Abstract
Objective
We report longitudinal data from 144 type III SMA pediatric and adult patients treated with nusinersen as part of an international effort.
Methods
Patients were assessed using Hammersmith Functional Motor Scale Expanded (HFMSE), Revised Upper Limb Module (RULM), and 6‐Minute Walk Test (6MWT) with a mean follow‐up of 1.83 years after nusinersen treatment.
Results
Over 75% of the 144 patients had a 12‐month follow‐up. There was an increase in the mean scores from baseline to 12 months on both HFMSE (1.18 points, p = 0.004) and RULM scores (0.58 points, p = 0.014) but not on the 6MWT (mean difference = 6.65 m, p = 0.33).
When the 12‐month HFMSE changes in the treated cohort were compared to an external cohort of untreated patients, in all untreated patients older than 7 years, the mean changes were always negative, while always positive in the treated ones. To reduce a selection bias, we also used a multivariable analysis. On the HFMSE scale, age, gender, baseline value, and functional status contributed significantly to the changes, while the number of SMN2 copies did not contribute. The effect of these variables was less obvious on the RULM and 6MWT.
Interpretation
Our results expand the available data on the effect of Nusinersen on type III patients, so far mostly limited to data from adult type III patients.
Introduction
Spinal muscular atrophy (SMA) is an autosomal recessive disorder caused by mutations in the survival motor neuron 1 gene (SMN1), characterized by the degeneration of the α‐motor neurons of the anterior horn cells of the spinal cord resulting in progressive muscle weakness. 1 Classically, three types with pediatric onset (SMA I–III) and one adult type have been identified (SMA IV) based on the age of symptoms onset and maximum motor achievement. 2 Type III SMA, or Kugelberg–Welander disease, is the mildest form and is characterized by clinical heterogeneity. Clinical presentation generally occurs between 18 months and 18 years when patients have reached all the early motor development milestones, including walking. 3 A proportion of them loses this ability, while others will maintain it indefinitely, showing only minimal muscle weakness. Type III patients are further subdivided according to the onset of clinical signs in types IIIA and IIIB including based on the onset of symptoms before and after 3 years of age. 4
Nusinersen, an antisense oligonucleotide administered intrathecally, targets pre‐mRNA splicing of the SMN2 gene, increasing inclusion of exon 7 in the SMN2 mRNA splicing and the amount of functional SMN protein. 5 It was approved by the United States Food and Drug Administration (FDA) in 2016 and by the European Medicines Agency (EMA) in 2017, based on two pivotal clinical trials demonstrating the effectiveness in different types of SMA 6 , 7 in infants and young children. While the early real‐world data have mainly focused on type I patients, 8 , 9 , 10 , 11 and more recent studies have reported data in adults, 12 , 13 , 14 , 15 , 16 , 17 , 18 less has been reported in pediatric patients or, more generally, to cover the spectrum of treated younger and older type III patients who were also not included in the pivotal trials. 19 Furthermore, as there is reported evidence of the variability of the progression of type III in relation to a number of variables, such as age and functional status, 20 , 21 , 22 the interpretation of the limited real‐world data available is also affected by the lack of comparison with reference data from untreated patients.
The aim of this study was to report real‐world data in a large cohort of ambulant and non‐ambulant type III patients treated with nusinersen in order to establish 12‐month changes and the possible effect of different variables, such as baseline values, age, and others on the magnitude of changes. For the measures for which reference data were available, we also wished to correlate the changes observed in the treated cohort to recent longitudinal data collected in untreated patients.
Methods
The data used in this study were collected from the International SMA Registry (United States, Italy, and United Kingdom) 23 or, in a few cases from datasets belonging to the same ISMAR centers but collected before June 2018. The study was approved by the institutional review board (ethics committee) in each center (No. 0030504/18). Written informed consent was obtained from all participants (or guardians of participants) in the study.
All patients with a genetically confirmed diagnosis of SMA and a clinically confirmed diagnosis of type III SMA and on treatment with nusinersen for at least 12 months were included in the study. Type III SMA was subdivided into IIIA or IIIB according to the age at symptom onset (before or after 3 years) 4 In accordance with the clinical routine of each center, patients were assessed using the Hammersmith Functional Motor Scale Expanded (HFMSE), Revised Upper Limb Module (RULM), and 6‐Minute Walk Test (6MWT) by trained clinical evaluators.
HFMSE
The scale consists of 33 items, investigating the child’s ability to perform various activities. 24 Each item is scored on a 3‐point scoring system, with a score of 2 for “performs without modification,” 1 “performs with modification/ adaptation,” and 0 for “unable to perform.” The total score can range from 0, if all the activities are failed, to 66, if all the activities are achieved.
RULM
The scale consists of an entry item to establish functional levels and 19 items covering distal to proximal movements of the upper extremities. 25 Of the 19 items, 18 are scored on a 3‐point scoring system and 1 item is scored on a 2‐point scoring system. The total score ranges from 0, if all the items cannot be performed, to 37, if all the activities are achieved fully without any compensation.
6MWT
The 6MWT measures the maximum distance a person can walk in 6 min over a 25‐m linear course. It has been shown to be a valid and reliable assessment of exercise capacity and functional walking ability in SMA patients. 26 Distance walked over the entire 6‐minute time period, distance covered each minute, and the time to complete each 25‐m interval was recorded. Clinical evaluators used common procedure manuals and were trained at in‐person meetings. Details of the training and reliability sessions have already been reported. 22 , 27 , 28
Each center had a different schedule of assessments, according to their routine clinical practice but it was agreed that all patients should have at least one assessment after 12 months from the first dose of nusinersen, between the 6th and 7th dose of nusinersen.
Statistical analysis
Demographic and clinical characteristics were summarized using frequencies (percentage) for categorical variables and mean (standard deviation (SD)) or median (1st–3rd quartile) for continuous variables, unless otherwise stated.
