Abstract
Objective:
The consequences of a low autopsy rate are not considered in determining the cause of death.
Method:
We have analyzed the Cause of Death Register of the Swedish National Board of Health and Welfare since it started 1969 to and including 2016 to visualize the decline in the frequency of clinical autopsies over time and evaluated the effect on the quality of the cause of death diagnoses.
Results:
Over the five decades studied, the frequency of clinical autopsies declined from almost 40% to less than 5%. The rate of decline was not even. Political decisions and changes of healthcare organization in Sweden affected the slope of decline of autopsies superimposed on a linear decline over time reflecting changes in clinical routines. A request of clinical autopsies was highly dependent on the level of care at the time of death, with the lowest number of requests for persons who died in nursing homes. The age at the time of death was a major factor affecting the number of autopsies, resulting in an autopsy rate of less than 1% in the ages where most persons die. Although men were autopsied more often than women, a gender-specific difference was not seen after correction for the age of death. We also found a higher rate of unspecific and irrelevant diagnosis in the cases not autopsied and we know from earlier studies by us and other authors that the cause of death diagnoses were missed in between 30% and 50% of the cases not autopsied.
Conclusion:
The decline in the clinical autopsy rate reduced the value of the death certificate register. An increase in the number of autopsies performed will improve the understanding of disease and cause of death, as well as to better inform next of kin.
Keywords: Autopsy, cause of death, death certificate errors, clinical autopsy, forensic autopsy, gender differences, age dependence, autopsy and level of care
Introduction
The objective of this study concerns the quality of the healthcare system’s cause of death reporting. With the decreasing number of autopsies, death certificates based on only clinical diagnoses have become a dominant source of data on the cause of death. However, studies have reported that the documentation regarding the cause of death in death certificates is often inaccurate and incomplete. Cardiovascular deaths may be overestimated because of cardiovascular events being inappropriately labelled as the underlying cause of death on many death certificates.1,2 In a study by Hazard et al., 4 50 death certificates were reviewed, and in 82% of them, multiple errors were identified. The errors were the result of staff inexperience, fatigue, time constraints, lack of familiarity with the deceased, and a perceived lack of understanding about the importance of death certificates. 3 Other international studies have dealt with the ability of physicians to write accurate death certificates.4,5 In a study from Greece, 1 5828 death certificates relating to patients who had died of natural causes were studied. The findings showed that almost every certificate contained errors, of which 65% were regarded as major errors. They also found that the place of death was associated with the incidence of major errors, which appeared to relate more to primary care centres than to hospitals. The interpretation made was that death certificates cannot be used reliably as routine data for epidemiological research and public health policies as they do not accurately describe the cause of death. 1 In Sweden, the decline in post-mortem examinations has continued, despite several studies confirming the value of autopsies by demonstrating that non-diagnosed diseases such as cardiovascular diseases, infectious diseases and cancer were found at a markedly higher frequency after autopsy.6,7 This increased knowledge was essential for determining and registering the cause of death in more than a quarter of the cases that were examined.6,8
The consequences of the decline in the autopsy rate and doubt in the quality of the cause of death register are complex and hard to estimate, but involve kinsfolk, the healthcare system and society. It is obviously a risk that the statistics on causes of death are based mainly on clinical diagnoses that are not confirmed by autopsy.2,9,10 According to Bayer-Garner et al., 11 it is important that clinicians understand the value of an autopsy for the improvement of medical care and quality assurance. A lack of understanding of the value of an autopsy has been reported as a reason for the decline in autopsy rates. 11 Another study found that the main reason for not requesting an autopsy was the assumption that the cause of death was known, ignoring the value of the autopsy as a tool for quality control. 12 Autopsies have traditionally been used in undergraduate medical education; however, in recent decades, they have stopped being an important teaching tool, although several studies have confirmed their value.8,13–17 Burton and Underwood 18 state in their review in Lancet 2007 that autopsies are underused in clinical practice and highlight the importance of the fact that many doctors are not familiar with autopsy routines and underestimate their value.
The literature cited above describes a lack of incentive for the medical profession for quality assurance of cause of death diagnoses not requested by the authority. The post-mortem examination is expensive and introduces a risk of being criticized by next of kin for missed diagnosis and maltreatment. Currently, these questions are noted in several countries worldwide, but no activity has been observed that would remedy this contradiction between diagnostic quality and post-mortem examinations. A clear example of this is that neither of the healthcare insurance systems in the United States, Medicaid or Medicare, compensate for the costs of autopsies or have hospital autopsy competence as a requisite for getting support from these insurance programmes.
In this article, we have compared data extracted from the cause of death certificates based only on clinical information available before death, with certificates based on information gained by an autopsy. We also present data from the Cause of Death Register of the Swedish National Board of Health and Welfare from 1969, when the register gained its present form, to 2016. In a recent article from 2017 the Swedish cause of death register is described in more detail (ref nummer). The questions we address in this article concern the quality aspects of the register caused by a reduced autopsy rate: how does autopsy affect the quality of death certificate; how many certificates are missing or inappropriate in the register; and how do changes over time in the number and frequencies of clinical and forensic autopsies for men and women correlate to changes in the healthcare system concerning how dead people have been taken care of and where they die. 19
Materials and methods
This retrospective study comprises two parts: (a) one local case study on the cause of death of patients who died at a university hospital, some of whom were autopsied and some not, and (b) one national registry study from mortality statistics from the Swedish National Board of Health and Welfare.
