Abstract
Study Design:
This is a systematic review.
Objective:
To systematically review (1) the reliability of the physical examination of the spine using telehealth as it pertains to spinal pathology and (2) patient satisfaction with the virtual spine physical examination.
Methods:
We searched EMBASE, PubMed, Medline Ovid, and SCOPUS databases from inception until April 2020. Eligible studies included those that reported on performing a virtual spine physical examination. Two reviewers independently assessed all potential studies for eligibility and extracted data. The primary outcome of interest was the reliability of the virtual spine physical exam. Secondary outcomes of interest were patient satisfaction with the virtual encounter.
Results:
A total of 2321 studies were initially screened. After inclusion criteria were applied, 3 studies (88 patients) were included that compared virtual with in-person spine physical examinations. These studies showed acceptable reliability for portions of the low back virtual exam. Patient satisfaction surveys were conducted in 2 of the studies and showed general satisfaction (>80% would recommend).
Conclusions:
These results suggest that the virtual spine examination may be comparable to the in-person physical examination for low back pain, though there is a significant void in the literature regarding the reliability of the physical examination as it pertains to specific surgical pathology of the spine. Because patients are overall satisfied with virtual spine assessments, validating a virtual physical examination of the spine is an important area that requires further research.
Keywords: spine, surgery, cervical, virtual physical exam, telemedicine, COVID-19
Introduction
Technological advancements have revolutionized communication between individuals, thus profoundly affecting human relationships. One of the key relationships that has been changed by advances in communication is that between the patient and the provider. Telemedicine is defined by The Institute of Medicine as “the use of electronic information and communications technologies to provide and support health care when distance separates participants.” 1,2 It has allowed for rapid access to shared and remote medical expertise, no matter where the patient or relevant information is located. 3 Essentially, telemedicine has allowed the utilization of telecommunications for the purpose of diagnosing and treating patients in remote locations. 4
Technologies used for telemedicine have significantly increased in popularity in recent years in the fields of both medicine and surgery. With advancements in computer sciences and engineering, health care providers are able to provide care and education to patients without being limited by geographic location. Naturally, this would erode barriers such as cost, distance to travel, childcare, time from work, or other factors that would have otherwise prevented patients from receiving the care they need. One systematic review demonstrated that telemedicine reduced costs by up to US $176 by significantly reducing both the distance traveled and time spent. 5 Ultimately, this allows greater access to specialty care in rural locations or areas that are experiencing medical shortages. 4 Although one can raise the argument that lack of in-person interaction would decrease the quality of care and reduce patient satisfaction, several studies have shown the contrary, 6 -8 with equivalent efficiency, similar satisfaction, and significantly reduced patient costs for the video visits. 8 As such, telemedicine has been applied to a wide array of surgical specialties, including, endocrine surgery, orthopaedics, ENT, colorectal surgery, vascular surgery, neurosurgery, transplant, oncological surgery, urology, and pediatric and plastic surgery. 2,5,9
In today’s current world of COVID-19, spinal surgeons are in need of accurate, validated, and comprehensive virtual physical exams because nonessential visits have been postponed or canceled in many parts of the world. In order for a spine surgeon to properly perform a telemedicine visit, a virtual spine physical exam that is both reliable and practical must be available for use. We, therefore, sought to perform a systematic review to evaluate the available evidence in regard to the virtual spine physical exam as it pertains to the evaluation and diagnosis of spinal pathology. This information has the potential to be widely applied beyond the current pandemic to allow access to care in remote areas where subspecialists may not be readily available.
Materials and Methods
Search Strategy
We performed a systematic review following the guidelines outlined by the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA). Two independent reviewers in duplicate searched the EMBASE, PubMed, Medline Ovid, and SCOPUS databases from inception until April 2020 using the search terms (spine OR spinal OR back OR ‘low back’ OR neurologic OR neck OR cervical OR thoracic OR lumbar) AND (physical OR exam) AND (telemedicine OR telehealth OR virtual OR ‘video visit’ OR ‘phone visit’ OR ‘remote visit’) in all possible combinations.
