Abstract
Background
Understanding trends in the incidence and outcomes of myocardial infarction and stroke, and how these are influenced by changes in cardiovascular risk factors can inform health policy and healthcare provision.
Methods
We identified all patients 30 years or older with myocardial infarction or stroke in Scotland. Risk factor levels were determined from national health surveys. Incidence, potential impact fractions and burden attributable to risk factor changes were calculated. Risk of subsequent fatal and non-fatal events (myocardial infarction, stroke, bleeding and heart failure hospitalization) were calculated with multi-state models.
Findings
From 1990 to 2014, there were 372,873 (71±13 years) myocardial infarctions and 290,927 (74±13 years) ischemic or hemorrhagic strokes. Age-standardized incidence per 100,000 fell from 1,069 (95% confidence interval, 1,024-1,116) to 276 (263-290) for myocardial infarction and from 608 (581-636) to 188 (178-197) for ischemic stroke. Systolic blood pressure, smoking and cholesterol decreased, but body-mass index increased, and diabetes prevalence doubled. Changes in risk factors accounted for a 74% (57-91%) reduction in myocardial infarction and 68% (55-83%) reduction in ischemic stroke. Following myocardial infarction, the risk of death decreased (30% to 20%), but non-fatal events increased (20% to 24%) whereas the risk of both death (47% to 34%) and non-fatal events (22% to 17%) decreased following stroke.
Interpretation
Over the last 25 years, substantial reductions in myocardial infarction and ischemic stroke incidence are attributable to major shifts in risk factor levels. Deaths following the index event decreased for both myocardial infarction and stroke, but rates remained substantially higher for stroke.
Funding
British heart foundation
Research in Context.
Evidence before this study
We searched Ovid Medline (from 01/01/1995 to 01/08/2020) for search terms ‘cardiovascular risk factors’, ‘incidence’, ‘myocardial infarction’, ‘stroke’ and ‘outcomes’. We identified several studies including systematic reviews evaluating trends in incident myocardial infarction or stroke. Several studies evaluated impact of changes in risk factors on coronary death. We found no large contemporary nationwide studies comparing the clinical burden of stroke and myocardial infarction, evaluating the impact of population changes in risk factors on fatal and non-fatal disease and the short- and longer-term fatal and non-fatal clinical sequalae following index event.
Added value of this study
In a large contemporary nationwide patient level linkage study we show that substantial reductions in myocardial infarction and ischemic stroke incidence are associated with reductions in systolic blood pressure, smoking and cholesterol but attenuated by increases in body mass index and diabetes prevalence. Importantly, we now show that in addition to the incidence of both myocardial infarction and stroke declining, the temporal difference in the incidence has also narrowed. Deaths following the index event decreased for both myocardial infarction and stroke, but rates remained substantially higher for stroke. The clinical burden of stroke, both in terms of incidence and case-fatality, now contributes to a greater burden of acute cardiovascular disease.
Implications of all the available evidence
Substantial reductions in the incidence of both myocardial infarction and ischemic stroke can be achieved by addressing biological and behavioural risk factors. These observations have major implications for countries in low- and middle-income settings where rates of hypertension and dyslipidaemia are rising as well as the residual risk from persistent uncontrolled risk factors in high-income countries. We also highlight the increasing influence of obesity and diabetes on acute cardiovascular events, which have implications for all countries given that both risk factors are rising worldwide. Finally, differences in the burden of myocardial infarction and stroke are narrowing, particularly in women, and monitoring these trends is essential for the planning of healthcare provision in the decades that follow.
Alt-text: Unlabelled box
1. Introduction
Planning of healthcare provision for acute cardiovascular disease requires an understanding of population trends in both the incidence and subsequent clinical outcomes following acute presentation. Insights into how these trends have been impacted by changes in risk factor profiles over time are needed to inform public health policy. Despite considerable overlap between myocardial infarction and stroke, with shared pathophysiological mechanisms, risk factors and management, they have rarely been studied concurrently.[1] Previous studies comparing incidence for these two conditions were not contemporary.[1], [2], [3] Those reporting trends for myocardial infarction have predominantly been limited to fatal events,[4], [5], [6], [7], [8], [9]whilst stroke studies have been limited to smaller cohorts and younger populations.[10,[11], [12], [13]] Whilst the associations between risk factors and myocardial infarction[14] or stroke[15,16] have been studied,the impact of temporal changes in risk factors on the incidence of both, and in those with and without fatal presentations, remains uncertain.
The last two decades has seen substantial changes in the management and outcomes of myocardial infarction and stroke.[12,[17], [18], [19], [20], [21], [22], [23]] Most studies have reported trends in morbidity and mortality during the acute phase,[13,24,25] with studies of the longer term sequelae scarce[26] and report inconsistent findings.[27], [28], [29], [30], [31]
Reliable information about the comparative epidemiology regarding clinical burden, risk factor impact and the subsequent sequelae following myocardial infarction and stroke remains scarce. To inform public health policy and healthcare provision, we investigated the impact of population changes in risk factors over 25 years on incident myocardial infarction and stroke. We also report on changes in risk of subsequent fatal events, and single and multiple non-fatal events following index non-fatal myocardial infarction or stroke.
2. Methods
2.1. Study population, design and data sources
An individual patient-level linkage study (Supplement figure 1) using national datasets in Scotland (Supplementary text 1) included all patients 30 yearsof age or older with myocardial infarction or stroke from January 1st, 1990 to December 21st, 2014 with follow-up until December 31st, 2017. Using a 5-year lookback period (Supplementary text 2), index cases were identified as ICD-10 coded hospitalisations or deaths without prior hospitalisation(Supplementary table 1).Age at incident event, sex, comorbidity and area-based measure of deprivation using the Scottish Index of Multiple Deprivation (SIMD) were extracted.[32]
All index cases were linked to prior and subsequent hospital episodes and deaths from the National Health Service (NHS) Scottish Morbidity Register and National Records of Scotland using theCommunity Health Index, a register of all Scottish NHS patients. Age- and sex-stratified mid-year population estimates were obtained from National Records of Scotland. Non-fatal events consisted of heart failure, stroke, myocardial infarction and bleeding. Access to the data was approved by the NHS Scotland Public Benefit and Privacy Panel for Health and Social Care.
Age-, sex- and year-stratified population distribution of cardiovascular risk factors (systolic blood pressure, total cholesterol, body mass index and the prevalence of smoking and diabetes mellitus) were estimated from the Scottish Health Survey.[33] The Scottish Health Survey uses a multistage stratified clustered probability sampling design to ensure the results are representative of the population (Supplementary text 3). The surveys were conducted in 1995, 1998, 2003 and then annually from 2008. Age- and sex-stratified risk ratios for each risk factor were extracted from the published literature.[[14], [15], [16],34]
2.2. Statistical analysis
Baseline characteristics were summarised in 5-year intervals by index event.
