Abstract
Study Design:
Retrospective study.
Objective:
Previous studies have demonstrated that increased implant density (ID) results in improved coronal deformity correction. However, low-density constructs with strategically placed fixation points may achieve similar coronal correction. The purpose of this study was to identify key zones along the spinal fusion where high ID statistically correlated to improved coronal deformity correction. Our hypothesis was that high ID within the periapical zone would not be associated with increased percent Cobb correction.
Methods:
We identified patients with Lenke type 1 curves with a minimum 2-year follow up. The instrumented vertebral levels were divided into 4 zones: (1) cephalad zone, (2) caudal zone, (3) apical zone, and (4) periapical zone. High and low percent Cobb correction groups were compared, high percent Cobb group was defined as percent correction >67%. Total ID, total concave ID, total convex ID, and ID within each zone of the curve were compared between the groups. A multivariable analysis was performed to identify independent predictors for coronal correction. Subsequently increased and decreased thoracic kyphosis (TK) groups were compared, increased TK was defined as post-operative TK being larger than preoperative TK and decreased TK was defined as post-operative TK being less than preoperative TK.
Results:
The cohort included 68 patients. The high percent Cobb group compared with the low percent Cobb group had significantly greater ID for the entire construct, the total concave side, the total convex side, the apical convex zone, the periapical zone, and the cephalad concave zone. The high percent Cobb group had greater pedicle screw density for the total construct, total convex side, and total concave side. In the multivariate model ID and pedicle screw density remained significant for percent Cobb correction. Ability to achieve coronal balance was not statistically correlated to ID (P = .78).
Conclusions:
Increased ID for the entire construct, the entire convex side, the entire concave side, and within each spinal zone was associated with improved percent Cobb correction. The ability to achieve coronal balance was not statistically influence by ID. The results of this study support that increasing ID along the entire length of the construct improves percent Cobb correction.
Keywords: adolescent idiopathic scoliosis, implant density, pedicle screw distribution
Introduction
Adolescent idiopathic scoliosis (AIS) is a spinal deformity in the coronal, sagittal, and axial plane that develops during growth. The primary goal of surgical management in AIS is to prevent curve progression. The secondary goal of surgery is to correct deformity in the coronal and sagittal planes to minimize disfigurement. Posterior spinal fusion (PSF) with segmental pedicle screw fixation is the current standard of care for the surgical management of AIS. However, the ideal distribution and implant density (ID) of pedicle screws remains unclear, and wide variability exists in construct designs between spinal surgeons. 1
Pedicle screw fixation provides 3-column fixation of the vertebral body with improved biomechanical properties and ability to correct coronal and transverse plane deformity compared to hybrid and all hook constructs. 2 - 13 In addition, pedicle screws allow for fewer segments to be utilized in the fusion and diminish the need for anterior surgery. 4,6,14 Despite these benefits, pedicle screw implantation has greatly increased the cost of scoliosis surgery and pedicle screws may be associated with residual hypokyphosis of the thoracic spine. 15 -17
The ID was a numeric value devised to demonstrate how the number of fixation points along a fusion correlated with the ability to achieve a greater curve correction. 18 High implant density (HD) constructs have been associated with increased construct stiffness and improved ability to correct the spinal deformity. 18 -24 However, many authors advocate for low implant density (LD) constructs as a way to decrease the total cost associated with surgery, to decrease operative time, minimize intraoperative blood loss, and minimize the risk of neurologic injury that can occur with pedicle screw placement.
Selectively choosing the position of fixation points along the concave and convex sides of the fusion is likely equally, or potentially more important than ID in achieving spinal correction. A number of studies have investigated how ID impacts curve correction. However, the regions along the length of the fusion that need to contain more or less screws to achieve maximal correction remains unknown. Identification of the key fixation points or zones of fixation along the fusion would allow spinal surgeons to potentially minimize the number of pedicle screws utilized without compromising percent correction.
In this study, the length of the spinal fusion was divided into 4 zones (apical, periapical, cephalad, and caudad zones), and ID was determined within each of these zones. The primary objective of the study was to analyze the impact of ID within each of these zones in order to determine where higher ID correlates with improved percent curve correction. Secondary objectives of the study were to determine the impact of pedicle screws compared with hybrid constructs on percent curve correction and to determine if LD constructs resulted in decreased percent curve correction.
