five indices: the number of unique webpage views, the number of (unique) users who registered for a course, the number of clinicians who registered with the service for the first time (i.e., new clinicians who had not previously registered with the DMHS), the number of courses that were prescribed by registered clinicians, and the number of times COVID-specific resources were accessed. Note that users could register for multiple courses. To provide the most conservative estimate of service utilisation, current estimates are based on unique users (i.e., only one course registration was counted for each registrant).
2.4.2. User characteristics
2.4.2.1. Demographic characteristics
To register for a THIS WAY UP or Just a Thought course, individuals created an account on the website (www.thiswayup.org.au or www.justathought.co.nz) and reported their gender and age. Users could choose to report their postcode and, for THIS WAY UP users, where they had heard about the service. The Australian Statistical Geography Standards (Australian Bureau of Statistics, 2013) were used to classify THIS WAY UP users as residing in major cities or rural, regional or remote communities. The Urban Rural 2020 Generalised Dataset (New Zealand Geographic Data Service, 2020) was used to classify Just a Thought users as residing in major cities or rural communities.
2.4.2.2. Clinical characteristics
Course registrants who commenced a THIS WAY UP or Just a Thought course completed measures of symptom severity, which we used to assess users' clinical characteristics. The administration of measures was dependent on the course selected (i.e., core symptomatology was assessed, but to minimize user burden, not every measure was administered in every course). The most commonly completed measures (and those included in this evaluation) comprised the Kessler Psychological Distress Scale (K-10), Patient Health Questionaire-9 (PHQ-9) and Generalized Anxiety Disorder-7 (GAD-7), with a small subset of THIS WAY UP users (those undertaking a mindfulness-based course) completing the Short Warwick-Edinburgh Mental Well-being Scale (SWEMWBS). Completion of questionnaires was optional, and users could access courses without undertaking any measures.
The Kessler Psychological Distress Scale (K-10) is a 10-item measure of psychological distress experienced in the preceding two weeks with each item rated as either “none”, “a little”, “some”, “most” or “all” of the time (Kessler et al., 2002). Total scores ≥20 indicate probable mental disorder(s) (Andrews and Slade, 2001) with total K-10 scores of 10–19, 20–24, 25–29 and 30–50 indicative of no, mild, moderate and severe mental health problems, respectively (Australian Bureau of Statistics, 2003). Evidence of internal consistency (α = 0.93), test re-test reliability (r = 0.80 over 1–2 weeks), convergent and discriminant validity, and treatment sensitivity has been provided (Furukawa et al., 2003; Merson et al., 2021; Sunderland et al., 2012).
The Patient Health Questionaire-9 (PHQ-9) is a 9-item self-report screening tool for probable major depressive disorder (MDD) in the preceding two weeks (Kroenke et al., 2001). Respondents rate their symptoms as “not at all”, “on several days”, “on more than half the days” or “on nearly every day” with total scores ≥10 indicating probable MDD (Kroenke et al., 2001). Evidence of internal consistency (α = 0.79) and test-retest reliability (r = 0.84 over 48 h) has been provided, as has evidence of convergent, divergent, and criterion validity, and treatment sensitivity (Kroenke et al., 2001).
The Generalized Anxiety Disorder-7 (GAD-7) is a self-report screener for generalised anxiety disorder (GAD). Respondents reported how often they experience symptoms in the past two weeks as either “not at all”, “on several days”, “on more than half the days” or “on nearly every day”. Total scores ≥10 are indicative of a probable GAD diagnosis (Spitzer et al., 2006). Studies have provided evidence to support the reliability (α = 0.92, ICC = 0.83 over one week) and validity of the GAD-7 (e.g., convergent/divergent validity; criterion validity with respect to diagnosis via structured interview; treatment sensitivity) (Löwe et al., 2008; Newby et al., 2013; Spitzer et al., 2006).
The Short Warwick-Edinburgh Mental Well-being Scale (SWEMWBS) is a 7-item measure of mental wellbeing for the general population (Tennant et al., 2007). Each item (e.g., optimism about future) is scaled from 1 to 5, with higher scores indicating better wellbeing. Ng Fat et al. (2017) have proposed cut-scores for ‘low’ (total scores = 7–19.3), ‘medium’ (total scores = 20.0–27.0) and ‘high’ (total scores = 28.1–35) wellbeing. Evidence supporting internal reliability (α = 0.83–0.93) and temporal stability (r = 0.72 over 1 week) has been reported, as has evidence supporting the measure's convergent/divergent validity, criterion validity, and treatment sensitivity (Bartram et al., 2013; Ng Fat et al., 2017; Shah et al., 2018).
2.5. Analyses
2.5.1. Service utilisation before and during the COVID-19 pandemic
THIS WAY UP website activity from Australia and Just a Thought website activity from New Zealand was extracted from Google Analytics on 25th August 2020 and 25th November 2020, respectively. All analyses were performed in SPSS v26.0.
To estimate service utilisation in the DMHS, we first counted the unique number of 1) webpage views of THIS WAY UP and Just a Thought; 2) people who registered for a course, 3) new clinicians who registered with the service, and 4) courses that were prescribed by registered clinicians. So that service use during the pandemic could be compared to service use prior to the pandemic, these counts were conducted in the aforementioned 3-month time periods, specifically, during the COVID pandemic in Australia and New Zealand (12th March 2020- 11th June 2020), 0–3 months prior to the COVID period (12th December 2019 to 11th March 2020), 3–6 months prior to the pandemic period (12th September 2019 to 11th December 2019), and 9–12 months prior to the pandemic period (12th March 2019 to 11th June 2019). To estimate COVID-related differences in service utilisation across time periods, we computed the percentage change in each service use count comparing the COVID period to each of the pre-COVID periods. As in Titov et al. (2020) and Staples et al. (2020), % increase in service use during COVID = (during-COVID period count / pre-COVID comparison period count) − 1.
2.5.2. Characteristics of DMHS course registrants before and during the COVID-19 pandemic period
To estimate differences in demographic and clinical characteristics across the pre-COVID and during-COVID groups within THIS WAY UP, χ2 tests and one-way ANOVAs were utilised. For THIS WAY UP categorical variables, an omnibus χ2 test of the four groups of course registrants (3 pre-COVID and one during-COVID group) was conducted followed by three planned pairwise contrasts comparing the during-COVID with the three pre-COVID groups separately (using adjusted p value of .0167 [0.05/3]). For THIS WAY UP continuous variables, an omnibus one-way ANOVA estimated differences across the four groups, followed by three a-priori pairwise comparisons between the during-COVID group and each of the three pre-COVID groups separately (adjusted p = .0167 [0.05/3]). For the Just a Thought service, differences in demographic and clinical characteristics across the two pre-COVID groups and one during-COVID group were also estimated with χ2 tests and independent samples t-tests.
