Abstract
Study Design:
Systematic review and meta-analysis.
Objectives:
We performed this meta-analysis to evaluate whether endoscopic discectomy (ED) shows superiority compared with the current gold standard of microdiscectomy (MD) in management of lumbar disc disease.
Materials and Methods:
We conducted independent and duplicate electronic database search including PubMed, Embase, and Cochrane Library from 1990 till April 2020 for studies comparing ED and MD in the management of lumbar disc disease. Analysis was performed in R platform using OpenMeta[Analyst] software.
Results:
We included 27 studies, including 11 randomized controlled trials (RCTs), 7 nonrandomized prospective, and 9 retrospective studies involving 4018 patients in the meta-analysis. We stratified the results based on the study design. Considering the heterogeneity in some results between study designs, we weighed our conclusion essentially based on results of RCTs. On analyzing the RCTs, superiority was established at 95% confidence interval for ED compared with MD in terms of functional outcomes like Oswestry Disability Index (ODI) score (P = .008), duration of surgery (P = .023), and length of hospital stay (P < .001) although significant heterogeneity was noted. Similarly, noninferiority to MD was established by ED in other outcomes like visual analogue scale score for back pain (P = .860) and leg pain (P = .495), MacNab classification (P = .097), recurrences (P = .993), reoperations (P = .740), and return-to-work period (P = .748).
Conclusion:
Our meta-analysis established the superiority of endoscopic discectomy in outcome measures like ODI score, duration of surgery, overall complications, length of hospital stay and noninferiority in other measures analyzed. With recent advances in the field of ED, the procedure has the potential to take over the place of MD as the gold standard of care in management of lumbar disc disease.
Keywords: endoscopic discectomy, microdiscectomy, lumbar disc disease, disc herniation, gold standard, PROM
Introduction
Lumbar disc herniation is a common cause of low back pain and radicular symptoms of patients presenting to any spine outpatient department. 1,2 Compression of nerve root by the herniated nucleus pulposus of the disc and associated inflammatory reaction are the 2 crucial factors that result in disabling lumbosacral radicular syndrome. 3 Although conservative trial relieves the pain in most of the cases, around 15% to 20% fail to improve necessitating surgical management. 4 Among the array of methods available microdiscectomy(MD) has been considered as the gold standard in surgical management of lumbar disc disease. 5
With the gaining popularity of the endoscopic approach in the management of lumbar disc disease, endoscopic discectomy (ED) has also become one of the common methods of surgical management. 6 Although ED had limited indications in the earlier days, with the advancement in the technology and tools used, the domains of its use have been extended. Moreover, with its advantages like surgery under local anesthesia, less damage to the bone and paraspinal musculature, and fast postoperative recovery ED is taking over the place of MD in the management of lumbar disc disease. 7,8 Despite many reviews and meta-analysis being available in literature comparing both the surgical procedures, they were limited by the number and the quality of evidence available, which prevented them to give a conclusive evidence on the superiority between the procedures. Hence, there is a need for a systematic review and meta-analysis with high-quality evidence currently available to establish the superiority of ED compared with the existing gold standard procedure MD in the management of lumbar disc disease.
We performed this meta-analysis to comprehensively analyze whether ED shows superiority compared with MD in the management of lumbar disc disease.
Materials and Methods
This meta-analysis was conducted following the guidelines of Back Review Group of Cochrane Collaboration 9 and reported based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement. 10
Search Strategy
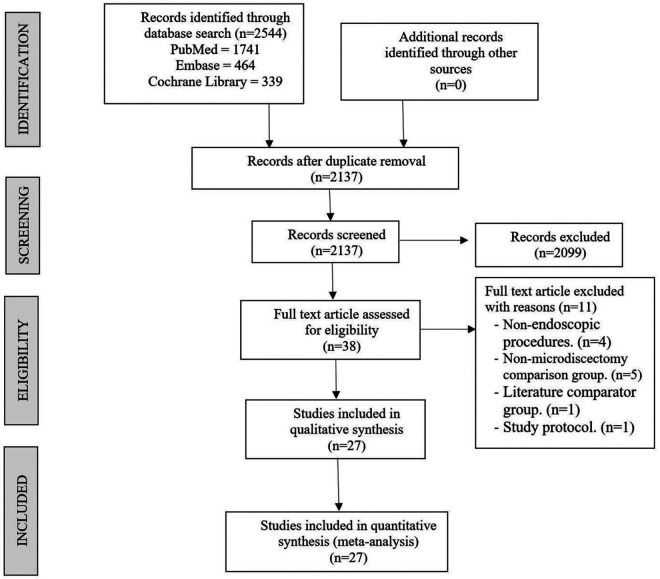
Two reviewers performed an independent electronic literature search for studies comparing ED and MD for surgical management of lumbar disc disease. We searched the following databases: PubMed, Embase, and the Cochrane Library up to April 2020. No language or date restrictions were applied. Keywords used for search were as follows: “lumbar disc herniation,” “microdiscectomy,” “endoscopic discectomy,” “minimally invasive discectomy,” “transforaminal discectomy,” “interlaminar discectomy,” along with Boolean operators “AND,” “OR,” and “NOT.” The reference lists of the selected articles were also searched to identify studies not identified in the primary search. As per the inclusion and exclusion criteria, eligible studies were included in the meta-analysis. Discrepancy between the authors was resolved through discussion until a consensus was obtained. A detailed study selection flow diagram is given in Figure 1.
Figure 1.
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow diagram of the included studies.
Inclusion Criteria
Studies were included if they met the following PICOS criteria. Population includes patients with lumbar disc disease while intervention is endoscopic discectomy and comparator group is microdiscectomy. Outcomes measured were visual analogue scale (VAS) score, Oswestry Disability Index (ODI), MacNab classification, overall complication rate, recurrence rate, reoperation rate, operation time, length of hospital stay, and return-to-work period. We included any study design satisfying the above PICO criteria, but we planned to stratify the results based on the study design to increase the robustness of the results arrived out of analysis.
Exclusion Criteria
Trials were excluded if they had the characteristics such as studies involving nonendoscopic procedures, studies using literature comparator group, studies involving animal models or anatomical studies.
Data Extraction
Two reviewers retrieved independently relevant data from articles included for analysis. Study characteristics such as study type, year of publication, authors, country, number of patients enrolled, and follow-up duration were extracted. Baseline characteristics such as mean age, gender proportions, preoperative pain and functional scores were also extracted. Primary outcome measures such as VAS score and ODI at final follow-up and MacNab classification along with secondary outcome measures such as overall complication rate, recurrence rate and reoperation rate and other outcome measures such as duration of surgery, length of hospital stay, and return-to-work period were the outcome data extracted.
In the case of studies with multiple comparator groups, only data of the MD and ED groups was taken for analysis. For missing data, we tried to contact the original author first. If it failed, we calculated the missed values from other available data using formulas in the Cochrane Handbook for Systematic Reviews of Interventions. Any disagreement in data collection was resolved until a consensus was attained by discussion.