Study Screening
All titles, abstracts, and full texts were screened in duplicate by 2 reviewers (JP, BBB) to assess all potential studies for eligibility. Any disagreements at the title and abstract stages were discussed among the reviewers and resolved by the senior author. Consensus was reached for final eligibility of all articles.
Assessment of Study Eligibility
We defined inclusion and exclusion criteria for this systematic review a priori. Inclusion criteria were studies (1) in English, (2) on humans, (3) pertaining to the use of a virtual (video or telephone) or remote exam (not in person, not using an assistant to perform the physical exam), and (4) pertaining to the physical examination of cervical, thoracic, or lumbar pathology. Exclusion criteria consisted of nonclinical studies. The primary outcome of interest was the reliability of the virtual spine or back physical exam. Secondary outcomes of interest were patient satisfaction with the virtual exam.
Assessment of Study Quality
To assess the quality and potential risk for bias in the included studies, the Methodical Index for Non-Randomized Studies (MINORS) 10 was utilized. This is a validated instrument specifically designed to asses and index the quality of nonrandomized control studies using a set of 12 items to be assessed for each study. Each item is given a grade of either 0 (not reported), 1 (reported, but inadequate), or 2 (reported and adequate). A MINORS score was calculated for each included study and reviewed by 2 team members for consistency.
Data Abstraction and Statistical Analyses
Data relating to the virtual examination of the cervical, thoracic, or lumbar spine was abstracted from the included studies. Demographic data was also abstracted, including study author, publication year, study type, type of virtual assessment (video vs telephone), age and sex of patients, and region of the spine examined. Descriptive statistics are presented with weighted means or percentages where applicable. Information on patient satisfaction with the virtual encounter was also abstracted from the included studies when possible.
Results
Study Identification
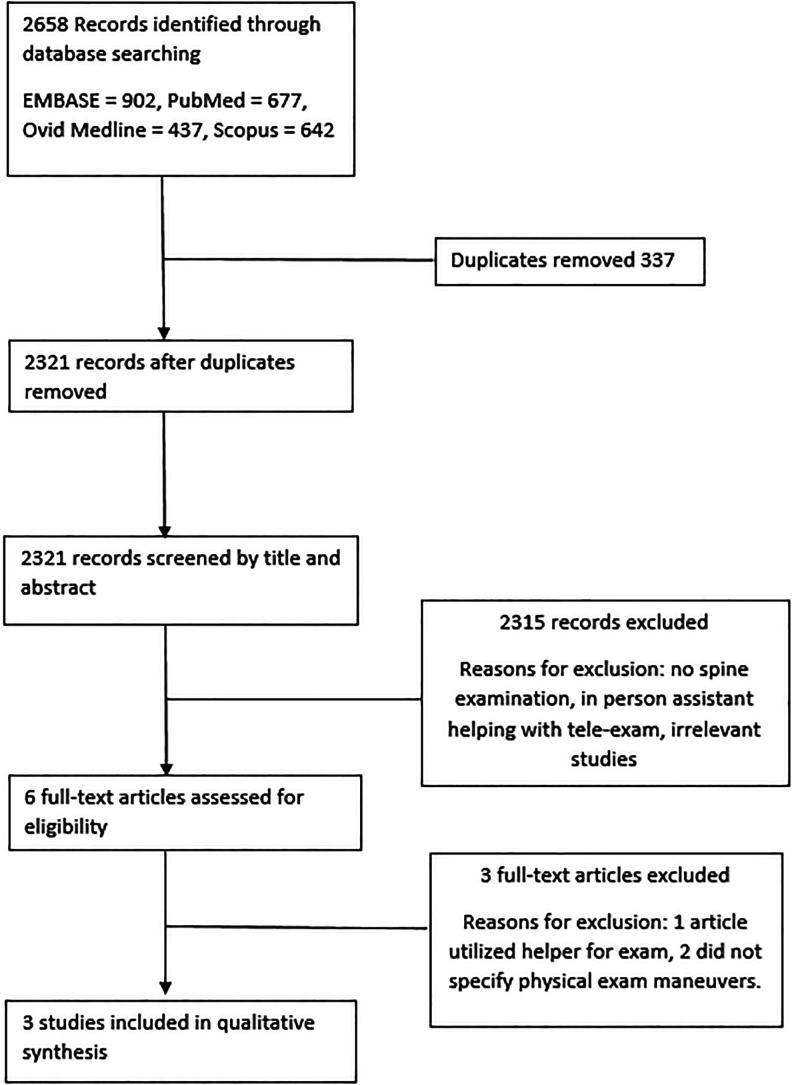
The results of the search are synthesized in Figure 1. Of 2658 records initially identified, 337 duplicates were then removed, leaving 2321 unique records, which were then screened by 2 independent reviewers (JP, BBB). The first level of screening consisted of an assessment of titles and abstracts to identify all potentially relevant studies. A total of 2315 records were removed because they either did not perform a virtual back or spine physical exam, used an in-person assistant to help with the virtual exam, or were otherwise irrelevant. Any disagreements were resolved by the senior author (IA). This resulted in 6 possible studies for a secondary review. A thorough full-text assessment of these studies was then performed to ensure that they met all inclusion criteria. At this level of review, 3 articles were excluded. One article used an in-person assistant for the virtual exam, and 2 articles did not mention performing or assessing any virtual physical exam maneuvers. The remaining 3 articles 11 -13 were found to utilize audiovisual electronic communication to perform a spinal exam. See Table 1 for study demographics.