3. Results
3.1. Service utilisation before and during the COVID-19 pandemic
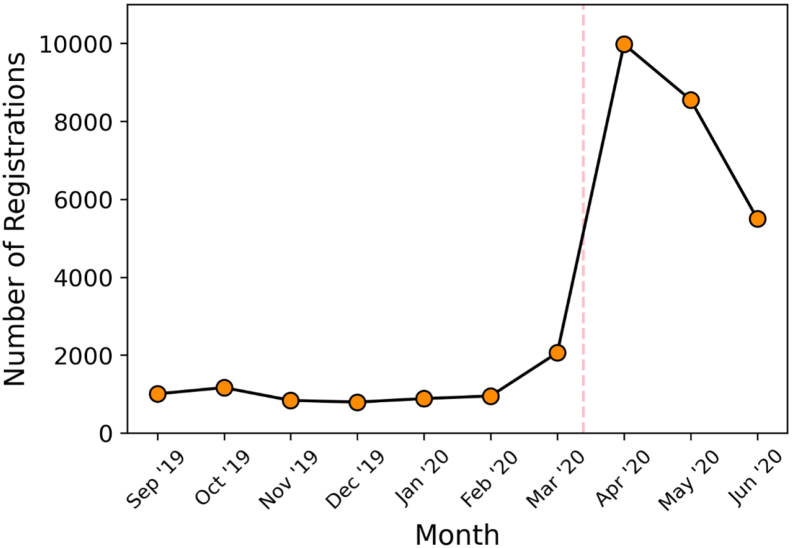
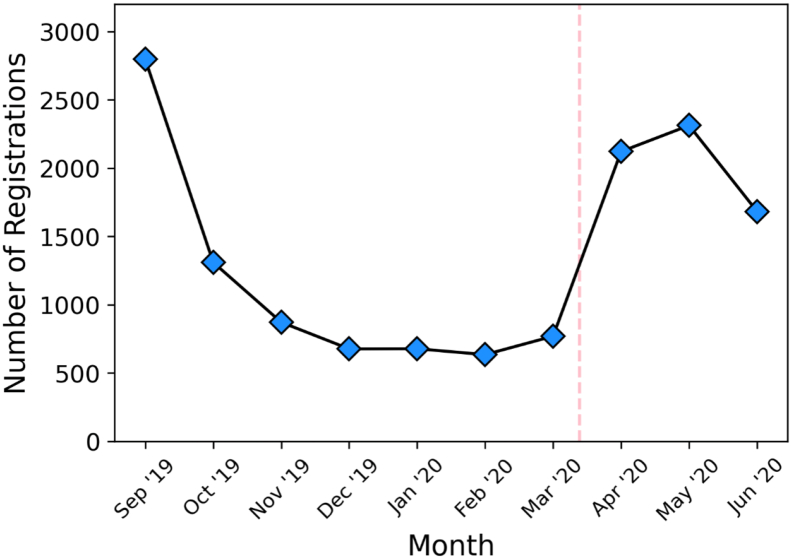
Fig. 1, Fig. 2 show the number of unique THIS WAY UP and Just a Thought course registrations in each whole month leading up to and during the COVID-19 pandemic in Australia and New Zealand (1st September 2019 to 30th June 2020). Fig. 1, Fig. 2 clearly demonstrate that there were large increases in the number of monthly course registrations from March to April 2020 in both services which coincided with the WHO's confirmation of the pandemic and the time when Australia and New Zealand implemented their national containment measures for the first time, i.e., border closures, supervised quarantine, strict social distancing. Course registrations peaked in April for THIS WAY UP and in May for Just a Thought. Course registrations in both DMHS then gradually decreased in June 2020, although counts of registrations remained consistently elevated compared to the pre-COVID period.
Fig. 1.
THIS WAY UP number of unique Australian course registrations in the months leading up to and during the COVID-19 pandemic in Australia (1st September 2019–30th June 2020). The dashed line indicates the date when COVID-19 was declared a pandemic by the World Health Organisation (12/03/2020).
Fig. 2.
Just a Thought number of unique New Zealand course registrations in the months leading up to and during the COVID-19 pandemic in New Zealand (1st September 2019–30th June 2020). The dashed line indicates the date when COVID-19 was declared a pandemic by the World Health Organisation (12/03/2020).
Table 1 provides estimates of service utilisation for the pre-COVID and during-COVID periods in the DMHS, and clearly shows that service utilisation significantly increased during the COVID period relative to the pre-COVID time periods. Compared to all three pre-COVID time periods, consistent increases in service use indices, especially course registrations, were observed for the THIS WAY UP service during the early COVID period in Australia. THIS WAY UP service use in the 3 months prior to the COVID period tended to be lower than the other pre-COVID periods. It is likely that this reduced service use is due to the summer holiday and bushfire season that occurred in Australia over December 2019 to February 2020. It is possible that seasonal factors may be particularly associated with counts of new clinician registrations and course prescriptions. As seen in Table 1, compared to the other pre-COVID periods, counts of clinician registrations at THIS WAY UP were lower during the summer holiday period (0–3 months before COVID) while counts of course prescriptions were higher. This suggests that during the summer holiday period in Australia, fewer new clinicians were signing up for the service, although overall, clinicians were prescribing more courses for their patients to do. Nevertheless, the number of new clinicians registering for THIS WAY UP and the number courses prescribed by clinicians dramatically increased during the early COVID period in Australia (by ~400–500%) compared to previous time periods.
Table 1.
Service utilisation of unique THIS WAY UP and Just a Thought users for the during-COVID period versus the three pre-COVID periods.
| Counts of service use in each period |
% increases in service use during the COVID period |
||||||
|---|---|---|---|---|---|---|---|
| COVID perioda | Comparison periods before COVID period |
Comparison periods before COVID period |
|||||
| 0–3 months beforeb | 3–6 months beforec | 9–12 months befored | 0–3 months before | 3–6 months before | 9–12 months before | ||
| THIS WAY UP | |||||||
| Webpage views | 878,925 | 582,352 | 738,414 | 731,700 | 50.9% | 19.0% | 20.1% |
| Course registrations | 21,872 | 2806 | 2948 | 2933 | 679.5% | 641.9% | 645.7% |
| Clinician registrations | 4247 | 613 | 852 | 884 | 592.8% | 398.5% | 380.4% |
| Course prescriptions | 7478 | 1246 | 1088 | 1047 | 500.2% | 587.3% | 614.2% |
| Just A Thought | |||||||
| Webpage views | 167,972 | 22,937 | 74,307 | – | 632.3% | 126.1% | – |
| Course registrations | 5442 | 1907 | 5054 | – | 185.4% | 7.68% | – |
| Clinician registrations | 441 | 181 | 688 | – | 143.6% | −35.9% | – |
| Course prescriptions | 794 | 480 | 685 | – | 65.4% | 15.9% | – |
Notes. % increase in service use during the COVID period = (COVID period count / pre-COVID comparison count) − 1.