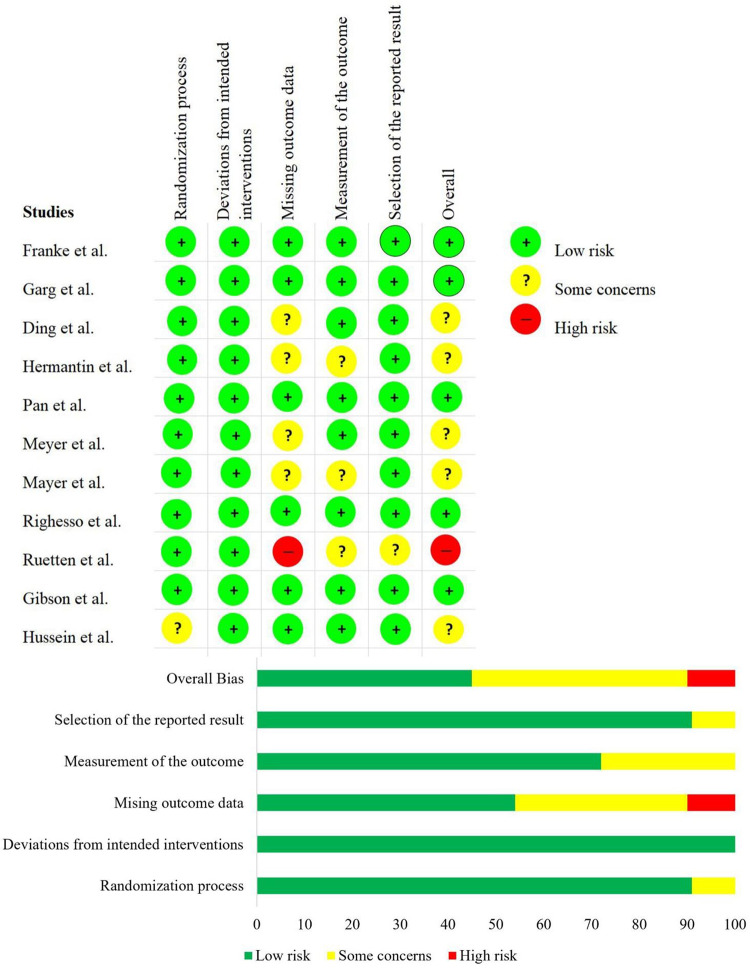
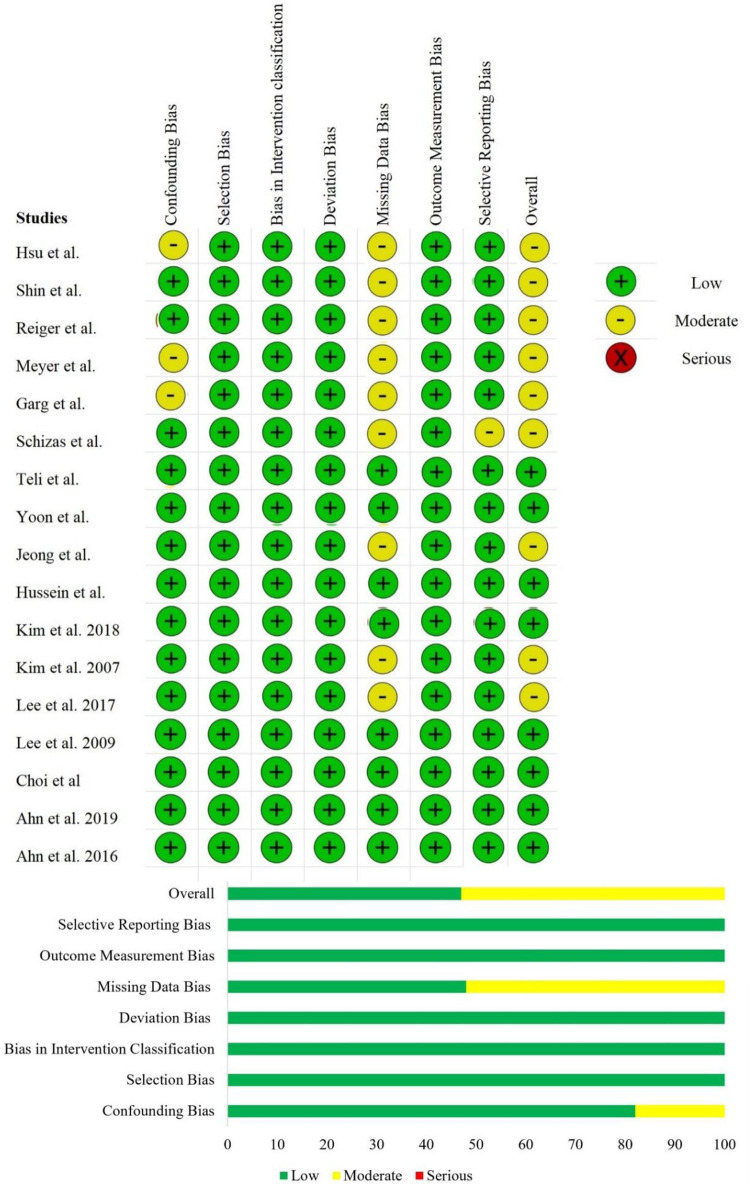
Risk of Bias and Quality Assessment
The methodological quality of the included studies was assessed independently by 2 reviewers using The Cochrane Collaboration’s RoB 2 tool for randomized controlled trials (RCTs) and ROBINS-I tool for nonrandomized studies, which has 5 and 7 domains of bias assessment, respectively. 11,12
Statistical Analysis
Meta-analysis was conducted in R platform with OpenMeta[Analyst]. 13 For dichotomous variable outcomes, odds ratio (OR) with 95% confidence interval (CI) was used and for continuous variable outcomes, weighted mean difference (WMD) with 95% CI was used. Superiority or noninferiority was established based on the overall estimate of the ED group for every outcome analyzed and its 95% CI distribution in the logarithmic scale compared with the MD group. Heterogeneity was assessed using I2 test. 14 If I2 < 50% and P > .1, we used a fixed-effects model to evaluate, otherwise, a random-effects model was used. Sensitivity analyses were performed to explore the source of heterogeneity when it existed. Publication bias was analyzed using funnel plot and Egger regression test.
Results
Search Results
Electronic database search resulted in 2544 articles which after initial screening for duplicate removal gave a total of 2137 articles. Title and abstract screening were done in those 2137 articles and 2099 of them were excluded. A total of 38 articles qualified for full-text review of which 11 were excluded. Finally, 27 studies, including 11 RCTs, 15 -25 7 nonrandomized prospective studies, 26 -32 and 9 retrospective studies 33 -41 with a total of 4018 patients were included in our analysis. List of studies excluded from full-text review is given in the Supplementary File 1. PRISMA flow diagram of study selection is given in Figure 1. The general characteristics of the studies included in our review are given in Table 1. We stratified the results of the meta-analysis by analyzing the results of included RCTs, nonrandomized prospective, and retrospective studies individually to know the effect of study design on the outcome measured in the included studies.
Table 1.
General Characteristics of the Included Studies.
| Study No. | Authors | Year | Country | Study design | Sample size, n | Gender (male), n | Mean age (years) | Follow-up period (years) | Lost to Follow-up, n | ||
|---|---|---|---|---|---|---|---|---|---|---|---|
| ED group | MD group | ED group | MD group | ||||||||
| 1 | Ding et al 15 | 2017 | China | Randomized controlled trial | 100 | 27 | 30 | 43.9 | 41.3 | 1 | 0 |
| 2 | Franke et al 16 | 2009 | Germany | Randomized controlled trial | 100 | NR | NR | NR | NR | 1 | NR |
| 3 | Garg et al 17 | 2011 | India | Randomized controlled trial | 112 | 44 | 36 | 38 | 37 | 1 | NR |
| 4 | Gibson et al 18 | 2016 | United Kingdom | Randomized controlled trial | 143 | 40 | 30 | 39 | 42 | 2 | 10 |
| 5 | Hermantin et al 19 | 1999 | United States | Randomized controlled trial | 60 | 17 | 22 | 40 | 39 | 2.6 | NR |
| 6 | Hussein et al 20 | 2016 | Egypt | Randomized controlled trial | 80 | 21 | 20 | 31.9 | 30.5 | 2.1 | 7 |
| 7 | Mayer et al 21 | 1993 | Germany | Randomized controlled trial | 40 | 14 | 12 | 42.7 | 39.8 | NR | NR |
| 8 | Meyer et al 22 | 2020 | Brazil | Randomized controlled trial | 47 | 16 | 14 | 45.2 | 47.2 | 1 | NR |
| 9 | Pan et al 23 | 2016 | China | Randomized controlled trial | 106 | 31 | 26 | 42.8 | 39.5 | 1.3 | NR |
| 10 | Righesso et al 24 | 2007 | Brazil | Randomized controlled trial | 40 | 13 | 10 | 46 | 42 | 3.1 | NR |
| 11 | Ruetten et al 25 | 2008 | Germany | Randomized controlled trial | 200 | NR | NR | NR | NR | 2 | 22 |
| 12 | Akcakaya et al 26 | 2016 | Turkey | Prospective study | 30 | NR | NR | NR | NR | NR | NR |
| 13 | Hsu et al 27 | 2012 | Taiwan | Prospective study | 123 | 45 | 38 | 50.4 | 44.2 | 2 | 22 |
| 14 | Kim et al 28 | 2018 | Korea | Prospective study | 146 | 24 | 37 | 54.2 | 46.6 | 1.2 | 5 |
| 15 | Rieger et al 29 | 2019 | Germany | Prospective study | 740 | 119 | 101 | 78 | 76 | 2.7 | 190 |
| 16 | Schizas et al 30 | 2005 | Switzerland | Prospective study | 28 | 6 | 9 | 41.5 | 43 | 1 | NR |
| 17 | Shin et al 31 | 2008 | Korea | Prospective study | 30 | 5 | 7 | 48.1 | 42.7 | NR | NR |
| 18 | Yoon et al 32 | 2012 | Korea | Prospective study | 72 | 13 | 16 | 56.4 | 45.8 | 1.6 | 23 |
| 19 | Ahn et al 33 | 2015 | Korea | Retrospective cohort study | 178 | 32 | 34 | 22.1 | 22.4 | 1.2 | NR |
| 20 | Ahn et al 34 | 2019 | Korea | Retrospective cohort study | 298 | 94 | 85 | 40.4 | 38.7 | 5 | 0 |
| 21 | Choi et al 35 | 2016 | Korea | Retrospective cohort study | 44 | 14 | 13 | 38 | 33.9 | 0.5 | 1 |
| 22 | Jeong et al 36 | 2006 | Korea | Retrospective cohort study | 47 | 16 | 14 | 56 | 56.4 | 1 | NR |
| 23 | Kim et al 37 | 2007 | Korea | Retrospective cohort study | 915 | 392 | 188 | 44.4 | 34.9 | 2.2 | 13 |
| 24 | Lee et al 38 | 2017 | Korea | Retrospective cohort study | 83 | 30 | 25 | 50.1 | 50.2 | 2.3 | NR |
| 25 | Lee et al 39 | 2009 | Korea | Retrospective cohort study | 54 | 22 | 16 | 47.7 | 42 | 2.8 | NR |
| 26 | Lee et al 40 | 2006 | Korea | Retrospective cohort study | 60 | 22 | 22 | 39.6 | 39.3 | 3.1 | NR |
| 27 | Teli et al 41 | 2010 | Italy | Retrospective cohort study | 142 | 48 | 45 | 40 | 39 | 2 | NR |
Abbreviations: ED, endoscopic discectomy; MD, microdiscectomy; NR, not reported.