Figure 1.
Flowchart of selected studies.
Table 1.
Demographics of Included Studies.
| Study authors | |||
|---|---|---|---|
| Truter et al 11 | Palacín-Marín et al 12 | Peterson et al 13 | |
| Publication year | 2014 | 2013 | 2018 |
| Study design | Single-blinded validation | Descriptive study of repeated measures | Descriptive study of repeated measures |
| Telemedicine type | eHAB conference system | “TPLUFIB-WEB” web-based system | Zoom teleconferencing system |
| Total n | 26 | 15 | 47 |
| Sex, n (%) | Male: 11 (42%) | Male: 6 (40%) | Male: 14 (30%) |
| Female: 15 (58%) | Female: 9 (60%) | Female: 33 (70%) | |
| Average age, years | 43 | 37 | 48.6 |
| Spine region examined primarily | Lumbar | Lumbar | Lumbar |
Virtual Spine Exam
Truter et al 11 performed a single-blinded validation study of 26 patients with low back pain comparing telerehabilitation assessments of spinal posture, passive straight leg raise (SLR), and active movements of the lumbar spine, with a face-to-face assessment by a physical therapist. Patients were first randomized to either undergoing a video assessment or face-to-face assessment. All patients underwent both exams, but in a different order, and a different physical therapist performed each exam. Posture was assessed in the coronal and sagittal planes. In the coronal plane, therapists evaluated patients for clinically evident scoliosis and postural symmetry. In the sagittal plane, they assessed lumbar lordosis, thoracic kyphosis, and overall alignment. Active movement assessment entailed evaluation of flexion, extension, and lateral flexion of the spine and grading these as either full or restricted. For evaluation of SLR, the classic description was performed during the face-to-face assessment, but during the video assessment, the patient’s friend or an untrained nonclinical assistant aided in maintaining full knee extension with flexion of the hip, and for that reason, the results of this aspect of their exam are excluded from our analysis. Results from this study showed no statistically significant agreement for postural assessments between the face-to-face and video assessments. The authors found statistically significant (P ≤ .001) percentages of exact agreement in identifying if a spinal movement was painful. In evaluation of lumbar range of motion, a strong correlation was found in flexion (r = 0.89) and extension (r = 0.83) measurements. When analyzing the quality of this study, a MINORS score of 22 was calculated, with the only points deducted being for lack of mention of a prospective calculation of needed sample size.