Incidence modelling: Generalized additive models were used to estimate trends in incident myocardial infarction and stroke. Annual incident hospitalisations were aggregated by 10-year age intervals and sex separately for index myocardial infarction and stroke. Person-time, using the same covariates, was calculated using the population mid-year estimates (Supplementary text 2). For incidence rates, a log link and Poisson error distribution were used with a scaling factor (quasi-Poisson) to allow for overdispersion. Annual incidence rates were standardized to the European Standard Population.[35]
Burden: For each risk factor, regression models were constructed from baseline health survey data to estimate age-, sex- and year-stratified values (Supplement text 4). The number of events prevented, delayed or caused as a result of a change in risk factor level was estimated using data from three sources: the age-, sex- and year-stratified incident count, the age- and sex-stratified (where available) relative risk and absolute change in age- and sex-stratified risk factor level. Distributions were combined via Monte Carlo sampling to produce estimates of the potential impact fraction[36] (a measure of the proportional reduction in the disease or mortality risk, when the risk factor distributions change) and a final count distribution for each age-, sex- and year-strata of events prevented, delayed or caused by change in risk factor levels(Supplementary text 5).
Multistate outcome models: Time to subsequent fatal and non-fatal events (3-year follow-up) was modelled using multi-state models for index non-fatal myocardial infarction and stroke. Weibull accelerated failure time models were fitted, adjusting for age, sex, deprivation, cohort period and comorbidity (Supplementary text 6). Estimated risks were presented at the population level stratified by cohort period and standardized using the count data of the remaining categorical variables (sex, deprivation and comorbidity) as well as by age, sex, deprivation, comorbidity and cohort period. Statistical analyses were performed in R version 3.5.1 (Vienna, Austria).
Role of funding source: Funders had no role in study design, data collection, data analysis, interpretation or writing of the report
3. Results
From 1990 to 2014, among 605,996 patients, there were 372,873 (71±13 years, 43% female) and 290,927 (74±13 years, 55% female) index myocardial infarctions and strokes respectively. Compared to stroke, patients with myocardial infarction were younger and more likely to be male.Across the cohort periods, there was a modest narrowing in social inequalities (Table 1, Supplementary table 2 and 3).
Table 1.
Baseline characteristics in patients with index fatal and non-fatal myocardial infarction or stroke stratified by 5-year calendar groups.
| Variable | Index Condition | 1990 to 1994 | 1995 to 1999 | 2000 to 2004 | 2005 to 2009 | 2010 to 2014 |
|---|---|---|---|---|---|---|
| Number | Myocardial infarction | 100,929 | 82,330 | 69,415 | 58,513 | 61,686 |
| Stroke | 64,870 | 64,593 | 58,563 | 52,043 | 50,858 | |
| Age, years (mean [SD]) | Myocardial infarction | 70.2 (12.2) | 70.9 (12.5) | 71.5 (13.1) | 71.3 (13.6) | 70.2 (13.9) |
| Stroke | 74.0 (12.2) | 74.0 (12.6) | 74.0 (13.1) | 73.5 (13.5) | 73.4 (13.6) | |
| Sex, females(%) | Myocardial infarction | 44,435 (44.0) | 36,220 (44.0) | 30,080 (43.3) | 24,403 (41.7) | 24,559 (39.8) |
| Stroke | 37,149 (57.3) | 36,222 (56.1) | 32,628 (55.7) | 28,155 (54.1) | 26,931 (53.0) | |
| Past medical history | ||||||
| Ischemic heart disease (%) | Myocardial infarction | 10,069 (10.0) | 10,887 (13.2) | 10,381 (15.0) | 9,713 (16.6) | 9,425 (15.3) |
| Stroke | 6,462 (10.0) | 7,274 (11.3) | 6,780 (11.6) | 6,341 (12.2) | 5,961 (11.7) | |
| Cerebrovascular disease (%) | Myocardial infarction | 4,934 (4.9) | 4,663 (5.7) | 3,725 (5.4) | 2,856 (4.9) | 2,616 (4.2) |
| Stroke | 4,422 (6.8) | 4,093 (6.3) | 2,727 (4.7) | 2,044 (3.9) | 1,666 (3.3) | |
| Heart failure (%) | Myocardial infarction | 6,507 (6.4) | 6,445 (7.8) | 5,467 (7.9) | 4,156 (7.1) | 3,663 (5.9) |
| Stroke | 3,717 (5.7) | 3,765 (5.8) | 3,138 (5.4) | 2,482 (4.8) | 2,299 (4.5) | |
| Coronary revascularisation (%) | Myocardial infarction | 619 (0.6) | 818 (1.0) | 878 (1.3) | 1408 (2.4) | 1490 (2.4) |
| Stroke | 372 (0.6) | 675 (1.0) | 828 (1.4) | 1154 (2.2) | 1391 (2.7) | |
| Cardiac devices, (%) | Myocardial infarction | 343 (0.3) | 433 (0.5) | 436 (0.6) | 458 (0.8) | 573 (0.9) |
| Stroke | 282 (0.4) | 423 (0.7) | 418 (0.7) | 469 (0.9) | 547 (1.1) | |
|
Deprivation (SIMD), quintile (%) |
||||||
| One (most deprived) | Myocardial infarction | 27,438 (27.7) | 21,903 (26.8) | 17,959 (26.0) | 14,069 (24.2) | 15,079 (24.6) |
| Stroke | 17,357 (27.3) | 16,833 (26.2) | 14,958 (25.7) | 12,649 (24.4) | 11,988 (23.7) | |
| Two | Myocardial infarction | 24,060 (24.3) | 19,993 (24.5) | 16,645 (24.1) | 13,585 (23.4) | 14,122 (23.1) |
| Stroke | 15,115 (23.8) | 15,343 (23.9) | 13,738 (23.6) | 11,856 (22.9) | 11,370 (22.5) | |
| Three | Myocardial infarction | 19,904 (20.1) | 16,455 (20.2) | 13,846 (20.1) | 11,883 (20.4) | 12,278 (20.1) |
| Stroke | 12,717 (20.0) | 12,957 (20.2) | 11,621 (20.0) | 10,514 (20.3) | 10,136 (20.1) | |
| Four | Myocardial infarction | 15,546 (15.7) | 12,993 (15.9) | 11,307 (16.4) | 10,288 (17.7) | 10,841 (17.7) |
| Stroke | 10,298 (16.2) | 10,470 (16.3) | 9,799 (16.8) | 9,079 (17.5) | 9,099 (18.0) | |
| Five (least deprived) | Myocardial infarction | 12,053 (12.2) | 10,272 (12.6) | 9,233 (13.4) | 8,326 (14.3) | 8,880 (14.5) |
| Stroke | 8,139 (12.8) | 8,586 (13.4) | 8,121 (13.9) | 7,650 (14.8) | 7,890 (15.6) |
3.1. Incidence of myocardial infarction and stroke
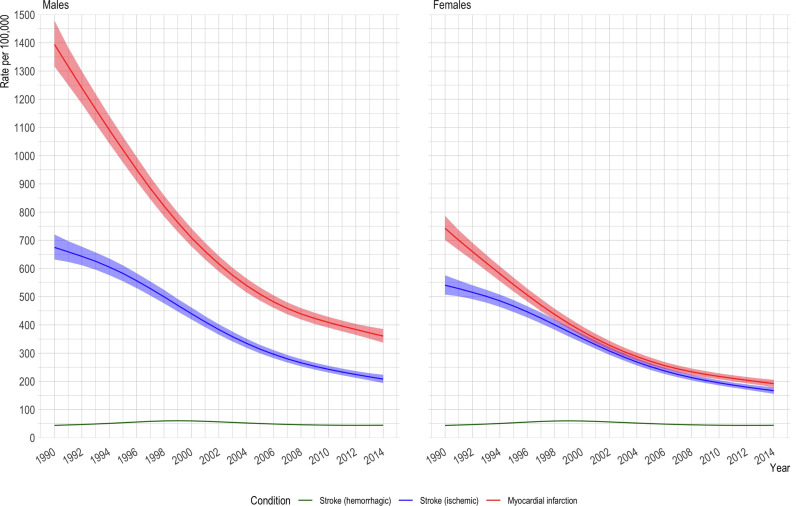
Age-standardized incidence per 100,000 fell from 1,069 [95% confidence interval 1,024 to 1,116] to 276 [263 to 290] for myocardial infarction, and from 608 [581 to 636] to 188 [178 to 197] for ischemic stroke but remained unchanged (44 [43 to 45] to 44[44 to 45]) for hemorrhagic stroke (Supplementary table 4). Similar trends were observed in males and females (Figure 1) with the highest reductions observed in older age groups (Supplementary figure 2).