Quality Assessment
The methodological quality of the included randomized and nonrandomized studies are given in Figures 2 and 3, respectively.
Figure 2.
Risk of bias evaluation of the randomized controlled trials using the RoB 2 tool.
Figure 3.
Risk of bias evaluation of the nonrandomized studies using the ROBINS-I tool.
Primary Outcomes
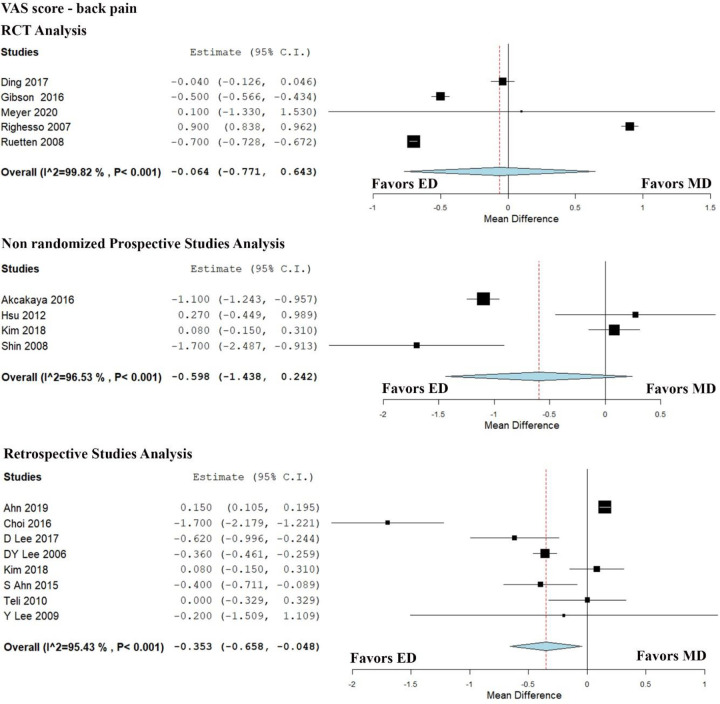
VAS Score: Back Pain at Final Follow-up
We analyzed 16 studies involving 1718 patients that reported VAS score for back pain at the final follow-up. The average VAS score for leg pain of the ED and MD groups was 1.82 and 2.18, respectively. ED group and MD group showed a reduction of 3.47 and 3.02 in the VAS scale, respectively, compared with the preoperative values. Significant heterogeneity existed between the studies (I2 = 99.47%, P < .001). Hence, a random-effects model was used. On analyzing the results of 5 RCTs, we did not find any significant reduction in the VAS score for back pain in the ED group compared with the MD group (WMD = −0.064, 95% CI [−0.771, 0.643], P = .860) as shown in Figure 4. Similar results were noted on analyzing the results of nonrandomized prospective studies (WMD = −0.598, 95% CI [−1.438, 0.242], P = .163), whereas retrospective studies showed a significant reduction in the VAS score for back pain in the ED group compared to MD group (WMD = −0.353, 95% CI [−0.658, −0.048], P = .023) with significant heterogeneity (I2 = 95.426%, P < .001) as shown in Figure 4.
Figure 4.
Forest plot of randomized controlled trials (RCTs) and nonrandomized prospective and retrospective studies comparing visual analogue scale (VAS) score for back pain between the endoscopic discectomy (ED) group and the microdiscectomy (MD) group.
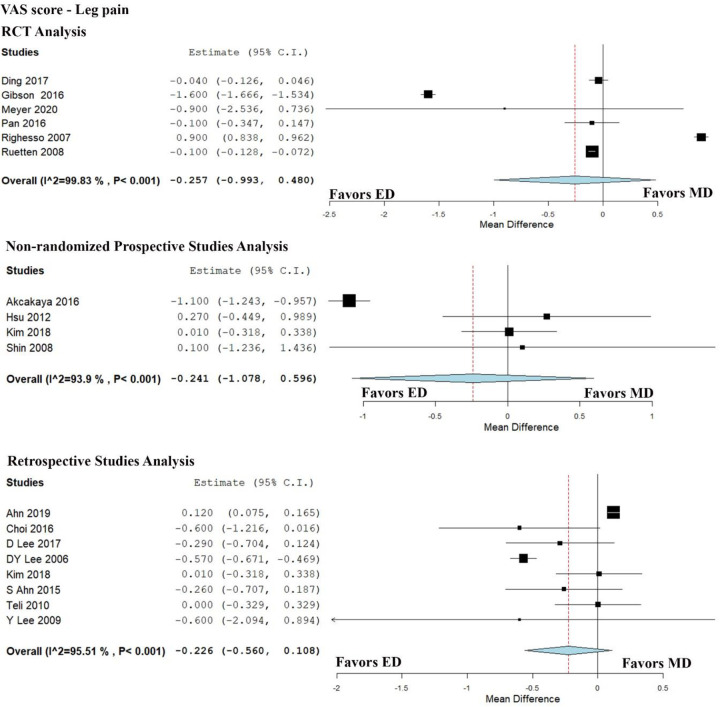
VAS Score: Leg Pain at Final Follow-up
We analyzed 17 studies involving 1824 patients that reported VAS score for leg pain at the final follow-up. ED group and MD group showed a reduction of 5.6 and 5.7 in the VAS scale, respectively compared with the preoperative values. The average VAS scores for leg pain at final follow-up for the ED and MD groups were 1.67 and 1.95, respectively. Significant heterogeneity existed between the studies (I2 = 99.52%, P < .001). Hence, a random-effects model was used. On analyzing the results of 6 RCTs, we did not find any significant reduction in the VAS score for leg pain in the ED group compared with the MD group (WMD = −0.064, 95% CI [−0.771, 0.643], P = .860) as shown in Figure 5. Similarly, on analyzing the results of nonrandomized prospective and retrospective studies also we did not find any significant reduction in the VAS score for leg pain in the ED group compared with the MD group (WMD = −0.241, 95% CI [−1.078, 0.596], P = .573) and (WMD = −0.226, 95% CI [−0.560, 0.108], P = .184), respectively, as shown in Figure 5.
Figure 5.