(a) In the study of medical records and death certificates, we collected information on patients who were registered at the Karolinska University Hospital, Stockholm, between 2008 and 2009 and who died at the hospital. Over these 2 years, 1588 adult patients died at the hospital, of which 174 (11%) were autopsied. The clinics selected for the study comprised active research clinics, all of which were well experienced in handling patient deaths. These clinics were the same as those chosen for a previous study of nurses’ and physicians’ attitudes to autopsy 20 and a study on the process of handling autopsies, from receiving consent to reporting findings and diagnoses. 8 From the three clinics examined, we collected information on all patients who died and compared the relevance of the death certificates using the same criteria used by the National Board of Health and Welfare in its statistics. When the National Board of Health and Welfare only show the presented diagnoses codes, we compared the diagnoses on the death certificates with the data collected from the patients’ medical records.
From the pathology department, we received data regarding which patients had been given complete clinical post-mortem examinations and which patients had not been examined. Using this list, we collected the medical records and death certificates of the deceased patients at each ward. We compared the relevance of all diagnoses reported on the death certificates to information collected from the medical records on patients who had been autopsied or patients who had not been autopsied. We used the information on the main clinical diagnoses and the underlying cause of death. For estimation of relevance, we used the same classification of specific or unspecific diagnosis as used by the Swedish National Board of Health and Welfare in its statistics. Diagnoses on the death certificates supported by information in the medical records including results of ante-mortem diagnostic examinations using laboratory as well as imaging techniques were regarded as specific, while those that were not confirmed in medical records or that were too broad, such as heart failure, cardiac arrest and respiratory insufficiency, were regarded as unspecific. Post-mortem imaging techniques were not used at the hospital at the time of the study for the patients that were not autopsied.
(b) In the registry study, we used the Swedish official register on the cause of death, from its start in 1969 up to and including 2016. The register is maintained by the Swedish National Board of Health and Welfare, which also delivered the data on all people who died in Sweden during the years studied. All information was anonymized, and no individuals could be identified from the data we received from the authority. We asked for data on the number of deaths for men and women, age at the time of death, and the number of clinical and forensic autopsies performed on men and women in different age groups. We also asked for data regarding where the respective people had died, and the number of clinical and forensic autopsies performed on individuals who died in a hospital, nursing home, or in their own homes. In addition, we collected quality data on the information, that is, the number of death certificates missing and the number of certificates with unspecific information on the cause of death that could not be coded. The data were used to calculate the number of deaths and autopsy rates as presented in the figures below. We have chosen to present national data in which all regions in Sweden were included. The number of people registered as deceased in Sweden has been consistent since the end of the 1970s, when it reached 90,000, with a variation between years of around 5%. Data on the number of autopsies are the actual data and have not been corrected for the variations in the number of deceased people.
Ethics
The Regional Ethical Board in Stockholm approved this study (2011/208-31). The part of the study that uses anonymized data from the Swedish Board of Health and Welfare did not require ethical approval (2017/5:1).
Statistics
The statistic calculations presented in the study were performed by statistician Eva Hagel at the Medical Statistics Unit, Department of Learning, Informatics, Management and Ethics, Karolinska Institutet. The method used for this study was Fisher’s exact test.
Results
In the three clinics investigated in study A, we were able to access the death certificates of 221 cases. Of these cases, 178 had not been autopsied and 33 had been. In the cases that had not been examined after death, 27 of the diagnoses were classified as unspecific, while the number of cases that were examined after death, before completing the death certificate, was two. The differences between the clinics were noticeable in the number of autopsied cases, as well as in the number of unspecific diagnoses, with two clinics having no unspecific diagnoses and one clinic having two. The number of patients in this study is limited and, despite the indicative differences between autopsied and not autopsied patients, the difference was not significant (p value 0.268) but indicated that autopsies do improve the quality of the cause of death diagnosis. From a healthcare quality perspective, it is therefore of interest to describe the decline in autopsy rate over time on a national basis.
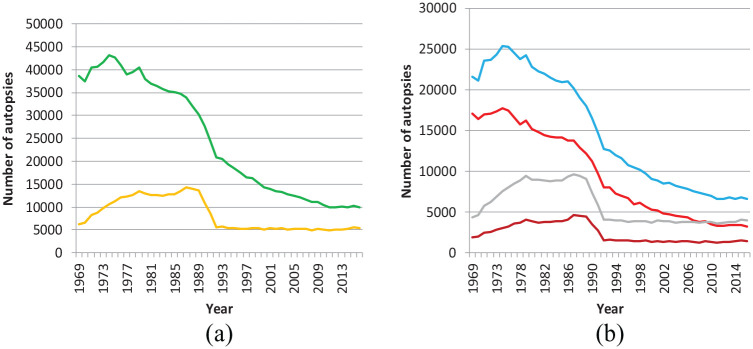
From the register study B, the number of post-mortem examinations performed on a national basis in Sweden from 1969 to 2016 is shown in Figure 1(a) and (b). Figure 1(a) shows the total number of autopsies performed, clinical and forensic, with a decline in the number of autopsies from around 40,000 per year to 10,000 per year, that is, a reduction of 30,000 examinations per year. From the slope of the curve, it can be concluded that the drop in the total number of autopsies has been constant, starting from the late 1970s. The forensic autopsies as presented in Figure 1(a) have also dropped but with a different slope. The steep reduction at around 1990 coincided with changes in the assignment of people who died outside hospitals or nursing homes. Forensic autopsies have been stable since the 1990s, with a total number of around 5000 cases per year.