Methods
We queried our medical record for pediatric patients that had underwent PSF for idiopathic scoliosis between the years 2005-2008 and 2013-2015 by a single senior surgeon (R.D.F). The reason for the selection of specific years was that in 2005-2008 the surgeon utilized LD constructs, and from 2013-2015 the surgeon tended to utilize HD constructs. Patients were excluded from the study if they had neuromuscular scoliosis, congenital scoliosis, juvenile scoliosis, insufficient imaging, and idiopathic curves other than Lenke type 1. Cases meeting inclusion criteria underwent chart review to obtain further demographic, operative, and clinical information.
A total of 273 PSF patients were identified within the specified years. After excluding patients, 94 patients were identified as having Lenke type 1 AIS curves. The final cohort consisted of 68 patients as 26 patients had either insufficient imaging or follow up for inclusion. The final cohort included 29 patients from 2005-2008 and 39 patients from 2013-2015. For each patient, the instrumented fusion levels were subdivided into 4 zones: (1) cephalad zone, (2) caudal zone, (3) apical zone, and (4) periapical zone (Figure 1).
Figure 1.
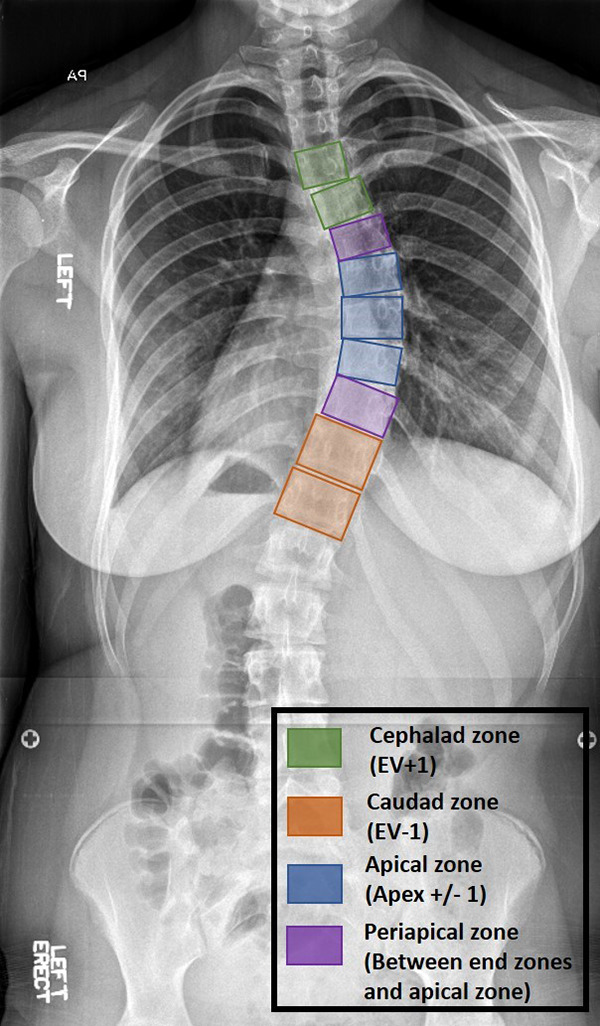
Depiction of the different spinal zones investigated for implant density.
For each patient the ID was calculated for the entire construct, the concave side, the convex side, and within each zone of the fusion. ID was defined as the number of fixation points implanted per vertebra (pedicle screw, hook, or sublaminar wire). Maximum ID was 2 for a level indicating a point of fixation on the concave and convex sides. The ID of the total concave side and convex side were calculated as a percentage with 100% indicating a fixation point at every level of the selected fusion. In addition to ID, pedicle screw density was calculated for the entire construct, the concave side, and the convex side. Pedicle screw density was defined as the percent of fixation points occupied by a pedicle screw compared with a hook or sublaminar wire.
Patients were divided into high and low percent Cobb correction groups. The high percent Cobb correction group was defined as correction greater than the median percent Cobb correction (67%) of the cohort, and the low percent Cobb correction group was defined as correction less 67%. The 2 groups were compared for ID of the total convex side, the total concave side, and each respective zone using Welch’s t tests. A bivariate linear regression model was used to examine the relationship between total implant density and percent Cobb correction. A multivariable regression model was used to examine the impact of curve flexibility, Lenke lumbar modifier, number of levels fused, total implant density, implant density within each zone, and pedicle screw density on percent Cobb correction. Statistical significance was set at an α level of .05.