Forest plot of randomized controlled trials (RCTs) and nonrandomized prospective and retrospective studies comparing visual analogue scale (VAS) score for leg pain between the endoscopic discectomy (ED) group and the microdiscectomy (MD) group.
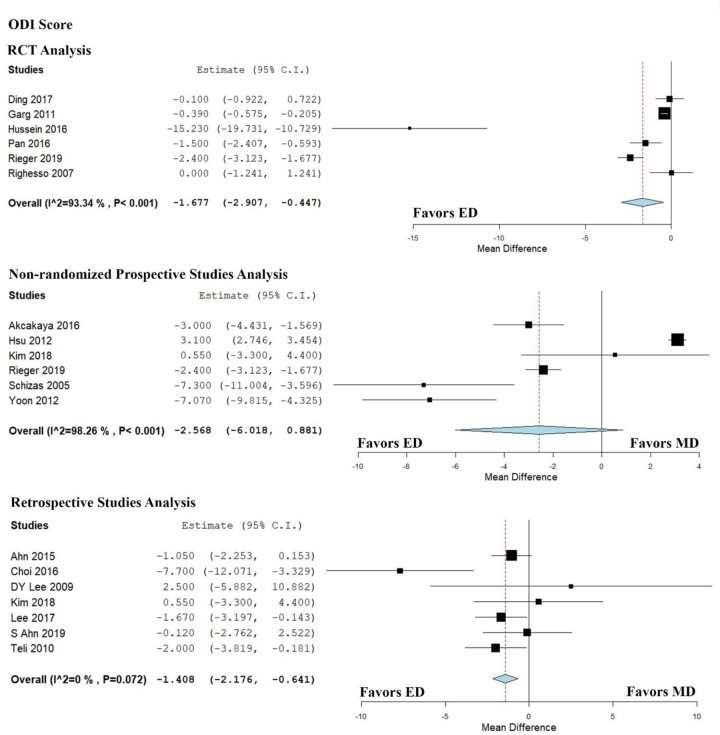
ODI Score at Final Follow-up
We analyzed 17 studies involving 2566 patients that reported ODI scores at the final follow-up. The average ODI score of the ED and MD groups was 12.17% and 14.72%, respectively. Significant heterogeneity existed between the studies (I2 = 96.73%, P < .001). Hence, a random-effects model was used. On analyzing the results of 6 RCTs, we found a significant reduction in the ED group compared with the MD group (WMD = −1.677, 95% CI [−2.907, −0.447], P = .008) as shown in Figure 6. Similar results were noted on analyzing the results of retrospective studies (WMD = −1.408, 95% CI [−2.176, −0.641], P < .001), whereas nonrandomized prospective studies did not show a significant reduction in the ODI score postoperatively in the ED group compared with the MD group (WMD = −2.568, 95% CI [−6.018, 0.881], P = .144) as shown in Figure 6.
Figure 6.
Forest plot of randomized controlled trials (RCTs) and nonrandomized prospective and retrospective studies comparing Oswestry Disability Index (ODI) scores between the endoscopic discectomy (ED) group and the microdiscectomy (MD) group.
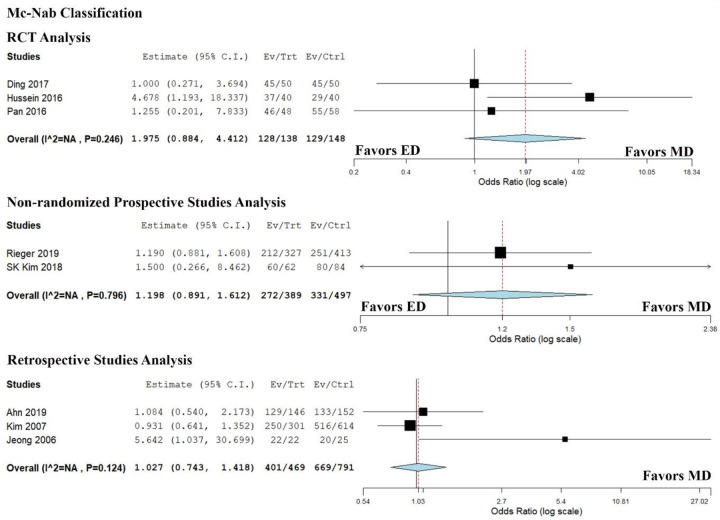
MacNab Classification at Final Follow-up
We analyzed 8 studies involving 2432 patients that categorized their outcomes based on MacNab classification. To make the ordinal data into dichotomous data for meta-analysis, excellent or good were defined as clinical success, while fair and poor categories were defined unsuccessful. All the included studies had minimum follow-up period of 1 year (range: 1-5 years). A total of 80.4% (801 of 996) patients in the ED group and 78.6% (1129 of 1436) patients in the MD group were successful. There was no significant heterogeneity between individual studies included in the analysis (I2 = 11.86%, P = .338). On analyzing the results of 3 RCTs, we did not find a significant difference between the groups (OR = 1.975, 95% CI [0.884, 4.412], P = .097) as shown in Figure 7. Similar results were noted between the groups in nonrandomized prospective (OR = 1.198, 95% CI [0.891, 1.612], P = .232) and retrospective studies (OR = 1.027,95% CI [0.743, 1.418], P = .873) as shown in Figure 7.
Figure 7.
Forest plot of randomized controlled trials (RCTs) and nonrandomized prospective and retrospective studies comparing McNab classification between the endoscopic discectomy (ED) group and the microdiscectomy (MD) group.
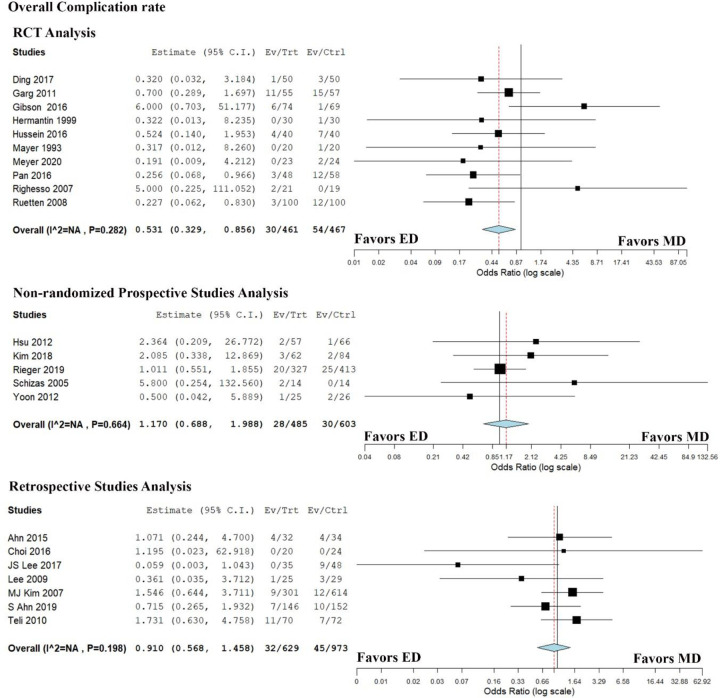
Secondary Outcomes
Overall Complication Rate
We analyzed 22 studies involving 3618 patients that reported their complications. Complications were noted in 5.7% (90 of 1575) patients in the ED group and 6.3% (129 of 2043) patients in the MD group. There was no significant heterogeneity between individual studies included in the analysis (I2 = 18.8%, P = .211). On analyzing the results of 10 RCTs, we found the ED group to have a significantly lesser overall complications compared with the MD group (OR = 0.531, 95% CI [0.329, 0.856], P = .009) as shown in Figure 8. While analyzing the results of nonrandomized prospective studies and retrospective studies we did not find significant difference between the groups (OR = 1.170, 95% CI [0.688, 1.988], P = .563) and (OR = 0.910, 95% CI [0.568, 1.458], P = .696), respectively, as shown in Figure 8.
Figure 8.
Forest plot randomized controlled trials (RCTs), nonrandomized prospective and retrospective studies comparing overall complication rate between the endoscopic ED group and the microdiscectomy (MD) group.