During-COVID period = 12th March 2020 to 11th June 2020.
0–3 months before the COVID period = 12th December 2019 to 11th March 2020.
3–6 months before the COVID period = 12th September 2019 to 11th December 2019.
9–12 months before the COVID period = 12th March to 11th June 2019 (i.e., the same 3-month period as the during-COVID period the year prior).
As Table 1 also shows, service use in Just a Thought increased during the COVID period in New Zealand. However, service use varied across the two pre-COVID time periods, and it is likely that this reflects seasonal variations in service use as well as different phases in the promotion of the service. Six months prior to the pandemic in New Zealand, the Just a Thought service was launched. Like the during-COVID period, the launch of the service was characterised by robust direct-to-public marketing and promotional activities that saw the rapid mass uptake of the service by consumers and clinicians. Compared to the launch period, service utilisation increased during the COVID period (increased website activity = 126% from 74,307 page views to 167,972 page views, course registrations = 8% from 5054 to 5442 registrations, and prescriptions = 16% from 685 to 794 prescriptions). Although fewer new clinicians registered with Just a Thought during the COVID-19 period compared to the launch, clinicians issued more course prescriptions during the COVID period, which may be indicative of greater utilisation in routine practice for some clinicians. Increases in Just a Thought service utilisation during-COVID were pronounced compared to the 3 months prior. Increases in website views (630%, from 22,937 to 167,972 page views), course registrations (185%, from 1907 to 5442 registrations), clinician registrations (144% from 181 to 441), and course prescriptions (65% from 480 to 794) may have been accentuated because this pre-COVID period coincided with the summer holidays in New Zealand which is typically a low-service activity period.
In terms of users' engagement with the COVID-specific content, from 5th April to 11th June 2020, the THIS WAY UP COVID-specific website had 23,503 visits, with the audio-guide downloaded 1459 times and the COVID support documents downloaded 1936 times. From 3rd April to 11th June 2020, the Just a Thought COVID-specific web page had 112,236 unique views. Staying on Track attracted 2613 registrations and 1337 resource downloads (additional COVID resources were downloaded 2617 times).
3.2. Characteristics of DMHS course registrants before and during the COVID-19 pandemic period
Table 2, Table 3 provide the demographic and clinical characteristics of course registrants accessing the DMHS before and during the pandemic, and demonstrate that the characteristics of registrants remained relatively stable across the pre- and during-COVID time periods. On average, registrants were in their mid to late 30s. Most registrants were female, resided in major cities in Australia and New Zealand, and enrolled in self-guided courses. Groups from both DMHS were characterised by high rates of probable mental disorder with approximately 50–60% of registrants reporting symptom severity consistent with probable MDD and/or GAD. Over two thirds of the THIS WAY UP registrants reported clinically significant psychological distress, and on average, these registrants reported experiencing low levels of wellbeing. Over 80% of the Just a Thought registrants reported clinically significant psychological distress.
Table 2.
Demographic and clinical characteristics of unique THIS WAY UP course registrants for the during-COVID period versus the three pre-COVID periods.
| Characteristics of course registrants in each group |
Differences in characteristics across groups |
|||||||
|---|---|---|---|---|---|---|---|---|
| COVID perioda | Comparison groups before COVID period |
Overall test of group differences | Pairwise test of COVID group vs. pre-COVID group |
|||||
| 0–3 months beforeb | 3–6 months beforec | 9–12 months befored | 0–3 months before | 3–6 months before | 9–12 months before | |||
| Demographics | ||||||||
| N | 21,872 | 2806 | 2948 | 2933 | ||||
| Age M (SD), range | 37.06 (13.28), 12–93 | 36.50 (13.53), 13–81 | 37.79 (13.67), 12–85 | 38.89 (13.81), 12–90 | F = 20.51*** | t = −2.09 | t = 2.75** | t = 6.93*** |
| Gender (% F) | 68.9% | 64.3% | 64.7% | 65.4% | χ2 = 48.90*** | χ2 = 24.52*** | χ2 = 21.42*** | χ2 = 14.81*** |
| Self-guided % | 86.8% | 83.1% | 86.5% | 86.0% | χ2 = 29.33*** | χ2 = 28.91*** | χ2 = 0.21 | χ2 = 1.63 |
| Regional/rural users % | 28.7% | 30.3% | 30.2% | 32.6% | χ2 = 15.33** | χ2 = 2.17 | χ2 = 1.93 | χ2 = 13.58*** |
| Professional recommend % | 44.5% | 53.5% | 48.9% | 47.6% | χ2 = 78.94*** | χ2 = 66.91*** | χ2 = 16.68*** | χ2 = 8.52** |
| Clinical characteristics | ||||||||
| K10 M (SD), n |
27.76 (7.90), 14,285 | 26.64 (7.80), 1755 | 27.26 (7.71), 1866 | 26.23 (7.66), 1820 | F = 28.54*** | t = −5.62*** | t = −2.60** | t = −7.83*** |
| % K10 > 20 | 72.0% | 66.5% | 72.2% | 67.7% | χ2 = 22.57*** | χ2 = 14.80*** | χ2 = 0.01 | χ2 = 9.81** |
| % K10 > 30 | 38.6% | 34.4% | 36.3% | 30.7% | χ2 = 49.26*** | χ2 = 11.05** | χ2 = 3.45 | χ2 = 41.32*** |
| PHQ-9 M (SD), n |
12.32 (6.45), 11,391 | 11.94 (6.21), 859 | 12.01 (6.35), 925 | 11.55 (6.23), 818 | F = 4.69** | t = −1.66 | t = −1.39 | t = −3.30** |
| % PHQ-9 > 10 | 56.9% | 52.7% | 56.1% | 52.1% | χ2 = 11.92** | χ2 = 5.58 | χ2 = 0.21 | χ2 = 7.16** |
| GAD-7 M (SD), n |
11.28 (5.31), 8516 | 11.71 (5.01), 537 | 11.81 (5.03), 572 | 11.57 (5.08),485 | F = 3.07 | t = 1.81 | t = 2.34 | t = 1.19 |
| % GAD-7 > 10 | 53.6% | 56.4% | 59.6% | 59.6% | χ2 = 14.71** | χ2 = 1.64 | χ2 = 7.86** | χ2 = 6.66* |
| SWEMWBS M (SD), n |
18.92 (3.39), 3166 | 19.44 (3.64), 265 | 19.09 (3.13), 229 | 19.58 (3.52), 283 | F = 4.79** | t = 2.39 | t = 0.75 | t = 3.10** |
Notes. F = female; M = mean; SD = standard deviation; PHQ-9 = Patient Health Questionnaire-9; GAD-7 = Generalized Anxiety Disorder 7-item Scale; K-10 = Kessler Psychological Distress Scale; SWEMWBS = Short Warwick-Edinburgh Mental Well-being Scale. ***p < .001 **p < .01, *p < .0167 (0.05/3).