In this manuscript, we present two different analyses. First, we analyzed all the patients with a follow‐up at 1 year of treatment in order to evaluate the 12‐month changes in the functional measures. Comparisons of measurements from baseline to 12‐months were performed using the estimates and 95% confidence intervals (CI) of pre–post‐differences and the Wilcoxon signed‐rank test. Twelve‐month changes were also analyzed subdividing the cohort according to the functional status (sitters vs. walkers), SMA type III subtypes (IIIA and IIIB), and according to the age (pediatric (<18 years) vs. adults). Following the previous literature, we also reported details on 12‐month trajectories with changes grouped as stable (±2 points), improved (>+2) or declined (>−2). 22
As a number of patients failed the 12‐month assessment because of restricted access to hospitals during the COVID‐19 pandemic or for other reasons, and since no imputation was performed on missing data, we also added a second analysis using a mixed model to estimate the changes for the whole type III population in order to exclude possible selection bias. The model was set up with measurements at baseline, age, sex, time, disease duration, SMN2 copy number, disease onset, and SMA function as fixed effects and patient as a random effect. To make inferences about mean slopes according to the age of onset, the model was expanded by including appropriate main effect and interaction terms in the model.
Results
One‐hundred forty‐four SMA type III patients (age range: 30 months–68.27 years) were enrolled in the study. Of the 144, 139 had an SMN1 homozygous deletion of exon 7/8, 4 had an SMN1 compound heterozygous deletion and a point mutation, and 1 had a compound heterozygous or homozygous point mutation in SMN1.
All patients were treatment naïve at baseline. The mean duration of follow‐up was 1.83 (±0.61) years. Table 1 describes the baseline characteristics and demographics of the cohort.
Table 1.
Baseline characteristics of the SMA type III‐treated patients according to the disease onset.
| All | IIIA | IIIB | |
|---|---|---|---|
| N | 144 | 74 | 70 |
| Sex, n (%) | |||
| Male | 84 (58.33) | 40 (54.05) | 44 (62.86) |
| Female | 60 (41.67) | 34 (45.95) | 26 (37.14) |
| Age at baseline (years), median (1st–3rd quartile) | 16.42 (9.14–35.69) | 12.60 (5.5–26.27) | 23.22 (13.07–43.94) |
| Age < 18 years, n (%) | 77 (53.47) | 51 (68.92) | 26 (37.14) |
| Median age in pediatric population (1st–3rd quartile), years | 9.50 (5.50–13.43) | 8.01 (4.40–13.11) | 11.74 (9.24–15.08) |
| Age ≥ 18 years, n (%) | 67 (46.53) | 23 (31.08) | 44 (62.86) |
| Median age in adult population (1st–3rd quartile), years | 36.60 (26.27–47.08) | 35.40 (27.10–39.00) | 38.84 (25.51–49.35) |
| Disease duration (years), median (1st–3rd quartile) | 12.10 (4.4–28.89) | 10.41 (3.51–25.11) | 13.33 (4.66–31.43) |
| SMN2 copy number, n (%) | |||
| 1 | 0 (0.00) | 0 (0.00) | 0 (0.00) |
| 2 | 11 (7.64) | 4 (5.41) | 7 (10.00) |
| 3 | 56 (38.88) | 40 (54.05) | 16 (22.85) |
| 4 | 14 (9.72) | 8 (10.81) | 6 (8.57) |
| 4+ | 29 (20.14) | 6 (8.11) | 23 (32.86) |
| Unknown | 34 (23.61) | 16 (21.62) | 18 (25.71) |
| SMA function, n (%) | |||
| Non‐sitter | 3 (2.08) | 3 (4.05) | 0 (0.00) |
| Sitter | 62 (43.06) | 40 (54.05) | 22 (31.43) |
| Walker | 79 (54.86) | 31 (41.89) | 48 (68.57) |
| Baseline HFMSE score, median (1st–3rd quartile) |
41 (23–54) N = 130 |
32.50 (15–50) N = 66 |
48.5 (28.0–58.5) N = 64 |
| Baseline RULM score, median (1st–3rd quartile) |
31 (24–37) N = 116 |
27 (22–32) N = 56 |
35.5 (29.5–37.0) N = 60 |
| Baseline 6MWT meter, median (1st–3rd quartile) |
321.5 (166–425) N = 62 |
283 (107–397) N = 23 |
356 (236–434) N = 39 |
| Follow‐up (years), mean (SD) | 1.83 (0.61) | 1.91 (0.63) | 1.75 (0.58) |
| No of visits, median (range) | 5 (2–11) | 6 (2–11) | 5 (3–11) |
No serious adverse events (S‐AE) were reported at the time of data collection, most frequent AE were all related to the procedure (headache, nausea, back pain), and have not been reported consistently by all patients.
One hundred and four of the 144 had 12‐month assessments on at least one measure and were analyzed for the primary analysis on the 12‐month changes. Other 26 patients had at least 6‐months follow‐up and were retained for the mixed model analysis. In these cases, clinical follow‐up visits were missed because of restrictions to the access to clinics related to the COVID‐19 pandemic. A flow chart describing patient selection from the whole cohort is available in Figure 1.
Figure 1.
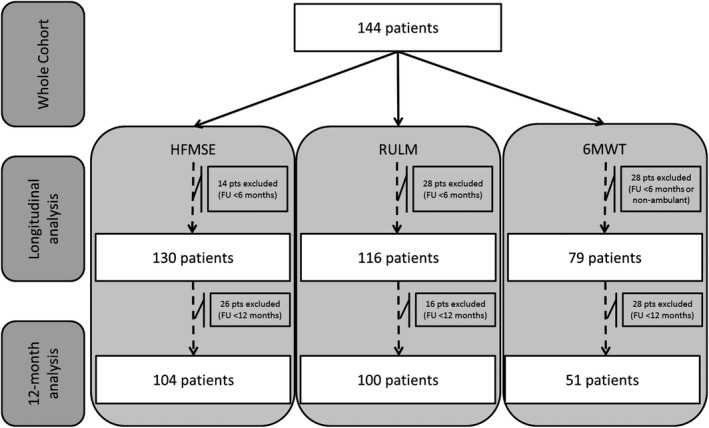
Flow chart of patient selection.
HFMSE
12‐month changes
Complete data both at baseline and at 12 months were available in 104/144 (72.22%) patients for the HFMSE.
In the 104 patients with HFMSE scores available at baseline and after 12 months/6 infusions (median days from baseline = 359.5 (range 286–436 days)), the HFMSE scores significantly increased between the two assessments (mean difference = 1.18 (95%CI: 0.37–1.99), p = 0.004).
