Our “do-it-yourself” model simulates the angles of cardiac surgery.
Central Message.
The majority of cardiothoracic surgery trainees believe that practice improves surgical skill. A “do-it-yourself” simulator can be easily constructed to practice various aspects of cardiac surgery.
Perspective.
Survey of cardiothoracic surgery trainees reveals that the majority believe practice is important for improving surgical skill. However, impediments include time, instruction, and equipment. With these principles in mind, we describe a “do-it-yourself” (DIY) simulator that optimizes ease-of-use for trainees' busy schedules and serves as a platform for virtual instruction amidst the COVID-19 pandemic.
See Commentaries on pages 112 and 114.
Our group has previously described how practice is essential to the development of expertise in a variety of domains.1 In this article, we present the results of a survey of current cardiothoracic surgical trainees on their attitudes regarding the utility of practice. Based on these findings, we describe our prototype “do-it-yourself” (DIY) simulator, emphasizing future directions for inculcating a habit of practice among trainees, especially given the increasing reliance on virtual platforms amidst the coronavirus disease 2019 (COVID-19) pandemic (Video 1).
Methods
In collaboration with the Thoracic Surgery Residents Association, a 19-question survey was distributed to current cardiothoracic trainees in all training pathways (n = 531) from October 1 to December 31, 2019. The full survey is available in the Online Data Supplement. The survey aimed to evaluate institutional culture, trainee habits (eg, frequency, duration, setting), attitudes, and perceived impediments to practice (eg, instruction, space, equipment, motivation, and time). Practice was defined broadly as any or all of the following activities: knot-tying, suturing, and tissue handling, either in a simulation or an animal tissue laboratory setting. Standard descriptive statistics were used. Comparative statistics were performed using χ2 tests or analysis of variance techniques where appropriate. All statistical analysis was performed using Stata/IC 15.1 (StataCorp LLC, College Station, Tex). This study was deemed exempt by the institutional review board at the University of Pennsylvania.
Survey Results
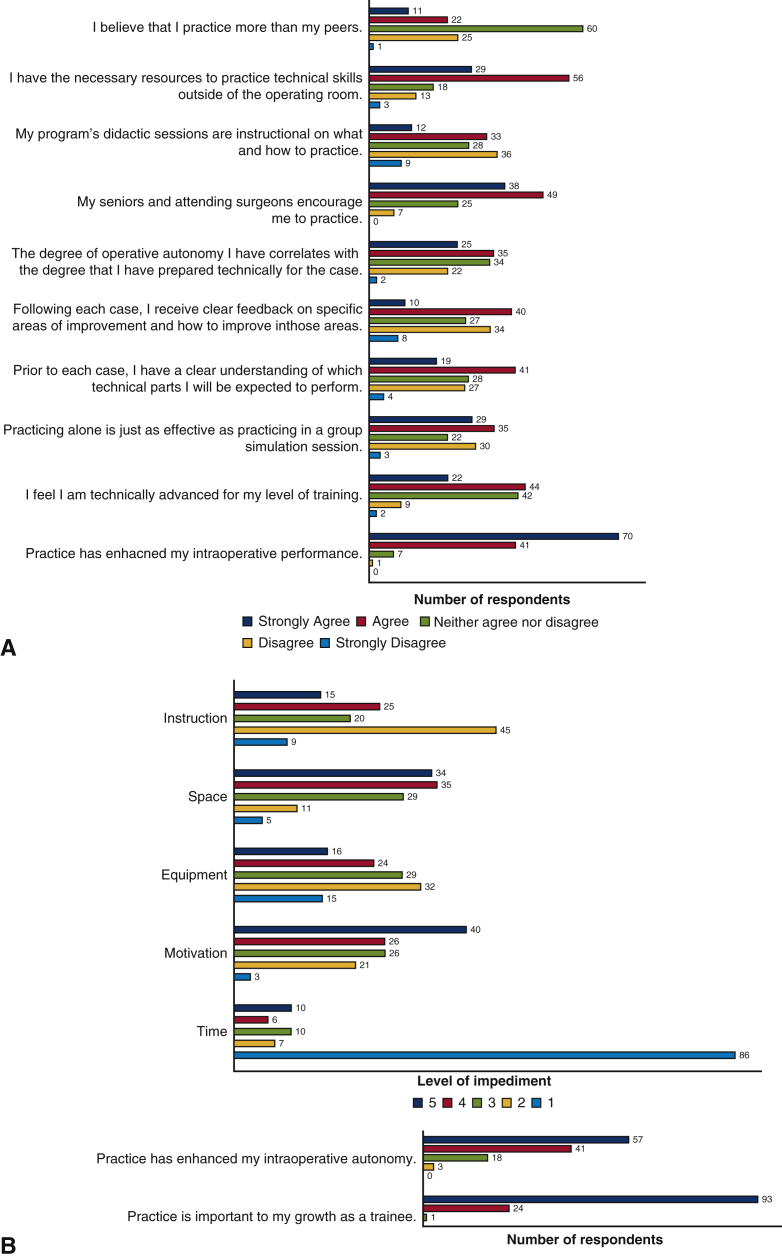
The survey was completed by 119 trainees (24.7%). The majority agreed or strongly agreed that practice is important to their growth (98%, 117/119) and that practice generally enhances intraoperative performance (93%, 111/119) and autonomy (82%, 98/119). Most felt they received encouragement to practice from seniors and attendings (73%, 87/119).