Figure 1.
Number of autopsies in Sweden 1969–2016.
(a) Total number of clinical and forensic autopsies, 1969–2016.
 Total autopsy number
Total autopsy number  Forensic autopsies number.
Forensic autopsies number.
(b) Total number of clinical and forensic autopsies, 1969–2016.
 Men
Men  Women
Women  Forensic, Men
Forensic, Men  Forensic, Women.
Forensic, Women.
Figure 1(b) shows the total number of autopsies and the number of forensic autopsies on men and women. In the 1970s, almost half of all deceased persons (49% of men and 45% of women) were autopsied in Sweden, while in 2016 the total rate was 11%: 7% of women and 15% of men. It is interesting to note that although the numbers of deaths per gender are similar, women were examined less often than men in 2016.
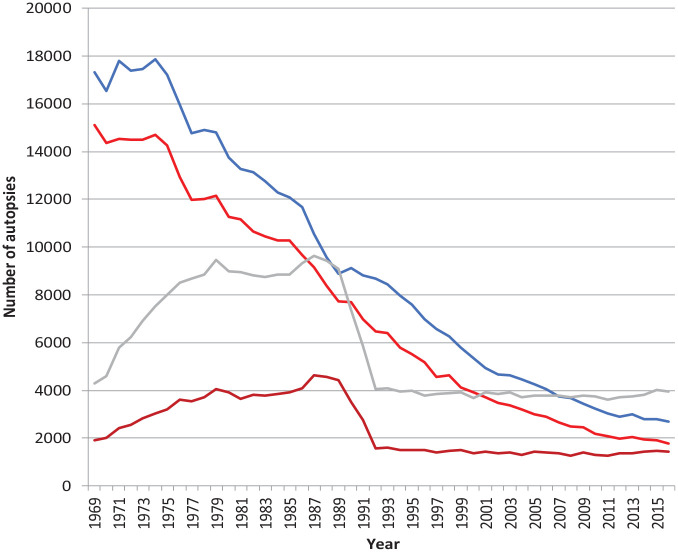
Figure 2 shows the number of clinical and forensic autopsies for men and women from 1969 to 2016. The slopes of the curves on clinical autopsies confirm the gradual decrease in the number of examinations for both sexes. From around 2007, the number of forensic examinations on men exceeded clinical autopsies – a situation that could also arise for women by around 2020.
Figure 2.
Number of clinical and forensic autopsies, men and women 1969–2016.
Clinical autopsy, men  Clinical autopsy, women.
Clinical autopsy, women. 
Forensic autopsy, men  Forensic autopsy, women.
Forensic autopsy, women. 
The frequencies of autopsies, autopsies performed/number of deaths, on both genders are shown in Figure 3(a) and (b). The total frequencies (Figure 3(a) include forensic and clinical autopsies. It is obvious that more men than women were examined, and this difference was persistent over time. In Figure 3(b), clinical examinations, the figures have been corrected for the effect of forensic examinations, showing that until 1990, male and female autopsy frequencies were the same and decreased at the same rate, while after 1990, clinical autopsies on men were more frequent than on women. In 1970, the frequency of clinical autopsies for men was 38% and for women 39%, while in 2016 the corresponding values were 6% for men and 4% for women.
Figure 3.
The frequency of total and clinical autopsies.
The number of autopsies per number of deaths, %
(a) Total autopsy rate men and women  Men
Men  Women.
Women.
(b) Clinical autopsy rate men and women  Men
Men  Women.
Women.
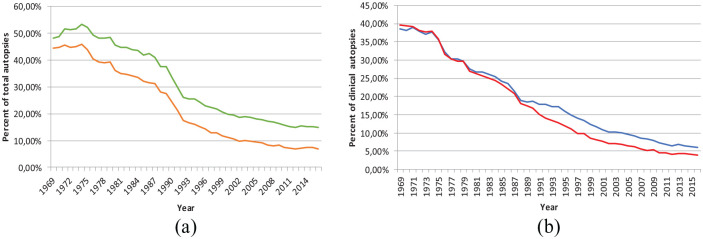
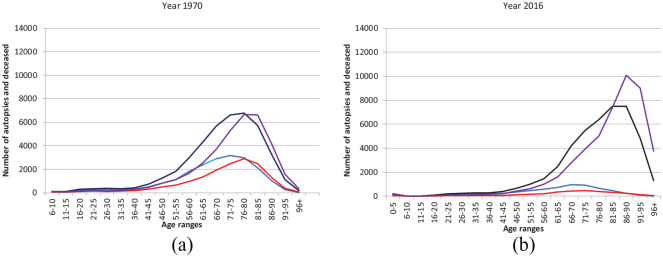
Figure 4(a) and (b) presents the autopsy frequencies for both sexes at different ages over the period we studied. In the 1970s, when the number of autopsies was still high, the relative autopsy rate was around 60% for both sexes and reasonably stable up to the age of around 60–65. For elderly people, the frequency decreased to below 20%. With the decreasing number of autopsies, it can be noted that the relative decrease was moderate for children under the age of 15 but very marked for elderly people, decreasing to less than 1% in the oldest age groups.