The mean 12‐month increase in the HFMSE scores was significant in both sitters and walkers. A sensitivity analysis was performed excluding the three non‐sitter patients and the results did not change.
When subdivided into IIIA and IIIB subtypes, the increase in scores was significant in IIIB patients and showed only a trend of significance in IIIA. Details of the analysis are reported in Table 2 and Table S1.
Table 2.
Changes in HFMSE, 6‐minute walk test, and RULM score (12 months vs. baseline) in the overall SMA III population, according to the patient onset, ambulatory status, and age groups.
| N | Baseline Mean Score (95%CI) | 12‐month Mean Score (95%CI) | Mean difference (95%CI) | p‐value | |
|---|---|---|---|---|---|
| HFMSE score | |||||
| All | 104 | 37.56 (36.98–38.13) | 38.74 (38.17–39.31) | 1.18 (0.37–1.99) | 0.004 |
| Type IIIA | 49 | 33.55 (32.49–34.61) | 34.57 (33.51–35.63) | 1.02 (−0.47–2.51) | 0.179 |
| Type IIIB | 55 | 41.13 (40.56–41.69) | 42.45 (41.89–43.02) | 1.33 (0.53–2.12) | 0.001 |
| Non‐ambulant | 43 | 19.79 (18.82–20.76) | 21.27 (20.27–22.28) | 1.48 (0.09–2.88) | 0.038 |
| Ambulant | 60 | 50.55 (49.85–51.25) | 51.61 (50.92–52.30) | 1.06 (0.08–2.04) | 0.034 |
| Pediatric | 59 | 43.05 (42.22–43.88) | 44.58 (43.73–45.44) | 1.53 (0.34–2.72) | 0.0123 |
| Adults | 45 | 30.75 (29.97–31.53) | 31.54 (30.79–32.30) | 0.79 (−0.29–1.87) | 0.148 |
| RULM score | |||||
| All | 100 | 29.33 (29.00–29.66) | 29.91 (29.58–30.24) | 0.58 (0.12–1.04) | 0.014 |
| Type IIIA | 44 | 26.52 (26.02–27.02) | 27.77 (27.27–28.27) | 1.25 (0.54–1.96) | 0.001 |
| Type IIIB | 56 | 31.53 (31.12–31.95) | 31.59 (31.17–32.01) | 0.05 (−0.53–0.64) | 0.857 |
| Non‐ambulant | 46 | 24.65 (24.16–25.15) | 25.61 (25.10–26.12) | 0.95 (0.24–1.66) | 0.0009 |
| Ambulant | 53 | 33.98 (33.54–34.42) | 34.30 (33.86–34.73) | 0.32 (−0.30–0.94) | 0.313 |
| Pediatric | 45 | 31.90 (31.40–32.39) | 33.15 (32.65–33.66) | 1.26 (0.55–1.97) | 0.0007 |
| Adults | 55 | 27.31 (26.91–27.71) | 27.38 (26.99–27.78) | 0.07 (−0.48–0.63) | 0.792 |
| RULM score (baseline RULM score <37) | |||||
| All | 73 | 26.49 (26.06–26.93) | 27.38 (26.95–27.82) | 0.89 (0.28–1.50) | 0.005 |
| Type IIIA | 39 | 25.17 (24.63–25.73) | 26.61 (26.06–27.17) | 1.44 (0.65–2.22) | 0.0005 |
| Type IIIB | 34 | 28.00 (27.33–28.67) | 28.26 (27.59–28.94) | 0.26 (−0.68–1.22) | 0.581 |
| Non‐ambulant | 43 | 23.62 (23.12–24.13) | 24.80 (24.28–25.33) | 1.18 (0.45–1.91) | 0.002 |
| Ambulant | 29 | 31.61 (30.80–32.41) | 32.21 (31.43–32.99) | 0.60 (−0.52–1.72) | 0.289 |
| Pediatric | 31 | 29.52 (28.82–30.22) | 31.41 (30.68–32.13) | 1.88 (0.87–2.90) | 0.0004 |
| Adults | 42 | 24.38 (23.87–24.88) | 24.62 (24.12–25.11) | 0.24 (−0.47–0.94) | 0.505 |
| 6MWT score | |||||
| All | 51 | 321.00 (311.29–330.71) | 327.65 (317.94–337.35) | 6.65 (−7.08–20.37) | 0.339 |
| Type IIIA | 18 | 279.89 (264.90–294.88) | 269.83 (254.84–284.82) | −10.06 (−31.25–11.14) | 0.341 |
| Type IIIB | 33 | 343.42 (330.98–355.87) | 359.18 (346.74–371.63) | 15.76 (−1.84–33.36) | 0.078 |
| Pediatric | 34 | 319.87 (306.92–332.82) | 330.20 (316.85–343.55) | 10.32 (−8.28–28.93) | 0.272 |
| Adults | 17 | 323.03 (308.23–337.83) | 323.55 (309.55–337.55) | 0.52 (−19.85–20.89) | 0.959 |
Dark grey shaded cells: statistical significance.
Details on 12‐month trajectories with changes grouped as stable (±2 points), improved (>+2) or declined (>−2) are reported in Table S2.
Longitudinal data analysis
In a multivariable analysis including 130/144 (90.28%) patients with at least 6‐months follow‐up (median follow‐up of 1.86 years (range 0.5–3.11 years), no significant differences between the different SMA III subtypes (p for interaction between time and SMA type = 0.541) (Fig. 2A,B). Age, SMA functional status, HFMSE at baseline, and SMA III subtype were all factors significantly contributing to the changes, while SMN2 copy was not (Table S3).
Figure 2.