Most trainees believed they practice the same or less than their peers (72%, 86/119). Most reported practicing less than 2 hours per week (71%, 85/119), whereas a small minority noted practicing more than 5 hours per week (6%, 7/119). The majority of trainees reported practicing at home (59%, 70/119), whereas fewer reported practicing in a simulation laboratory (24%, 29/119) or other settings within a hospital (17%, 20/119). Approximately one half viewed practicing alone to be just as effective as practicing within group simulation sessions (53%, 64/119; Figure 1).
Figure 1.
Survey results. A, Attitudes regarding practice among cardiothoracic surgery trainees. Trainees rated their level of agreement to several statements regarding their attitudes towards practice on a scale of strongly disagree to strongly agree. B, Impediments to practice. Trainees rated several factors on a scale of 1 to 5 on level of impediment to practice, with 1 being biggest impediment and 5 being lowest impediment.
Trainees who practice at least 1 to 2 hours per week reported practicing mostly at home, whereas those who practice less than 1 to 2 hours reported practicing mostly outside their home (P = .01). Practicing at least 1 to 2 hours per week correlated with feelings of enhanced operative performance (P < .01), autonomy (P < .01), and likelihood of receiving encouragement (P < .01) and clear feedback (P = .02).
Lack of time was perceived to be the largest impediment to practice (78%, 93/119; Figure 1, B), followed by lack of adequate instruction (47%, 54/114) and adequate practice equipment (40%, 47/116), especially among those who practice at home (P = .02). Lack of space was the least significant barrier to practice (14%, 16/114). Only 42% (50/119) felt they received clear feedback on specific areas of improvement and ways to improve following an operative case (Figure 1).
Discussion
In this survey of current cardiothoracic surgery trainees, the majority reported that practicing outside of the operating room was helpful to improving their skills and enhancing their intraoperative performance. Most reported practicing alone or at home and noted that their greatest impediments were lack of time, equipment, and instruction. To help foster a culture of practice, especially while remaining mindful of physical and social restrictions imposed on training by the coronavirus pandemic (COVID-19), we aimed to address each of these concerns with practical solutions.
Simulator Blueprint: DIY, At-Home, Modular, and Virtually Conducive
First, we offer an early, viable framework of a DIY simulator platform to facilitate the convenient practice of surgical skills at home. These models have not been previously outlined in print, although early video proofs of concepts have been presented.2,3
Do-it-yourself, affordable, accessible
In our model, all items had to be inexpensive and easily obtainable from a regular hardware store, or an online source such as Amazon (Table 1). To aid in distribution of concept and implementation, a shopping list was created on Amazon Prime (https://www.amazon.com/hz/wishlist/ls/1V7DT73HQ33GI?ref_=wl_share) with essential starter items.
Table 1.