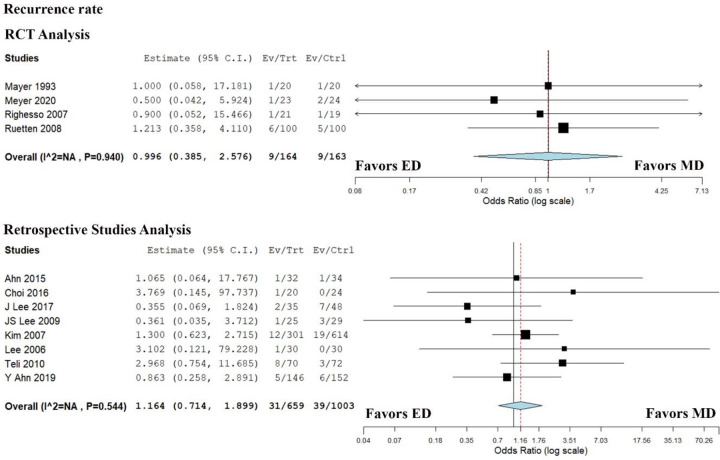
Recurrence Rate
We analyzed 18 studies involving 2575 patients that reported their recurrence of symptoms. Recurrences were noted in 4.8% (54 of 1119) patients in the ED group and 3.9% (58 of 1456) patients in the MD group. There was no significant heterogeneity noted among the studies included in the analysis (I2 = 0%, P = .952). On analyzing the results of 4 RCTs we did not find any difference between the groups (OR = 0.996, 95% CI [0.385, 2.576], P = .993) as shown in Figure 9. Similar results were noted on analysis of retrospective studies (OR = 1.1641, 95% CI [0.714, 1.899], P = .542) as shown in Figure 9.
Figure 9.
Forest plot of randomized controlled trials (RCTs) and retrospective studies comparing recurrence rates between the endoscopic discectomy (ED) group and the microdiscectomy (MD) group.
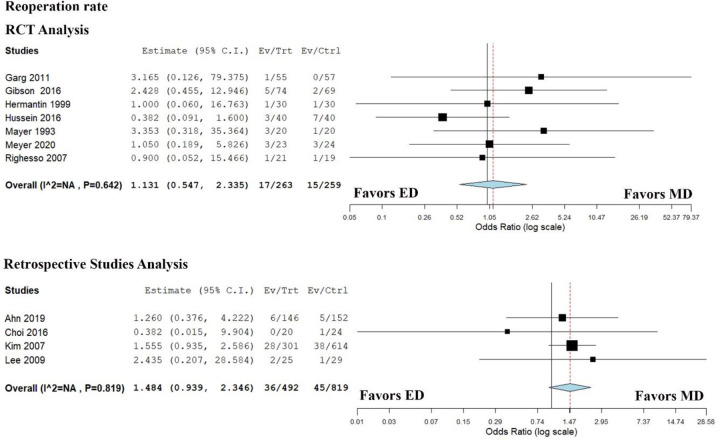
Reoperation Rate
We analyzed 13 studies involving 2056 patients that reported their total reoperations in both groups. A total of 7.8% (68 of 864) patients in the ED group and 5.8% (70 of 1192) patients in the MD group required reoperation. There was no significant heterogeneity noted among the studies included in the analysis (I2 = 0%, P = .902). On analyzing the results of 7 RCTs, we did not find any difference between the groups (OR = 1.131, 95% CI [0.547, 2.335], P = .740) as shown in Figure 10. Similar results were noted in retrospective studies concerning reoperation rates (OR = 1.484, 95% CI [0.939, 2.346], P = .091) as shown in Figure 10.
Figure 10.
Forest plot of randomized controlled trials (RCTs) and retrospective studies comparing reoperation rates between the endoscopic discectomy (ED) group and the microdiscectomy (MD) group.
Other Outcomes
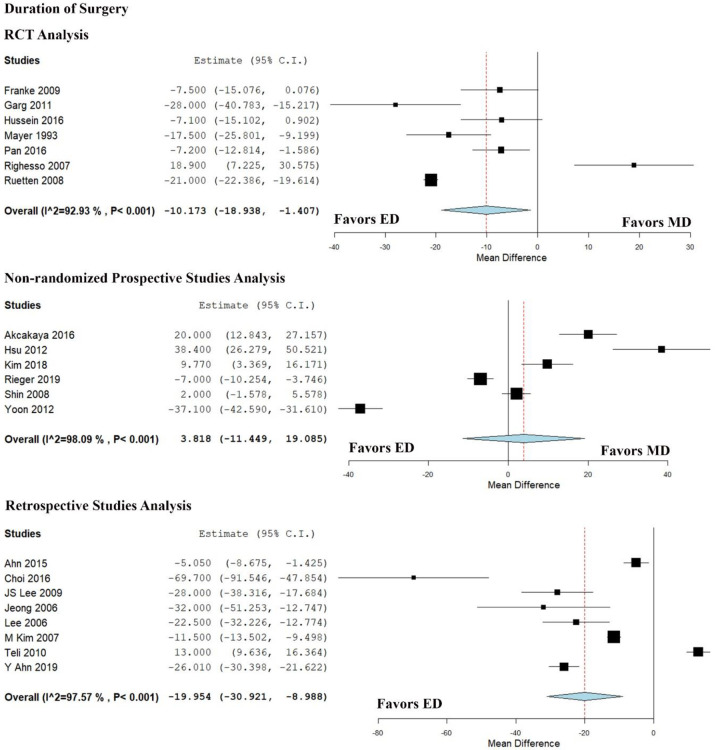
Duration of Surgery
We analyzed 22 studies involving 23 524 patients that reported the duration of surgery in both the groups. The average duration of surgery for ED and MD was 63.37 and 73.19 minutes, respectively. Significant heterogeneity existed between the studies (I2 = 97.55%, P < .001). Hence, a random-effects model was used. On analyzing the results of 7 RCTs, we found a significant reduction in operative time in the ED group compared with the MD group (WMD = −10.173, 95% CI [−18.938, −1.407], P = .023) as shown in Figure 11. Similar results were given by retrospective studies (WMD = −19.954, 95% CI [−30.921, −8.988], P < .001), whereas nonrandomized prospective studies did not show any significant difference between the groups (WMD = 3.818, 95% CI [−11.449, 19.085], P = .624) as shown in Figure 11.
Figure 11.
Forest plot of randomized controlled trials (RCTs) and nonrandomized prospective and retrospective studies comparing duration of surgery between the endscopic discectomy (ED) group and the microdiscectomy (MD) group.
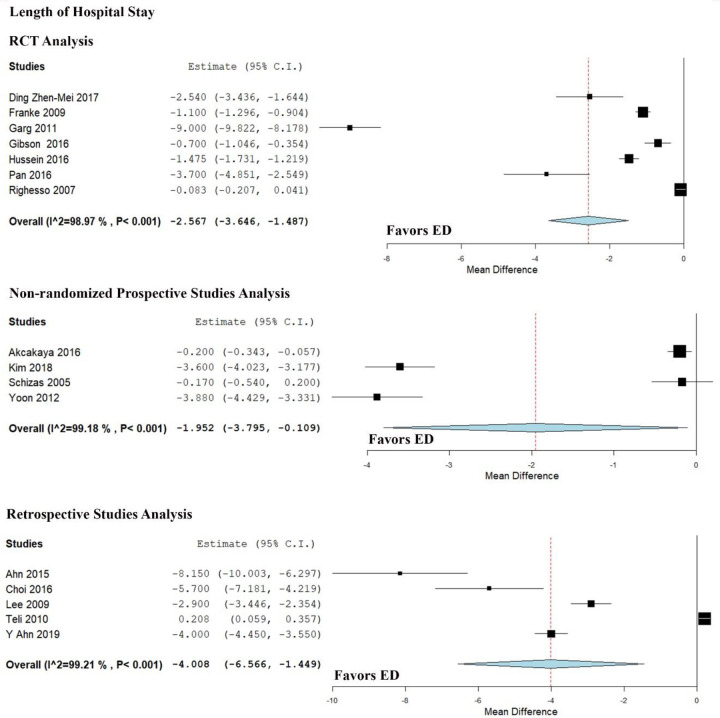
Length of Hospital Stay
We analyzed 17 studies involving 1600 patients that reported the length of hospital stay in both the groups. The average length of hospital stay for ED and MD was 2.84 and 5.74 days, respectively. Significant heterogeneity existed between the studies (I2 = 98.9%, P < .001). Hence, a random-effects model was used. On analyzing the results of 7 RCTs, we found a significant reduction in the length of hospital stay in the ED group compared with the MD group (WMD = −2.567, 95% CI [−3.646, −1.487], P < .001) as shown in Figure 12. Similar results were given by nonrandomized prospective studies (WMD = −1.952, 95% CI [−3.795, −0.109], P = .038) and retrospective studies (WMD = −4.008, 95% CI [−6.566, −1.449], P = .002) as shown in Figure 12.