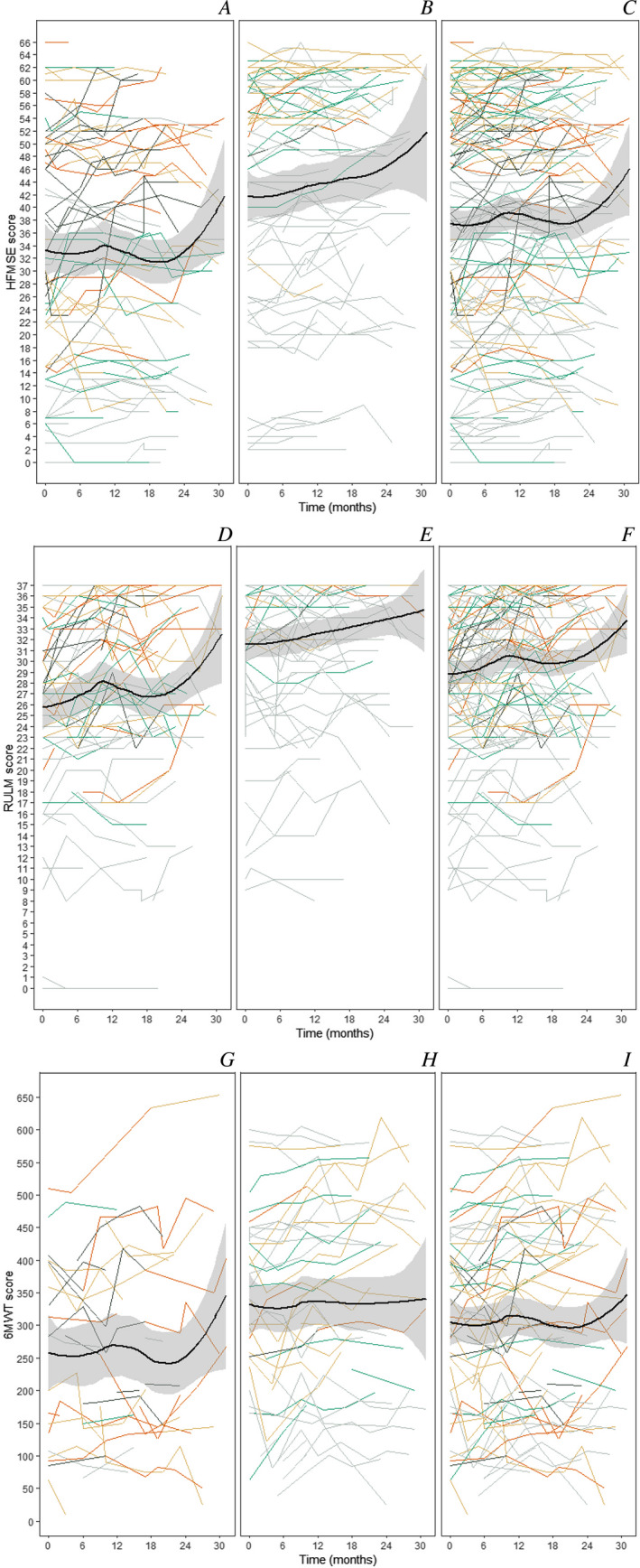
Mean rate of changes in assessments. Panels (A–C): Mean rate of change in HFMSE scores for all type III (C) and subtypes (IIIA: A, IIIB: B). Panels (D–F): Mean rate of change in RULM score for all type III (F) and subtypes (IIIA: D, IIIB: E). Panels (G–I) Mean rate of change in 6MWT for all type III (I) and subtypes (IIIA: G, IIIB: H). Polynomial line (ribbon: 95% CI) describes progression overtime. Color coding for age at baseline: dark grey line: <5 years; orange line: 5–7 years; dark yellow line: 8–14 years; green line: 15–19 years; light grey line: >20 years.
RULM
12‐month changes
Complete data both at baseline and at 12 months were available in 100/144 (69.44%) patients for the RULM.
In the 100 patients with RULM score available after 12 months/6 infusions (median days from baseline = 363.00 (range 286–436 days), RULM scores significantly increased from baseline to 12 months (mean difference = 0.58 (95%CI: 0.12–1.04)). The mean 12‐month RULM increase was significant in sitters but not in walkers. A sensitivity analysis was performed excluding the three non‐sitter patients and the results did not change.
When subdivided into subtypes, the increase was significant in IIIA patients but not in IIIB. Details of the analysis are reported in Table 2 and Table S4.
At 12 months, of the 100 patients analyzed, 8.0% (n = 8) declined more than 2 points, 75.0% (n = 75) remained stable, and 17.0% (n = 17) improved more than 2 points. Details on 12‐month trajectories with changes grouped as stable (±2 points), improved (>+2) or declined (>−2) are reported in Table S2.
In a sensitivity analysis excluding 27 patients with baseline RULM scores equal to 37, the 12‐month changes were slightly larger (0.89 vs. 0.58).
Longitudinal data analysis
In a multivariable analysis including 116/144 (80.55%) patients who had at least 6‐months follow‐up (and a median follow‐up of 1.88 years (range 0.5–3.11 years), there was no significant differences between the different SMA III subtypes (p for interaction between time and SMA type = 0.269) (Fig. 2C,D). Age and RULM at baseline were significantly contributing to the changes, while SMA functional status, RULM at baseline, and SMA III subtype and SMN2 copy were not (Table S5).
6MWT
12‐month changes
Complete data both at baseline and at 12 months were available in 51/79 (64.56%) walker patients for the 6MWT assessment.
In 51 patients with 6MWD available at baseline and after 12 months/6 infusions (median days from baseline = 306 (range 286–436 days)), the 6MWT did not significantly increase from baseline to 12 months (mean difference = 6.65 (95%CI: −7.08–20.37)).
When subdivided into subtypes, the increase showed a trend in significance in both type IIIA and IIIB patients. Details of the analysis are reported in Table 2 and Table S6.
Longitudinal data analysis
In a multivariable analysis including the 79 walker patients who had at least 6‐months follow‐up (median length of follow‐up equal to 1.90 years (range 0.77–3.11 years)), there was a difference in the slope according to the SMA subtype (p for interaction between time and SMA type = 0.002) (Fig. 2E,F). Age, 6MWT at baseline were significantly contributing to the changes, while SMA III subtype and SMN2 copy were not (Table S7).
Figure 3 shows the changes in treated patients subdivided according to age groups in relation to published natural history data in untreated patients also subdivided according to the same criteria. Table S8 reports the details of the two cohorts.
Figure 3.