Fig. 1.
Age standardized incidence rate per 100,000 for myocardial infarction, ischemic stroke and hemorrhagic stroke.
3.2. Changes in risk factors, potential impact fraction and burden
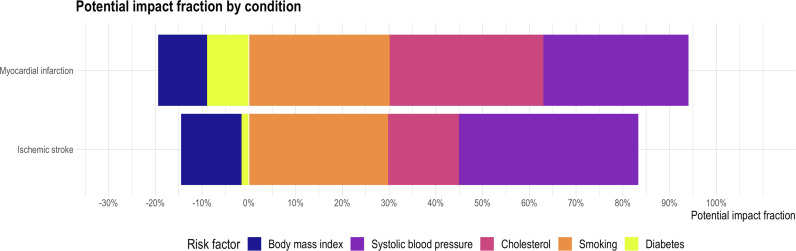
Over the 25 years, age- and sex-standardized risk factor levels reduced for systolic blood pressure (140 [139 to 140] to 129 [129 to 130] mmHg), smoking prevalence (58 [54 to 63] to 25 [24 to 26] %) and cholesterol concentrations (6.4 [6.2 to 6.6] to 5.1 [5.0 to 5.3] mmol/L). Body mass index (27.2 [27.0 to 27.4) to 28.1 [28.0 to 28.2] kg/m2) and diabetes prevalence (4 [3 to 5] to 9 [8 to 9] %) increased. The trends remained consistent across the majority of age and sex strata(Supplementary figure3). Changes in risk factor prevalence accounted for a 74 [57-91] % and 68 [55-83] % age- and sex-standardized reduction in myocardial infarction and ischemic stroke. This was predominantly driven by reduction in systolic blood pressure for ischemic stroke and in cholesterol and smoking rates for myocardial infarction (Figure 2a). In contrast, we observed a 20 [16 to 26] % and 15 [11 to 21] % increase in myocardial infarction and ischemic stroke incidence attributable to changes in body-mass index and diabetes prevalence (Supplementary table 5) Differences were observed in the potential impact fractions according to age and sex. Reductions in smoking rates and increase in body-mass index had the largest impact on younger people whilst increases in diabetes prevalence predominantly impacted the elderly (Supplementary figure 4and table 6).
Fig. 2a.
Stack barplot showing potential impact fraction for myocardial infarction and ischemic stroke by risk factor change from 1990 to 2014.
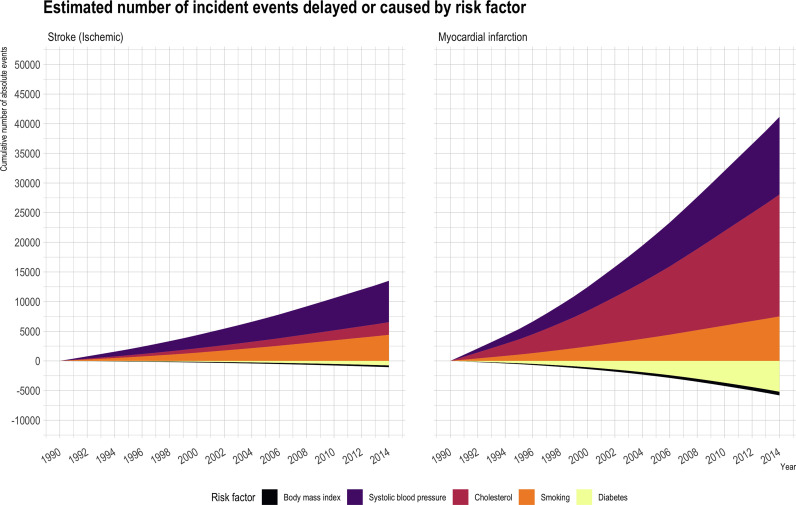
Changes in risk factors over 25 years had a larger impact on reducing burden for incident myocardial infarction (net reduction in events 34,762 [23,412 to 43,727]) than for ischemic stroke (13,247 [9,390 to 16,938])(Figure 2b, Supplementary table 7). For myocardial infarction, a reduction in smoking rates prevented 9,362 [7,811 to 11,046] events, but the increase in diabetes prevalence contributed to 7,544 [4,769 to 10,377] additional events.
Fig. 2b.
Stack plot showing absolute number of index myocardial infarction and ischemic stroke events delayed / prevented or caused by change in risk factor level.
3.3. Outcomes following incident cases
Crude 30-day and 3-year case-fatality rates, including index deaths, fell for myocardial infarction and ischemic or hemorrhagic stroke(Table 2) with similar trends observed on restricting analyses to index non-fatal cases(Supplementary table8).
Table 2.