List of required materials
| Item | Cost |
|---|---|
| Shoebox | – |
| Surgical gloves | – |
| Wooden boards (5 × 10 inch) | $7.50 |
| Small nails | $5.49 |
| Rubber bands | $5.49 |
| Small screw eye | $0.75 |
| Rice | $8.08 |
| Small plastic bags | $8.69 |
| Felt | $11.99 |
| Hair ties | $5.25 |
| Triple Grip Third Hand (Micro-Mark, Berkeley Heights, NJ) | $12.65 |
| Medium-sized twisting balloons | $17.10 |
| Duct tape | $5.93 |
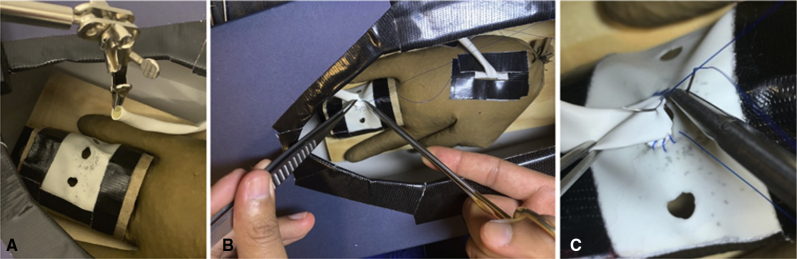
Modular design with graduated complexity
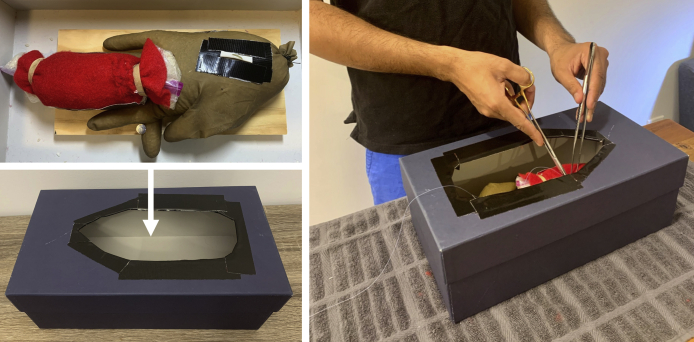
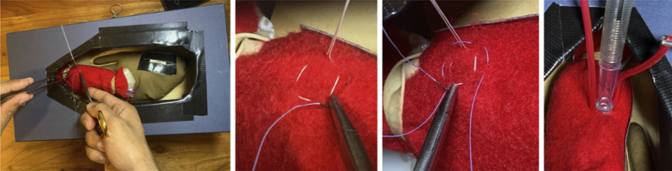
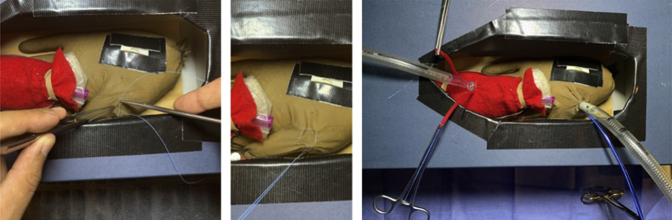
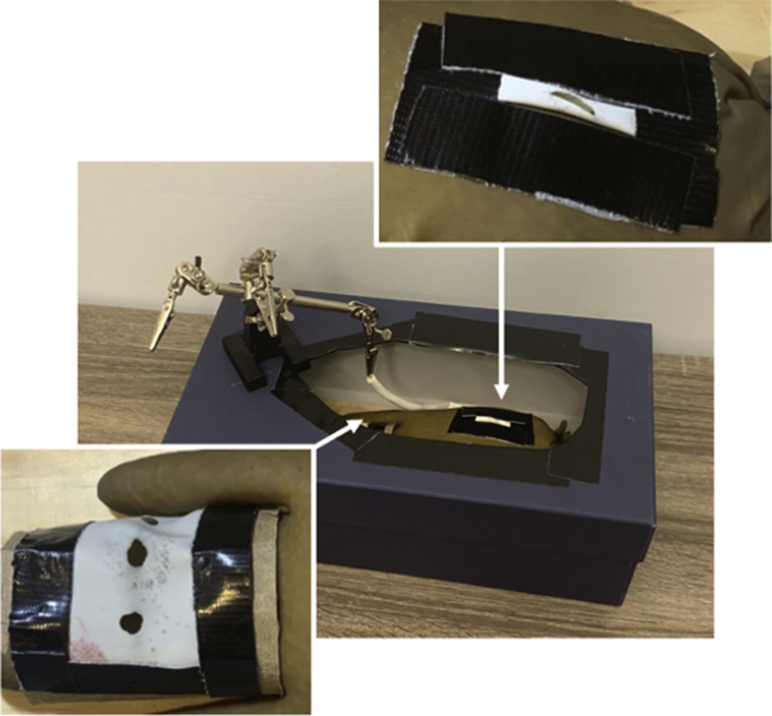
To allow for practice of multiple aspects of cardiac surgery, we used a modular concept in design. A shoebox with an oval hole cut out of the lid serves as the structural foundation to simulate the size and depth of a median sternotomy. Interchangeable inserts are placed within the box to allow for practice of a variety of skills (Figure 2). Based on this modular design, here we outline potential drills that trainees can set up at home to practice a variety of techniques in cardiac surgery:
-
1.Fundamental skills
-
•Linear suturing (Figures E1 and E2)
-
•Needle angles (Figure E3)
-
•Knot tying (Figure E4)
-
•
-
2.Cannulation drills
-
•Aortic cannulation (Figures E5 and E6)
-
•Venous cannulation (Figure E7)
-
•Bicaval cannulation (Figure E8)
-
•Left ventricular vent cannulation (Figure E9)
-
•
-
3.Coronary anastomosis drills
-
•Distal anastomosis (Figures E10 and E11)
-
•Proximal anastomosis (Figure E12)
-
•
Figure 2.