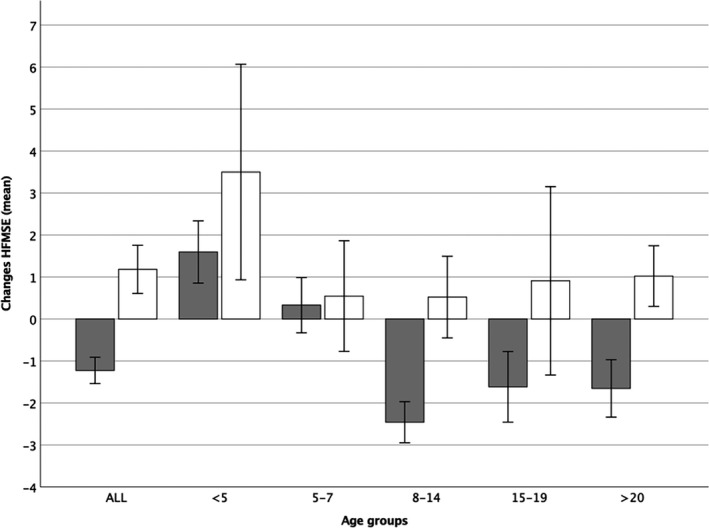
Mean 12‐months changes in external untreated controls and treated cohort. Color coding: dark grey: untreated controls, 22 white: treated cohort.
DISCUSSION
The aim of this study was to report real‐world data in a large cohort of type III patients treated with nusinersen, including both pediatric and adult patients, filling a gap in the literature that has mainly focused on adult type III patients 12 , 13 , 14 , 15 , 16 , 17 , 18 or on types I and II SMA in the pediatric age. 29 , 30 The analysis of this data, however, should be interpreted with caution as should consider the clinical heterogeneity of type III SMA, as well as the number of variables such as wide age range, age of onset (types IIIA and IIIB), functional status (from non‐sitters to fully ambulant), baseline functional scores, duration of disease before the initiation of nusinersen, and genotype (number of SMN2 copies) that could all play a role in determining the response. Because of this, rather than providing just a single estimate of the changes in the whole cohort, we analyzed the data identifying subgroups based on these variables.
As over 75% had two assessments at a 12‐month distance, we first looked at the 12‐month changes, reporting positive changes in all three measures. These results are at variance with natural history studies in type III patients showing a 12‐month decline on all the three measures used in the present study. 22 , 31 , 32
A more detailed comparison with untreated patients was possible for the HFMSE because of the availability of recently published 12‐month HFMSE longitudinal data collected in untreated patients. 22 As in the natural history study, untreated patients were subdivided according to age groups and functional status, this allowed a much more accurate matching of the subgroups than an overall comparison between two groups with a wide age and functional range.
The analysis of the different age subgroups allowed further considerations. After the age of 7 years, the mean HFMSE 12‐month changes in the untreated patients were always negative and none of the patients showed any improvement. 22 This was significantly different from what was observed in the treated patients in whom the mean changes were always positive and the number of individual patients with negative changes was limited. Irrespective of the absolute values of positive changes, the delta between treated and untreated after the age of 7 was always between 2.5 and 3 points. Before the age of 7 years, type III untreated patients had positive mean 12‐month changes but the treated group had a larger improvement. Before the age of 5, there was a delta of 1.9 points between treated and untreated, but the difference did not reach significance. This comparison could not be replicated with the RULM and the 6MWT as the limited reference data 31 , 32 would not have allowed an appropriate matching of the age and functional subgroups.
Our results in a large cohort including both adults and patients confirm previous findings in adult patients, 14 , 16 , 17 , 18 , 33 suggesting that there is a 12‐month treatment effect in type III patients irrespective of their ambulatory status and that the changes can be observed on one or more functional measures, depending on age and functional status.
It is of note that each functional subgroup showed some improvement on at least one scale and that none of the scales in isolation was able to identify all patients who had a functional improvement, likely reflecting the large variability of the functional characteristics of the individuals studied. The RULM changes were larger and achieved significance in type IIIA rather than in type IIIB and in non‐ambulant patients, while the HFMSE was significant in both ambulant and non‐ambulant and in type IIIB. These results suggest that the different scales should be used in combination as each of them contributes to detect possible changes in different groups of patients.
A number of patients had longer follow‐up, with a mean duration of follow‐up of 1.8 years. Although the data collected after 12 months are still incomplete, our results suggest that the improvement observed in the first year is maintained over time with a further increase in scores after the first year.
In order to reduce the possibility of a selection bias, we also performed a different analysis including all assessments from all the type III patients who had at least 6‐months follow‐up, in an attempt to identify which variable contributed to the possible changes in the individual measures. On the HFMSE scale, age, gender, baseline value, and functional status all contributed to the changes, while the number of SMN2 copies did not but this should be interpreted with caution as data on SMN2 copy number were not available in 24% of the patients.
The effect of the different variables was less obvious on the RULM and even less on the 6MWT. This probably reflects the different constructs of these measures as the HFMSE covers a wider spectrum of abilities than the other two that are partly targeting distinct functional groups. While the 6MWT can only be performed in ambulant patients, 13 the RULM is more appropriate for weaker patients as it often reaches ceiling scores in stronger ambulant type III patients. Another possible explanation is that changes in the 6MWT may be better appreciated with a longer follow up, as previously reported In the CS12 Nusinersen study, long term extension of the CS2 open‐label study. 13 Further studies in larger cohort using the 6MWT may also help to better understand how to use the 6MWT in SMA. Following recent recommendations, 34 we used the raw 6MWD scores as the optimal reference equations for calculating % predicted 6MWD in this patient population is not known.
In conclusion, our findings expand the available data on the effect of Nusinersen on type III patients, so far mostly limited to adult patients. Our results also highlight the variability of responses in relation to treatment and the need for a comprehensive assessment of various functional aspects. As the pattern of changes varies in relation to age and functional severity, the relevance of the response to treatment is better appreciated if the observed changes are compared to the changes observed in untreated patients with similar age and functional status. The topic of minimal clinically important difference warrants further study and will assist the clinician in presenting reasonable expectations to an SMA type III patient treated with nusinersen.