During-COVID period = 12th March 2020 to 11th June 2020.
0–3 months before the COVID period = 12th December 2019 to 11th March 2020.
3–6 months before the COVID period = 12th September 2019 to 11th December 2019.
9–12 months before the COVID period = 12th March to 11th June 2019 (i.e., the same 3-month period as the during-COVID period the year prior).
Table 3.
Demographic and clinical characteristics of unique Just a Thought course registrants for the during-COVID period versus the two pre-COVID periods.
| Characteristics of course registrants in each group |
Differences in characteristics across groups |
||||
|---|---|---|---|---|---|
| COVID perioda | Comparison groups before COVID period |
Pairwise test of COVID group vs. pre-COVID group |
|||
| 0–3 months beforeb | 3–6 months beforec | 0–3 months before | 3–6 months before | ||
| Demographics | |||||
| n | 5442 | 1907 | 5054 | ||
| Age M (SD), range | 39.81 (14.66), 12–95 | 37.00 (14.39), 12–88 | 7.78 (13.71), 13–89 | t = −4.13⁎⁎⁎ | t = −2.82⁎⁎ |
| Gender (% F) | 80.2% | 75.2% | 78.5% | χ2 = 21.66⁎⁎⁎ | χ2 = 5.15 |
| Self-guided % | 94.4% | 88.8% | 93.8% | χ2 = 68.46⁎⁎⁎ | χ2 = 1.64 |
| Rural users % | 13.5% | 13.9% | 11.5% | χ2 = 0.20 | χ2 = 9.04⁎⁎ |
| Professional recommend % | 22.6% | 41.7% | 19.1% | χ2 = 258.28⁎⁎⁎ | χ2 = 19.53⁎⁎⁎ |
| Clinical characteristics | |||||
| K10 M (SD), n | 29.60 (8.13), 2332 | 29.79 (7.78), 1489 | 28.61 (7.86), 3671 | t = 0.71 | t = −4.77⁎⁎⁎ |
| % K10 > 20 | 86.2% | 86.4% | 82.6% | χ2 = 0.03 | χ2 = 13.68⁎⁎ |
| % K10 > 30 | 46.2% | 47.5% | 42.5% | χ2 = 0.62 | χ2 = 7.99⁎⁎⁎ |
| PHQ-9 M (SD), n | 13.30 (6.58), 2194 | 13.47 (6.50), 1455 | 12.44 (6.48), 3571 | t = 0.84 | t = −4.81⁎⁎ |
| % PHQ-9 > 10 | 63.2% | 64.1% | 58.4% | χ2 = 0.34 | χ2 = 12.69⁎⁎⁎ |
| GAD-7 M (SD), n | 11.60 (5.36), 2219 | 11.61 (5.24), 1463 | 10.66 (5.25), 3598 | t = 0.07 | t = −6.58⁎⁎⁎ |
| % GAD-7 > 10 | 56.1% | 57.1% | 49.2% | χ2 = 0.39 | χ2 = 26.08⁎⁎⁎ |
Notes. F = female; M = mean; SD = standard deviation; K-10 = Kessler Psychological Distress Scale; PHQ-9 = Patient Health Questionnaire-9; GAD-7 = Generalized Anxiety Disorder 7-item Scale.
During-COVID period = 12th March 2020 to 11th June 2020.
0–3 months before the COVID period = 12th December 2019 to 11th March 2020.
3–6 months before the COVID period = 12th September 2019 to 11th December 2019.
p < .001.
p < .01.
3.2.1. Demographic characteristics
In THIS WAY UP, the during-COVID registrants were more likely to be female, register for a self-help (vs. clinician-guided) course, reside in a major Australian city (vs. a regional, rural and/or remote locality), and be less likely to have heard about the service from their health care clinician than the pre-COVID users (see Table 2).
In Just a Thought (Table 3), during-COVID registrants were more likely to be older, female, and to enrol in a self-guided course, and were less likely to have heard about Just a Thought from a health care professional compared to those who engaged with the service 3 months prior to the pandemic confirmation. Compared to individuals who engaged with Just a Thought 6 months before the pandemic confirmation, the during-COVID registrants were more likely to be older, reside in rural communities, and to have heard about Just a Thought from a health care professional. However, gender distribution was similar across these two groups, as was the proportions of registrants who enrolled in a self-guided (vs. clinician-guided) course.
3.2.2. Clinical characteristics
Compared to THIS WAY UP pre-COVID registrants, individuals engaging with the service during the COVID period reported slightly higher mean levels of psychological distress and depression symptom severity on average, as well as higher rates of probable MDD and higher proportions of clinically significant psychological distress (see Table 2). Mean levels of anxiety symptom severity and wellbeing did not significantly vary across the THIS WAY UP pre- and during-COVID groups. Rates of probable GAD were marginally lower in the during-COVID group compared to the pre-COVID group.
For Just a Thought registrants, we did not observe any significant differences in the clinical characteristics of the during-COVID registrants and those who engaged with the service 3 months prior to the pandemic confirmation (see Table 3). Compared to those who engaged with Just a Thought 6 months before the pandemic, during-COVID registrants reported marginally higher mean levels of psychological distress, and depression and anxiety symptom severity, as well as higher proportions of probable GAD and MDD.
4. Discussion
Our understanding of the magnitude of the mental health challenge secondary to COVID-19 is growing. Healthcare systems around the world are exploring ways of enhancing capacity to meet this rising need, including utilisation and integration of DMHS into existing health care systems (e.g., Poulton et al., 2020). In this study, DMHS utilisation increased considerably during the COVID-19 pandemic in Australia and New Zealand across all service use indices. We observed some differences in service use across the DMHS. Pre- to during-COVID increases in website visits were more pronounced in the Just a Thought service, whereas increases in course registrations and new clinician registrations were higher for THIS WAY UP. Reasons for these differences may reflect the different ages, funding structures, and promotional activities of the two DMHS. Nevertheless, our results highlight the responsivity of DMHS to scale-up service provision to meet increased demands.