Figure 12.
Forest plot of randomized controlled trials (RCTs) and nonrandomized prospective and retrospective studies comparing length of hospital stay between the endoscopic discectomy (ED) group and the microdiscectomy (MD) group.
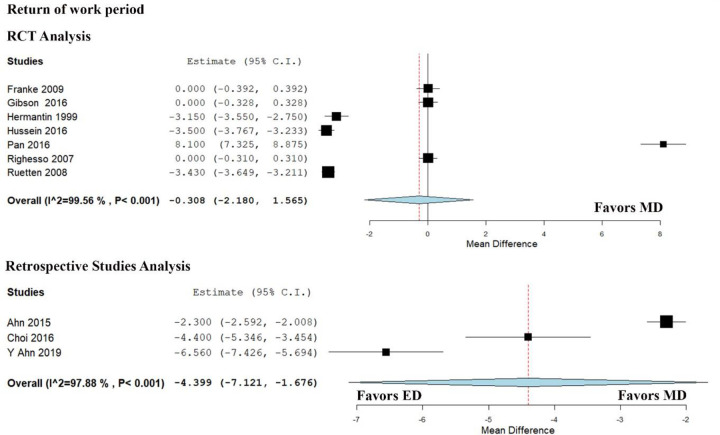
Return-to-Work Period
We analyzed 11 studies involving 1188 patients that compared the duration for return to work after surgery between the groups. The average duration for return to work in ED and MD was 4.75 and 6.19 weeks, respectively. Significant heterogeneity existed between the studies (I2 = 99.34%, P < .001). Hence, a random-effects model was used. On analyzing the results of RCTs also we did not find a significant difference between the groups (WMD = −0.308, 95% CI [−2.180, 1.565], P = .748) as shown in Figure 13. Whereas on analysis of retrospective studies, we found a significant reduction in return-to-work duration in the ED group compared with the MD group (WMD = −4.399, 95% CI [−7.121, −1.676], P = .002) as shown in Figure 13.
Figure 13.
Forest plot of randomized controlled trials (RCTs) and retrospective studies comparing return-to-work period between the endoscopic discectomy (ED) group and the microdiscectomy (MD) group.
Sensitivity Analysis
A sensitivity analysis was performed in each analysis. All the results (VAS score, ODI score, MacNab classification, complications, recurrences, reoperations, duration of surgery, length of hospital stay) were not significantly altered by sequentially omitting each study in the meta-analysis within each study design. On the other hand, consistency of the results was maintained after reanalysis by changing to the random-effects model.
Publication Bias Analysis
Publication bias was analyzed using funnel plot and Egger regression test for the meta-analysis on complication rate between the ED and MD groups. There was no evidence of publication bias by the Egger regression test (P = .528) and funnel plot as shown in Figure 14. All the studies lay within the 95% CI and were distributed evenly about the axes, implying minimal publication bias.
Figure 14.

Funnel plot for complication rate in included studies.
Discussion
Main Findings
We comprehensively and systematically reviewed all the available literature comparing endoscopic discectomy with microdiscectomy for lumbar disc disease and stratified the results based on the study designs. Considering the discrepancy in the meta-results in some of the outcomes analyzed between study designs, we derived our conclusions essentially based on the meta-results of the RCTs. We found that superiority was established at 95% CI for ED compared with MD in terms of functional outcomes like ODI score (P = .008), duration of surgery (P = .023), overall complication rate (P < .009), and length of hospital stay (P < .001) from analyzing RCTs as shown in Figures 6, 11, 8, and 12, respectively. Although, significant heterogeneity was noted among the included studies. Moreover, noninferiority to MD was established by ED in other outcomes like VAS score for back pain (P = .860), VAS score for leg pain (P = .495), MacNab classification (P = .097), recurrences (P = 0.993), reoperations (P = .740), and return-to-work period (P = .748) considering the RCT results exclusively as shown in figures 4, 5, 7, 9, 10, and 13, respectively.
Comparison With Other Meta-Analyses
Qin et al 42 did a meta-analysis including 9 studies (2 RCTs, 1 prospective study, and 6 retrospective studies) with 1585 patients comparing ED and MD procedure for lumbar disc disease. Although the analysis was underpowered with limited studies, a statistically significant difference was noted for ED compared with MD regarding hospital stay and return-to-work period. They concluded that ED could be an alternative to MD considering the more minimally invasive nature of the procedure. The major limitation of the analysis was limited high-quality evidence to establish the robustness of their results.
Kim et al 43 did a meta-analysis on the Korean population from 7 retrospective studies comparing ED and MD. Although they found significant differences favoring ED from their meta-analysis on VAS score, ODI score, duration of surgery and hospital stay, they could not establish the superiority of the procedure considering the study designs taken under analysis and suggested for a large RCT to verify their findings. Our meta-analysis involving 11 RCTs has demonstrated that ED was superior to MD on various outcome measures taken for analysis. Zhang et al 44 in their meta-analysis of 9 studies involving 1527 patients found ED superior to MD only in the length of hospital stay. The major limitation of their study is the limited number of studies available for analysis of different outcomes. Barber et al 45 in their meta-analysis comparing the outcomes of ED with MD from 26 studies noted similar findings as that of our study but they failed to analyze the duration of surgery and their functional outcomes based on MacNab classification. Moreover, our analysis included 3 more studies 22,29,34 published after their analysis, which added to the number and quality of the evidence synthesized from our study with 1085 additional patients.
Chen et al 46 did a network meta-analysis on the complication rates of different discectomy techniques for the management of lumbar disc herniation. In their analysis, they found that both MD and ED were the safest of other procedures for lumbar discectomy like tubular discectomy or percutaneous laser disc decompression. Our study compared the 2 safest procedures and established the superiority of ED in various outcome measures. Our results were further strengthened by the network meta-analysis by Feng et al 47 comparing 7 different surgical interventions for lumbar disc herniation. They concluded ED to be the procedure of choice to increase the success rate and decrease the complication rate.
Our analysis of 27 studies including 11 RCTs, 7 nonrandomized prospective studies, and 9 retrospective studies involving 4018 patients is the largest of all meta-analyses done so far on the subject to establish the superiority of the endoscopic discectomy as an upgrade to the current gold standard microdiscectomy procedure. We had 8 to 22 studies being involved for every outcome analyzed making the results more robust.
Functional Outcome
Parker et al, 48 in their study on long-term functional outcomes of the surgical procedures for lumbar disc disease, reported that 32% of the patients suffered above moderate back pain after microdiscectomy procedure. Both MD and ED were considered minimally invasive compared with traditional open lumbar discectomy. However, Akcakaya et al 26 in their study analyzed the muscle injury between ED and MD for lumbar disc disease and found a significant rise in the serum creatinine phosphokinase levels at 6, 12, and 24 hours postoperatively in MD compared with ED (P < .004). This substantiates the superiority of ED over MD in being the least invasive of all the procedures with significantly less ODI score as seen in our analysis. ED was usually performed under local anesthesia enabling the surgeon to confirm adequate decompression before the patient leaves the operating room. 7,8 This ensures shorter hospital stay and early return to work as established in our analysis. Cochrane review by Rasouli et al 49 compared the efficacy of minimally invasive discectomy procedures including endoscopic discectomy and open/microdiscectomy. They found minimally invasive discectomy procedures to have a lower risk of complications and lesser hospital stay as seen in our analysis.
Complications
Since the gold standard MD procedure involves partial resection of ligamentum flavum and lamina with retraction of dura and root, chances of complications like a dural tear, dysesthesia and infection were found to be higher in MD compared with ED. 46 Besides, the problems due to epidural scar and hematoma need to be solved along with postoperative lumbar instability. 47 On the other hand, with the advances in endoscopic devices with greater maneuverability, the incidence of such complications are limited in ED. This was reinforced by Chen et al 46 and Feng et al 47 based on the results of their network meta-analysis on complications of different discectomy techniques for lumbar disc herniation. Both the network meta-analyses considered ED as the safest of all discectomy procedures with maximum success rate. Our meta-analysis established the noninferiority of ED compared with MD in terms of overall complications or recurrences or reoperation rates.