Conflict of Interest
Coratti, De Sanctis, Montes, Glanzman, Dunaway Young, Pane, Messina, D’Amico, Darras, Bertini, Sansone, Day, Bovis, Muntoni, De Vivo, Finkel, Bruno, Mercuri, and Duong report personal fees from BIOGEN S.R.L. outside the submitted work; Coratti, Pera, De Sanctis, Montes, Glanzman, Dunaway Young, Duong, Sframeli, Scoto, Darras, Bertini, Day, Muntoni, De Vivo, Finkel, Bruno, and Mercuri report personal fees from ROCHE outside the submitted work; Coratti, De Sanctis, Glanzman, Pane, Messina, Darras, Bertini, Sansone, Day, Muntoni, De Vivo, Finkel, Bruno, and Mercuri report from personal fees AVEXIS outside the submitted work; Dunaway Young reports personal fees SMA FOUNDATION outside the submitted work; Dunaway Young, Montes, and Pasternak report personal fees from SCHOLAR ROCK outside the submitted work; D’Amico, Day, Finkel, Mercuri, and Duong report from personal fees NOVARTIS outside the submitted work; Martens, Salmin, Morando, Rohwer, Mizzoni, Antonaci, Frongia, Civitello, and Patanella have nothing to disclose.
Supporting information
Table S1. HFMSE descriptive statistics (Mean, SD, Min, Max) of the 12‐month cohort.
Table S2. 12‐month trajectories grouped as stable (+2 points), improved (>+2) or declined (>−2) HFMSE and RULM.
Table S3. Change in HFMSE score for type III. Dark grey cells: statistical significance
Table S4. RULM descriptive statistics (Mean, SD, Min, Max) of the 12‐month cohort.
Table S5. Change in RULM score for type III. Dark grey cells: statistical significance
Table S6. 6MWT descriptive statistics (Mean, SD, Min, Max) of the 12‐month cohort.
Table S7. Change in 6MWT distance for type III walkers. Dark grey cells: statistical significance.
Table S8. Mean and standard deviations comparison of the treated population and external untreated controls. Dark grey shaded cells: statistical significance.
Acknowledgments
The SMA REACH UK working group: UK ‐ Great Ormond Street Hospital; University College London; Birmingham Heartlands Hospital; Leeds Children Hospital; Evelina Children’s Hospital, London; The Robert Jones and Agnes Hunt Orthopaedic Hospital, Oswestry; Sheffield Teaching Hospital. The support of the SMA Trust and of MDUK to the activities of the Dubowitz Neuromuscular Centre is gratefully acknowledged. The National Institute for Health Research Biomedical Research Centre at Great Ormond Street Hospital for Children NHS Foundation Trust and University College London. The SMA Foundation and Cure SMA are gratefully acknowledged for supporting the PNCR sites within the US iSAMC network. Famiglie SMA is gratefully acknowledged for supporting the Italian SMA Network (Telethon UILDM project, GSP 13002). The support of Biogen to the iSMAC registry is gratefully acknowledged. Biogen had no role in the study design or interpretation. Some authors are representative members of the ERN NMW network (EM, EB, MP, AD, CB).
Appendix A.
iSMAC group
| Name | Location | Role | Contribution |
|---|---|---|---|
| Gian Luca Vita | Department of Clinical and Experimental Medicine and Centro Clinico Nemo Sud, University of Messina, Messina, Italy | MD | Clinical support and coordination among the team |
| Emilio Albamonte | Neurorehabilitation Unit, University of Milan, Neuromuscular Omnicentre Clinical Center, Niguarda Hospital, Milan | MD | Clinical support and coordination among the team |
| Marina Pedemonte | Center of Experimental and Translational Myology, IRCCS Istituto Giannina Gaslini, Genoa, Italy | MD | Clinical support and coordination among the team |
| Noemi Brolatti | Center of Experimental and Translational Myology, IRCCS Istituto Giannina Gaslini, Genoa, Italy | MD | Clinical support and coordination among the team |
| Giulia Norcia | Centro Clinico Nemo, Fondazione Policlinico Universitario Agostino Gemelli IRCCS, Rome, Italy | PT | Performed the assessments |
| Lavinia Fanelli | Centro Clinico Nemo, Fondazione Policlinico Universitario Agostino Gemelli IRCCS, Rome, Italy | PT | Performed the assessments |
| Nicola Forcina | Centro Clinico Nemo, Fondazione Policlinico Universitario Agostino Gemelli IRCCS, Rome, Italy | PT | Performed the assessments |
| Sara Carnicella | Centro Clinico Nemo, Fondazione Policlinico Universitario Agostino Gemelli IRCCS, Rome, Italy | PT | Performed the assessments |
| Adelina Carlesi | Unit of Neuromuscular and Neurodegenerative Disorders, Department of Neurosciences, IRCCS Bambino Gesù Children's Hospital, Rome, Italy | PT | Performed the assessments |
| Annamaria Bonetti | Unit of Neuromuscular and Neurodegenerative Disorders, Department of Neurosciences, IRCCS Bambino Gesù Children's Hospital, Rome, Italy | PT | Performed the assessments |
| Giulia Colia | Unit of Neuromuscular and Neurodegenerative Disorders, Department of Neurosciences, IRCCS Bambino Gesù Children's Hospital, Rome, Italy | PT | Performed the assessments |
| Vincenzo Di Bella | Department of Clinical and Experimental Medicine and Centro Clinico Nemo Sud, University of Messina, Messina, Italy | PT | Performed the assessments |
| Gloria Ferrantini | Centro Clinico Nemo, Fondazione Policlinico Universitario Agostino Gemelli IRCCS, Rome, Italy | MD | Clinical support and coordination among the team |
| Diletta Rossi | Centro Clinico Nemo, Fondazione Policlinico Universitario Agostino Gemelli IRCCS, Rome, Italy | Study nurse | Data entry and clinical support |
| Antonella Longo | Unit of Neuromuscular and Neurodegenerative Disorders, Department of Neurosciences, IRCCS Bambino Gesù Children's Hospital, Rome, Italy | Study nurse | Data entry and clinical support |
| Simona Lucibello | Centro Clinico Nemo, Fondazione Policlinico Universitario Agostino Gemelli IRCCS, Rome, Italy | MD | Clinical support and coordination among the team |
| Katia Agata Patanella | Institute of Neurology, Department of Neurosciences, Catholic University, Rome, Italy. | MD | Clinical support and coordination among the team |