Simulator design. In our “do-it-yourself” simulator model, a shoebox with an oval hole cut out of the lid is used to simulate a median sternotomy. Various modules are placed inside the shoebox to allow for simulation of multiple aspects of cardiac surgery. Each individual module is constructed from inexpensive, readily obtainable items, including felt, surgical gloves, nails, a wooden board, rubber bands, and balloons, as shown here.
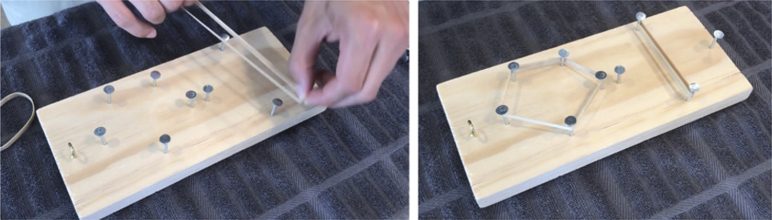
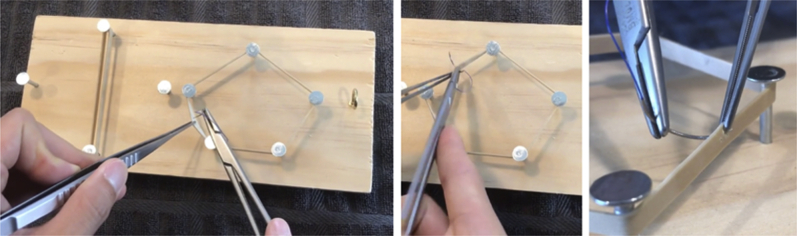
Figure E1.
Basic surgical skills module. The basic skills module is constructed by arranging nails in cross and pentagonal shapes on a 5- × 10-inch wooden board. The nails are used as anchors around which rubber bands are positioned as shown.
Figure E2.
Linear suturing. A rubber band is positioned around 2 anchoring points. The orientation may be parallel or perpendicular to the trainee. Needles can be passed forehand (shown), backhand, or alternating (shown). A full-length suture can be used to practice appropriate suture spacing. Alternatively, a needle with only a small suture tail can be used to focus on needle angles, needle handling and reloading, and forceps dexterity.
Figure E3.
Annular suturing. A rubber band is positioned around 4 or 5 anchoring points to create an annular shape. Needles can be passed forehand, backhand, or alternating. A full-length suture can be used to practice appropriate suture spacing. Alternatively, a needle with only a small suture tail can be used to focus on needle angles, needle handling and reloading, and forceps dexterity.
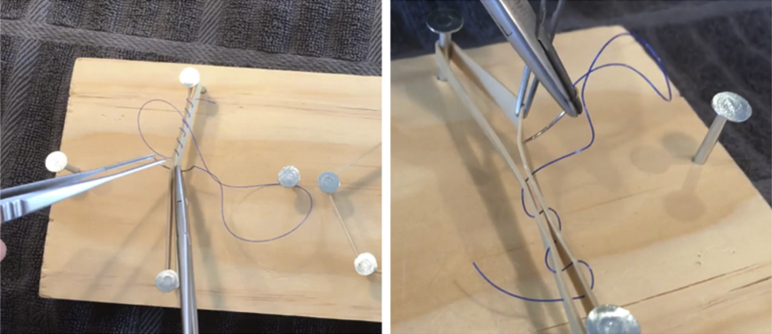
Figure E4.
