Abstract
A 22-year-old woman was diagnosed with thyrotoxicosis 8 weeks after the diagnosis of a mild COVID-19 infection. She had reported significant unexplained weight loss after testing positive for COVID-19, but failed to seek medical attention. She recovered well from COVID-19, but presented to the emergency department with worsening symptoms of thyrotoxicosis after 2 months. In view of her known history of previously treated Graves’ disease, a recurrence of Graves’ thyrotoxicosis was suspected. A positive thyroid stimulating hormone receptor antibody confirmed the diagnosis. She was started on carbimazole and propranolol treatment with significant improvement of her symptoms.
Keywords: COVID-19, thyroid disease
Background
SARS-CoV-2, the causative agent for COVID-19, has been reported to be a trigger for new or recurrent autoimmune thyroid disease. The acute inflammatory response to SARS-CoV-2 is believed to trigger an immunological response causing reactivation of Graves’ disease. A handful of similar cases have been reported and our index case sheds more light on this possible complication post infection with SARS-CoV-2.
Case presentation
A 22-year-old woman tested positive for COVID-19 on a PCR nasal swab test in November 2020. Her symptoms were significant for mild coryza and dysgeusia. She recovered completely with no treatment. She reported significant unexplained weight loss of 15 kg during this time despite a normal appetite.
On 9 January 2021, she presented to the emergency department with episodes of palpitations, presyncope and hot flushes associated with chest tightness. She denied neck pain, hoarseness or pain on swallowing. Her thyroid function tests revealed new-onset thyrotoxicosis with a thyroid stimulating hormone (TSH) of 0.009 (0.3–3 μIU/mL), a free T4 (fT4) of 38.81 (11.9–20.3 pmol/L) and a free T3 of 14.8 (3.5–6.5 pmol/L). On examination, her blood pressure was normal at 136/86 mm Hg, pulse was regular at 100 bpm and she was afebrile. Cardiac, respiratory and abdominal examinations were normal. A fine tremor of the outstretched hands was observed and her ankle reflexes were increased. She did not have any evidence of neck goitre or signs of ophthalmopathy.
The patient was known to suffer from diabetes mellitus and polycystic ovary syndrome. Her medication was significant for metformin and the contraceptive pill. She had previously treated Graves’ disease in 2018 where she was administered the antithyroid drug carbimazole for 1½ years. Thyroid function tests prior to the diagnoses of COVID-19 were last taken in September 2019 and were normal (table 1).
Table 1.
Blood investigations
| Results Prior to COVID-19 infection (September 2019) |
Results 9 January 2021 |
Results 13 February 2021 |
Results 7 April 2021 |
Range | |
| TSH | 0.3 | 0.009 | 0.009 | <0.008 | 0.3–3 μIU/mL |
| Free thyroxine | 15 | 38.81 | 20.11 | 29.56 | 11.9–20.3 pmol/L |
| Free triiodothyronine | 5 | 14.8 | 13.1 | 3.5–6.5 pmol/L | |
| TSH receptor antibody | 6.9 | 0.1–1.0 IU/L | |||
| Antithyroid peroxidase antibody | <10 | 0.0–50 IU/mL | |||
| White cell count | 9.46 | 4.3–11.4×109/L | |||
| Neutrophils | 6.03 | 1.9–7.7×109/L | |||
| C reactive protein | 11.2 | 0–5 mg/L | |||
| Erythrocyte sedimentation rate | 19 | 17–21 mm first hour |
TSH, thyroid stimulating hormone.
Further blood investigations showed normal white cell count and C reactive protein levels, ruling out subacute thyroiditis as a possible cause for her thyrotoxicosis (table 1). She was started on carbimazole 40 mg daily and propranolol 40 mg three times a day in January 2021 in view of a clinical suspicion of recurrent Graves’ disease. Her TSH receptor antibody was positive at 6.9 IU/L (0.1–1.0 IU/L). This confirmed a recurrence of Graves’ disease.
Repeat thyroid function tests in February 2021 after 1 month of treatment with carbimazole 40mg/day showed significant improvement (table 1). The dose was reduced to 10 mg/day at this point, but had to be increased again to 15 mg/day in April 2021 in view of worsening fT4 levels. She is currently doing well on treatment and is being followed up regularly at our clinic.
Investigations
An ultrasound scan of the thyroid showed a normal-sized gland with a heterogeneous texture. There were pseudonodules and fibrous septations throughout the gland in keeping with chronic thyroiditis (figure 1). There was a mosaic pattern of increased Doppler flow bilaterally (figure 2).
Figure 1.