| Chiara Bravetti | Centro Clinico Nemo, Fondazione Policlinico Universitario Agostino Gemelli IRCCS, Rome, Italy | Study nurse | Data entry and clinical support |
| Michela Catteruccia | Unit of Neuromuscular and Neurodegenerative Disorders, Department of Neurosciences, IRCCS Bambino Gesù Children's Hospital, Rome, Italy | MD | Clinical support and coordination among the team |
| Daniela Leone | Centro Clinico Nemo, Fondazione Policlinico Universitario Agostino Gemelli IRCCS, Rome, Italy | MD | Clinical support and coordination among the team |
| Beatrice Berti | Centro Clinico Nemo, Fondazione Policlinico Universitario Agostino Gemelli IRCCS, Rome, Italy | MD | Clinical support and coordination among the team |
| Concetta Palermo | Centro Clinico Nemo, Fondazione Policlinico Universitario Agostino Gemelli IRCCS, Rome, Italy | MD | Clinical support and coordination among the team |
| Tim Estilow | Department of Occupational Therapy, The Children's Hospital of Philadelphia, Pennsylvania. | PT | Performed the assessments |
| Donnielle Rome‐Martin | Departments of Neurology and Pediatrics, Columbia University Irving Medical Center, New York, USA | PT | Performed the assessments |
| Elizabeth Maczek | Department of Neurology, Boston Children's Hospital, Harvard Medical School, Boston, MA | PT | Performed the assessments |
| Courtney Dias | Department of Neurology, Boston Children's Hospital, Harvard Medical School, Boston, MA | PT | Performed the assessments |
| Alessandra Di Bari | Neurorehabilitation Unit, University of Milan, Neuromuscular Omnicentre Clinical Center, Niguarda Hospital, Milan | Study nurse | Data entry and clinical support |
| Amelia Signorino | Department of Clinical and Experimental Medicine and Centro Clinico Nemo Sud, University of Messina, Messina, Italy | PT | Data entry and clinical support |
| Alexis Levine | Department of Neurology, Boston Children's Hospital, Harvard Medical School, Boston, MA | Coordinators | Data entry and clinical support |
| Nancy Videon | Departments of Neurology and Pediatrics, Columbia University Irving Medical Center, New York, USA | Coordinators | Data entry and clinical support |
| Aixa Rodriguez | Nemours Children’s Hospital, University of Central Florida College of Medicine, Orlando, USA | Coordinators | Data entry and clinical support |
| Julia Balashkina | Nemours Children’s Hospital, University of Central Florida College of Medicine, Orlando, USA | Coordinators | Data entry and clinical support |
| Katharine Hagerman | Departments of Neurology and Pediatrics, Stanford University School of Medicine, Stanford, CA, United States of America | Coordinators | Data entry and clinical support |
| Richard Gee | Departments of Neurology and Pediatrics, Stanford University School of Medicine, Stanford, CA, United States of America. | PT | Performed the assessments |
| Bill Martens | Neuromuscular Disease Center, Strong Memorial Hospital, University of Rochester, Rochester, NY | IT team | Provided IT support, reports, and descriptive analysis |
| Felice Catania | Astir s.r.l., Milan, Italy. | IT team | Provided IT support, reports, and descriptive analysis |
Funding Information
The support of the SMA Trust and of MDUK to the activities of the Dubowitz Neuromuscular Centre is gratefully acknowledged. The National Institute for Health Research Biomedical Research Centre at Great Ormond Street Hospital for Children NHS Foundation Trust and University College London. The SMA Foundation and Cure SMA are gratefully acknowledged for supporting the PNCR sites within the US iSAMC network. Famiglie SMA is gratefully acknowledged for supporting the Italian SMA Network (Telethon UILDM project, GSP 13002). The support of Biogen to the iSMAC registry is gratefully acknowledged.
Funding Statement
This work was funded by Fondazione Telethon grant GSP 13002; SMA Trust ; MDUK; National Institute for Health Research Biomedical Research Centre; NHS Foundation Trust; SMA Foundation ; Cure SMA .
References
- 1. D'Amico A, Mercuri E, Tiziano FD, Bertini E. Spinal muscular atrophy. Orphanet J Rare Dis 2011;6:71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Dubowitz V. Chaos in classification of the spinal muscular atrophies of childhood. Neuromuscul Disord 1991;1:77–80. [DOI] [PubMed] [Google Scholar]
- 3. Pera MC, Coratti G, Berti B, et al. Diagnostic journey in spinal muscular atrophy: is it still an odyssey? PLoS One 2020;15:e0230677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Zerres K, Rudnik‐Schoneborn S, Forrest E, et al. A collaborative study on the natural history of childhood and juvenile onset proximal spinal muscular atrophy (type II and III SMA): 569 patients. J Neurol Sci 1997;146:67–72. [DOI] [PubMed] [Google Scholar]
- 5. Rigo F, Hua Y, Krainer AR, Bennett CF. Antisense‐based therapy for the treatment of spinal muscular atrophy. J Cell Biol 2012;199:21–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Finkel RS, Mercuri E, Darras BT, et al. Nusinersen versus sham control in infantile‐onset spinal muscular atrophy. N Engl J Med 2017;377:1723–1732. [DOI] [PubMed] [Google Scholar]
- 7. Mercuri E, Darras BT, Chiriboga CA, et al. Nusinersen versus sham control in later‐onset spinal muscular atrophy. N Engl J Med 2018;378:625–635. [DOI] [PubMed] [Google Scholar]
- 8. Pechmann A, Langer T, Wider S, Kirschner J. Single‐center experience with intrathecal administration of nusinersen in children with spinal muscular atrophy type 1. Eur J Paediatr Neurol 2018;22:122–127. [DOI] [PubMed] [Google Scholar]
- 9. Pane M, Palermo C, Messina S, et al. Nusinersen in type 1 SMA infants, children and young adults: preliminary results on motor function. Neuromuscul Disord 2018;28:582–585. [DOI] [PubMed] [Google Scholar]
