To the Editor:
We read with interest the 2 case reports of acute kidney injury (AKI) associated with semaglutide use, described by Leehey et al,1 given the risks associated with AKI.2,3 In light of the reported kidney benefits of glucagon-like peptide-1 receptor agonists (GLP-1RAs),4,5 we investigated whether GLP-1RAs are associated with increased risk for AKI, pooling data from cardiovascular outcome trials that enrolled high- or very-high-risk individuals with type 2 diabetes mellitus.
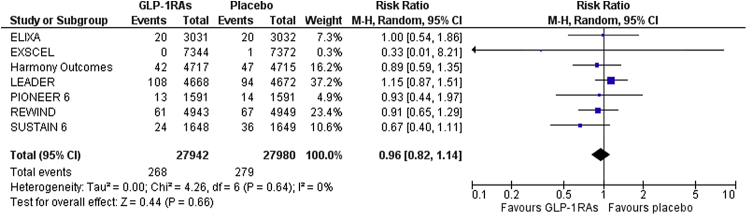
We set as primary safety outcome the incidence of AKI. Two independent reviewers (DP and AB) extracted data from eligible reports using a pilot tested data extraction form. Differences were calculated with the use of risk ratio (RR) after implementation of the Mantel-Haenszel random effects formula. Statistical heterogeneity among studies was assessed by using I2 statistics. Analyses were performed using RevMan 5.3 software. Discrepancies between reviewers were solved by discussion, consensus, or arbitration by a third senior reviewer (MD).
Pooled data from 7 cardiovascular outcome trials with GLP-1RAs provided a total of 55,943 patients. Risk of bias was low across all selected trials. GLP-1RA treatment resulted in a nonsignificant decrease in risk for AKI (RR = 0.96; 95% CI: 0.82 to 1.14; Fig 1). When restricting our analysis to the 2 dedicated semaglutide trials, we observed no difference (RR = 0.74; 95% CI: 0.49 to 1.13; I2 = 0%).
Figure 1.
Effect of glucagon-like peptide-1 receptor agonists compared to placebo on the risk for acute kidney injury.
Notably, the 2 patients described by Leehey et al1 had CKD stage 3b-4, an understudied population in the relevant literature. Accordingly, while GLP-1RAs do not increase the risk for AKI on a population level, caution is likely prudent in administering to patients with advanced CKD, particularly given potential effects on volume status owing to adverse gastrointestinal events associated with treatment.6 Close monitoring of such patients is always required, especially within the first months after initiation of a GLP-1RA.
Article Information
Financial Disclosure
The authors declare that they have no relevant financial interests.
Peer Review
Received February 10, 2021. Accepted February 17, 2021 after editorial review by the Editor-in-Chief.
References
- 1.Leehey D.J., Rahman M.A., Borys E., Picken M.M., Clise C.E. Acute kidney injury associated with semaglutide. Kidney Med. 2021;3(2):282–285. doi: 10.1016/j.xkme.2020.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Coca S.G., Singanamala S., Parikh C.R. Chronic kidney disease after acute kidney injury: a systematic review and meta-analysis. Kidney Int. 2012;81(5):442–448. doi: 10.1038/ki.2011.379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Odutayo A., Wong C.X., Farkouh M. AKI and long-term risk for cardiovascular events and mortality. J Am Soc Nephrol. 2017;28(1):377–387. doi: 10.1681/ASN.2016010105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kristensen S.L., Rørth R., Jhund P.S. Cardiovascular, mortality, and kidney outcomes with GLP-1 receptor agonists in patients with type 2 diabetes: a systematic review and meta-analysis of cardiovascular outcome trials [published correction appears in Lancet Diabetes Endocrinol. 2020 Mar;8(3):e2] Lancet Diabetes Endocrinol. 2019;7(10):776–785. doi: 10.1016/S2213-8587(19)30249-9. [DOI] [PubMed] [Google Scholar]
- 5.Sarafidis P., Ferro C.J., Morales E. SGLT-2 inhibitors and GLP-1 receptor agonists for nephroprotection and cardioprotection in patients with diabetes mellitus and chronic kidney disease. A consensus statement by the EURECA-m and the DIABESITY working groups of the ERA-EDTA [published correction appears in Nephrol Dial Transplant. 2020 Aug 1;35(8):1452. Wiecek, Andrej [corrected to Wiecek, Andrzej]] [published correction appears in Nephrol Dial Transplant. 2020 Oct 1;35(10):1825] Nephrol Dial Transplant. 2019;34(2):208–230. doi: 10.1093/ndt/gfy407. [DOI] [PubMed] [Google Scholar]
- 6.Htike Z.Z., Zaccardi F., Papamargaritis D., Webb D.R., Khunti K., Davies M.J. Efficacy and safety of glucagon-like peptide-1 receptor agonists in type 2 diabetes: a systematic review and mixed-treatment comparison analysis. Diabetes Obes Metab. 2017;19(4):524–536. doi: 10.1111/dom.12849. [DOI] [PubMed] [Google Scholar]