Palacín-Marín et al 12 performed a descriptive study of repeated measures using a crossover design of 15 individuals with low back pain. This study also attempted to assess the likeness of an in-person assessment to a teleassessment. The outcomes of interest included lumbar spine mobility, back muscle endurance assessments, and lumbar motor controls. All patients completed questionnaires related to disability, pain, health-related quality of life, and kinesiophobia. Statistical analysis performed included Cronbach reliability estimates. On all categories, the Cronbach α reliability estimate between telerehabilitation and face-to-face systems was either good (α = .75) or very good (α = .94-.96). When analyzing the quality of this study, a MINORS score of 22 was calculated, with the only points deducted being for lack of mention of a prospective calculation of needed sample size.
Peterson et al 13 conducted a similar study in which 47 patients with low back pain underwent both a face-to-face assessment and a telerehabilitation encounter and then were categorized into a specific therapy protocol. Outcomes of interest included SLR, the active SLR, judgments of centralization/peripheralization, and judgments of aberrant motion. Once these were assessed, patients were then classified into an intervention group. Uniquely, the SLR was performed by the patient using a belt to passively elevate the leg with the knee in extension until resistance was felt. Analysis performed identified no statistically significant differences in the judgment on different variables between the virtual and in-person exam except for SLR greater than 91°, for which there was only a 35.1% agreement. The remaining variables had 48.9% to 59.6% agreement. For a summary of physical exam results, see Table 2. When analyzing the quality of this study, a MINORS score of 24 was calculated, with no points being deducted.
Table 2.
Reliability of Virtual Spine Physical Exam as Compared With In-person Exam.
| Study authors | |||
|---|---|---|---|
| Truter et al 11 | Palacín-Marín et al 12 | Peterson et al 13 | |
| Reliability measure | Pearson correlation (P value) | Cronbach α | Percentage agreement (P value) |
| Exam components | Lumbar flexion (cm): 0.89 (<.0001) | Lateral flexion (degrees): .751 | Centralization/peripheralization: 48.9 (.84) |
| Lumbar extension (cm): 0.83 (<.0001) | Finger-floor distance frontal (cm): .992 | Straight leg raise >91°: 35.1 (.00) | |
| Lateral flexion right (cm): 0.69 (<.0001) | Finger-floor distance ride side lateral (cm): .972 | Straight leg raise >10° asymmetry: 55.3 (.30) | |
| Lateral flexion left (cm): 0.67 (.001) | Sorensen test: .796 | Straight leg raise large but <91°: 53.2 (.51) | |
| Anterior straight leg rise: .968 | Active straight leg raise: 56.4 (.18) | ||
Patient Satisfaction With the Virtual Exam
Both Truter et al 11 and Peterson et al 13 evaluated patient satisfaction with telerehabilitation assessments. Truter et al 11 used a six 100-mm Visual Analog Scale (VAS) to assess satisfaction. They noted that overall, patients reported a good level of satisfaction with the virtual encounter, reporting a mean VAS score >80 for overall satisfaction and >80 when asked if participants would recommend the virtual exam to someone who cannot travel. However, there was not a good level of satisfaction when participants were asked if they thought that the virtual exam was as good as the in-person exam, with a mean VAS score of <40. Notably, the reasons why patients may not have felt the virtual exam was as good as the in-person exam were not further explored or reported. Peterson et al 13 used a 5-point Likert Scale to assess patient satisfaction. Overall, they reported that 56% of patients noted that the teleassessment was as good as the face-to-face assessment and that 97% of patients agreed or strongly agreed that they would recommend telerehabilitation to someone unable to travel. The exact number of participants studied for these responses was not reported; only the raw percentages were made available. Similar to the study by Truter et al, 11 for the 44% of participants who did not feel that the virtual exam was as good as the face-to-face exam in this study, the reasons for this were not further explored or reported. See Table 3 for a comprehensive summary of patient satisfaction results.