It is likely that the cause of the increased service utilisation seen in both DMHS during the COVID period relates to a combination of factors. The heightened level of COVID-related concern and distress in the community may have motivated people to seek support online given the significant disruptions to face-to-face mental health service provision during the COVID-19 pandemic (Jayawardana and Gannon, 2021). Indeed there have been widespread reports across the globe of reductions in the number of face-to-face or in-person mental health consultations, including outpatient appointments, hospital admissions, and emergency department attendances (e.g., Bowman et al., 2021; Dragovic et al., 2020; Garriga et al., 2020; Tromans et al., 2020). The heightened media exposure of the DMHS in this study, coupled with the waiving of course fees in the THIS WAY UP service, may have also contributed to increased service use during the COVID period. Our findings are consistent with those of the MindSpot digital mental health service which reported an 89% increase in website visits, 90% increase in telephone calls, and 16.7% increase in clinical assessments during the early months of COVID pandemic in Australia (Titov et al., 2020; Staples et al., 2020). Our results are also consistent with the substantial increase in the consumption of other remotely-delivered mental health supports during the COVID period in Australia and New Zealand, such as telephone calls to mental health helplines, telehealth mental health consultations, and mental health website visits (e.g., Jayawardana and Gannon, 2021; Looi et al., 2020; Medhora, 2020). Taken together with other studies, our results demonstrate that large numbers of individuals sought online psychological support and interventions in the early months of the pandemic in Australia and New Zealand. This is highly consistent with the concerns about poorer mental health across the globe during the pandemic (e.g., Andersson et al., 2020; Holmes et al., 2020).
Across the DMHS in this study we observed the most robust uptake for self-guided courses. Most THIS WAY UP and Just a Thought registrants sought self-help resources or courses across all time periods, but especially during the COVID-19 period. This highlights the demand for these resources as well as the potential utility of direct-to-public promotional activities for DMHS, particularly when access to clinician-based services may be limited. A clear advantage of online self-help CBT is that it can be readily accessed by large groups of people. While evidence suggests that unguided iCBT is less effective than guided iCBT for people with depression, its effectiveness for individuals with mild and subthreshold depression symptom severity may be comparable to guided iCBT (Karyotaki et al., 2021). Also, a recent meta-analysis of digital interventions for anxiety disorders found no significant differences between the treatment effects of guided verses unguided interventions (Pauley et al., 2021). While there is some indication that treatment adherence associated with guided iCBT is similar to that of face-to-face CBT (van Ballegooijen et al., 2014), some studies have shown that adherence to self-guided iCBT courses is lower than adherence to guided iCBT courses (Berger et al., 2011a; Berger et al., 2011b; Titov et al., 2008). Nevertheless, there are many benefits of self-guided digital mental health interventions, including anonymity, convenience, affordability, scalability, and portability (Marshall et al., 2019, Marshall et al., 2020). Although THIS WAY UP courses have a firm evidence-base, there are a vast variety of self-help digital mental health interventions that are publicly available and the efficacy of many of these tools is unknown (Marshall et al., 2019, Marshall et al., 2020). It is important for governments and health care systems across the globe to promote evidence-based interventions, especially during periods of crisis and high demand like the COVID-19 pandemic.
As predicted, we did not observe marked differences between the demographic and clinical characteristics of pre- and during-COVID registrants in either DMHS. The demographic profile of DMHS registrants in this study is largely consistent with the typical demographic characteristics of users of other routine care DMHS (e.g., Titov et al., 2018). Consistent with Staples et al. (2020), we found limited evidence of elevated psychological distress or elevated anxiety and depression symptom severity in the during-COVID registrants versus pre-COVID registrants from either DMHS in this study. Elevations were not consistently found, and the magnitude of differences was modest. Thus, while the mean severity of symptoms reported by DMHS registrants was comparable before and during the pandemic, the volume of DMHS registrants reporting clinically significant symptoms increased dramatically in the COVID period. These findings concur with multiple studies that have reported the increased prevalence of clinically significant mental health symptoms in the populations of Australia and New Zealand during COVID (e.g., Gasteiger et al., 2021; Rossell et al., 2021), and confirm the considerable global mental health impact of the pandemic.
5. Limitations
Current indices of service utilisation provide an estimate of engagement, but website visits and course registrations cannot represent the complexity of users' experiences with DMHS. We did not assess the duration and frequency of course registrants' practise of the therapy skills taught in the online courses and as such the extent of course usage is unclear. Preliminary reports suggest that a number of THIS WAY UP courses continue to be effective under pandemic conditions in terms of reducing primary symptom severity, although overall rates of course completion appear somewhat lower given the higher enrolment into self-guided courses during the pandemic (see Li et al., 2021; Li et al., 2020; Mahoney et al., 2021a; Mahoney et al., 2021b; Sharrock et al., 2021). However, further studies need to explore the quality and effectiveness of user engagement with DMHS during the pandemic in reducing ill health and enhancing quality of life.
Like many studies of routine care provision, assessments in this study were based on voluntarily completed self-report measures and missing responses were inevitable. Detailed information regarding registrants' personal circumstances was not collected (e.g., unemployment, physical health status [including COVID-19 status], in lockdown/quarantine, health workers, carers of young children or elderly etc.) which precludes conclusions about specific populations. Additionally, information regarding course registrants' ethnicity and socio-economic status were not collected in THIS WAY UP, and as such the relationship between these factors and consumers' uptake of and access to digital tools could not be estimated. Future research is needed to examine equity of access to DMHS across a diverse range of populations.
This study reports on the early COVID-19 period in Australia and New Zealand and may not generalise to later time periods and other regions around the world. It is also very important to emphasise that the degree of COVID-19 transmission (and associated adversities) experienced in Australia and New Zealand differs substantially from other countries (e.g., see Jefferies et al., 2020). As of mid-June 2021, the total number of COVID cases (per million people) has been estimated at 101,163 in the USA and 67,716 in the UK, while the number of COVID cases (per million people) in Australia and New Zealand was 1188 and 562, respectively (Dong et al., 2020; Ritchie et al., 2021). Similarly, as of early June 2021, the number of COVID-related deaths (per million people) in the USA (~1814) and the UK (~1888) are substantially higher than those in Australia (~36) and New Zealand (~5) (Dong et al., 2020; Ritchie et al., 2021). Clearly, future studies are needed to understand the comparative short and longer-term impacts of the pandemic internationally.