Fatal and non-fatal outcomes in patients with fatal and non-fatal index myocardial infarction and stroke stratified by 5- calendar year groups.
| Outcome type | Index Condition | Outcome time | 1990 to 1994 | 1995 to 1999 | 2000 to 2004 | 2005 to 2009 | 2010 to 2014 |
|---|---|---|---|---|---|---|---|
| Myocardialinfarction | Myocardial infarction | 30 days | 1,333 (1.5) | 1,486 (2.1) | 1,560 (2.7) | 1,501 (3.1) | 2,976 (5.5) |
| One year | 4,581 (5.1) | 3,892 (5.5) | 3,816 (6.6) | 3,535 (7.2) | 5,550 (10.2) | ||
| Three years | 7,086 (7.9) | 5,453 (7.8) | 5,163 (8.9) | 4,860 (9.9) | 7,337 (13.5) | ||
| Stroke | 30 days | 201 (0.4) | 236 (0.4) | 188 (0.3) | 191 (0.4) | 151 (0.3) | |
| One year | 920 (1.7) | 802 (1.3) | 684 (1.2) | 645 (1.3) | 600 (1.2) | ||
| Three years | 1,710 (3.2) | 1,513 (2.5) | 1,268 (2.3) | 1,190 (2.4) | 1,175 (2.4) | ||
| Stroke | Myocardial infarction | 30 days | 76 (0.1) | 234 (0.3) | 206 (0.4) | 199 (0.4) | 209 (0.4) |
| One year | 295 (0.3) | 791 (1.1) | 741 (1.3) | 698 (1.4) | 780 (1.4) | ||
| Three years | 699 (0.8) | 1,515 (2.2) | 1,320 (2.3) | 1,254 (2.6) | 1,399 (2.6) | ||
| Stroke | 30 days | 928 (1.7) | 1,152 (1.9) | 1,005 (1.8) | 1,037 (2.1) | 1,264 (2.6) | |
| One year | 5,249 (9.7) | 5,214 (8.8) | 4,232 (7.7) | 3,774 (7.7) | 3,453 (7.1) | ||
| Three years | 7,831 (14.4) | 7,618 (12.8) | 6,159 (11.2) | 5,405 (11.0) | 5,048 (10.4) | ||
| Heart failure | Myocardial infarction | 30 days | 1,223 (1.4) | 1,326 (1.9) | 1,301 (2.2) | 1,284 (2.6) | 1,353 (2.5) |
| One year | 4,895 (5.5) | 4,671 (6.7) | 4,274 (7.4) | 3,479 (7.1) | 3,665 (6.8) | ||
| Three years | 7,267 (8.1) | 6,694 (9.5) | 5,837 (10.1) | 4,847 (9.9) | 5,105 (9.4) | ||
| Stroke | 30 days | 200 (0.4) | 196 (0.3) | 165 (0.3) | 160 (0.3) | 133 (0.3) | |
| One year | 1,206 (2.2) | 1,225 (2.1) | 978 (1.8) | 852 (1.7) | 836 (1.7) | ||
| Three years | 2,337 (4.3) | 2,384 (4.0) | 1,899 (3.5) | 1,659 (3.4) | 1,693 (3.5) | ||
| Bleeding | Myocardial infarction | 30 days | 142 (0.2) | 192 (0.3) | 297 (0.5) | 443 (0.9) | 538 (1.0) |
| One year | 854 (1.0) | 897 (1.3) | 1,222 (2.1) | 1,457 (3.0) | 1,804 (3.3) | ||
| Three years | 1,877 (2.1) | 1,916 (2.7) | 2,226 (3.8) | 2,489 (5.1) | 2,997 (5.5) | ||
| Stroke | 30 days | 529 (1.0) | 591 (1.0) | 585 (1.1) | 495 (1.0) | 479 (1.0) | |
| One year | 2,020 (3.7) | 1,775 (3.0) | 1,720 (3.1) | 1,546 (3.1) | 1,466 (3.0) | ||
| Three years | 3,406 (6.3) | 2,981 (5.0) | 2,939 (5.4) | 2,699 (5.5) | 2,620 (5.4) | ||
| Death | Myocardial infarction | 30 days | 39,557 (44.1) | 27,735 (39.5) | 19,711 (34.0) | 13,752 (28.0) | 10,044 (18.5) |
| One year | 45,899 (51.2) | 32,732 (46.6) | 24,544 (42.4) | 18,204 (37.1) | 14,528 (26.8) | ||
| Three years | 52,106 (58.1) | 37,567 (53.5) | 28,959 (50.0) | 22,229 (45.3) | 19,427 (35.9) | ||
| Stroke | 30 days | 15,162 (28.0) | 17,961 (30.2) | 14,734 (26.9) | 11,370 (23.2) | 9,341 (19.3) | |
| One year | 24,665 (45.5) | 26,722 (45.0) | 22,784 (41.5) | 18,223 (37.1) | 15,639 (32.3) | ||
| Three years | 32,049 (59.1) | 33,675 (56.7) | 28,986 (52.9) | 23,708 (48.3) | 21,205 (43.9) |
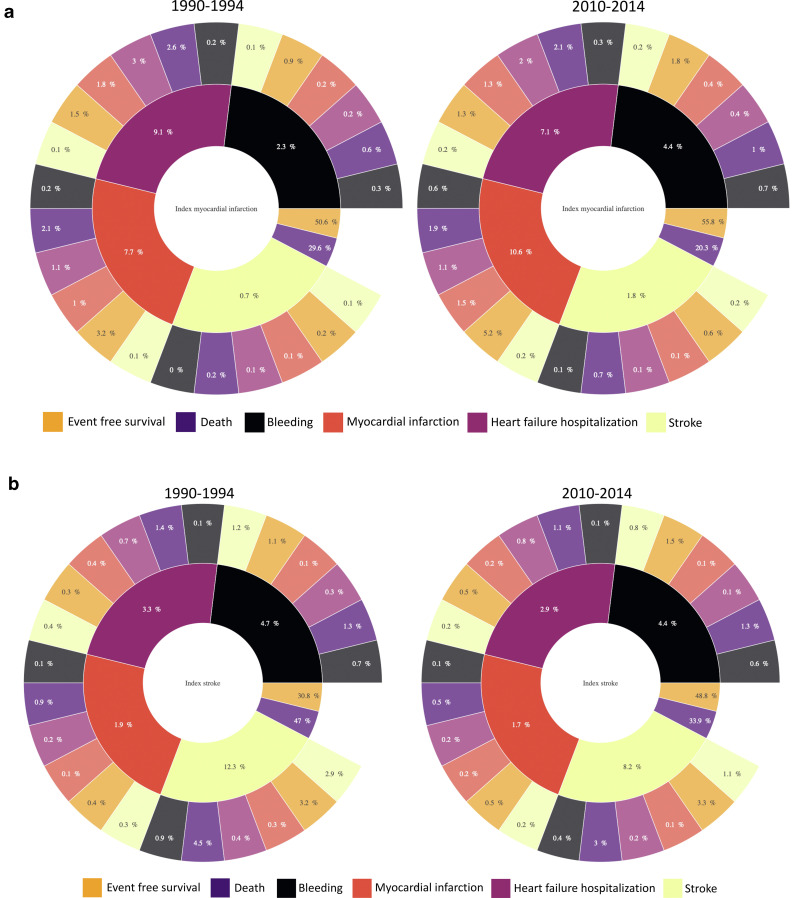
Following myocardial infarction and stroke, the risk of death with no interceding event decreased from 30% to 20% and from 47% to 34% respectively. Risk of any subsequent non-fatal event increased for myocardial infarction (from 20% to 24%) but decreased for stroke (from 22% to 17%). Following myocardial infarction, there was an increase in recurrent myocardial infarction (from 7.7% to 10.6%) and bleeding (from 2.3% to 4.4%) although heart failure hospitalisations fell (from 9.1% to 7.1%). Following stroke, the risk of recurrent stroke was reduced (from 12.3% to 8.2%) and bleeding remained unchanged (from 4.7% to 4.4%) (Figure 3). Risks following the index event differed when evaluated by age, sex, deprivation and comorbidity. An online interactive web application reports the standardized risk of fatal and non-fatal eventsat 3-years for index myocardial infarction and stroke by period and stratified by age, sex, deprivation, and comorbidity (https://ihwph-hehta.shinyapps.io/614967/).