Figure 4.
The total autopsy frequency in different age groups. The number of total autopsies per number of deaths at different age groups. (a) Total autopsy frequency for men and women in 1970. (b) Total autopsy frequency for men and women in 2016.
Age groups  Men
Men  Women.
Women.
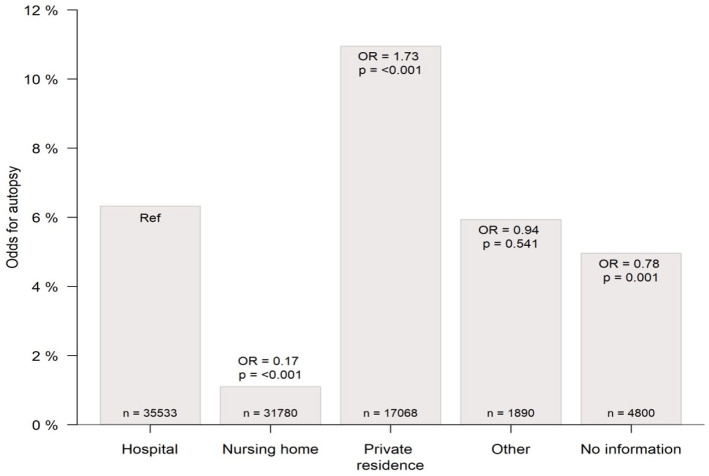
We also examined the frequency of autopsies dependent on the level of care and the location at which the person died (Figure 5). Because of an inconsistent procedure for reporting the place of death, we chose to report only from the end of the period, when the reports appear to be more reliable. From the register, it was noted that most men died in hospitals, while most women died in nursing homes. For both sexes, the number of people that died in their homes represented less than half of those that died in hospitals. The odds ratios for autopsies were significantly lower for nursing homes compared to hospitals (OR = 0.171, p0 < 0.001) and significantly higher for private homes compared to hospitals (OR = 1.578, p0 < 0.001). The figures for the whole country were comparable to those collected only from the city of Stockholm.
Figure 5.
The probability of autopsy depending on the level of care at the time of death.
n represents the number of people that died at each location during 2016.
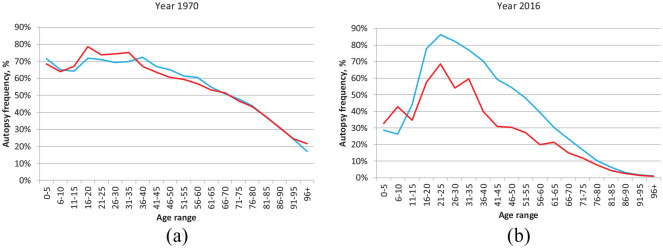
From the statistics, it appears that the relative number of autopsies is low at the highest ages, a trend that is more evident as the number of autopsies decreases. In Figure 6(a) and (b), we have graphically presented data from 1970 and 2016 on the number of people who died at different ages, and the number of autopsies performed on men and women at different ages. Men died at a slightly younger age than women. In 1970, the peak age at which most people died was 75–80 for men and 80–85 for women. At this time, the frequency of autopsies was still high, and the peak number of examinations coincided with the time when most people died. In the latter part of the investigated period, the age when people died was higher for both sexes: 80–85 for men and 85–90 for women, although the peak number of autopsies at this time, when the frequency of autopsies was significantly lower, did not coincide with the peak age of death. The conclusion that can be drawn from the data is that when fewer people were autopsied, the elderly were not selected.
Figure 6.
The number of autopsies and number of deceased men and women, age groups. (a) The number of autopsies and number of deceased men and women, 1970, age groups. (b) The number of autopsies and number of deceased men and women, 2016, age groups.
 Autopsy, men
Autopsy, men  Autopsy, women.
Autopsy, women.
 Deceased, men
Deceased, men  Deceased, women.
Deceased, women.
Although registration of the cause of death is mandatory and must be sent to the authority responsible for the register by the responsible physician within 3 weeks of death, a number of cases are missing. From 1997, when these types of data were available, up to 2015, the number of missing certificates gradually increased from around 0.5% to slightly below 1%. In addition to missing forms, some forms were not correctly filled in. In the inadequately completed forms, the cause of death was regarded as unspecific or too general to be related to a specific disease code. These forms represent around 2.5% of all cases registered. In total, these data indicate that registry data have a formal error frequency of 3.5%, including only missing and incorrectly completed forms (the numbers are not shown in figures or tables). To this error should be added uncertainty in diagnosis, particularly regarding cases that were not autopsied.2,3,8
Discussion
The dramatic reduction in clinical post-mortem examinations is a global phenomenon and has been reported on all continents for several decades.21–25 In countries such as the United Kingdom, the number of clinical autopsies is less than 1%, although most countries show numbers that are close to the autopsy rates in Sweden, that is, 11%. Turnbull et al. 25 describe the hospital autopsies in the UK 2013 as extinct in a quarter of the UK NHS Trusts and endangered in the rest. The statistics are, however, unclear and are not based on national statistics in all countries. The objective of this study concerns the quality of the cause of death diagnoses reported from the healthcare system. Our work in this article represents the first publication in recent years in which complete autopsy statistics in Sweden have been presented and evaluated.