Knot tying. A small screw eye is used for practicing knot tying. Alternatively, knots can be tied around rubber bands. Suture (shown), free ties, or fine sewing thread can be used.
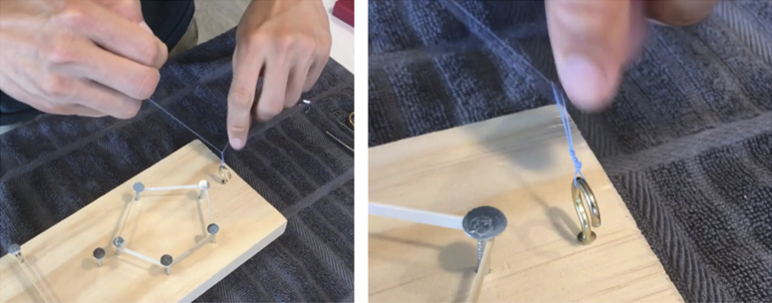
Figure E5.
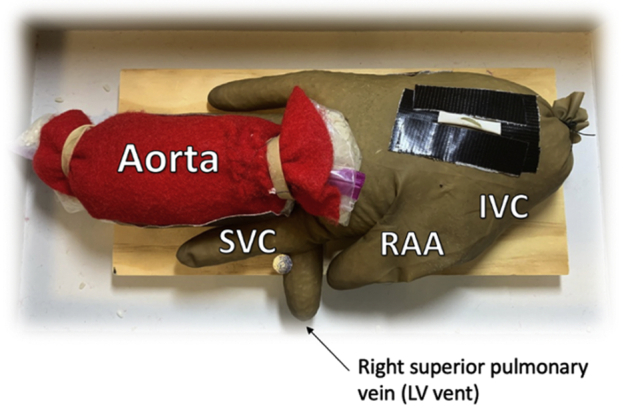
Cannulation module. A left-handed surgical glove simulates the heart. It is filled with rice to give shape and volume. The first finger serves as the superior vena cava (SVC), the second finger is angled using a nail and simulates the right superior pulmonary vein, the thumb serves as the right atrial appendage (RAA), and the base represents the inferior vena cava (IVC). A small plastic bag is filled with rice and wrapped in felt to simulate the ascending aorta. LV, Left ventricular.
Figure E6.
Aortic cannulation. Purse-string sutures are positioned on the lesser curvature of the simulated aorta. The felt layer allows for practice of partial-thickness bites.
Figure E7.
Right atrial cannulation. The thumb of the left-sided surgical glove simulates the right atrial appendage. Purse-string sutures can be positioned on the face of this surface or around it to simulate cannulation of the face (shown) or the appendage of the right atrium, respectively.
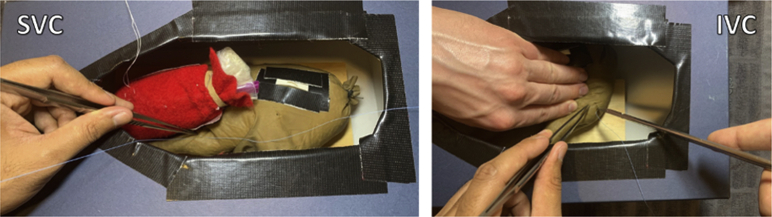
Figure E8.
Bicaval cannulation. A purse-string suture is placed in the first finger of the glove, which simulates the superior vena cava (SVC). Cannulation of the inferior vena cava (IVC) is simulated by reflecting the glove cranially and flattening its surface.
Figure E9.
Left ventricular vent cannulation. A purse-string suture is positioned in the second finger of the surgical glove, which is angled laterally using a nail to simulate the right superior pulmonary vein.