A second analysis was performed comparing high-density (HD) and low-density (LD) constructs. The median ID of the entire cohort was 1.56. HD constructs were defined as an ID ≥1.56, and LD constructs were defined as an ID <1.56. In the current literature no gold standard exists for what constitutes a low and high ID construct, and the authors of this manuscript acknowledge that a value of 1.56 was picked based on this cohort alone. The HD and LD groups were compared for percent Cobb correction, coronal balance, and loss of correction at 1-year following surgery using Welch’s t tests.
Results
The cohort included 68 pediatric patients with AIS that had Lenke type 1 curves. The cohort was predominantly female (79.4%). The average age at time of surgery was 14.3 years (range 11-20 years). The cohort included 32 Lenke 1A, 22 Lenke 1B, and 14 Lenke 1C cases. The average thoracic Cobb angle for the overall cohort was 56.9° ± 8.5°, and the average bending Cobb angle was 33.0° ± 8.2° (Table 1). Overall, the mean Cobb correction for the cohort was 67%, and the mean ID for the entire construct was 1.56. The average IDs in the respective zones were, cephalad zone 1.5 ± 0.32, caudal zone 1.75 ± 0.3, apical zone 1.6 ± 0.38, and periapical zone 1.3 ± 0.48 (Table 1). Of the surgical patients from 2005-2008 26 of 29 patients had LD constructs, and the average ID was 1.34 ± 0.22. Of the patients treated between 2013 and 2015, 38 of 39 patients had HD constructs, and the average ID was 1.77 ± 0.12.
Table 1.
Initial Curve Description and Implant Distribution.
| Initial curve description | |
|---|---|
| Thoracic Cobb angle (mean ± SD) | 56.9° ± 8.5° |
| Bending Cobb angle (mean ± SD) | 33.0° ± 8.2° |
| Lenke 1A | n = 32 |
| Lenke 1B | n = 22 |
| Lenke 1C | n = 14 |
| Implant distribution | |
| Zone of curve | Implant density |
| Total curve | 1.56 ± 0.28 |
| Total convex side | 65.2% ± 17.9% |
| Total concave side | 91.2% ± 13.8% |
| Cephalad zone | 1.5 ± 0.32 |
| Caudal zone | 1.75 ± 0.3 |
| Apical zone | 1.6 ± 0.38 |
| Periapical zone | 1.3 ± 0.48 |
Total ID significantly correlated with percent Cobb correction (r2 = 0.3, P < .001). In the multivariable model total implant density (P < .001), total ID along the convex side (P < .001), total ID along the concave side (P < .001), ID of the concave apical zone (P = .02), ID of the convex apical zone (P = .004), ID of the concave periapical zone (P < .001), ID of the convex periapical zone (P = .002), ID of the concave cephalad zone (P < .001), and pedicle screw density (P < .001) were significantly associated with improved percent Cobb correction (Table 2). Curve flexibility, length of fixation, ID of the convex cephalad zone, and ID of the convex and concave caudal zones were not associated with improved percent Cobb correction.
Table 2.
Multivariable Analysis for Improved Percent Cobb Correction.
| Variable | Coefficient | CI | P |
|---|---|---|---|
| Implant density (ID) | |||
| Total ID | 29.1 | 17.94, 40.27 | <.001 |
| Total convex side ID | 0.38 | 0.20, 0.57 | <.001 |
| Total concave side ID | 0.53 | 0.29, 0.75 | <.001 |
| Concave apical zone ID | 0.22 | 0.03, 0.41 | .02 |
| Convex apical zone ID | 0.19 | 0.06, 0.31 | .004 |
| Concave periapical zone ID | 0.24 | 0.11, 0.38 | <.001 |
| Convex periapical zone ID | 0.16 | 0.06, 0.26 | .002 |
| Concave cephalad zone ID | 0.28 | 0.14, 0.43 | <.001 |
| Convex cephalad zone ID | 0.01 | −0.14, 0.15 | .912 |
| Concave caudad zone ID | 0.19 | −0.07, 0.46 | .15 |
| Convex caudad zone ID | 0.06 | −0.09, 0.21 | .43 |
| Additional variables | |||
| Pedicle screw density | 0.42 | 0.25, 0.59 | <.001 |
| Curve flexibility | −0.16 | −0.52, 0.20 | .37 |
| Length of fusion | −0.52 | −2.57, 1.53 | .61 |
The high percent Cobb correction and the low percent Cobb correction groups each had 34 patients. The high percent Cobb correction group had a percent Cobb correction >67%. Comparing the 2 groups, the high percent Cobb correction group had significantly greater ID for the total convex side (71.7% vs 57.8%, P = .001), the total concave side (95.9% vs 85.8%, P = .003), the apical convex zone (78.7% vs 60.4%, P = .007), the periapical convex zone (58.2% vs 37.7%, P = .01), the periapical concave zone (95.4% vs 82.0%, P = .02), and the cephalad concave zone (93.1% vs 78.1%, P = .007) (Table 3). The high percent Cobb correction group had greater pedicle screw densities of the entire construct (93.7% vs 77.9%, P < .001), the concave side (97.6% vs 77.8%, P < .001), and the convex side (87.9% vs 78.4%, P = .01).