Fig. 3.
Population risks from multistate models – unscaled sunburst plots showing stratum standardized risks for the population for fatal and non-fatal sequalae following index non-fatal myocardial infarction (A) and stroke (B). Note: A web application has been created (https://ihwph-hehta.shinyapps.io/614967/) to illustrate the predicted risks for up-to three levels for fatal or non-fatal subsequent events and four levels for subsequent fatal events. The web application also provides conditional probabilities of risks stratified by age, sex, deprivation, presence or absence of comorbidity and cohort period. An adjunct explanatory document has also been submitted to summarize how to use the web-application. On publication, the web application will be updated with the explanation.
4. Discussion
There have been substantial changes in the epidemiology of myocardial infarction and stroke over the last 25 years. The incidence of myocardial infarction and ischemic stroke has reduced 3- to 4-fold with differences in the age-standardized incidence narrowing for both men and women. We estimate that over two-thirds of these reductions can be attributed to major changes in population risk factors with substantial falls in systolic blood pressure, cholesterol concentrations and smoking rates albeit attenuated by increases in body-mass index and diabetes prevalence. Outcomes following myocardial infarction and stroke have also changed substantially. Death following the index event has decreased for both myocardial infarction and stroke, but absolute rates remain high particularly for stroke. Finally, the risk of subsequent non-fatal clinical events is diverging with rising recurrent events following myocardial infarction and falling following stroke.
The trends in myocardial infarction and stroke incidence reported here are consistent with many previous studies across industrialized countries over the last three decades. Whilst these prior studies have predominantly focused on trends in the incidence of coronary deaths[4], [5], [6], [7], [8], [9] or non-fatal stroke,[20]we observe consistent reductions in the incidence of both fatal and non-fatal myocardial infarction and stroke. Ford et al observed a 50% reduction in coronary deaths from 1980 to 2000 in the United States.[8] Across a similar time period, the Oxford Vascular study, with robust case ascertainment, reported a 40% reduction in non-fatal stroke.[37] In our study, the contemporaneous reductions in fatal and non-fatal myocardial infarction and ischemic stroke were even greater. Importantly, we now show that the incidence of both conditions has continued to decline in the decade that followed and the differences in the incidence narrowing.
Our analysis also showed a trend towards a reduction in social inequality. The proportion of patients with incident myocardial infarction and stroke has steadily decreased (from 28% to 25% and 27% to 24% respectively) in the most deprived group and increased (from 12% to 15% and 13% to 16%) in the least deprived group. Across the United Kingdom, McCartney et al showed that the most deprived group experienced the highest absolute reduction in incident coronary mortality but on the relative scale the rate of reductions are higher for the least deprived groups.[38]
In our study, over two-thirds of the reduction in the incidence of myocardial infarction and stroke can be attributed to changes in risk factor prevalence over 25 years. We demonstrated considerable reductions in systolic blood pressure, cholesterol and smoking, similar to changes observed in other industrialized countries.[39,40] For reductions in incident myocardial infarction, changes in systolic blood pressure, cholesterol and smoking rates contributed equally, whereas change in systolic blood pressure was the major determinant of the reduction in incident stroke. Increases in the screening and treatment of hypertension and dyslipidaemia, together with the use of more potent pharmacotherapies, alongside transformative public health efforts, such as smoking bans in public places, are likely to account for a large part of the reductions observed in our study.[39,[41], [42], [43], [44]] Whilst smoking rates fell across age groups, the greatest reductions were observed in younger persons, particularly women. Smoking increases the risk of myocardial infarction 6-fold in women, compared to 3-fold in men.[14] Stronger associations coupled with the greatest temporal reduction, made smoking the single most important factor associated with the reduction in myocardial infarctionand stroke in young women.
Whilst the majority of risk factor changes have been favorable, two exceptions are noteworthy and concerning. Increases in body-mass index and a doubling in the prevalence of diabetes has contributed considerably to incident myocardial infarction and stroke, attenuating the gains observed from better cholesterol and blood pressure control and reduced smoking rates. In our analysis, body-mass index increased in younger persons, but was unchanged in the elderly, and this contributed to an estimated increase in incident stroke and myocardial infarction by a third and quarter respectively. Whilst the prevalence of diabetes doubled, increases were more marked in the elderly, and given the stronger association between diabetes and coronary heart disease, this contributed to a 20% increase in incident myocardial infarction, with little impact on incident stroke. Overall, we estimate that across all age groups in the population, the increasing prevalence of diabetes contributed to as many incident myocardial infarctions as were prevented by the reduction in smoking. Public health efforts now need to urgently focus on managing obesity and diabetes to further curb cardiovascular disease.[45,46]
In parallel to these major changes in cardiovascular risk factors and the incidence of myocardial infarction and stroke, our analysis also demonstrate important changes in morbidity and mortality in those who survive the index event. Across the 25-year period,the case-fatality rate declined from approximately 1 in 3 to 1 in 5 following myocardial infarction, and from 1 in 2 to 1 in 3 following stroke. Improving survival for both these conditions likely reflects improvements in secondary prevention[47] and antithrombotic[48]pharmacotherapy, introduction of acute stroke units,[49] and coronary revascularisation strategies.[50]However, as illustrated in our online interactive web application, the absolute risks of death across the population and across age, sex and deprivation strata remain substantially higher for stroke compared to myocardial infarction. In addition to the higher case-fatality rate following stroke, there has been a substantial narrowing in the differences between the incidence of myocardial infarction and stroke since 1990. Indeed, the incidence rates of myocardial infarction and ischemic stroke are now identical in women. As a consequence, stroke now contributes to an increasingly greater burden of acute cardiovascular events and healthcare provision needs to recognize this.