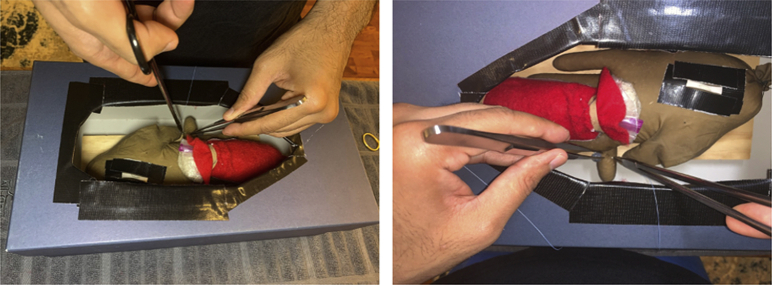
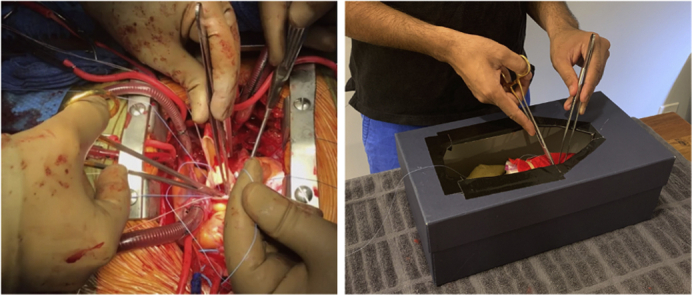
Figure E10.
Coronary module. Twisting balloons are cut into short segments and taped onto the rice-filled glove in the distribution of the left anterior descending (shown), obtuse marginal, and right coronary. A small “arteriotomy” is made in each segment with a knife or fine scissor. With the twisting balloons positioned in the orientation of the coronaries, the rice-filled glove can be positioned to simulate the exposure of each distal anastomosis. To simulate the ascending aorta, a large square hole is cut in the center of a toilet paper roll, over which a piece of surgical glove with small holes is taped.
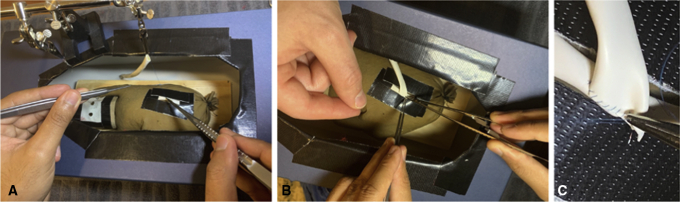
Figure E11.
Distal anastomosis. The Third Hand is positioned on the lid of the shoebox with an alligator clip pointing downwards, which holds the free graft (A). Release of the alligator clip allows the graft to “parachute” down (B) and the anastomosis can be completed (C).
Figure E12.
Proximal anastomosis. The Triple Grip Third Hand (Micro-Mark, Berkeley Heights, NJ) is positioned on the lid of the shoebox with an alligator clip pointing downwards, which holds the free graft (A). Release of the alligator clip allows the graft to “parachute” down (B) and the anastomosis can be completed (C).
Can DIY Simulation Help Integrate Practice Into Trainees' Busy Schedules?
Lack of time was identified as the greatest impediment to practice in our survey. Many different low- and high-fidelity models or practice regimens for simulation training have been proposed over the years, some offered regionally versus nationally, and some provided in a bootcamp setting versus as a part of a longitudinal curriculum.4, 5, 6, 7, 8, 9, 10, 11, 12 Whatever the method, to establish a culture of practice, our survey results reinforce the notion that it must be mindful of the users' scarcity of time, energy, and motivation and ensure that trainees find the process as convenient and streamlined as possible. Sometimes, trainees may only have 10 to 20 minutes to practice before sleeping to prepare for a case the next day. Similarly, they may only have a brief duration between cases to practice immediately after leaving the operating room based on feedback received from the attending surgeon. Thus, optimizing the efficiency of a simulator can transform practice from a major undertaking into a routine component of a trainee's schedule, reversing the perception that there is “too little time.”
A successful paradigm must optimize accessibility, affordability, and ease-of-use, as outlined herein. While commercial simulators currently exist on the market, and some have been distributed to senior trainees with funding from programs or national organizations, their cost is often prohibitive for use at a more general level such as with junior residents, operative advanced practice providers, and even subinterns preparing for rotations. Moreover, a simulator should be durable enough to withstand the wear-and-tear of repetitive suturing. While materials such as silicone and animal tissue are highly effective for certain types of teaching sessions, they are prone to wearing-down and decomposing, respectively. For these reasons, our DIY model is made with inexpensive, durable, and easily replaceable parts such as rubber bands, felt, balloons, hair ties, and surgical gloves, which reduce set-up and clean-up time. By contrast, models that require the users to carefully reconstruct or reset after each use can discourage repetition.