Table 3.
High Percent Cobb Correction Versus Low Percent Cobb Correction: Zonal Implant Density (ID) and Cobb Correction.
| Zone | High percent Cobb correction ID (>67% Cobb correction) | Low percent Cobb Correction ID (<67% Cobb correction) | P |
|---|---|---|---|
| Total construct | 1.67 | 1.44 | <.001 |
| Total concave side | 95.9% | 85.8% | .003 |
| Total convex side | 71.7% | 57.8% | .001 |
| Apical convex | 78.7% | 60.4% | .007 |
| Apical concave | 95.8% | 88.5% | .12 |
| Periapical concave | 95.4% | 82% | .02 |
| Periapical convex | 58.2% | 37.7% | .01 |
| Cephalad concave | 93.1% | 78.1% | .007 |
| Cephalad convex | 66.6% | 64.0% | .64 |
| Caudad concave | 98.6% | 93.7% | .14 |
| Caudad convex | 81.9% | 75.0% | .25 |
The high ID group and the low ID groups each had 34 patients. The average percent Cobb correction in the high ID group was 71.6% and the average percent Cobb correction in the low ID group was 57.10% (P < .001) (Table 4). The high ID had average improvement of coronal balance of 1.04 cm and the low ID group had average improvement of coronal balance of 1.1 cm (P = .776). Both groups had minimal loss of correction at 1 year. The average cost of the high ID hardware was US$11 489.88, and the average cost of the low ID hardware was US$7173.96.
Table 4.
Comparison of HIgh-Density (HD) and Low-Density (LD) Constructs.
| LD constructs (ID < 1.56) | HD constructs (ID ≥ 1.56) | P | |
|---|---|---|---|
| % Cobb correction | 57.1 | 71.6 | <.001 |
| Improvement in coronal balance (cm) | 1.1 | 1.04 | .78 |
| Loss of correction at 1 year (%) | 4.65 | 2.1 | .045 |
| Estimated blood loss (mL) | 905 | 812 | .56 |
| Total cost of implants (mean) | $7173.96 | $11 489.88 | <.001 |
Abbreviation: ID, implant density.
Discussion
Implant density, defined as the number of fixation points utilized compared with the total available sites, was first described in 2009. 18 Since its installment into the literature a multitude of studies, and 2 study groups, Minimize Implants Maximize Outcomes and Spinal Deformity Study Group, have thoroughly investigated this topic. However, a definitive answer to if ID correlates to percent Cobb correction remains unclear with select studies demonstrating improved correction with HD constructs. 17,18,21 -24 In contrast, a number of other studies demonstrate no difference in Cobb correction between HD and LD constructs. 16,25 -30 In our cohort, increasing ID was significantly associated with improved percent Cobb correction. One strength of our study is the use of multivariate analysis. In this model, ID and pedicle screw density were predictive of percent Cobb correction. This data coincides with the single other study utilizing a multivariable model to evaluate ID’s impact on curve correction. 21 The largest study investigating ID in the literature was a database review which included 952 patients and demonstrated a 69% correction with HD constructs (ID > 1.54) compared with a 66% correction in LD constructs (ID < 1.54), which was statistically significant (P = .002). 20 It is important to note that despite multiple studies investigating the topic of ID, currently no gold standard or definition has been published as to what constitutes a LD or a HD construct. The persistent inconsistency in outcomes, despite sufficient investigations, lead to the theory that implant distribution may impact curve correction to an equal or greater degree than ID, and with the correct screw placement LD constructs can achieve excellent curve correction.