Notwithstanding these limitations, our findings demonstrate that DMHS provide scalable access to evidenced-based mental health resources for a large number of individuals experiencing psychological distress. There is clear evidence to support the large demand and utility of DMHS in extending service provision within stepped and preventative models of care, and we anticipate that the use and integration of DMHS within the broader health system will persist beyond the pandemic. Collaborative marketing and promotion are also important for increasing awareness and facilitating the uptake of DMHS interventions. Finally, clinicians provide integral signposting and gatekeeping functions into DMHS for consumers, therefore their beliefs and behaviours towards digital tools can either promote access or act as a significant barrier. We encourage clinicians to continue exploring the multitude of ways that DMHS can augment in-person traditional services (see Newby et al., 2021 for a discussion), and we applaud the commitment of the Australian and New Zealand governments to support DMHS which has enabled widespread public access and workforce adoption of these services.
6. Conclusion
Service utilisation in two DMHS significantly increased following the outbreak of COVID-19 in Australia and New Zealand. In addition to the doubt and distress generated by the pandemic, increased service uptake was likely facilitated by robust service promotion, restricted access to traditional clinician-based services, and increased governmental and philanthropic funding and support. This study highlights how nimble, responsive, and scalable DMHS can be during challenging times.
Sources of funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
To view a demonstration of the courses, please contact the first author.
Following this period, additional funding meant that clinician-prescribed courses could continue to be freely accessed (but fees for self-directed courses resumed).
Contributor Information
Alison E.J. Mahoney, Email: alison.mahoney@svha.org.au.
Anna Elders, Email: anna.elders@justathought.co.nz.
Ian Li, Email: ian.li@svha.org.au.
Charlie David, Email: charlie.david@justathought.co.nz.
Hila Haskelberg, Email: hila.haskelberg@svha.org.au.
Hayley Guiney, Email: hayley.guiney@otago.ac.nz.
Michael Millard, Email: michael.millard@svha.org.au.
References
- Andersson G., Berg M., Riper H., Huppert J.D., Titov N. The possible role of internet-delivered psychological interventions in relation to the COVID-19 pandemic. Clin. Psychol. Eur. 2020;2(3):1–4. doi: 10.32872/cpe.v2i3.3941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andrews G., Basu A., Cuijpers P., Craske M.G., McEvoy P., English C.L., Newby J.M. Computer therapy for the anxiety and depression disorders is effective, acceptable and practical health care: an updated meta-analysis. J. Anxiety Disord. 2018;55:70–78. doi: 10.1016/j.janxdis.2018.01.001. [DOI] [PubMed] [Google Scholar]
- Andrews G., Slade T. Interpreting scores on the kessler psychological distress scale (K10) Aust. N. Z. J. Public Health. 2001;25(6):494–497. doi: 10.1111/j.1467-842X.2001.tb00310.x. [DOI] [PubMed] [Google Scholar]
- Australian Bureau of Statistics . Remoteness Structure. Volume 5. 2013. Australian Statistical Geography Standard (ASGS)https://www.abs.gov.au/ausstats/abs@.nsf/mf/1270.0.55.005 Retrieved from. [Google Scholar]
- Australian Bureau of Statistics Information paper: use of the Kessler psychological distress scale in ABS health surveys, Australia, 2007-08. 2003. https://www.abs.gov.au/ausstats/abs@.nsf/mf/4817.0.55.001 Retrieved from.
- Bartram D.J., Sinclair J.M., Baldwin D.S. Further validation of the Warwick-Edinburgh mental well-being scale (WEMWBS) in the UK veterinary profession: rasch analysis. Qual. Life Res. 2013;22(2):379–391. doi: 10.1007/s11136-012-0144-4. [DOI] [PubMed] [Google Scholar]
- Berger T., Caspar F., Richardson R., Kneubühler B., Sutter D., Andersson G. Internet-based treatment of social phobia: a randomized controlled trial comparing unguided with two types of guided self-help. Behav. Res. Ther. 2011;49(3):158–169. doi: 10.1016/j.brat.2010.12.007. [DOI] [PubMed] [Google Scholar]
- Berger T., Hämmerli K., Gubser N., Andersson G., Caspar F. Internet-based treatment of depression: a randomized controlled trial comparing guided with unguided self-help. Cogn. Behav. Ther. 2011;40(4):251–266. doi: 10.1080/16506073.2011.616531. [DOI] [PubMed] [Google Scholar]
- Bowman C., Branjerdporn G., Turner K., Kamara M., Tyagi N., Reyes N.J.D., Stapelberg N.J.C. The impact of viral epidemics and pandemics on acute mental health service use: an integrative review. Health Psychol. Rev. 2021;15(1):1–33. doi: 10.1080/17437199.2021.1886864. [DOI] [PubMed] [Google Scholar]
- Carlbring P., Andersson G., Cuijpers P., Riper H., Hedman-Lagerlöf E. Internet-based vs. face-to-face cognitive behavior therapy for psychiatric and somatic disorders: an updated systematic review and meta-analysis. Cogn. Behav. Ther. 2018;47(1):1–18. doi: 10.1080/16506073.2017.1401115. [DOI] [PubMed] [Google Scholar]
- Dong E., Du H., Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect. Dis. 2020;20(5):533–534. doi: 10.1016/S1473-3099(20)30120-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dragovic M., Pascu V., Hall T., Ingram J., Waters F. Emergency department mental health presentations before and during the COVID-19 outbreak in Western Australia. Australas. Psychiatry. 2020;28(6):627–631. doi: 10.1177/1039856220960673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisk M., Livingstone A., Pit S.W. Telehealth in the context of COVID-19: changing perspectives in Australia, the United Kingdom, and the United States. J. Med. Internet Res. 2020;22(6) doi: 10.2196/19264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Furukawa T.A., Kessler R.C., Slade T., Andrews G. The performance of the K6 and K10 screening scales for psychological distress in the australian National Survey of mental health and well-being. Psychol. Med. 2003;33(2):357–362. doi: 10.1017/s0033291702006700. [DOI] [PubMed] [Google Scholar]
- Garriga M., Agasi I., Fedida E., Pinzón-Espinosa J., Vazquez M., Pacchiarotti I., Vieta E. The role of mental health home hospitalization care during the COVID-19 pandemic. Acta Psychiatr. Scand. 2020;141(5):479–480. doi: 10.1111/acps.13173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gasteiger N., Vedhara K., Massey A., Jia R., Ayling K., Chalder T., Broadbent E. Depression, anxiety and stress during the COVID-19 pandemic: results from a New Zealand cohort study on mental well-being. BMJ Open. 2021;11(5) doi: 10.1136/bmjopen-2020-045325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gearing R.E., Schwalbe C.S., MacKenzie M.J., Brewer K.B., Ibrahim R.W., Olimat H.S., Al-Krenawi A. Adaptation and translation of mental health interventions in middle eastern Arab countries: a systematic review of barriers to and strategies for effective treatment implementation. Int. J. Soc. Psychiatry. 2013;59(7):671–681. doi: 10.1177/0020764012452349. [DOI] [PubMed] [Google Scholar]