Table 3.
Patient Satisfaction With Virtual Spine Exam.
| Study and measurement tool | Would recommend to friend unable to travel | Virtual exam as good as face-to-face exam | Could see therapist at all times/visual clarity | Could hear therapist at all times/audio clarity | Felt equally connected | Confidence in exam | Overall satisfaction |
|---|---|---|---|---|---|---|---|
| Truter et al 11 : mean response on 100-mm VAS | >80 | <40 | >65 | >65 | Did not assess | >60 | >80 |
| Peterson et al 13 : percentage agreement on Likert Scale | 97 | 56 | 83 | 98 | 66 | Did not assess | Did not assess |
Abbreviation: VAS, Visual Analog Scale.
Discussion
The present review found 3 studies that evaluate the reliability of the virtual physical examination of the spine as compared with the in-person exam, with overall heterogeneous results. These studies did show acceptable reliability for some virtual low back pain physical exam maneuvers and showed poor reliability and disagreement on others. Overall, these studies show that the virtual spine examination may be comparable to the in-person physical examination for low back pain in certain aspects. However, these studies were significantly limited because they only performed small portions of the lumbar spine examination, primarily pertaining to the physical therapy literature. Specifically, a comprehensive physical examination of the cervical, thoracic, or lumbar spine that would be of aid to the diagnosis of the specific spinal pathology via telemedicine platforms was not found. This includes detailed telemedicine assessments of upper and lower motor strength, comprehensive dermatomal sensory exams, or reflexes, in the context of performing a dedicated spine exam. Although the reviewed studies are a good foundation for further investigation, they also highlight the need for a validated virtual comprehensive physical examination of the spine.
With regard to satisfaction, the present review found that 2 of the 3 studies identified reported on patient satisfaction, both showing that patients were satisfied and would recommend the exam to someone unable to travel. However, both studies also showed that many patients in these studies did not think the exam was as good as the face-to-face assessment. Unfortunately, neither study further investigated why patients may have felt that the virtual exam was not as good as the in-person one. This is potentially valuable information that likely warrants further study. Although these 2 small and limited studies do show some promise in regard to potential patient satisfaction with the virtual spine physical exam, further research and higher-quality evidence is needed to adequately address this issue, particularly with a more focused physical examination of the spine as well as further investigation into patient satisfaction.
This systematic review did identify some interesting results in studies that were focused on telemedicine physical exams of very specific neurological patient subsets (stroke, multiple sclerosis and polyneuropathy), although usually requiring an in-person assistant to aid in the physical exam portion in most cases. It is evident that teleneurology has already established itself as a reliable alternative for face-to-face encounters, especially in rural and underserved areas. It has been shown that there is good reliability between in-person and telemedicine assessment of strokes utilizing the National Institutes of Health Stroke Scale (NIHSS) and modified NIHSS (mNIHSS). 14 The NIHSS and mNIHSS both include limited motor (assessing for extremity drift) and basic sensory exams as part of their assessment. 14 Although these scales and assessments are designed for a very specific subset of patients, the virtual use of these exams to accurately identify and change medical management provide some insight into the future possibilities for the treatment of spine patients.
In the polyneuropathy literature, there is evidence that the Veterans Affairs Neuropathy Scale can be successfully administered via telemedicine to examine, diagnose, and monitor polyneuropathy symptoms in patients. 15,16 This scale assesses components such as gait, Romberg test, knee reflexes, and pinprick sensation, 15 again all partial components of a comprehensive spinal exam. Unfortunately, these exams currently require an in-person assistant to complete all portions successfully, limiting their completion to certain subsets of patients.
Similarly, in the multiple sclerosis literature, studies have investigated the reliability of performing a telemedicine assessment of the Expanded Disability Status Scale (EDSS). The EDSS is a scale specifically designed to assess disability and function over time in multiple sclerosis patients and incorporates very basic aspects of motor and sensory examinations. 17 Kane et al 18 found variable agreement between the in-person and remote examiners on different aspects of the EDSS, though once again, an assistant was required to complete the physical exam.