The distribution of fixation points along the fusion has become the interest of recent studies, and ultimately, could result in standardization of pedicle screw placement. The principle aim of our study was to determine in which zones of the spinal fusion (caudad zone, cephalad zone, apical zone, and periapical zone) does increasing ID lead to improved Cobb correction. We sought to demonstrate zones where pedicle screws should be placed, and zones where pedicle screws may not be needed, to limit the use of pedicle screws without threatening curve correction. In our patients, the ID along the concave side of the fusion (91.2%) was greater than the convex side (65.2%). The average ID in each zone were 1.75 (caudal zone), 1.6 (apical zone), 1.5 (cephalad zone), and 1.3 (periapical zone). In the high percent Cobb correction group, the IDs in the apical convex zone, the periapical convex and concave zones, and the cephalad concave zone were significantly greater than in the low percent Cobb correction group. The ID in the remaining zones; apical concave, cephalad convex, and caudal convex and concave were not significantly different between the high and low percent Cobb correction groups. Additionally, in the multivariable model ID of the total concave, the total convex, the concave cephalad zone, the apical zones, and the periapical zones were individually related to improved percent Cobb correction.
Evaluating how the distribution of pedicle screws affects percent Cobb correction is difficult due to the innumerable possibilities of screw positioning for each fusion. For example, a 10-level fusion has 400 different possible pedicle screw combinations. Recurring patterns for LD constructs have emerged including interval fixation, skipped fixation, and key pedicle screw placement. 24,29 -35 Interval fixation indicates skipping pedicle screws along both the concave and convex sides of the fusion. Skipped fixation indicates 100% implant density along the concavity with alternating pedicle screw placement along the convexity. And key pedicle screw placement places pedicle screws at the cephalad levels, caudad levels, and at the apex of the curve. Caution needs to be maintained when utilizing the above nomenclature as inconsistencies in definitions exist between studies. The studies, in general, are comparative studies of the above screw patterns with regard to radiographic and clinical outcomes to consecutively instrumented fusions. 24,30,31,33,34 One randomized control study compared 23 patients managed with key pedicle screw placement (average ID 1.18) with 23 patients managed with skipped pedicle screw placement (average ID 1.6) and demonstrated no difference in radiographic or clinical outcomes at 2-year follow-up. 29 Similar to studies on ID, discrepancy exists in the outcomes for the screw pattern studies. The majority of studies demonstrate similar percent Cobb correction between the LD constructs and consecutively instrumented (ID 2.0) constructs. 30,31,33 However, Ketenci et al 24 reported improved percent Cobb correction and transverse plane correction in the HD construct compared to interval fixation.
The above studies demonstrate the efficacy of specific screw patterns but provide less information on which of the screws are necessary or which screws may still not be required to provide correction. In a recent study, 279 Lenke type 1 curves were reviewed from the Spinal Deformity Database and the IDs of the entire construct, the convex side, the concave side, the caudad zone, the cephalad zone, the apical zone, and the periapical zones were assessed as predictors of percent Cobb correction. In a multivariable model total ID, ID of the concave side, and ID of the apical concavity were significant for percent Cobb correction. The conclusion from the author was that LD constructs are efficacious, but screws need to be placed at the apical concavity. 23 In our study, the same spinal zones were compared, and similarly total ID was predictive of percent Cobb correction. However, our outcomes demonstrated greater percent Cobb correction with increased ID in the periapical zones in addition to the apical zone. The results of our study demonstrate improved correction with increasing ID, and the positions of the fixation points were less important than the increased fixation.
During surgical correction fixation was achieved with pedicle screws, sublaminar wires, or hooks. Hybrid fixation was utilized in the earlier treated patients with a trend toward pedicle screw fixation in the later treated patients. It has become largely accepted that pedicle screw fixation allows for a greater correction to hybrid and all hook constructs. 2,3,5 -8,30 In our high percent Cobb correction group a greater pedicle screw density was observed for the total construct, total convex side, and total concave side. These results were consistent with previously reported outcomes. One concern of our study was that pedicle screw density was confounding the results on ID distribution; however, the multivariable model demonstrates that both ID and pedicle screw density individually improve percent Cobb correction.