Approach Selection
Apart from concentrating on the method of discectomy, the underlying pathology of disc degeneration and the patient’s clinical symptoms should guide us toward the approach selection process. 6 Although there are 2 different approaches in ED, the choice of approach either interlaminar or transforaminal route is based on the localization of the pathology to be addressed. 25 Paracentral and lateral recess disc herniation can be addressed in interlaminar approach whereas foraminal and far lateral herniations can be better addressed via transforaminal route. 8,25
However, in earlier days, considering the limitations of each procedure based on the clinical scenario, the treatment plan was devised to help us efficiently achieve the surgical goals. But nowadays, procedure-based barrier walls have become more porous due to the advancement in imaging technology and minimally invasive surgical tools. Endoscopic procedures can perform on par with open procedures, including interbody fusion, apart from discectomy and decompression, without any significant damage to paravertebral muscles and ligaments. 20,23 Moreover, the ability to perform under local anesthesia with minimal sedation as a day care procedure helps us to achieve faster recovery with preserved stability. This makes the procedure to establish an upgrade in the current standard of care in the management of lumbar disc disease.
Limitations
The only limitation of the current meta-analysis was the significant heterogeneity that existed among the outcomes measures between the studies included. In order to address the role of study designs as a source of heterogeneity, we stratified the individual results based on the study design to look into the discrepancy between their individual meta-results. It was noted that, in parameters like VAS for leg pain, McNab classification, recurrence rate, reoperation rate and length of hospital stay similar conclusion was achieved irrespective of the study designs. Retrospective studies differed from the meta-results of RCTs and nonrandomized prospective studies in outcomes like VAS for back pain, ODI score, and return-to-work period. It was mainly due to the clinical heterogeneity of the included population such as type of surgery (primary/revision), surgical indications, treatment prior to surgery and varied duration of follow-up which resulted in inconsistency. Whereas nonrandomized prospective studies also differed from the meta-results of RCTs in outcomes like overall complication rate and duration of surgery. Another possible reason for the heterogeneity could be the variability of the surgical expertise of the authors which significantly alters the outcomes in endoscopic procedures. 27 Hence, we weighed our conclusion essentially based on the meta-results of the RCTs to uphold its quality.
Conclusion
Our meta-analysis established the superiority of endoscopic discectomy in outcome measures like ODI score, duration of surgery, overall complications, length of hospital stay and non-inferiority in other measures analyzed. With recent advances in the field of ED, the procedure has the potential to take over the place of MD as the gold standard of care in the management of lumbar disc disease.
Supplemental Material
Supplemental Material, Supp_File_1 for Is Endoscopic Discectomy the Next Gold Standard in the Management of Lumbar Disc Disease? Systematic Review and Superiority Analysis by Sathish Muthu, Eswar Ramakrishnan and Girinivasan Chellamuthu in Global Spine Journal
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Sathish Muthu, MS(Ortho)  https://orcid.org/0000-0002-7143-4354
https://orcid.org/0000-0002-7143-4354
Supplemental Material: Supplemental material for this article is available online.
References
- 1. Da VDW, Simons E, Riphagen II, et al. Physical examination for lumbar radiculopathy due to disc herniation in patients with low-back pain. Cochrane Database Syst Rev. 2010;(2):CD007431. [DOI] [PubMed] [Google Scholar]
- 2. Amin RM, Andrade NS, Neuman BJ. Lumbar disc herniation. Curr Rev Musculoskelet Med. 2017;10:507-516. doi:10.1007/s12178-017-9441-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kobayashi S, Takeno K, Yayama T, et al. Pathomechanisms of sciatica in lumbar disc herniation effect of periradicular adhesive tissue on electrophysiological values by an intraoperative straight leg raising test. Spine (Phila Pa 1976). 2010;35:2004–2014. doi:10.1097/BRS.0b013e3181d4164d [DOI] [PubMed] [Google Scholar]
- 4. Lee YC, Zotti MG, Osti OL. Operative management of lumbar degenerative disc disease. Asian Spine J. 2016;10:801-819. doi:10.4184/asj.2016.10.4.801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Koebbe CJ, Maroon JC, Abla A, El-Kadi H, Bost J. Lumbar microdiscectomy: a historical perspective and current technical considerations. Neurosurg Focus. 2002;13:E3. [DOI] [PubMed] [Google Scholar]
- 6. Ruetten S, Komp M, Merk H, Godolias G. Use of newly developed instruments and endoscopes: full-endoscopic resection of lumbar disc herniations via the interlaminar and lateral transforaminal approach. J Neurosurg Spine. 2007;6:521–530. [DOI] [PubMed] [Google Scholar]
- 7. Gibson JNA, Cowie JG, Iprenburg M. Transforaminal endoscopic spinal surgery: the future “gold standard” for discectomy? A review. Surgeon. 2012;10:290–296. [DOI] [PubMed] [Google Scholar]
- 8. Jhala A, Mistry M. Endoscopic lumbar discectomy: experience of first 100 cases. Indian J Orthop. 2010;44:184-190. doi:10.4103/0019-5413.62051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. van Tulder M, Furlan A, Bombardier C, Bouter L; Editorial Board of the Cochrane Collaboration Back Review Group. Updated method guidelines for systematic reviews in the Cochrane Collaboration Back Review Group. Spine (Phila Pa 1976). 2003;28:1290–1299. [DOI] [PubMed] [Google Scholar]
- 10. Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and metaanalyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Sterne JAC, Savović J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. [DOI] [PubMed] [Google Scholar]
- 12. Sterne JAC, Hernán MA, Reeves BC, et al. ROBINS-I: a tool for assessing risk of bias in non-randomized studies of interventions. BMJ. 2016;355:i4919. doi:10.1136/bmj.i4919 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Wallace BC, Dahabreh IJ, Trikalinos TA, Lau J, Trow P, Schmid CH. Closing the gap between methodologists and end-users: R as a computational back-end. J Stat Soft. 2012;49:5. [Google Scholar]
- 14. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Ding Z-M, Tao Y-Q. Clinical outcomes of percutaneous transforaminal endoscopic discectomy versus fenestration discectomy in patients with lumbar disc herniation. J Int Transl Med. 2017;5:29–33. [Google Scholar]
- 16. Franke J, Greiner-Perth R, Boehm H, et al. Comparison of a minimally invasive procedure versus standard microscopic discotomy: a prospective randomised controlled clinical trial. Eur Spine J. 2009;18:992-1000. doi:10.1007/s00586-009-0964-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Garg B, Nagraja UB, Jayaswal A. Microendoscopic versus Open Discectomy for Lumbar Disc Herniation: A Prospective Randomised Study. J Orthop Surg (Hong Kong). 2011;19:30–34. doi/10.1177/230949901101900107 [DOI] [PubMed] [Google Scholar]
- 18. Gibson JNA, Subramanian AS, Scott CEH. A randomised controlled trial of transforaminal endoscopic discectomy vs microdiscectomy. Eur Spine J. 2017;26:847–856. [DOI] [PubMed] [Google Scholar]
- 19. Hermantin FU, Peters T, Quartararo LG, Kambin P. A prospective, randomized study comparing the results of open discectomy with those of video-assisted arthroscopic microdiscectomy. J Bone Joint Surg Am. 1999;81:958–965. [DOI] [PubMed] [Google Scholar]