Within the orthopaedic physiotherapy literature, there is limited available evidence with regard to the reliability of performing any aspect of the general orthopaedic physical exam via telemedicine without an assistant. Cabana et al 19 investigated the reliability of the telemedicine physical exam on postoperative total knee arthroplasty patients. They compared exam findings such as swelling, knee range of motion, and scar appearance between the telemedicine and in-person exams. Overall, they found variable reliability in the agreement between the different aspects of the exam and concluded that further research with a larger number of participants was needed. Russell et al 20 assessed diagnostic accuracy of in-person versus telemedicine evaluations of ankle pain in a small subset of 15 patients. Part of this included performing a virtual physical examination of ankle range of motion, single-leg squat, and gait. Their outcome of interest was solely obtaining the correct diagnosis. They reported good reliability in forming the correct ankle pathological diagnosis between the telemedicine and in-person exams. No analysis was performed grading the virtual exam against the face-to-face exam.
Strengths and Limitations
The present study is the first to systematically review the evidence with regard to the virtual physical examination of the spine, providing both an overview of the present state of the literature as well as optimism regarding use and overall patient satisfaction with telemedicine in patients with spinal pathology. Importantly, the present study provides future direction for critical research in this area. This study is limited by the strength of evidence of available literature on the topic, which was primarily level 2 and 3 evidence given the study design of the included studies. However, when assessing the quality of these studies using the MINORS criteria, the quality of these studies was acceptable. Other limitations include small patient samples of 26, 15, and 47, respectively. Additionally, given the fact that the 3 included studies reported on different physical exam maneuvers and used heterogeneous statistical reporting methods, it was not possible to perform any meaningful meta-analysis of their findings. This again highlights the need for future research into a validated comprehensive virtual spine examination. Finally, the 3 included studies all utilized new patients who were recruited for study purposes. Therefore, no distinction is able to be made on whether or not there are any differences in the effectiveness or patient satisfaction of a virtual spine exam between new patients or established patients who have already developed a patient-physician relationship. Developing and maintaining a strong patient-physician relationship is an important component of providing quality patient care, and whether or not this relationship can be reliably formed via telemedicine in regard to spine patients is still unknown. Similarly, because neither study that assessed patient satisfaction further assessed why some patients did not feel that the virtual exam was as good as the in-person exam, this also leaves a void of valuable information that warrants further future investigation.
Conclusion
As technology and health systems continue to advance, the role and demand for telemedicine in delivering efficient, convenient, and appropriate care to patients will continue to expand. Whereas many fields in medicine have already begun investigating and incorporating telemedicine exams into their practice, this has not yet occurred as prominently in spine surgery. The purpose of this systematic review was to perform a comprehensive summary of the literature that exists on performing a virtual spine physical exam. Although limited studies have begun to investigate aspects of this, this review found that there is no validated or reliable comprehensive spine virtual physical exam that would allow the accurate diagnosis of pathology pertaining to the cervical, thoracic, or lumbar spine. This review highlights significant need for further research and evidence in this area to provide the best possible care for patients with limited access or resources.