An additional concern of low ID constructs is loss of correction over time. Biomechanics studies have demonstrated improved construct stiffness with HD constructs. 19 Loss of correction over time has been reported in the literature with LD constructs. 35 In the cohort, the low ID group’s Cobb angle decreased by 4.56% compared with 2.1% in the high ID group at 1-year following surgery. Although this was statistically significant between the groups, this minor difference between the groups is likely not clinically significant.
Our study has a number of limitations. First, our primary outcome was coronal curve correction. We did not compare pre- and postoperative thoracic kyphosis or axial rotation of the apical vertebra. Thoracic kyphosis could not be reliably measured in the radiographs used in data collection. It is clear that patient outcomes following AIS surgery are not solely dependent on coronal plane correction. Limiting the number of fixation points limits the ability to perform segmental derotation. Despite the potential to achieve similar coronal curve correction with LD constructs, transverse plane correction may be decreased without the ability to segmentally derotate. Second, we did not report patient reported functional outcome scores between our groups. Unfortunately, we did not have this data available during data collection. However, previous studies have been consistent in demonstrating no difference in patient reported outcome scores between HD and LD constructs. 23 A strength of our study was all of the data was collected at a single institution, not from a large multicenter database, and all of the surgeries were performed by a single senior author. A single surgeon eliminates variability in the technique to correct the deformity as could be present in many of the previous studies. The surgeon performing these surgeries performed the same correctional maneuvers for all of the patients utilizing the Cotrel-Dubbouset technique of rod rotation. Additionally, our study was the first study to look at ID in high versus low percent Cobb correction groups, all previous studies separated groups based on a LD and HD constructs.
Conclusion
Our hypothesis was rejected, and total ID was significantly associated with improved percent Cobb correction. Our results support that increasing ID leads to improved percent Cobb correction, and the distribution of the fixation points is less important than the increased fixation. Previous studies demonstrated that fixation within the periapical zones was not associated with improved percent Cobb correction; however, our data demonstrates increased fixation within these zones improved coronal curve correction. Additionally, similar to previous studies, pedicle screws were superior to hooks and sublaminar wires for achieving greater percent Cobb correction. The outcomes of this study support the trend in the pediatric spine community over time of transitioning from hybrid constructs to pedicle screw constructs and transitioning from lower to higher density implant constructs to achieve the most deformity correction. Our data does not advocate for the use of HD or LD constructs, as patient outcomes were not evaluated, but we do demonstrate that increasing total ID, total convex ID, total concave ID, and ID within the apical and periapical zones leads to improved coronal correction.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Brian L. Dial, MD  https://orcid.org/0000-0002-7992-5975
https://orcid.org/0000-0002-7992-5975
References
- 1. Aubin CE, Labelle H, Ciolofan OC. Variability of spinal instrumentation configurations in adolescent idiopathic scoliosis. Eur Spine J. 2007;16:57–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Liljenqvist U, Lerner T, Bullmann V. Selective fusion of idiopathic scoliosis with respect to the Lenke classification [in German]. Orthopade. 2009;38:189-192,194–197. [DOI] [PubMed] [Google Scholar]