In contrast to the consistent reductions in case fatality for both myocardial infarction and stroke, the risk of non-fatal sequelae is diverging with an increase in recurrent events following myocardial infarction and a decrease following stroke. Following myocardial infarction, the risk of recurrent myocardial infarction increased from 8% to 11% likely reflecting changes in the clinical definition,the introduction of more sensitive troponin assays[51,52] and improving survival from the index event. The observation that subsequent bleeding rates doubled is likely to be a consequence of the increasing use of more potent anti-platelet and anti-thrombotic therapies.[53] The risk of recurrent stroke was reduced without change in bleeding rates, perhaps suggesting the management of other risk factors is responsible for improved outcomes.[15]
There are several potential strengths to our study. First, our approach ensured complete follow-up in those patients who remained resident in Scotland during the study period. Similar approaches have been used to deliver randomized clinical trials[54,55] and cohort studies.[32,56] Second, our population consists of consecutive patients with myocardial infarction or stroke, avoiding selection bias and improving generalizability. Third, national administrative datasets in Scotland have been operational for decades, with mature, high quality and consistent data.[57] Diagnostic coding for both stroke and ischemic heart disease have been validated against case note reviews and audit data showing good accuracy.[58], [59], [60]
Several limitations need to be highlighted. First, when estimating the potential impact fraction, we assume that each risk factor is mutually exclusive.[61] In reality, both myocardial infarction and stroke occur as a consequence of numerous causal risk factors, rather than a single cause.[61] As such the estimates in the reduction in incidence for each individual risk factor is likely to be an over-estimate. Second, we did not consider the effect of lag times between changes in risk factor levels and incident disease in our analysis. The impact of smoking cessation is likely to be immediate, whereas the effects of weight gain and diabetes may not be observed for many years. Third, the population of Scotland is predominantly white, with small numbers of minority ethnic groups thereby precluding stratified analyses by ethnicity. Fourth, our study predominantly focuses on biological and behavioural risk factors to the exclusion of social ones. Finally, other outcomes following myocardial infarction and stroke are important, such as requirements for social and personal care, and these are not captured by our administrative data. Further, research is now needed to evaluate the role social risk factors and its influence on changes in risk factor levels and subsequent incidence of fatal and non-fatal cardiovascular disease.
Our findings have implications for public health policy and healthcare provision. Substantial reductions in the incidence of both myocardial infarction and ischemic stroke can be achieved by addressing biological and behavioural risk factors. These observations have major implications for countries in low- and middle-income settings where rates of hypertension[39] and dyslipidaemia[62] are rising as well as the residual risk from persistent uncontrolled risk factors in high-income countries. Despite the overall gains, we also highlight the increasing influence of obesity and diabetes on acute cardiovascular events, which have implications for all countries given that both risk factors are risingworldwide.[62,63] Finally, differences in the burden of myocardial infarction and stroke are narrowing, particularly in women, and monitoring these trends is essential for the planning of healthcare provision in the decades that follow.
In conclusion, our analysis highlights a considerable decline in incident myocardial infarction and stroke with over two-thirds of the reduction attributable to favorable changes in risk factor profiles, but increasing obesity and diabetes continue to contribute to the clinical burden.Important changes in the risk of subsequent events following index stroke and myocardial infarction have occurred. Whilst initial case-fatality following stroke has reduced considerably, absolute rates remain high.
Contributors: ASVS conceived the study. ASVS and DM designed the study. ASVS, DM, DC, JP, FA and KKL were involved in the analysis of the study. ASVS drafted the first version of the manuscript. All authors provided critical input into the paper.
Declaration of interest: JL has is on the Advisory Board and has received Research Consultancy fees from Novo Nordisk. This study was funded by the British Heart Foundation through an Intermediate Clinical Research Fellowship (FS/19/17/34172) and a Clinical Lecturer Starter Grant from the Academy of Medical Sciences. DAM is supported by a Wellcome Trust Intermediate Clinical Fellowship (201492/Z/16/Z). SVK is funded by a NRS Senior Clinical Fellowship (SCAF/15/02), the Medical Research Council (MC_UU_00022/2 and the Scottish Government Chief Scientist Office (SPHSU17). DC is funded by an unrestricted gift from Baillie Gifford. DEN is supported by the British Heart Foundation (CH/09/002, RG/16/10/32375, RE/18/5/34216) and Wellcome Trust (WT103782AIA). All other authors have no conflicts to declare.
Data sharing: We are unable to share individual patient level data including covariate data but this is available on application to the Information Services Division at Public Health Scotland and subject to approval from the NHS Scotland Public Benefit and Privacy Panel for Health and Social Care. Individual participant level on risk factors across the population surveys are available from the UK data service and accessible via https://www.gov.scot/publications/scottish-health-survey-dataset-information/.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.lanepe.2021.100141.
Appendix. Supplementary materials
References
- 1.Rothwell PM, Coull AJ, Silver LE. Population-based study of event-rate, incidence, case fatality, and mortality for all acute vascular events in all arterial territories (Oxford Vascular Study) Lancet. 2005;366:1773–1783. doi: 10.1016/S0140-6736(05)67702-1. [DOI] [PubMed] [Google Scholar]
- 2.Falkeborn M, Persson I, Terent A, Bergstrom R, Lithell H, Naessen T. Long-term trends in incidence of and mortality from acute myocardial infarction and stroke in women: Analyses of total first events and of deaths in the Uppsala Health Care Region, Sweden. Epidemiology. 1996;7:67–74. doi: 10.1097/00001648-199601000-00012. [DOI] [PubMed] [Google Scholar]
- 3.Hata J, Ninomiya T, Hirakawa Y. Secular trends in cardiovascular disease and its risk factors in Japanese: half-century data from the HisayamaStudy (1961-2009) Circulation. 2013;128:1198–1205. doi: 10.1161/CIRCULATIONAHA.113.002424. [DOI] [PubMed] [Google Scholar]
- 4.Hunink MG, Goldman L, Tosteson AN. The recent decline in mortality from coronary heart disease, 1980-1990.The effect of secular trends in risk factors and treatment. JAMA. 1997;277:535–542. [PubMed] [Google Scholar]
- 5.Goldman L, Cook EF. The decline in ischemic heart disease mortality rates.An analysis of the comparative effects of medical interventions and changes in lifestyle. Ann Intern Med. 1984;101:825–836. doi: 10.7326/0003-4819-101-6-825. [DOI] [PubMed] [Google Scholar]