We present in this article the national statistics over an extensive period regarding clinical and forensic post-mortem examinations. The Swedish register data mirror the global trend of reduction of clinical autopsies. Superimposed on this trend, our data also give a clear indication of how political decisions in Swedish healthcare have affected the willingness to request clinical autopsies after death from natural causes. In addition to our descriptive statistics, we show how autopsies increase the value of the cause of death certificate. With the low autopsy frequencies noted, we can conclude that the quality of the cause of death register is insufficient for its purpose and should motivate action from the authority responsible for the register. In addition, it also affects the quality of the information given to next of kin, a situation that will probably cause an increase in the number of autopsies requested by the relatives of the deceased. 8
In the register part of this study, we present data originating from the death register of the Swedish National Board of Health and Welfare over a period of 46 years, from 1969 up to and including 2016. During this period, the authority registered death in Sweden in a consistent way suitable for comparative studies over time. It is obvious that during the period in which we had access to complete data on causes of death in the register, medical care has changed dramatically. Technical developments increased medical knowledge, and better treatment has led to a perception that autopsies may no longer be necessary.24,26,27 Other drastic changes are that patients do not spend as much time in the healthcare system as they did just a decade or two ago and often die in their homes or in community nursing homes. The mortality register is influenced not only by medical priorities but also by political decisions and changes in the organization of healthcare in the society and the education of the medical profession.13,28
The decline in the number of autopsies was not a straight line but comprised three different phases. The decline became evident at the beginning of the 1980s but accelerated at the end of that decade and the beginning of the 1990s. It is obvious from the shape of the curve that the decline is at least biphasic and composed of one almost constant decline over time in combination with a more abrupt change in the early 1990s. The steep slope at the beginning of the 1990s can be explained by a change in the definition of forensic examinations. Before 1989, forensic pathologists examined all deceased people who died outside hospitals or nursing homes. In 1989, it was decided that only people for whom an unnatural cause of death could not be excluded should be examined by forensic pathologists. 29 People who died outside hospitals or nursing homes and in cases where there was no suspicion of the unnatural cause of death were transported to hospital morgues but were rarely examined. 28 In this reform, forensic examinations were reduced from 14,000 cases per year to about one-third, with a limited effect on the number of clinical examinations. The abrupt reduction of forensic examinations is related to a reduction of the number of examinations performed by forensic pathologists on persons that died of natural causes or disease. It can be argued that this reform created a situation where unnatural death or crime was not detected. Since then, forensic autopsies have been constant at around 5000 cases per year. Clinical autopsies performed at the pathology departments of hospitals decreased rapidly and constantly from 30,000 in the mid-1970s to just below 10,000 in the year 2000. By 2010, the number of clinical autopsies was around 5000, slowly decreasing thereafter.
The decrease in the frequency of clinical autopsies, not including forensic examinations, was very similar for males and females until the 1990s. After this time, there was a noticeable and consistently higher frequency of male clinical autopsies compared to females. From our data, we can conclude that the men died younger than women, and more men than women were examined at forensic departments at any age group up to the age of 70. The gender difference that appeared for the frequency of clinical autopsies was minor and did not depend on a selection process in which women were not selected for an autopsy simply because they were women. Rather, the reasons related to the age at which the person died and the tendency not to request autopsies at higher ages. The gender difference for children was not consistent and could not be confirmed.
The age of death was important regarding the decision to request a post-mortem examination. Children and young people below 15 years of age were examined at a frequency of around 40%, increasing to 70% between 20 and 45 years of age, from which point it decreased, reaching the lowest frequencies of below 5% at above 80 years of age. Half of the children who died before the age of 10 were examined by forensic pathologists and half in hospital pathology departments, reflecting that children often died from accidents. From the age of 15 and up to the age of 45–50 years, forensic autopsies were dominant for both genders, with a relative overweight for men. Above 80 years of age, there was no gender difference in forensic examinations. In general, all deceased people transferred to forensic departments were examined, which is a major difference compared to people who died of natural causes in the healthcare system.