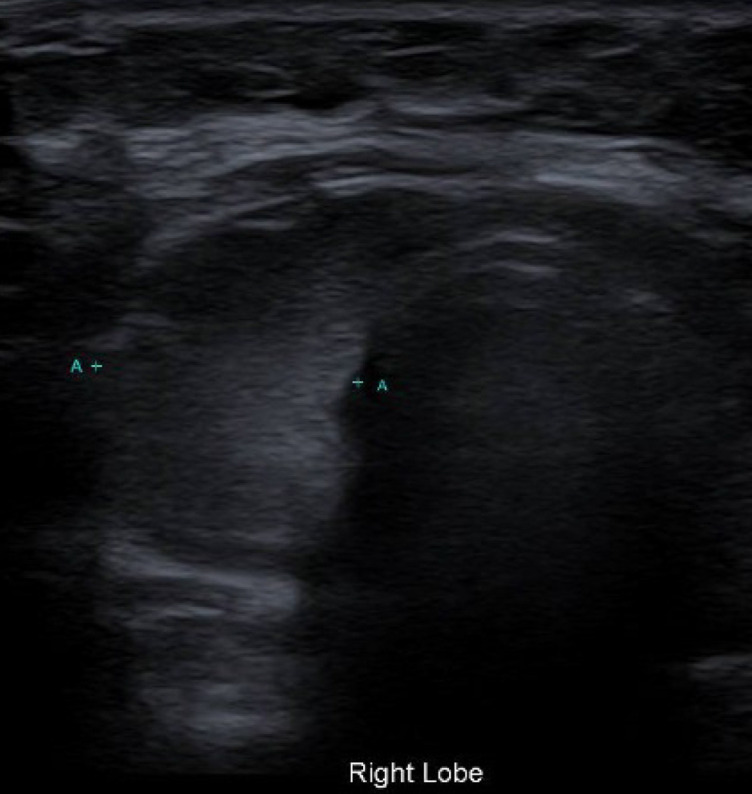
An ultrasound scan showing the right lobe of the thyroid gland. There were pseudonodules and fibrous septations throughout the gland in keeping with chronic thyroiditis.
Figure 2.
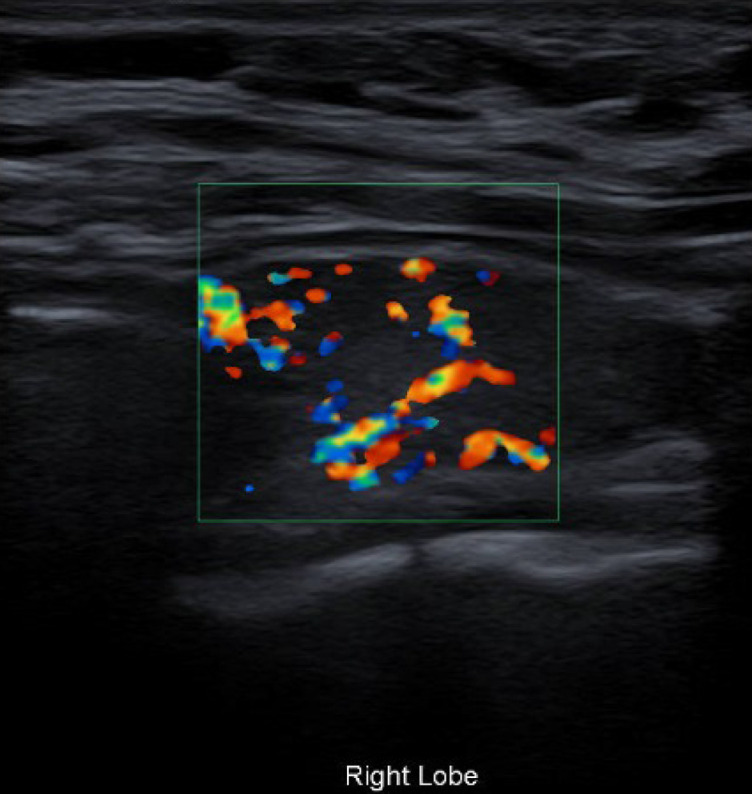
A mosaic pattern of increased Doppler flow is seen in the right lobe.
Differential diagnosis
The differential diagnosis of thyrotoxicosis post COVID-19 includes different forms of thyroiditis, such as inflammatory or subacute thyroiditis and autoimmune hyperthyroidism.1 In the above case, a previous history of treated Graves’ disease suggested that this might be a recurrence of Graves’ disease triggered by an infection with SARS-CoV-2. This was confirmed with a high TSH receptor antibody level and ultrasound scan, which was suggestive of Graves’ disease. Moreover, inflammatory or subacute thyroiditis was ruled out as the patient did not report neck pain and her white cell count, neutrophil count and C reactive protein levels were in the normal range.