- 6.Capewell S, Morrison CE, McMurray JJ. Contribution of modern cardiovascular treatment and risk factor changes to the decline in coronary heart disease mortality in Scotland between 1975 and 1994. Heart. 1999;81:380—6.. doi: 10.1136/hrt.81.4.380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Capewell S, Beaglehole R, Seddon M, McMurray J. Explanation for the decline in coronary heart disease mortality rates in Auckland, New Zealand, between 1982 and 1993. Circulation. 2000;102:1511—6. doi: 10.1161/01.cir.102.13.1511. [DOI] [PubMed] [Google Scholar]
- 8.Ford ES, Ajani UA, Croft JB. Explaining the decrease in U.S. deaths from coronary disease, 1980-2000. N Engl J Med. 2007;356:2388–2398. doi: 10.1056/NEJMsa053935. [DOI] [PubMed] [Google Scholar]
- 9.Hotchkiss JW, Davies CA, Dundas R. Explaining trends in Scottish coronary heart disease mortality between 2000 and 2010 using IMPACTSEC model: retrospective analysis using routine data. BMJ. 2014;348:g1088. doi: 10.1136/bmj.g1088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sarti C, Stegmayr B, Tolonen H. Are changes in mortality from stroke caused by changes in stroke event rates or case fatality? Results from the WHO MONICA Project. Stroke. 2003;34:1833–1840. doi: 10.1161/01.STR.0000081224.15480.52. [DOI] [PubMed] [Google Scholar]
- 11.Li L, Scott CA, Rothwell PM. Oxford Vascular S. Trends in Stroke Incidence in High-Income Countries in the 21st Century: Population-Based Study and Systematic Review. Stroke. 2020;51:1372–1380. doi: 10.1161/STROKEAHA.119.028484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Feigin VL, Forouzanfar MH, Krishnamurthi R. Global and regional burden of stroke during 1990-2010: findings from the Global Burden of Disease Study 2010. Lancet. 2014;383:245–254. doi: 10.1016/s0140-6736(13)61953-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Feigin VL, Lawes CM, Bennett DA, Barker-Collo SL, Parag V. Worldwide stroke incidence and early case fatality reported in 56 population-based studies: a systematic review. Lancet Neurol. 2009;8:355–369. doi: 10.1016/S1474-4422(09)70025-0. [DOI] [PubMed] [Google Scholar]
- 14.Yusuf S, Hawken S, Ounpuu S. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364:937—52. doi: 10.1016/S0140-6736(04)17018-9. [DOI] [PubMed] [Google Scholar]
- 15.O'Donnell MJ, Chin SL, Rangarajan S. Global and regional effects of potentially modifiable risk factors associated with acute stroke in 32 countries (INTERSTROKE): a case-control study. Lancet. 2016;388:761–775. doi: 10.1016/S0140-6736(16)30506-2. [DOI] [PubMed] [Google Scholar]
- 16.O'Donnell MJ, Xavier D, Liu L. Risk factors for ischaemic and intracerebral haemorrhagic stroke in 22 countries (the INTERSTROKE study): a case-control study. Lancet. 2010;376:112—23. doi: 10.1016/S0140-6736(10)60834-3. [DOI] [PubMed] [Google Scholar]
- 17.Moran AE, Oliver JT, Mirzaie M. Assessing the Global Burden of Ischemic Heart Disease: Part 1: Methods for a Systematic Review of the Global Epidemiology of Ischemic Heart Disease in 1990 and 2010. Glob Heart. 2012;7:315–329. doi: 10.1016/j.gheart.2012.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yeh RW, Sidney S, Chandra M, Sorel M, Selby JV, Go AS. Population trends in the incidence and outcomes of acute myocardial infarction. N Engl J Med. 2010;362:2155–2165. doi: 10.1056/NEJMoa0908610. [DOI] [PubMed] [Google Scholar]
- 19.Chen J, Normand SL, Wang Y, Drye EE, Schreiner GC, Krumholz HM. Recent declines in hospitalizations for acute myocardial infarction for Medicare fee-for-service beneficiaries: progress and continuing challenges. Circulation. 2010;121:1322–1328. doi: 10.1161/CIRCULATIONAHA.109.862094. [DOI] [PubMed] [Google Scholar]
- 20.Feigin VL, Lawes CM, Bennett DA, Anderson CS. Stroke epidemiology: a review of population-based studies of incidence, prevalence, and case-fatality in the late 20th century. Lancet Neurol. 2003;2:43–53. doi: 10.1016/s1474-4422(03)00266-7. [DOI] [PubMed] [Google Scholar]
- 21.Chung SC, Gedeborg R, Nicholas O. Acute myocardial infarction: a comparison of short-term survival in national outcome registries in Sweden and the UK. Lancet. 2014;383:1305—12. doi: 10.1016/S0140-6736(13)62070-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Global Burden of Disease Stroke Expert G. Methodology of the global and regional burden of stroke study. Neuroepidemiology. 2012;38:30–40. doi: 10.1159/000334744. [DOI] [PubMed] [Google Scholar]
- 23.Roth GA, CO Johnson, Nguyen G. Methods for Estimating the Global Burden of Cerebrovascular Diseases. Neuroepidemiology. 2015;45:146–151. doi: 10.1159/000441083. [DOI] [PubMed] [Google Scholar]
- 24.Myerson M, Coady S, Taylor H, Rosamond WD, Goff DC, Jr., ARIC Investigators Declining severity of myocardial infarction from 1987 to 2002: the Atherosclerosis Risk in Communities (ARIC) Study. Circulation. 2009;119:503–514. doi: 10.1161/CIRCULATIONAHA.107.693879. [DOI] [PubMed] [Google Scholar]
- 25.Brieger D, Fox KA, Fitzgerald G. Predicting freedom from clinical events in non-ST-elevation acute coronary syndromes: the Global Registry of Acute Coronary Events. Heart. 2009;95:888–894. doi: 10.1136/hrt.2008.153387. [DOI] [PubMed] [Google Scholar]
- 26.Johansson S, Rosengren A, Young K, Jennings E. Mortality and morbidity trends after the first year in survivors of acute myocardial infarction: a systematic review. BMC CardiovascDisord. 2017;17:53. doi: 10.1186/s12872-017-0482-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Vora AN, Rao SV. Temporal Trends in Bleeding among Acute Coronary Syndrome Patients: Is It Going Up or Down? Does It Matter? Cardiology. 2015;132:159–162. doi: 10.1159/000434641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wellings J, Kostis JB, Sargsyan D, Cabrera J, Kostis WJ. Myocardial Infarction Data Acquisition System Study G. Risk Factors and Trends in Incidence of Heart Failure Following Acute Myocardial Infarction. Am J Cardiol. 2018;122:1–5. doi: 10.1016/j.amjcard.2018.03.005. [DOI] [PubMed] [Google Scholar]
- 29.Goldberg RJ, Spencer FA, Yarzebski J. A 25-year perspective into the changing landscape of patients hospitalized with acute myocardial infarction (the Worcester Heart Attack Study) Am J Cardiol. 2004;94:1373–1378. doi: 10.1016/j.amjcard.2004.07.142. [DOI] [PubMed] [Google Scholar]
- 30.Ogren J, Irewall AL, Soderstrom L, Mooe T. Serious hemorrhages after ischemic stroke or TIA - Incidence, mortality, and predictors. PLoS One. 2018;13 doi: 10.1371/journal.pone.0195324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Petty GW, Brown RD, Jr., Whisnant JP, Sicks JD, O'Fallon WM, Wiebers DO. Frequency of major complications of aspirin, warfarin, and intravenous heparin for secondary stroke prevention.A population-based study. Ann Intern Med. 1999;130:14–22. doi: 10.7326/0003-4819-130-1-199901050-00004. [DOI] [PubMed] [Google Scholar]
- 32.Shah ASV, McAllister DA, Gallacher P. Incidence, Microbiology, and Outcomes in Patients Hospitalized With Infective Endocarditis. Circulation. 2020;141:2067–2077. doi: 10.1161/CIRCULATIONAHA.119.044913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Scottish Health Survey. 2020. Accessed 14/12/2020, 2020, at https://www.gov.scot/collections/scottish-health-survey/.
- 34.GBD 2013 Risk Factors Collaborators . Vol. 386. 2015. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks in 188 countries, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013; p. 2287—323. (Lancet). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.European Standard Population. 2020. Accessed 23/12/2020, 2020, at https://www.opendata.nhs.scot/dataset/standard-populations/resource/edee9731-daf7-4e0d-b525-e4c1469b8f69.