In the healthcare system, the level of care affected the decision to perform a post-mortem examination. From the register, we extracted information on autopsies on people who died in a hospital, in a nursing home, or in their own homes. It could be concluded from the partly incomplete data from 2016 that the tendency to request an autopsy was higher if the person died at home than if the death occurred in a hospital, where the responsible physician probably had access to more clinical information about the disease that caused the death. The lowest frequency was found if death occurred in a nursing home, where patients were of a higher age and where the focus was on care at the end of life rather than on diagnostic investigations and treatment. We saw no significant differences between national figures in this respect in comparison to data from Stockholm. The Swedish National Board of Health and Welfare is responsible for the Cause of Death Register and the quality of the data, and therefore also collects data on compliance with the regulations on how healthcare providers report the cause of death. When the form is filled in, the physicians only have access to the clinical data available in the medical record. If an autopsy is needed, it must be requested. There is, however, no requirement for post-mortem examinations, and an increasing number of death certificates are filled in based only on clinical data. The quality of the register depends on the quality of the data reported and that all deaths are reported. Although reporting cause of death is mandatory, not all death certificates reached the authority and not all certificates contained data that were specific enough to understand the cause of death. In the Swedish Cause of Death Register, between 1% and 1.5% are not reported and around 2% are reported with diagnoses that are too unspecific and broad to be included in the diagnosis-specific register. These two reported sources of error together represented 3.5% of all deaths. The judgement of the authority about whether a diagnosis was specific was not based on a clinical evaluation of the deceased but solely on the specificity of the diagnostic term and how it could relate to a specific disease process. This decision was performed by a computer, based on a list of terms defined by the authority.
To illustrate the accuracy or relevance of the diagnostic terms used in our clinical material we have, in this article, looked at the specificity of diagnostic terms used in relation to existing clinical information from the medical records in cases where the cause of death was reported after a post-mortem examination or just based on clinical information without the support of an autopsy. In our evaluation, we selected three different university clinics at which personnel were experienced in the care of patients who were dying. The limitation of the study is the insufficient number of deaths examined, but we choose to use the data from these clinics because we have in the past performed two other studies on these clinics investigating the attitudes to autopsies among physicians and nurses as well as the quality and clinical usefulness of autopsies performed on deceased patients from these wards. Altogether, we found that of the 178 cases that were not autopsied, the number of cases reported to the authority with unspecific diagnoses was 27, while unspecific diagnoses after autopsy were less frequent, amounting to two of 33 cases. Even though the number of patients was too small for a significant result, we could conclude that unspecific diagnoses in death certificates were not rare and were most probably more frequent than suggested by the numbers presented by the Swedish National Board of Health and Welfare. In fact, post-mortem examinations contributed to a more accurate cause of death of higher relevance to the medical condition that caused the patient’s death. Ylijoki-Sørensen et al. 30 compared unspecific or ill-defined and unknown causes of death in Finland where the autopsy frequency has been maintained at a high level (25%–30%) with the same diagnosis codes in Denmark, where the total autopsy frequency is below 4%. All unspecific diagnoses were significantly higher in Denmark (13-fold) than in Finland. In Finland, all patients with unknown causes of death are autopsied. In addition, data from a Finnish study on validation of cause of death certificates that were questioned by the statisticians pointed out the value of correct mortality statistics.30,31
When it comes to evaluation of the cause of death, the quality of the death register could be questioned, not only because of missing certificates and unspecific diagnoses but also because without autopsies we can assume that there are many diagnoses that should have been included in death certificates that are missing. The relevance of post-mortem examinations to the accuracy of diagnoses has been well documented in several reports, including studies from our own hospital.6,7 In our own studies from 2017, we were able to conclude that clinically significant diagnoses were missing in more than 60% of cases when autopsies were not performed. 8
The autopsy as a clinical tool has developed from being virtually a mandatory process to an exceptional event, rarely requested. Therefore, today’s physicians are not trained to order an autopsy and the healthcare routine does not include this tool. The use of autopsies as an educational tool has decreased significantly over the last two decades in Sweden. 32 Many physicians in Swedish healthcare are educated abroad and have no or little experience of post-mortem examination. In 2010, 50% of the newly employed physicians were educated abroad. 33 Autopsies are emotionally challenging learning situations, and students need to participate in multiple autopsies to learn about procedures and the manifestation of pathological changes. 34 It is therefore not surprising that many physicians do not request an autopsy and are satisfied with the results of the clinical investigations and consider themselves capable of completing death certificates properly.
In our view, a way of balancing the shortcomings that result from a low autopsy rate is to inform those working in the healthcare system about these deficiencies and their consequences and raise awareness of the value of autopsy for medical staff, scientists, authorities and relatives to the deceased. It is therefore necessary to increase the use of autopsies as a learning tool in undergraduate education.13,15,35 This will change the attitudes and interests of the medical profession and nursing staff in clinical autopsies and could eventually increase the number of autopsies requested. Education will improve the ability of medical and nursing staff to communicate more effectively with relatives regarding the purpose of autopsies and the value of the information that is currently often inaccurate and incomplete. The implementation of educational programmes for this purpose will eventually also improve the quality of death certificates.
Conclusion
The quality of the cause of death diagnosis is highly dependent on whether an autopsy has been performed or not. The frequency of clinical post-mortal examinations has declined over the last three decades in most western countries. We have in this article visualized the decline in clinical autopsies in Sweden during the last five decades extracting data from the Cause of Death Register of the Swedish National Board of Health and Welfare since 1969. Despite the fact that the value of a clinical autopsy as a tool for determining the cause of death is not disputed, the frequency of clinical autopsies has been going down from a national level of almost 50% to below 5%. In the elderly age groups, the clinical autopsy rate was even lower going down to less than 1% in the age groups where most people die. The willingness to request autopsies was higher for people that died at relatively young ages compared to people that died at high age, especially those that die in a nursing home. There were no gender-specific differences noticed although more men were autopsied than women. This apparent difference could be explained by the fact that women died at higher ages than men and therefore were less often autopsied.
