Research Highlights
-
•
Refugees are at high risk for poor health and financial insecurity.
-
•
We use longitudinal data from Australia of cohort of refugees.
-
•
We investigate the relationship between social determinants of health, financial hardship, and health in refugees.
-
•
Women, those from Northern Africa, Sub-Sahara Africa and Middle East are more likely to have poor health.
-
•
Financial hardship is independently associated with poor health.
Keywords: Mental Health, Physical Health, Financial Hardship, Refugee, Humanitarian Migrant, Australia
Abstract
Refugees and asylum seekers are at a higher risk than the host population to poor health and financial stress. This study uses a unique longitudinal panel from Australia, the Building a New life in Australia (BNLA cohort) to understand the relationship over time between the social determinants of health, health, and financial hardship in refugees and asylum seekers. We employ a longitudinal; dynamic multivariate logistic regression to firstly estimate the relationship between the social determinants of health and poor physical and mental health. Next, we include variables related to financial hardship in our model to determine if there is an association independent of the social determinants of health. Finally, we estimate if there is a relationship between the number of financial hardships and poor physical and mental health. The results show that migrants from North Africa, the Middle East, and Sub-Sahara Africa and women are more likely to suffer from poor health. Financial hardship has an independent association with poor health. We find that going without meals had the highest odds of suffering from poor health. There was evidence of a dose response of financial hardship for those suffering from a limiting long-term health condition and post-traumatic stress syndrome. These findings suggest that refugees in Australia may need additional support past their first year to help them assimilate and contribute to economic productivity.
1. Introduction
Around the globe the share of international migrants has risen from 2.8% in 2000 to 3.5% in 2019 to reach nearly 227 million people (UNDESA (United Nations, Department of Economic, and Social Affairs) 2020). Among this total, forced migration accounted for the displacement of 65 million people in 2017 (Tulloch et al., 2016), with the growth between 2010 and 2017 in the number of asylum seekers and refugees1 (AS&R) as a result of persecution, conflict, generalized violence or human rights violation representing almost a quarter of the increase in the number of all international migrants (UNDESA (United Nations, Department of Economic, and Social Affairs) 2020). Given the scale of the phenomenon, the past two decades have seen an increasing recognition nationally and internationally of the importance of promoting health and wellbeing amongst this population to achieve sustainable development (World Health Organization Regional Office for Europe 2018).
Improving access to equitable health promotion, disease prevention and care for migrants is now explicitly recognised in the United Nations 2030 Agenda for Sustainable Development Goals (SDG) on achieving good health by understanding and acting on the more elevated risk factors that affect the health outcomes of migrants, as in the case of mental health problems, maternal health and exposure to and prevalence of contagious diseases (SDG 3); and on the conditions of inequality between countries and within countries that drive migration and exacerbate the unfavourable circumstances that migrants face in host countries (SDG 10) World Health Organization Regional Office for Europe (2018). Similarly, in 2008 the World Health Assembly launched resolution WHA61.17 urging Member States to “promote migrant-sensitive health policies and to promote equitable access to health promotion, disease prevention and care for migrants, without discrimination on the basis of gender, age, religion, nationality or race.” World Health Organization (2018)
On average approximately 13,000 people a year enter Australia as humanitarian migrants Parliament of Australia (2015) The Australian model for AS&R policy is based on a system of two pathways of obtaining asylum: offshore resettlement occurs when the person is found to be a refugee before arrival, whereas onshore resettlement occurs after arrival in Australia and a successful asylum application Andrew and Kaldor (2020). Offshore refugees and onshore refugees that entered with a valid visa can have access to permanent protection visa “which allows holders to live and work in Australia as permanent residents” Andrew and Kaldor (2020)2,3
The Australian government provides support through the Humanitarian Settlement Programme (HSP) to refugees (humanitarian migrants, HM) for up to the first 18 months of their life in Australia. This support package includes an orientation programme to life in Australia including laws and values, connections to local community groups and organisations, referral to mainstream and specialist support services, help with English and gaining employment, as well as access to education and training (Australian Government Department of Home Affairs 2020). An evaluation of the programme has found deficiencies in the management and meeting of key performance indicators of the HSP programme (Department of Home Affairs and Department of Social Services 2019). There is also no clear evidence on the long-term benefits to this marginalised group and if additional long-term support may be beneficial.
Understanding the health outcomes of AS&R relies on understanding that health for this population is influenced by the past conditions in their home country (poor or non-existent healthcare systems and the trauma of persecution), the nature of the migration journey, and, relevantly, the level of access to healthcare in transit and destination countries because of legal, cultural and financial barriers. The combination of these factors means that being a AS&R is in itself a determinant of health (World Health Organization Regional Office for Europe 2018, World Health Organization 2018). Moreover, the health of AS&R in host countries is often adversely affected by other social determinants of health, such as poverty and social and economic marginalization (Tulloch et al., 2016, World Health Organization Regional Office for Europe 2018). In particular, formal or informal barriers to employment, difficulties in access to transport, lack of social and support networks and exclusion from social security in the host country means that AS&R face a higher likelihood of financial strain potentially detrimental to their health.