Outcome and follow-up
The patient is clinically well on carbimazole treatment. She is being regularly followed up at our clinic to titrate the carbimazole dose according to her thyroid function tests.
Discussion
An infection with SARS-CoV-2 may trigger either known latent or new-onset autoimmunity.1 Few similar case reports of Graves’ disease post COVID-19 have been reported. In this index case, the patient suffered mild symptoms from COVID-19 infection. She gives a significant history of a 15 kg weight loss during her acute infection, which suggests that she was already biochemically hyperthyroid at that time, but unfortunately did not seek medical help. Her symptoms continued to worsen, and she eventually presented with clinical and biochemical features of thyrotoxicosis after 8 weeks.
Jimenez-Blanco et al report two separate cases of Graves’ recurrence post infection with SARS-CoV-2. Both patients were biochemically euthyroid prior to being diagnosed with COVID-19 infection. These include a 45-year-old woman, known to suffer from Graves’ disease, with two previous episodes treated with antithyroid drugs. In May 2020, she developed bilateral pneumonia secondary to COVID-19. She reported palpitations and nervousness and was diagnosed with thyrotoxicosis due to Graves’ disease. She was treated with methimazole, which resulted in rapid improvement of her symptoms.2
Another patient reported by the same authors was a 61-year-old woman, known case of Graves’ disease, with two previous episodes treated with antithyroid drugs. One month after the diagnosis of COVID-19, she was hospitalised and diagnosed with thyrotoxicosis. Radionuclide scan showed evidence of increased tracer uptake and an ultrasound showed increased vascularity of the thyroid gland. She was started on methimazole treatment and was biochemically euthyroid after 3 months.2
Mateu-Salat et al report another two cases. A 60-year-old with known Graves’ disease, treated at 23 years of age and in remission since, developed COVID-19 pneumonia in April 2020. She presented 5 weeks later with symptoms of thyrotoxicosis and was diagnosed with Graves. A 53-year-old woman suffered COVID-19 pneumonia and presented with thyrotoxicosis 1 month after. She was diagnosed with Graves’ disease and started treatment. This woman had no prior history of thyroid disease.3
Harris et al also report a 21-year-old woman who developed symptoms of thyrotoxicosis 16 days after mild COVID-19 infection and was diagnosed with new-onset Graves’ disease. She was treated with antithyroid drugs.4
Graves’ disease may be due to an immunological cascade triggered by the hyperinflammatory disease state induced by SARS-CoV-2 infection. The inflammatory phenomenon during COVID-19 seems to be mediated by Th1 cytokines as well as interleukin (IL)-6. The pathogenesis of Graves’ is Th2 autoimmune mediated, but increased levels of IL6 have been previously reported in Graves’ disease. Stress could also have a role in the pathogenesis of Graves’ relapse post COVID-19.2
Graves’ disease has been diagnosed both during and weeks after either mild or severe COVID-19 infection. It may present as a new diagnosis or a recurrence in patients with a known history of this autoimmune thyroid condition. It is an important differential to keep in mind when patients present with thyrotoxicosis post COVID-19 infections.
Learning points.
New or recurrent Graves’ disease may present during or a few weeks after mild or severe COVID-19 infection.
A low threshold for the diagnosis of Graves’ disease should be kept in mind in patients who present with symptoms of thyrotoxicosis post COVID-19.
These patients respond well to antithyroid medication.
Footnotes
Contributors: AM wrote up the case report and performed a literature review on thyroid disease related to COVID-19 infections.
Funding: The author has not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer-reviewed.
Ethics statements
Patient consent for publication
Obtained.
References
- 1.Caron P. Thyroiditis and SARS-CoV-2 pandemic: a review. Endocrine [Internet], 2021. Available: http://link.springer.com/10.1007/s12020-021-02689-y [DOI] [PMC free article] [PubMed]
- 2.Jiménez-Blanco S, Pla-Peris B, Marazuela M. COVID-19: a cause of recurrent Graves' hyperthyroidism? J Endocrinol Invest 2021;44:387–8. 10.1007/s40618-020-01440-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mateu-Salat M, Urgell E, Chico A. SARS-COV-2 as a trigger for autoimmune disease: report of two cases of Graves' disease after COVID-19. J Endocrinol Invest 2020;43:1527–8. 10.1007/s40618-020-01366-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Harris A, Al Mushref M. Graves' thyrotoxicosis following SARS-CoV-2 infection. AACE Clin Case Rep 2021;7:14–16. 10.1016/j.aace.2020.12.005 [DOI] [PMC free article] [PubMed] [Google Scholar]