- 36.Barendregt JJ, Veerman JL. Categorical versus continuous risk factors and the calculation of potential impact fractions. J Epidemiol Community Health. 2010;64:209–212. doi: 10.1136/jech.2009.090274. [DOI] [PubMed] [Google Scholar]
- 37.Rothwell PM, Coull AJ, Giles MF. Change in stroke incidence, mortality, case-fatality, severity, and risk factors in Oxfordshire, UK from 1981 to 2004 (Oxford Vascular Study) Lancet. 2004;363:1925–1933. doi: 10.1016/S0140-6736(04)16405-2. [DOI] [PubMed] [Google Scholar]
- 38.McCartney D, Scarborough P, Webster P, Rayner M. Trends in social inequalities for premature coronary heart disease mortality in Great Britain, 1994-2008: a time trend ecological study. BMJ Open. 2012;2 doi: 10.1136/bmjopen-2011-000737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.NCD Risk Factor Collaboration Worldwide trends in blood pressure from 1975 to 2015: a pooled analysis of 1479 population-based measurement studies with 19.1 million participants. Lancet. 2017;389:37–55. doi: 10.1016/S0140-6736(16)31919-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.NCD Risk Factor Collaboration Repositioning of the global epicentre of non-optimal cholesterol. Nature. 2020;582:73–77. doi: 10.1038/s41586-020-2338-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Williams B, Mancia G, Spiering W. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J. 2018;39:3021–3104. doi: 10.1093/eurheartj/ehy339. [DOI] [PubMed] [Google Scholar]
- 42.Mach F, Baigent C, Catapano AL. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Eur Heart J. 2020;41:111–188. doi: 10.1093/eurheartj/ehz455. [DOI] [PubMed] [Google Scholar]
- 43.Pell JP, Haw S, Cobbe S. Smoke-free legislation and hospitalizations for acute coronary syndrome. N Engl J Med. 2008;359:482–491. doi: 10.1056/NEJMsa0706740. [DOI] [PubMed] [Google Scholar]
- 44.O'Keeffe AG, Nazareth I, Petersen I. Time trends in the prescription of statins for the primary prevention of cardiovascular disease in the United Kingdom: a cohort study using The Health Improvement Network primary care data. ClinEpidemiol. 2016;8:123–132. doi: 10.2147/CLEP.S104258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kumanyika S, Dietz WH. Solving Population-wide Obesity - Progress and Future Prospects. N Engl J Med. 2020;383:2197–2200. doi: 10.1056/NEJMp2029646. [DOI] [PubMed] [Google Scholar]
- 46.Ingelfinger JR, Jarcho JA. Increase in the Incidence of Diabetes and Its Implications. N Engl J Med. 2017;376:1473–1474. doi: 10.1056/NEJMe1616575. [DOI] [PubMed] [Google Scholar]
- 47.Piepoli MF, Hoes AW, Agewall S. 2016 European Guidelines on cardiovascular disease prevention in clinical practice: The Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts)Developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR) Eur Heart J. 2016;37:2315–2381. doi: 10.1093/eurheartj/ehw106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ntaios G, Papavasileiou V, Diener HC, Makaritsis K, Michel P. Nonvitamin-K-antagonist oral anticoagulants in patients with atrial fibrillation and previous stroke or transient ischemic attack: a systematic review and meta-analysis of randomized controlled trials. Stroke. 2012;43:3298–3304. doi: 10.1161/STROKEAHA.112.673558. [DOI] [PubMed] [Google Scholar]
- 49.Langhorne P, Ramachandra S. Stroke Unit Trialists C. Organised inpatient (stroke unit) care for stroke: network meta-analysis. Cochrane Database Syst Rev. 2020;4 doi: 10.1002/14651858.CD000197.pub4. CD000197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Keeley EC, Boura JA, Grines CL. Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review of 23 randomised trials. Lancet. 2003;361:13–20. doi: 10.1016/S0140-6736(03)12113-7. [DOI] [PubMed] [Google Scholar]
- 51.Shah AS, McAllister DA, Mills R. Sensitive troponin assay and the classification of myocardial infarction. Am J Med. 2015;128 doi: 10.1016/j.amjmed.2014.10.056. 493-501.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Mills NL, Churchhouse AM, Lee KK. Implementation of a sensitive troponin I assay and risk of recurrent myocardial infarction and death in patients with suspected acute coronary syndrome. Jama. 2011;305:1210–1216. doi: 10.1001/jama.2011.338. [DOI] [PubMed] [Google Scholar]
- 53.Simonsson M, Wallentin L, Alfredsson J. Temporal trends in bleeding events in acute myocardial infarction: insights from the SWEDEHEART registry. Eur Heart J. 2020;41:833–843. doi: 10.1093/eurheartj/ehz593. [DOI] [PubMed] [Google Scholar]
- 54.Scot-Heart investigators Coronary CT Angiography and 5-Year Risk of Myocardial Infarction. N Engl J Med. 2018;379:924—33. doi: 10.1056/NEJMoa1805971. [DOI] [PubMed] [Google Scholar]
- 55.Shah ASV, Anand A, Strachan FE. High-sensitivity troponin in the evaluation of patients with suspected acute coronary syndrome: a stepped-wedge, cluster-randomised controlled trial. Lancet. 2018;392:919—28. doi: 10.1016/S0140-6736(18)31923-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Shah ASV, Sandoval Y, Noaman A. Patient selection for high sensitivity cardiac troponin testing and diagnosis of myocardial infarction: prospective cohort study. Bmj. 2017;359:j4788. doi: 10.1136/bmj.j4788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Mackay DF, Russell ER, Stewart K, MacLean JA, Pell JP, Stewart W. Neurodegenerative Disease Mortality among Former Professional Soccer Players. N Engl J Med. 2019;381:1801–1808. doi: 10.1056/NEJMoa1908483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.The West of Scotland Coronary Prevention Study Group Computerised record linkage: compared with traditional patient follow-up methods in clinical trials and illustrated in a prospective epidemiological study. J ClinEpidemiol. 1995;48:1441–1452. doi: 10.1016/0895-4356(95)00530-7. [DOI] [PubMed] [Google Scholar]
- 59.Turner M, Barber M, Dodds H. Agreement between routine electronic hospital discharge and Scottish Stroke Care Audit (SSCA) data in identifying stroke in the Scottish population. BMC Health Serv Res. 2015;15:583. doi: 10.1186/s12913-015-1244-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Soo M, Robertson LM, Ali T. Approaches to ascertaining comorbidity information: validation of routine hospital episode data with clinician-based case note review. BMC Res Notes. 2014;7:253. doi: 10.1186/1756-0500-7-253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Rowe AK, Powell KE, Flanders WD. Why population attributable fractions can sum to more than one. Am J Prev Med. 2004;26:243–249. doi: 10.1016/j.amepre.2003.12.007. [DOI] [PubMed] [Google Scholar]
- 62.NCD Risk Factor Collaboration Worldwide trends in diabetes since 1980: a pooled analysis of 751 population-based studies with 4.4 million participants. Lancet. 2016;387:1513–1530. doi: 10.1016/S0140-6736(16)00618-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.NCD Risk Factor Collaboration Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128.9 million children, adolescents, and adults. Lancet. 2017;390:2627–2642. doi: 10.1016/S0140-6736(17)32129-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.