The quality of the Cause of Death Register is highly dependent on that the death certificates are properly filled in and sent to the Swedish National Board of Health and Welfare in time. More than 98% of the deaths were reported and less than 2% of the reported deaths were not registered since the diagnoses listed were unspecific and could not be classified. The most severe threat to the quality of the register was, however, that an overwhelming number of death certificates were not based on information from a post-mortal examination. It has been well studied and convincingly shown that between 30% and 50% of the cause of death diagnoses are missed when autopsies are not performed, jeopardizing the quality of the register. With an autopsy frequency below 5% and missed diagnoses between 30% and 50%, the value of the register must be questioned. If the statistic value of the register shall be preserved, the number of clinical autopsies performed has to be increased to the benefits of the stakeholders of this information among authorities, scientists and not the least relatives to the diseased. In this article, we conclude that the decline in the clinical autopsy rate reduced the value of the death certificate register. An increase in the number of autopsies performed will improve the understanding of disease and cause of death, as well as to better inform next of kin. We suggest that the awareness of the shortcomings of cause of death diagnoses should be more widely spread and that autopsies as a tool in clinical education and training should be reintroduced for the education of medical staff, physicians as well as nurses.
In summary
The number of clinical autopsies in Sweden has declined from almost 50% to less than 5% during the last five decades.
The decline over time correlates to changes in the role of the forensic departments as well as to political changes in healthcare organizations.
The frequency of total post-mortem examination is highly dependent on the age at which patients die but also on where persons die. At the age where most people die, autopsies are rare, less than 1%
The quality of the cause of death diagnosis is highly dependent on whether an autopsy has been performed or not.
An increase in post-mortem examination by autopsies or post-mortem imaging techniques is necessary to improve the cause of death accuracy and information to next of kin.
Acknowledgments
We would like to acknowledge Jesper Hörnblad, quality manager for the Cause of Death register at the Swedish National Board of Health and Welfare for extracting the register data and statistician Eva Hagel at Karolinska Institutet for her help with the statistical analyses. We would also like to thank Christina Takman for her valuable help with this manuscript.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: Ethical approval for this study was obtained from The Regional Ethical Board in Stockholm with approval number (2011/208-31). We also applied to the Regional Ethical Board for the part of the study that uses anonymized data from the Swedish Board of Health and Welfare. The Board decided that this register study did not require ethical approval (2017/5:1).
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Informed consent: Written informed consent was obtained from all subjects before the study.
ORCID iD: Anders Rosendahl  https://orcid.org/0000-0002-5953-5267
https://orcid.org/0000-0002-5953-5267
References
- 1. Filippatos G, Andriopoulos P, Panoutsopoulos G, et al. The quality of death certification practice in Greece. Hippokratia 2016; 20(1): 19–25. [PMC free article] [PubMed] [Google Scholar]
- 2. Lakkireddy DR, Gowda MS, Murray CW, et al. Death certificate completion: how well are physicians trained and are cardiovascular causes overstated? Am J Med 2004; 117(7): 492–498. [DOI] [PubMed] [Google Scholar]
- 3. Pritt BS, Hardin NJ, Richmond JA, et al. Death certification errors at an academic institution. Arch Pathol Lab Med 2005; 129(11): 1476–1479. [DOI] [PubMed] [Google Scholar]
- 4. Hazard RH, Chowdhury HR, Adair T, et al. The quality of medical death certification of cause of death in hospitals in rural Bangladesh: impact of introducing the International Form of Medical Certificate of Cause of Death. BMC Health Serv Res 2017; 17(1): 688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Miki J, Rampatige R, Richards N, et al. Saving lives through certifying deaths: assessing the impact of two interventions to improve cause of death data in Peru. BMC Public Health 2018; 18(1): 1329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Alafuzoff I, Veress B. The selection for post-mortem examination: a retrospective analysis of 74 deceased surgical cases. Qual Assur Health Care 1993; 5(4): 345–349. [DOI] [PubMed] [Google Scholar]
- 7. Britton M. Diagnostic errors discovered at autopsy. Acta Med Scand 1974; 196(3): 203–210. [DOI] [PubMed] [Google Scholar]
- 8. Rosendahl A, Mjörnheim B, Takman C, et al. The clinical value of autopsies at a university hospital in Sweden. Nord J Nurs Res 2017; 37(3): 119–126. [Google Scholar]