- 20. Hussein M. Minimal incision, multifidus-sparing microendoscopic diskectomy versus conventional microdiskectomy for highly migrated intracanal lumbar disk herniations. J Am Acad Orthop Surg. 2016;24:805–813. [DOI] [PubMed] [Google Scholar]
- 21. Mayer HM, Brock M. Percutaneous endoscopic discectomy: surgical technique and preliminary results compared to microsurgical discectomy. J Neurosurg. 1993;78:216–225. [DOI] [PubMed] [Google Scholar]
- 22. Meyer G, DA Rocha ID, Cristante AF, et al. Percutaneous endoscopic lumbar discectomy versus microdiscectomy for the treatment of lumbar disc herniation: pain, disability, and complication rate-a randomized clinical trial. Int J Spine Surg. 2020;14:72-78. doi:10.14444/7010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Pan Z, Ha Y, Yi S, Cao K. Efficacy of transforaminal endoscopic spine system (TESSYS) technique in treating lumbar disc herniation. Med Sci Monit. 2016;22:530-539. doi:10.12659/msm.894870 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Righesso O, Falavigna A, Avanzi O. Comparison of open discectomy with microendoscopic discectomy in lumbar disc herniations: results of a randomized controlled trial. Neurosurgery. 2007;61:545–549. [DOI] [PubMed] [Google Scholar]
- 25. Ruetten S, Komp M, Merk H, Godolias G. Full-endoscopic interlaminar and transforaminal lumbar discectomy versus conventional microsurgical technique: a prospective, randomized, controlled study. Spine (Phila Pa 1976). 2008;33:931–939. [DOI] [PubMed] [Google Scholar]
- 26. Akçakaya MO, Yörükoğlu AG, Aydoseli A, Aras Y, Sabancı PA, Altunrende ME, et al. Serum creatine phosphokinase levels as an indicator of muscle injury following lumbar disc surgery: comparison of fully endoscopic discectomy and microdiscectomy. Clin Neurol Neurosurg. 2016;145:74–78. [DOI] [PubMed] [Google Scholar]
- 27. Hsu HT, Chang SJ, Yang SS, Chai CL. Learning curve of full-endoscopic lumbar discectomy. Eur Spine J. 2013;22:727-733. doi:10.1007/s00586-012-2540-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Kim SK, Kang SS, Hong YH, Park SW, Lee SC. Clinical comparison of unilateral biportal endoscopic technique versus open microdiscectomy for single-level lumbar discectomy: a multicenter, retrospective analysis. J Orthop Surg Res. 2018;13:22. doi:10.1186/s13018-018-0725-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Rieger B, Sitoci-Ficici KH, Reinshagen C, et al. Endoscopic and microscopic segmental decompression via translaminar crossover spinal approach in elderly patients. World Neurosurg. 2019;125:e361–e371. [DOI] [PubMed] [Google Scholar]
- 30. Schizas C, Tsiridis E, Saksena J. Microendoscopic discectomy compared with standard microsurgical discectomy for treatment of uncontained or large contained disc herniations. Neurosurgery. 2005;57(4 suppl):357–360. [DOI] [PubMed] [Google Scholar]
- 31. Shin DA, Kim KN, Shin HC, Yoon DH. The efficacy of microendoscopic discectomy in reducing iatrogenic muscle injury. J Neurosurg Spine. 2008;8:39–43. [DOI] [PubMed] [Google Scholar]
- 32. Yoon SM, Ahn SS, Kim KH, Kim YD, Cho JH, Kim DH. Comparative study of the outcomes of percutaneous endoscopic lumbar discectomy and microscopic lumbar discectomy using the tubular retractor system based on the VAS, ODI, and SF-36. Korean J Spine. 2012;9:215-222. doi:10.14245/kjs.2012.9.3.215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Ahn SS, Kim SH, Kim DW, Lee BH. Comparison of outcomes of percutaneous endoscopic lumbar discectomy and open lumbar microdiscectomy for young adults: a retrospective matched cohort study. World Neurosurg. 2016;86:250–258. [DOI] [PubMed] [Google Scholar]
- 34. Ahn Y, Lee SG, Son S, Keum HJ. Transforaminal endoscopic lumbar discectomy versus open lumbar microdiscectomy: a comparative cohort study with a 5-year follow-up. Pain Physician. 2019;22:295–304. [PubMed] [Google Scholar]
- 35. Choi KC, Kim JS, Park CK. Percutaneous endoscopic lumbar discectomy as an alternative to open lumbar microdiscectomy for large lumbar disc herniation. Pain Physician. 2016;19:E291–E300. [PubMed] [Google Scholar]
- 36. Jeong JS, Lee SH, Lee SJ, Hwang BW. The clinical comparison between open surgery and percutaneous endoscopic lumbar discectomy in extraforaminal lumbar disc herniation. J Korean Neurosurg Soc. 2006;39:413–418. [Google Scholar]
- 37. Kim MJ, Lee SH, Jung ES, et al. Targeted percutaneous transforaminal endoscopic diskectomy in 295 patients: comparison with results of microscopic diskectomy. Surg Neurol. 2007;68:623–631. [DOI] [PubMed] [Google Scholar]
- 38. Lee JS, Kim HS, Pee YH, Jang JS, Jang IT. Comparison of percutaneous endoscopic lumbar diskectomy and open lumbar microdiskectomy for recurrent lumbar disk herniation. J Neurol Surg A Cent Eur Neurosurg. 2018;79:447–452. [DOI] [PubMed] [Google Scholar]
- 39. Lee DY, Shim CS, Ahn Y, Choi YG, Kim HJ, Lee SH. Comparison of percutaneous endoscopic lumbar discectomy and open lumbar microdiscectomy for recurrent disc herniation. J Korean Neurosurg Soc. 2009;46:515-521. doi:10.3340/jkns.2009.46.6.515 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Lee SH, Chung SE, Ahn Y, Kim TH, Park JY, Shin SW. Comparative radiologic evaluation of percutaneous endoscopic lumbar discectomy and open microdiscectomy: a matched cohort analysis. Mt Sinai J Med. 2006;73:795–801. [PubMed] [Google Scholar]
- 41. Teli M, Lovi A, Brayda-Bruno M, et al. Higher risk of dural tears and recurrent herniation with lumbar micro-endoscopic discectomy. Eur Spine J. 2010;19:443-450. doi:10.1007/s00586-010-1290-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Qin R, Liu B, Hao J, et al. Percutaneous endoscopic lumbar discectomy versus posterior open lumbar microdiscectomy for the treatment of symptomatic lumbar disc herniation: a systemic review and meta-analysis. World Neurosurg. 2018;120:352–362. [DOI] [PubMed] [Google Scholar]
- 43. Kim M, Lee S, Kim HS, Park S, Shim SY, Lim DJ. A comparison of percutaneous endoscopic lumbar discectomy and open lumbar microdiscectomy for lumbar disc herniation in the Korean: a meta-analysis. Biomed Res Int. 2018;2018:9073460. doi:10.1155/2018/9073460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Zhang B, Liu S, Liu J, et al. Transforaminal endoscopic discectomy versus conventional microdiscectomy for lumbar discherniation: a systematic review and meta-analysis. J Orthop Surg Res. 2018;13:169. doi:10.1186/s13018-018-0868-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Barber SM, Nakhla J, Konakondla S, et al. Outcomes of endoscopic discectomy compared with open microdiscectomy and tubular microdiscectomy for lumbar disc herniations: a meta-analysis. Published online September 6, 2019. J Neurosurg Spine. 2019;1-14. doi:10.3171/2019.6.SPINE19532 [DOI] [PubMed] [Google Scholar]
- 46. Chen X, Chamoli U, Lapkin S, Castillo JV, Diwan AD. Complication rates of different discectomy techniques for the treatment of lumbar disc herniation: a network meta-analysis. Eur Spine J. 2019;28:2588–2601. [DOI] [PubMed] [Google Scholar]
- 47. Feng F, Xu Q, Yan F, et al. Comparison of 7 surgical interventions for lumbar disc herniation: a network meta-analysis. Pain Physician. 2017;20:E863–E871. [PubMed] [Google Scholar]
- 48. Parker SL, Xu R, McGirt MJ, Witham TF, Long DM, Bydon A. Long-term back pain after a single-level discectomy for radiculopathy: incidence and health care cost analysis. J Neurosurg Spine. 2010;12:178–182. [DOI] [PubMed] [Google Scholar]
- 49. Rasouli MR, Rahimi-Movaghar V, Shokraneh F, Moradi-Lakeh M, Chou R. Minimally invasive discectomy versus microdiscectomy/open discectomy for symptomatic lumbar disc herniation. Cochrane Database Syst Rev. 2014;(9):CD010328. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, Supp_File_1 for Is Endoscopic Discectomy the Next Gold Standard in the Management of Lumbar Disc Disease? Systematic Review and Superiority Analysis by Sathish Muthu, Eswar Ramakrishnan and Girinivasan Chellamuthu in Global Spine Journal