Some trainees may feel there is not enough time to practice regardless of how convenient and easy the process becomes. Others may feel that they are operating enough to not require any practice. However, we contend that finding time is a matter of priority and motivation. It is important to acknowledge the utility of a simulator is not to replace operative experience, but rather to augment it. Similar to other areas of virtuosic performance such as music or athletics, performing the entire act or operating from skin-to-skin, while valuable, may not offer opportunities to hone a specific component with focus, repetition, and feedback. A trainee will only get to cannulate once during a case, but if he or she needs improvement, could practice placing cannulation sutures daily multiple times in the span of 30 minutes on a DIY simulator. Even competent residents may find opportunities to further hone their skills through simulation.
Socialization of Practice—A (Virtual) Platform for Instruction and Feedback
Instruction is essential in surgical simulation to ensure that trainees are practicing correct techniques that can be used in the operating room and not inadvertently learning bad habits. In our survey of cardiothoracic surgery trainees, inadequate instruction was identified as an important impediment to practice.
The concept of a DIY, at-home simulator may seem at first antithetical to receiving adequate feedback. However, we emphasize that while the trainee may physically be isolated, a DIY simulator is not only compatible with but rather more conducive to formal instruction and exchange of feedback among surgeons. The compact, lightweight construction allows for easy transport to and from the hospital or to each other's homes to practice whenever schedules allow. Trainees can bring their individual simulators to educational sessions led by attending surgeons or senior residents, reinforcing their practice sessions at home. Moreover, since supervision is a limited resource outside of the operating room in such a clinically demanding field, it allows for a synergy between supervised and unsupervised sessions. A trainee can use the DIY simulator in between cases or other in-person simulation sessions. For example, immediately after a coronary artery bypass, a trainee could practice the sutures of a distal coronary anastomosis to reinforce what they just learned before having the opportunity to perform the anastomosis again with attending supervision in the next case. It is this iterative learning model, alternating between supervision and independence, that the DIY simulator aims to inculcate.
Perhaps more importantly, in the era of the COVID-19 pandemic, the use of small, inexpensive cellphone stands or other cameras can transform formal educational sessions into remote video meetings with participants using DIY simulators from the comfort of their own homes. Here, there are several considerable advantages:
-
1.
Virtual technology allows teachers to simultaneously observe multiple trainees from optimal angles at the same time while also having the option of recording the session and carefully analyzing trainees' motions from multiple vantage points to provide detailed feedback.
-
2.
Virtual feedback sessions are much easier to organize logistically from home at more frequent intervals, as educators and trainees alike will no longer be required to find a considerable length of time that works for everyone in the same physical location. It may become realistic to have programs such as brief weekly check-ins with residents—either in group or one-to-one settings—who are working on specific skills.
-
3.
Remote sessions are also not limited to a single institution or a setting but can reach a broader audience online. Other users and institutions can modify our DIY blueprint to best serve their educational needs, naturally encouraging a crowdsourcing and sharing of new ideas from an international community.
Regardless of what simulator training programs choose to use, this philosophy allows ease of virtual teaching without limitations in class size, time, or regionality while facilitating high-quality practice at home with the ability for real-time, detailed feedback.
Limitations
This manuscript aims to convey the potential of a DIY simulation paradigm based on recent survey of cardiothoracic surgery trainees and to offer a viable framework as a starting point. However, it does not offer empirical data regarding its implementation or efficacy, which is the most important test of any simulation design. Prospective studies to validate this model are planned.
Conclusions
A survey of cardiothoracic surgery trainees reveals that the majority believe practice is important for improving surgical skill. Impediments to practice include time, instruction, and equipment. With these principles in mind, a DIY simulator can be easily constructed to practice various aspects of cardiothoracic surgery from the comfort of trainees' and instructors' homes. Especially in the era of a pandemic when virtualization is not a luxury but a necessity, we contend this paradigm is important to the future development of simulation techniques.
Footnotes
Drs Kelly and Han contributed equally to this article.
Disclosures: The authors reported no conflicts of interest.
The Journal policy requires editors and reviewers to disclose conflicts of interest and to decline handling or reviewing manuscripts for which they may have a conflict of interest. The editors and reviewers of this article have no conflicts of interest.
Appendix E1
Supplementary Data
Authors John J. Kelly, Amit Iyengar, and Mark R. Helmers discuss the design and applications of our “do-it-yourself” cardiac surgery simulator. Video available at: https://www.jtcvs.org/article/S2666-2507(21)00378-3/fulltext.