Footnotes
Authors’ Note: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Ilyas Aleem, MD, MS  https://orcid.org/0000-0003-4818-8578
https://orcid.org/0000-0003-4818-8578
References
- 1. Institute of Medicine Committee on Evaluating Clinical Applications of Telemedicine, Field MJ. Telemedicine: A Guide to Assessing Telecommunications in Health Care. National Academies Press; 1996. [PubMed] [Google Scholar]
- 2. Harting MT, Wheeler A, Ponsky T, et al. ; APSA Informatics and Telemedicine Committee. Telemedicine in pediatric surgery. J Pediatr Surg. 2019;54:587–594. [DOI] [PubMed] [Google Scholar]
- 3. Strehle EM, Shabde N. One hundred years of telemedicine: does this new technology have a place in paediatrics? Arch Dis Child. 2006;91:956–959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Huang EY, Knight S, Guetter CR, et al. Telemedicine and telementoring in the surgical specialties: a narrative review. Am J Surg. 2019;218:760–766. [DOI] [PubMed] [Google Scholar]
- 5. Gunter RL, Chouinard S, Fernandes-Taylor S, et al. Current use of telemedicine for post-discharge surgical care: a systematic review. J Am Coll Surg. 2016;222:915–927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Portnoy JM, Waller M, De Lurgio S, Dinakar C. Telemedicine is as effective as in-person visits for patients with asthma. Ann Allergy Asthma Immunol. 2016;117:241–245. [DOI] [PubMed] [Google Scholar]
- 7. Wang CD, Rajaratnam T, Stall B, Hawa R, Sockalingam S. Exploring the effects of telemedicine on bariatric surgery follow-up: a matched case control study. Obes Surg. 2019;29:2704–2706. [DOI] [PubMed] [Google Scholar]
- 8. Viers BR, Lightner DJ, Rivera ME, et al. Efficiency, satisfaction, and costs for remote video visits following radical prostatectomy: a randomized controlled trial. Eur Urol. 2015;68:729–735. [DOI] [PubMed] [Google Scholar]
- 9. Valente DS, Eifler LS, Carvalho LA, Filho GAP, Riberio VW, Padoin AV. Telemedicine and plastic surgery: a pilot study. Plast Surg Int. 2015;2015:187505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg. 2003;73:712–716. doi:10.1046/j.1445-2197.2003.02748.x [DOI] [PubMed] [Google Scholar]
- 11. Truter P, Russell T, Fary R. The validity of physical therapy assessment of low back pain via telerehabilitation in a clinical setting. Telemed J E Health. 2014;20:161–167. [DOI] [PubMed] [Google Scholar]
- 12. Palacín-Marín F, Esteban-Moreno B, Olea N, Herrera-Viedma E, Arroyo-Morales M. Agreement between telerehabilitation and face-to-face clinical outcome assessments for low back pain in primary care. Spine (Phila Pa 1976). 2013;38:947–952. [DOI] [PubMed] [Google Scholar]
- 13. Peterson S, Kuntz C, Roush J. Use of a modified treatment-based classification system for subgrouping patients with low back pain: agreement between telerehabilitation and face-to-face assessments. Physiother Theory Pract. 2019;35:1078–1086. [DOI] [PubMed] [Google Scholar]
- 14. Meyer BC, Lyden PD. The modified National Institutes of Health Stroke Scale: its time has come. Int J Stroke. 2009;4:267–273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Wilson AM, Ong MK, Saliba D, Jamal NI. The Veterans Affairs Neuropathy Scale: a reliable, remote polyneuropathy exam. Front Neurol. 2019;10:1050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Wilson AM, Jamal NI, Cheng FM, et al. Teleneurology clinics for polyneuropathy: a pilot study. J Neurol. 2020;267:479–490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Kurtzke JF. Rating neurologic impairment in multiple sclerosis. Neurology. 1983;33:1444–1452. [DOI] [PubMed] [Google Scholar]
- 18. Kane RL, Bever CT, Ehrmantraut M, Forte A, Culpepper WJ, Wallin MT. Teleneurology in patients with multiple sclerosis: EDSS ratings derived remotely and from hands-on examination. J Telemed Telecare. 2008;14(4):190–194. [DOI] [PubMed] [Google Scholar]
- 19. Cabana F, Boissy P, Tousignant M, Moffet H, Corriveau H, Dumais R. Interrater agreement between telerehabilitation and face-to-face clinical outcome measurements for total knee arthroplasty. Telemed J E Health. 2010;16:293–298. [DOI] [PubMed] [Google Scholar]
- 20. Russell TG, Blumke R, Richardson B, Truter P. Telerehabilitation mediated physiotherapy assessment of ankle disorders. Physiother Res Int. 2010;15:167–175. [DOI] [PubMed] [Google Scholar]