- 10. Aragon‐Gawinska K, Seferian AM, Daron A, et al. Nusinersen in patients older than 7 months with spinal muscular atrophy type 1: a cohort study. Neurology 2018;91:e1312–e1318. [DOI] [PubMed] [Google Scholar]
- 11. Pane M, Coratti G, Sansone VA, et al. Nusinersen in type 1 spinal muscular atrophy: twelve‐month real‐world data. Ann Neurol 2019;86:443–451. [DOI] [PubMed] [Google Scholar]
- 12. Darras BT, Chiriboga CA, Iannaccone ST, et al. Nusinersen in later‐onset spinal muscular atrophy: long‐term results from the phase 1/2 studies. Neurology 2019;92:e2492–e2506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Montes J, Dunaway Young S, Mazzone ES, et al. Nusinersen improves walking distance and reduces fatigue in later‐onset spinal muscular atrophy. Muscle Nerve 2019;60:409–414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hagenacker T, Wurster CD, Günther R, et al. Nusinersen in adults with 5q spinal muscular atrophy: a non‐interventional, multicentre, observational cohort study. Lancet Neurol 2020;19:317–325. [DOI] [PubMed] [Google Scholar]
- 15. Jochmann E, Steinbach R, Jochmann T, et al. Experiences from treating seven adult 5q spinal muscular atrophy patients with nusinersen. Ther Adv Neurol Disord 2020;13:1756286420907803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Yeo CJJ, Simeone SD, Townsend EL, et al. Prospective cohort study of Nusinersen treatment in adults with spinal muscular atrophy. J Neuromuscul Dis 2020;7:257–268. [DOI] [PubMed] [Google Scholar]
- 17. Maggi L, Bello L, Bonanno S, et al. Nusinersen safety and effects on motor function in adult spinal muscular atrophy type 2 and 3. J Neurol Neurosurg Psychiatry 2020;91:1166–1174. [DOI] [PubMed] [Google Scholar]
- 18. Walter MC, Wenninger S, Thiele S, et al. Safety and treatment effects of nusinersen in longstanding adult 5q‐SMA type 3 ‐ a prospective observational study. J Neuromuscul Dis 2019;6:453–465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Osredkar D, Jílková M, Butenko T, et al. Children and young adults with spinal muscular atrophy treated with nusinersen. Eur J Paediatr Neurol 2020;30:1–8. [DOI] [PubMed] [Google Scholar]
- 20. Kaufmann P, McDermott MP, Darras BT, et al. Observational study of spinal muscular atrophy type 2 and 3: functional outcomes over 1 year. Arch Neurol 2011;68:779–786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Kaufmann P, McDermott MP, Darras BT, et al. Prospective cohort study of spinal muscular atrophy types 2 and 3. Neurology 2012;79:1889–1897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Coratti G, Messina S, Lucibello S, et al. Clinical variability in spinal muscular atrophy type III. Ann Neurol 2020;88:1109–1117. [DOI] [PubMed] [Google Scholar]
- 23. Mercuri E, Finkel R, Scoto MC, et al. Development of an academic disease registry for spinal muscular atrophy. Neuromuscul Disord 2019;29:794–799. [DOI] [PubMed] [Google Scholar]
- 24. O’Hagen JM, Glanzman AM, McDermott MP, et al. An expanded version of the Hammersmith Functional Motor Scale for SMA II and III patients. Neuromuscul Disord 2007;17:693–697. [DOI] [PubMed] [Google Scholar]
- 25. Mazzone ES, Mayhew A, Montes J, et al. Revised upper limb module for spinal muscular atrophy: development of a new module. Muscle Nerve 2017;55:869–874. [DOI] [PubMed] [Google Scholar]
- 26. Dunaway Young S, Montes J, Kramer SS, et al. Six‐minute walk test is reliable and valid in spinal muscular atrophy. Muscle Nerve 2016;54:836–842. [DOI] [PubMed] [Google Scholar]
- 27. Glanzman AM, Mazzone ES, Young SD, et al. Evaluator training and reliability for SMA global nusinersen trials1. J Neuromuscul Dis 2018;5:159–166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Coratti G, Pera MC, Lucibello S, et al. Age and baseline values predict 12 and 24‐month functional changes in type 2 SMA. Neuromuscul Disord 2020;30:756–764. [DOI] [PubMed] [Google Scholar]
- 29. Audic F, de la Banda MGG , Bernoux D, et al. Effects of nusinersen after one year of treatment in 123 children with SMA type 1 or 2: a French real‐life observational study. Orphanet J Rare Dis 2020;15:148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Gómez‐García de la Banda M, Amaddeo A, Khirani S, et al. Assessment of respiratory muscles and motor function in children with SMA treated by nusinersen. Pediatr Pulmonol 2021;56:299–306. [DOI] [PubMed] [Google Scholar]
- 31. Pera MC, Coratti G, Mazzone ES, et al. Revised upper limb module for spinal muscular atrophy: 12 month changes. Muscle Nerve 2019;59:426–430. [DOI] [PubMed] [Google Scholar]
- 32. Montes J, McDermott MP, Mirek E, et al. Ambulatory function in spinal muscular atrophy: age‐related patterns of progression. PLoS One 2018;13:e0199657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Veerapandiyan A, Eichinger K, Guntrum D, et al. Nusinersen for older patients with spinal muscular atrophy: a real‐world clinical setting experience. Muscle Nerve 2020;61:222–226. [DOI] [PubMed] [Google Scholar]
- 34. Goodwin AM, Cornett KMD, McKay MJ, et al. Limitations of 6‐minute walk test reference values for spinal muscular atrophy. Muscle Nerve 2020;61:375–382. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. HFMSE descriptive statistics (Mean, SD, Min, Max) of the 12‐month cohort.
Table S2. 12‐month trajectories grouped as stable (+2 points), improved (>+2) or declined (>−2) HFMSE and RULM.
Table S3. Change in HFMSE score for type III. Dark grey cells: statistical significance
Table S4. RULM descriptive statistics (Mean, SD, Min, Max) of the 12‐month cohort.
Table S5. Change in RULM score for type III. Dark grey cells: statistical significance
Table S6. 6MWT descriptive statistics (Mean, SD, Min, Max) of the 12‐month cohort.
Table S7. Change in 6MWT distance for type III walkers. Dark grey cells: statistical significance.
Table S8. Mean and standard deviations comparison of the treated population and external untreated controls. Dark grey shaded cells: statistical significance.