- 9. Johansson LA, Björkenstam C, Westerling R. Unexplained differences between hospital and mortality data indicated mistakes in death certification: an investigation of 1,094 deaths in Sweden during 1995. J Clin Epidemiol 2009; 62(11): 1202–1209. [DOI] [PubMed] [Google Scholar]
- 10. Tejerina EE, Padilla R, Abril E, et al. Autopsy-detected diagnostic errors over time in the intensive care unit. Hum Pathol 2018; 76: 85–90. [DOI] [PubMed] [Google Scholar]
- 11. Bayer-Garner IB, Fink LM, Lamps LW. Pathologists in a teaching institution assess the value of the autopsy. Arch Pathol Lab Med 2002; 126(4): 442–447. [DOI] [PubMed] [Google Scholar]
- 12. Blokker BM, Weustink AC, Hunink MG, et al. Autopsy of adult patients deceased in an academic hospital: considerations of doctors and next-of-kin in the consent process. PLoS ONE 2016; 11(10): e0163811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Bamber AR, Quince TA. The value of postmortem experience in undergraduate medical education: current perspectives. Adv Med Educ Pract 2015; 6: 159–170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Bamber AR, Quince TA, Barclay SI, et al. Medical student attitudes to the autopsy and its utility in medical education: a brief qualitative study at one UK medical school. Anat Sci Educ 2014; 7(2): 87–96. [DOI] [PubMed] [Google Scholar]
- 15. Brooks EG, Thornton JM, Ranheim EA, et al. Incorporation of autopsy case-based learning into PhD graduate education: a novel approach to bridging the ‘bench-to-bedside’ gap. Hum Pathol 2017; 68: 1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Ioan B, Neagu M, Manoilescu I, et al. Utility of autopsy in medical education–students’ opinions and attitudes. Rev Med Chir Soc Med Nat Iasi 2014; 118(3): 801–807. [PubMed] [Google Scholar]
- 17. McNamee LS, O’Brien FY, Botha JH. Student perceptions of medico-legal autopsy demonstrations in a student-centred curriculum. Med Educ 2009; 43(1): 66–73. [DOI] [PubMed] [Google Scholar]
- 18. Burton JL, Underwood J. Clinical, educational, and epidemiological value of autopsy. Lancet 2007; 369(9571): 1471–1480. [DOI] [PubMed] [Google Scholar]
- 19. Brooke HL, Talback M, Hornblad J, et al. The swedish cause of death register. Eur J Epidemiol. 2017;32: 765–773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Mjörnheim B, Rosendahl A, Eriksson LC, et al. Attitudes of nurses and physicians about clinical autopsy in neonatal and adult hospital care: a survey in Sweden. Nurs Res 2015; 64(4): 264–271. [DOI] [PubMed] [Google Scholar]
- 21. Goldman L, Sayson R, Robbins S, et al. The value of the autopsy in three medical eras. N Engl J Med 1983; 308(17): 1000–1005. [DOI] [PubMed] [Google Scholar]
- 22. Maeda S, Kamishiraki E, Starkey J, et al. Why are autopsy rates low in Japan? Views of ordinary citizens and doctors in the case of unexpected patient death and medical error. J Healthc Risk Manag 2013; 33(1): 18–25. [DOI] [PubMed] [Google Scholar]
- 23. Oluwasola OA, Fawole OI, Otegbayo AJ, et al. The autopsy: knowledge, attitude, and perceptions of doctors and relatives of the deceased. Arch Pathol Lab Med 2009; 133(1): 78–82. [DOI] [PubMed] [Google Scholar]
- 24. Scordi-Bello IA, Kalb TH, Lento PA. Clinical setting and extent of premortem evaluation do not predict autopsy discrepancy rates. Mod Pathol 2010; 23(9): 1225–1230. [DOI] [PubMed] [Google Scholar]
- 25. Turnbull A, Osborn M, Nicholas N. Hospital autopsy: endangered or extinct? J Clin Pathol 2015; 68(8): 601–604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Ayoub T, Chow J. The conventional autopsy in modern medicine. J R Soc Med 2008; 101(4): 177–181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Bassat Q, Castillo P, Alonso PL, et al. Resuscitating the dying autopsy. PLoS Med 2016; 13(1): e1001927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Lindstrom P, Janzon L, Sternby NH. Declining autopsy rate in Sweden: a study of causes and consequences in Malmo, Sweden. J Intern Med 1997; 242(2): 157–165. [DOI] [PubMed] [Google Scholar]
- 29. Rammer L, Gustavsson E, Forsberg M, et al. Shortcomings in the coverage of death occurring outside hospitals. Lakartidningen 1997; 94(50): 4759–4763. [PubMed] [Google Scholar]
- 30. Ylijoki-Sørensen S, Sajantila A, Lalu K, et al. Coding ill-defined and unknown cause of death is 13 times more frequent in Denmark than in Finland. Forensic Sci Int 2014; 244: 289–294. [DOI] [PubMed] [Google Scholar]
- 31. Lahti RA, Penttilä A. Cause-of-death query in validation of death certification by expert panel; effects on mortality statistics in Finland, 1995. Forensic Sci Int 2003; 131(2–3): 113–124. [DOI] [PubMed] [Google Scholar]
- 32. Rosendahl A. Has the clinical autopsy played its role? Karolinska Institutet, 2019, https://openarchive.ki.se/xmlui/bitstream/handle/10616/46747/Thesis_Anders%20Rosendahl.pdf?sequence=1&isAllowed=y
- 33. Närlid M. Every second newly hired doctor educated abroad. Lakartidningen 2010; 39: 2304–2305. [Google Scholar]
- 34. Weurlander M, Scheja M, Hult H, et al. Emotionally challenging learning situations: medical students’ experiences of autopsies. Int J Med Educ 2012; 3: 63–70. [Google Scholar]
- 35. Van den Tweel JG, Wittekind C. The medical autopsy as quality assurance tool in clinical medicine: dreams and realities. Virchows Arch 2016; 468(1): 75–81. [DOI] [PMC free article] [PubMed] [Google Scholar]