- 3. Suk SI, Kim JH, Kim SS, Lim DJ. Pedicle screw instrumentation in adolescent idiopathic scoliosis (AIS). Eur Spine J. 2012;21:13–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kim YJ, Lenke LG, Cho SK, Bridwell KH, Sides B, Blanke K. Comparative analysis of pedicle screw versus hook instrumentation in posterior spinal fusion of adolescent idiopathic scoliosis. Spine (Phila Pa). 2004;29:2040–2048. [DOI] [PubMed] [Google Scholar]
- 5. Kim YJ, Lenke LG, Kim J, et al. Comparative analysis of pedicle screw versus hybrid instrumentation in posterior spinal fusion of adolescent idiopathic scoliosis. Spine (Phila Pa 1976). 2006;31:291–298. [DOI] [PubMed] [Google Scholar]
- 6. Di Silvestre M, Bakaloudis G, Lolli F, Vommaro F, Martikos K, Parisini P. Posterior fusion only for thoracic adolescent idiopathic scoliosis of more than 80 degrees: pedicle screws versus hybrid instrumentation. Eur Spine J. 2008;17:1336–1349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Yilmaz G, Borkhuu B, Dhawale AA, et al. Comparative analysis of hook, hybrid, and pedicle screw instrumentation in the posterior treatment of adolescent idiopathic scoliosis. J Pediatr Orthop. 2012;32:490–499. [DOI] [PubMed] [Google Scholar]
- 8. Rafi S, Munshi N, Abbas A, Shaikh RH, Hashmi I. Comparative analysis of pedicle screw versus hybrid instrumentation in adolescent idiopathic scoliosis surgery. J Neurosci Rural Pract. 2016;7:550–553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Asher MA, Cook LT. The transverse plane evolution of the most common adolescent idiopathic scoliosis deformities. A cross-sectional study of 181 patients. Spine (Phila Pa 1976). 1995;20:1386–1391. [PubMed] [Google Scholar]
- 10. Kuklo TR, Potter BK, Polly DW, Jr, Lenke LG. Monaxial versus multiaxial thoracic pedicle screws in the correction of adolescent idiopathic scoliosis. Spine (Phila Pa 1976). 2005;30:2113–2120. [DOI] [PubMed] [Google Scholar]
- 11. Hwang SW, Samdani AF, Stanton P, et al. Impact of pedicle screw fixation on loss of deformity correction in patients with adolescent idiopathic scoliosis. J Pediatr Orthop. 2013;33:377–382. [DOI] [PubMed] [Google Scholar]
- 12. Brown CA, Lenke LG, Bridwell KH, Geideman WM, Hasan SA, Blanke K. Complications of pediatric thoracolumbar and lumbar pedicle screws. Spine (Phila Pa 1976). 1998;23:1566–1571. [DOI] [PubMed] [Google Scholar]
- 13. Gaines RW, Jr. The use of pedicle-screw internal fixation for the operative treatment of spinal disorders. J Bone Joint Surg Am. 2000;82:1458–1476. [DOI] [PubMed] [Google Scholar]
- 14. Luhmann SJ, Lenke LG, Kim YJ, Bridwell KH, Schootman M. Thoracic adolescent idiopathic scoliosis curves between 70 degrees and 100 degrees: is anterior release necessary? Spine (Phila Pa 1976). 2005;30:2061–2067. [DOI] [PubMed] [Google Scholar]
- 15. Larson AN, Polly DW, Jr, Ackerman DJ, et al. What would be the annual cost savings if fewer screws were used in adolescent idiopathic scoliosis treatment in the US? J Neurosurg Spine. 2016;24:116–123. [DOI] [PubMed] [Google Scholar]
- 16. Quan GM, Gibson MJ. Correction of main thoracic adolescent idiopathic scoliosis using pedicle screw instrumentation: does higher implant density improve correction? Spine (Phila Pa). 2010;35:562–567. doi:10.1097/BRS.0b013e3181b4af34 [DOI] [PubMed] [Google Scholar]
- 17. Larson AN, Aubin CE, Polly DW, Jr, et al. Are more screws better? a systematic review of anchor density and curve correction in adolescent idiopathic scoliosis. Spine Deform. 2013;1:237–247. doi:10.1016/j.jspd.2013.05.009 [DOI] [PubMed] [Google Scholar]
- 18. Clements DH, Betz RR, Newton PO, Rohmiller M, Marks MC, Bastrom T. Correlation of scoliosis curve correction with the number and type of fixation anchors. Spine (Phila Pa 1976). 2009;34:2147–2150. [DOI] [PubMed] [Google Scholar]
- 19. Deviren V, Acaroglu E, Lee J, et al. Pedicle screw fixation of the thoracic spine: an in vitro biomechanical study on different configurations. Spine (Phila Pa 1976). 2005;30:2530–2537. [DOI] [PubMed] [Google Scholar]
- 20. Larson AN, Polly DW, Jr, Diamond B, et al. Does higher anchor density result in increased curve correction and improved clinical outcomes in adolescent idiopathic scoliosis? Spine (Phila Pa 1976). 2014;39:571–578. [DOI] [PubMed] [Google Scholar]