- Gratzer D., Torous J., Lam R.W., Patten S.B., Kutcher S., Chan S., Yatham L.N. Our digital moment: innovations and opportunities in digital mental health care. Can. J. Psychiatr. 2020 doi: 10.1177/0706743720937833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes E.A., O'Connor R.C., Perry V.H., Tracey I., Wessely S., Arseneault L., Bullmore E. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. 2020;7(6):547–560. doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- International Monetary Fund . International Monetary Fund; Washington, DC: 2020. World Economic Outlook: A Long and Difficult Ascent. [Google Scholar]
- Jayawardana D., Gannon B. Use of telehealth mental health services during the COVID-19 pandemic. Aust. Health Rev. 2021 doi: 10.1071/AH20325. [DOI] [PubMed] [Google Scholar]
- Jefferies S., French N., Gilkison C., Graham G., Hope V., Marshall J., Priest P. COVID-19 in New Zealand and the impact of the national response: a descriptive epidemiological study. Lancet Public Health. 2020;5:e612–e623. doi: 10.1016/S2468-2667(20)30225-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karyotaki E., Efthimiou O., Miguel C., Bermpohl F.M.G., Furukawa T.A., Cuijpers P., Forsell Y. Internet-based cognitive behavioral therapy for depression: a systematic review and individual patient data network meta-analysis. JAMA Psychiatry. 2021;78(4):361–371. doi: 10.1001/jamapsychiatry.2020.4364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler R.C., Andrews G., Colpe L.J., Hiripi E., Mroczek D.K., Normand S.L., Walters E.E., Zaslavsky A.M. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol. Med. 2002;32(6):959–976. doi: 10.1017/s0033291702006074. [DOI] [PubMed] [Google Scholar]
- Kladnitski N., Smith J., Uppal S., James M.A., Allen A.R., Andrews G., Newby J.M. Transdiagnostic internet-delivered CBT and mindfulness-based treatment for depression and anxiety: a randomised controlled trial. Internet Interv. 2020;20 doi: 10.1016/j.invent.2020.100310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B. The PHQ-9: validity of a brief depression severity measure. J. Gen. Intern. Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li I., Chen A.Z., Newby J.M., Kladnitski N., Haskelberg H., Millard M., Mahoney A. 2021. The Uptake and Effectiveness of an Online Self-help Mindfulness Program During COVID-19. (Manuscript submitted for publication) [Google Scholar]
- Li I., Millard M., Haskelberg H., Hobbs M.J., Luu J., Mahoney A.E.J. 2020. COVID-19 Related Differences in the Uptake and Effects of Internet-based Cognitive Behavioural Therapy for Symptoms of Obsessive-compulsive Disorder. (Manuscript submitted for publication) [DOI] [PubMed] [Google Scholar]
- Looi J.C.L., Allison S., Bastiampillai T., Pring W. Private practice metropolitan telepsychiatry in larger Australian states during the COVID-19 pandemic: an analysis of the first 2 months of new MBS telehealth item psychiatrist services. Australas. Psychiatry. 2020;28(6):644–648. doi: 10.1177/1039856220961906. [DOI] [PubMed] [Google Scholar]
- Loughnan S.A., Butler C., Sie A.A., Grierson A.B., Chen A.Z., Hobbs M.J., Newby J.M. A randomised controlled trial of ‘MUMentum postnatal’: internet-delivered cognitive behavioural therapy for anxiety and depression in postpartum women. Behav. Res. Ther. 2019;116:94–103. doi: 10.1016/j.brat.2019.03.001. [DOI] [PubMed] [Google Scholar]
- Löwe B., Decker O., Müller S., Brähler E., Schellberg D., Herzog W., Herzberg P.Y. Validation and standardization of the Generalized Anxiety Disorder Screener (GAD-7) in the general population. Med. Care. 2008;46(3):266–274. doi: 10.1097/MLR.0b013e318160d093. [DOI] [PubMed] [Google Scholar]
- Luo M., Guo L., Yu M., Jiang W., Wang H. The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public – a systematic review and meta-analysis. Psychiatry Res. 2020;291 doi: 10.1016/j.psychres.2020.113190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahoney A., Li I., Grierson A.B., Haskelberg H., Millard M., Mason E. 2021. Internet-based Cognitive Behaviour Therapy for Insomnia Before and During the COVID-19. (Manuscript submitted for publication) [Google Scholar]
- Mahoney A., Li I., Haskelberg H., Millard M., Newby J.M. The uptake and effectiveness of online cognitive behaviour therapy for symptoms of anxiety and depression during COVID-19. J. Affect. Disord. 2021;292:197–203. doi: 10.1016/j.jad.2021.05.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshall J.M., Dunstan D.A., Bartik W. The digital psychiatrist: in search of evidence-based apps for anxiety and depression. Front. Psychiatry. 2019;10(831) doi: 10.3389/fpsyt.2019.00831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshall J.M., Dunstan D.A., Bartik W. The role of digital mental health resources to treat trauma symptoms in Australia during COVID-19. Psychol. Trauma Theory Res. Pract. Policy. 2020;12(S1):S269–S271. doi: 10.1037/tra0000627. [DOI] [PubMed] [Google Scholar]
- Medhora S. Calls to Lifeline jump 20 per cent as coronavirus crisis takes hold. March 27, 2020. https://www.abc.net.au/triplej/programs/hack/calls-to-lifeline-go-up-due-to-coronavirus-covid-19/12096922 Retrieved from.
- Merson F., Newby J., Shires A., Millard M., Mahoney A. The temporal stability of the kessler psychological distress scale. Aust. Psychol. 2021;56(1):38–45. doi: 10.1080/00050067.2021.1893603. [DOI] [Google Scholar]
- Newby J.M., Mackenzie A., Williams A.D., McIntyre K., Watts S., Wong N., Andrews G. Internet cognitive behavioural therapy for mixed anxiety and depression: a randomized controlled trial and evidence of effectiveness in primary care. Psychol. Med. 2013;43(12):2635–2648. doi: 10.1017/S0033291713000111. [DOI] [PubMed] [Google Scholar]
- Newby J.M., Mason E., Kladnistki N., Murphy M., Millard M., Haskelberg H., Mahoney A.E.J. Integrating internet cognitive behavioural therapy into routine clinical practice: a guide for clinicians. Clin. Psychol. 2021 doi: 10.1080/13284207.2020.1843968. [DOI] [Google Scholar]
- New Zealand Geographic Data Service Urban Rural indicator 2020 V1.0.0. 2020. https://datafinder.stats.govt.nz/layer/104269-urban-rural-2020-generalised Retrieved from.