References
- 1.Han J.J., Patrick W.L. See one-practice-do one-practice-teach one-practice: the importance of practicing outside of the operating room in surgical training. J Thorac Cardiovasc Surg. 2019;157:671–677. doi: 10.1016/j.jtcvs.2018.07.108. [DOI] [PubMed] [Google Scholar]
- 2.Kelly JJ, Han JJ, Patrick WL, Mays JC, Iyengar A, Helmers MR, et al. Development of A Low-cost, Home-based Cardiac Surgery Simulator: Part I–Basic Skills Module [abstract]. Presented at: 100th Annual Meeting of the American Association for Thoracic Surgery; April 25-28, 2020; New York, NY.
- 3.Kelly J.J., Iyengar A., Patrick W.P., Helmers M.R., Smood B.F., Han J.J. Cardiac surgery simulation—part 1: basic surgical skills. Multimed Man Cardiothorac Surg. 2020;2020 doi: 10.1510/mmcts.2020.073. [DOI] [PubMed] [Google Scholar]
- 4.Fann J.I., Calhoon J.H., Carpenter A.J., Merrill W.H., Brown J.W., Poston R.S. Simulation in coronary artery anastomosis early in cardiothoracic surgical residency training: the Boot Camp experience. J Thorac Cardiovasc Surg. 2010;139:1275–1281. doi: 10.1016/j.jtcvs.2009.08.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hicks G.L., Jr., Gangemi J., Angona R.E., Jr., Ramphal P.S., Feins R.H., Fann J.I. Cardiopulmonary bypass simulation at the Boot Camp. J Thorac Cardiovasc Surg. 2011;141:284–292. doi: 10.1016/j.jtcvs.2010.03.019. [DOI] [PubMed] [Google Scholar]
- 6.Trehan K., Kemp C.D., Yang S.C. Simulation in cardiothoracic surgical training: where do we stand? J Thorac Cardiovasc Surg. 2014;147:18–24.e2. doi: 10.1016/j.jtcvs.2013.09.007. [DOI] [PubMed] [Google Scholar]
- 7.Feins R.H., Burkhart H.M., Conte J.V., Coore D.N., Fann J.I., Hicks G.L., Jr. Simulation-based training in cardiac surgery. Ann Thorac Surg. 2017;103:312–321. doi: 10.1016/j.athoracsur.2016.06.062. [DOI] [PubMed] [Google Scholar]
- 8.Ribeiro I.B., Ngu J.M.C., Lam B.K., Edwards R.A. Simulation-based skill training for trainees in cardiac surgery: a systematic review. Ann Thorac Surg. 2018;105:972–982. doi: 10.1016/j.athoracsur.2017.11.036. [DOI] [PubMed] [Google Scholar]
- 9.Mokadam N.A., Fann J.I., Hicks G.L., Nesbitt J.C., Burkhart H.M., Conte J.V. Experience with the cardiac surgery simulation curriculum: results of the resident and faculty survey. Ann Thorac Surg. 2017;103:322–328. doi: 10.1016/j.athoracsur.2016.06.074. [DOI] [PubMed] [Google Scholar]
- 10.Enter D.H., Lee R., Fann J.I., Hicks G.L., Jr., Verrier E.D., Mark R. “Top Gun” competition: motivation and practice narrows the technical skill gap among new cardiothoracic surgery residents. Ann Thorac Surg. 2015;99:870–875. doi: 10.1016/j.athoracsur.2014.09.051. [DOI] [PubMed] [Google Scholar]
- 11.Hossien A. Low-fidelity simulator for technical connection to the cardiopulmonary bypass. Multimed Man Cardiothorac Surg. 2016 Jan 25;2016:mmv041. doi: 10.1093/mmcts/mmv041. [DOI] [PubMed] [Google Scholar]
- 12.Durko A., Thuijs D., Mahtab E., Bekkers J. How to construct and use a low-fidelity coronary anastomosis simulator. Multimed Man Cardiothorac Surg. 2019;2019 doi: 10.1510/mmcts.2019.006. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Authors John J. Kelly, Amit Iyengar, and Mark R. Helmers discuss the design and applications of our “do-it-yourself” cardiac surgery simulator. Video available at: https://www.jtcvs.org/article/S2666-2507(21)00378-3/fulltext.