- 21. Mac-Thiong JM, Ibrahim S, Parent S, et al. Defining the number and type of fixation anchors for optimal main curve correction in posterior surgery for adolescent idiopathic scoliosis. Spine J. 2017;17:663–670. [DOI] [PubMed] [Google Scholar]
- 22. Sanders JO, Diab M, Richards SB, et al. Fixation points within the main thoracic curve: does more instrumentation produce greater curve correction and improved results? Spine (Phila Pa 1976). 2011;36:E1402–E1406. [DOI] [PubMed] [Google Scholar]
- 23. Le Naveaux F, Aubin CE, Larson AN, et al. Implant distribution in surgically instrumented Lenke 1 adolescent idiopathic scoliosis: does it affect curve correction? Spine (Phila Pa 1976). 2015;40:462–468. [DOI] [PubMed] [Google Scholar]
- 24. Ketenci IE, Yanik HS, Demiroz S, Ulusoy A, Erdem S. Three-dimensional correction in patients with Lenke 1 adolescent idiopathic scoliosis: comparison of consecutive versus interval pedicle screw instrumentation. Spine (Phila Pa 1976). 2016;41:134–138. [DOI] [PubMed] [Google Scholar]
- 25. Bharucha NJ, Lonner BS, Auerbach JD, Kean KE, Trobisch PD. Low-density versus high-density thoracic pedicle screw constructs in adolescent idiopathic scoliosis: do more screws lead to a better outcome? Spine J. 2013;13:375–381. [DOI] [PubMed] [Google Scholar]
- 26. Rushton PR, Elmalky M, Tikoo A, Basu S, Cole AA, Grevitt MP. The effect of metal density in thoracic adolescent idiopathic scoliosis. Eur Spine J. 2016;25:3324–3330. [DOI] [PubMed] [Google Scholar]
- 27. Gebhart S, Alton TB, Bompadre V, Krengel WF. Do anchor density or pedicle screw density correlate with short-term outcome measures in adolescent idiopathic scoliosis surgery? Spine (Phila Pa 1976). 2014;39:E104–E110. [DOI] [PubMed] [Google Scholar]
- 28. Shen M, Jiang H, Luo M, et al. Comparison of low density and high density pedicle screw instrumentation in Lenke 1 adolescent idiopathic scoliosis. BMC Musculoskelet Disord. 2017;18:336. doi:10.1186/s12891-017-1695-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Gotfryd AO, Avanzi O. Randomized clinical study on surgical techniques with different pedicle screw densities in the treatment of adolescent idiopathic scoliosis types Lenke 1A and 1B. Spine Deform. 2013;1:272–279. doi:10.1016/j.jspd.2013.05.004 [DOI] [PubMed] [Google Scholar]
- 30. Luo M, Shen M, Wang W, Xia L. Comparison of consecutive, interval, and skipped pedicle screw techniques in moderate Lenke type 1 adolescent idiopathic scoliosis. World Neurosurg. 2017;98:563–570. doi:10.1016/j.wneu.2016.11.064 [DOI] [PubMed] [Google Scholar]
- 31. Li J, Cheung KM, Samartzis D, et al. Key-vertebral screws strategy for main thoracic curve correction in patients with adolescent idiopathic scoliosis. Clin Spine Surg. 2016;29:E434–E441. doi:10.1097/BSD.0000000000000129 [DOI] [PubMed] [Google Scholar]
- 32. Hwang CJ, Lee CK, Chang BS, Kim MS, Yeom JS, Choi JM. Minimum 5-year follow-up results of skipped pedicle screw fixation for flexible idiopathic scoliosis. J Neurosurg Spine. 2011;15:146–150. doi:10.3171/2011.4.SPINE10321 [DOI] [PubMed] [Google Scholar]
- 33. Morr S, Carrer A, de Quesada LIAG, Rodriguez-Olaverri JC. Skipped versus consecutive pedicle screw constructs for correction of Lenke 1 curves. Eur Spine J. 2015;24:1473–1480. [DOI] [PubMed] [Google Scholar]
- 34. Wang F, Xu XM, Lu Y, Wei XZ, Zhu XD, Li M. Comparative analysis of interval, skipped, and key-vertebral pedicle screw strategies for correction in patients with Lenke type 1 adolescent idiopathic scoliosis. Medicine (Baltimore). 2016;95:e3021. doi:10.1097/MD.0000000000003021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Wei XZ, Zhou XY, Yang YL, et al. Key Vertebral pedicle screw strategy for the correction of flexible Lenke type 1 adolescent idiopathic scoliosis: a preliminary study of a 5-year minimum radiographic follow-up. Spine (Phila Pa). 2017;42:1226–1232. doi:10.1097/BRS.0000000000002143 [DOI] [PubMed] [Google Scholar]