- Ng Fat L., Scholes S., Boniface S., Mindell J., Stewart-Brown S. Evaluating and establishing national norms for mental wellbeing using the short Warwick-Edinburgh mental well-being scale (SWEMWBS): findings from the health survey for England. Qual. Life Res. 2017;26(5):1129–1144. doi: 10.1007/s11136-016-1454-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pauley D., Cuijpers P., Papola D., Miguel C., Karyotaki E. Two decades of digital interventions for anxiety disorders: a systematic review and meta-analysis of treatment effectiveness. Psycho. Med. 2021;1(13) doi: 10.1017/S0033291721001999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pierce M., Hope H., Ford T., Hatch S., Hotopf M., John A., Abel K.M. Mental health before and during the COVID-19 pandemic: a longitudinal probability sample survey of the UK population. Lancet Psychiatry. 2020;7(10):883–892. doi: 10.1016/S2215-0366(20)30308-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poulton R., Gluckman P., Menzies R., Bardsley A., McIntosh T., Faleafa M. The Centre for Informed Futures; Koi Tu: 2020. Protecting and Promoting Mental Wellbeing During COVID-19 and Beyond.https://informedfutures.org/protecting-and-promoting-mental-wellbeing-beyond-covid-19/ Accessed 11th December 2020. [Google Scholar]
- Ritchie H., Ortiz-Ospina E., Beltekian D., Mathieu E., Hasell J., Macdonald B., Roser M. Coronavirus Pandemic (COVID-19) – the data. 2021. https://ourworldindata.org/coronavirus-data Retrieved from. [DOI] [PMC free article] [PubMed]
- Rossell S.L., Neill E., Phillipou A., Tan E.J., Toh W.L., Van Rheenen T.E., Meyer D. An overview of current mental health in the general population of Australia during the COVID-19 pandemic: results from the COLLATE project. Psychiatry Res. 2021;296 doi: 10.1016/j.psychres.2020.113660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sachs J.D., Horton R., Bagenal J., Amor Y.B., Caman O.K., Lafortune G. The lancet COVID-19 commission. Lancet. 2020;396(10249):454–455. doi: 10.1016/S0140-6736(20)31494-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shah N., Cader M., Andrews W.P., Wijesekera D., Stewart-Brown S.L. Responsiveness of the short Warwick Edinburgh mental well-being scale (SWEMWBS): evaluation a clinical sample. Health Qual. Life Outcomes. 2018;16(1):239. doi: 10.1186/s12955-018-1060-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharrock M., Mahoney A., Haskelberg H., Millard M., Newby J. 2021. Online Cognitive Behaviour Therapy for Symptoms of Health Anxiety During the COVID-19 Pandemic. (Manuscript submitted for publication) [Google Scholar]
- Smith J., Faux S.G., Gardner T., Hobbs M.J., James M.A., Joubert A.E., Andrews G. Reboot online: a randomized controlled trial comparing an online multidisciplinary pain management program with usual care for chronic pain. Pain Med. 2019;20(12):2385–2396. doi: 10.1093/pm/pnz208. [DOI] [PubMed] [Google Scholar]
- Spanhel K., Balci S., Baumeister H., Bengel J., Sander L.B. Cultural adaptation of internet- and mobile-based interventions for mental disorders: a systematic review protocol. Systematic Reviews. 2020;9:207. doi: 10.1186/s13643-020-01438-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer R.L., Kroenke K., Williams J.B., Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch. Intern. Med. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Staples L., Nielssen O., Kayrouz R., Cross S., Karin E., Ryan K., Titov N. Rapid report 2: symptoms of anxiety and depression during the first 12 weeks of the coronavirus (COVID-19) pandemic in Australia. Internet Interv. 2020;22 doi: 10.1016/j.invent.2020.100351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sunderland M., Wong N., Hilvert-Bruce Z., Andrews G. Investigating trajectories of change in psychological distress amongst patients with depression and generalised anxiety disorder treated with internet cognitive behavioural therapy. Behav. Res. Ther. 2012;50(6):374–380. doi: 10.1016/j.brat.2012.03.005. [DOI] [PubMed] [Google Scholar]
- Tennant R., Hiller L., Fishwick R., Platt S., Joseph S., Weich S., Stewart-Brown S. The Warwick-Edinburgh mental well-being scale (WEMWBS): development and UK validation. Health Qual. Life Outcomes. 2007;5:63. doi: 10.1186/1477-7525-5-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Titov N., Andrews G., Choi I., Schwencke G., Mahoney A. Shyness 3: randomized controlled trial of guided versus unguided internet-based CBT for social phobia. Aust. N. Z. J. Psychiatry. 2008;42(12):1030–1040. doi: 10.1080/00048670802512107. [DOI] [PubMed] [Google Scholar]
- Titov N., Dear B., Nielssen O., Staples L., Hadjistavropoulos H., Nugent M., Kaldo V. ICBT in routine care: a descriptive analysis of successful clinics in five countries. Internet Interv. 2018;13:108–115. doi: 10.1016/j.invent.2018.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Titov N., Staples L., Kayrouz R., Cross S., Karin E., Ryan K., Nielssen O. Rapid report: early demand, profiles and concerns of mental health users during the coronavirus (COVID-19) pandemic. Internet Interv. 2020;21 doi: 10.1016/j.invent.2020.100327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torous J., Jän Myrick K., Rauseo-Ricupero N., Firth J. Digital mental health and COVID-19: using technology today to accelerate the curve on access and quality tomorrow. JMIR Mental Health. 2020;7(3) doi: 10.2196/18848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tromans S., Chester V., Harrison H., Pankhania P., Booth H., Chakraborty N. Patterns of use of secondary mental health services before and during COVID-19 lockdown: observational study. BJPsych Open. 2020;6(6) doi: 10.1192/bjo.2020.104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Ballegooijen W., Cuijpers P., van Straten A., Karyotaki E., Andersson G., Smit J.H., Riper H. Adherence to internet-based and face-to-face cognitive behavioural therapy for depression: a meta-analysis. PLoS One. 2014;9(7) doi: 10.1371/journal.pone.0100674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wind T.R., Rijkeboer M., Andersson G., Riper H. The COVID-19 pandemic: the 'black swan' for mental health care and a turning point for e-health. Internet Interv. 2020;20 doi: 10.1016/j.invent.2020.100317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu T., Jia X., Shi H., Niu J., Yin X., Xie J., Wang X. Prevalence of mental health problems during the COVID-19 pandemic: a systematic review and meta-analysis. J. Affect. Disord. 2020 doi: 10.1016/j.jad.2020.11.117. [DOI] [PMC free article] [PubMed] [Google Scholar]