Because of the marginalised economic circumstances and poor health of many asylum seekers and refugees on arrival in host countries they are more likely to face financial hardship. Economic or financial hardship can be quantified by specific areas of economic/financial difficulty such as a shortage of food, energy poverty, reliance on credit, needing to pawn or sell possessions, or relying on aid from charity or community organisations. It is likely that economic hardship and poor health may be mutually reinforcing i.e. poor health increases the likelihood of economic hardship because of decreased opportunities for employment and financial hardship may increase the likelihood of poor health. Thus, a vicious circle may be created. To help promote good health and ensure that refugees can integrate and contribute to their host country it is essential to understand how the relationship between health and financial hardship evolves over time.
Previous studies exploring the relationship between financial strain and health in AS&R are scarce, in part because of lack of systematic data on the living conditions of AS&R (Tulloch et al., 2016). Exceptions include two studies done in Australia using the first wave of the Building a New Life in Australia Survey (BNLA) cohort study (Chen et al., 2017, Chen et al., 2017), that found economic hardship had an association with severe mental illness even after adjusting for confounding in a refugee population. Elsewhere, a study on Bhutanese refugees across seven cities in the United States found the inability to pay living expenses resulted in 4.1 times higher odds (95% Confidence interval:1.8, 9.5) of depressive symptoms in men and 4.5 times higher odds (95% CI: 2.0, 10.2) in women (Vonnahme et al., 2015); while a study of Sudanese refugees in Canada found food and medicine cost worries were statistically significantly associated with an increase in psychological distress (Simich et al., 2006). Moreover, preliminary evidence of a dose-response effect of financial hardship on AS&R health comes from a small study of 40 refugee children aged 8–16 living in London (UK) that found the number of financial hardships increased the odds of serious mental illness, with one financial hardship increasing the likelihood of serious mental illness by 50% and three or more hardships by 400% compared to no financial hardship reported (Heptinstall et al., 2004). The study also found that more financial hardships were correlated with worse general health, physical functioning, daily work ability and more bodily pain (Heptinstall et al., 2004).
Although the literature provides an intuitive account of the negative relationship between financial strain and health in refugee populations in host countries, an important shortcoming of studies to date is the cross-sectional nature of the studies, which limits our understanding of the mechanisms explaining the link between health and financial hardship in AS&R populations beyond observing that the two factors are likely to be correlated. There is also no evidence on this relationship evolves over time.
We hypothesize that the social determinants of health and financial hardship have a negative impact on the health of HM as they try to settle into their new host country. To address this hypothesis, we aim to explore the relationship between the social determinants of health, financial hardship and physical and mental health in a cohort of humanitarian migrants who arrived in Australia in 2013. To meet this aim we will focus on the following objectives:
-
1)
Estimate the relationship between the social determinants of health and health outcomes in a refugee population
-
2)
Estimate and determine if there is an independent association between financial hardship and health
-
3)
Estimate if there is a dose relationship between increasing financial hardship and health
2. Methods
2.1. Study design
This is a longitudinal study using data from four years (2013–2017) of the Building a New Life in Australia (BNLA) (Edwards et al., 2017) study. The survey was available for completion in English and 14 other languages. BNLA covered the following topics: family composition and demographics, housing and neighbourhood, English language proficiency, education and training, employment and income, immigration experience, health, self-sufficiency, community support, personal resources and life satisfaction, and life in Australia.
2.2. Sampling
The BNLA study follows a sample of humanitarian migrants (HMs) (refugees) who resettled in Australia in 2013. Respondents are re-interviewed annually. Eligible humanitarian migrants were identified using the Settlement Database and recruited from 11 sites across Australia. These were chosen to maximise recruitment and ensure representativeness of less common visa subclasses. The main respondent was the lead applicant in the visa application as identified in the Settlement Database. A total of 4,035 migrating units were eligible, of which 2,031 were successfully contacted. The study recruited 1,509 migrating units i.e. an individual or group of people granted visas under the same application. 78.3% of the participants were offshore visa holders with the remainder being onshore visa holders. A total of 1,509 primary respondents were enrolled into the study, approximately 80% responded to 3 or more years of data collection with 60.6% contributing to all four waves.
2.3. Inclusion and exclusion criteria
Inclusion Criteria:
-
1)
The principal respondent of a household who was aged 18 and over.
-
2)
Respondents who participated in all four years of data question and answered all questions used in the analysis
Exclusion Criteria
-
1)
Other household members including children under the age of 18
-
2)
Respondents who did not participate in all years of data collection or did not respond to questions used in the analysis
2.4. Data
A description of the outcome, key explanatory variables, and other covariates included in our analysis is presented in Table 1.
Table 1.
Variable names and descriptions.
| Variable Name | Description |
|---|---|
| Outcome Variables: | |
| Self-rated physical health | 0-if the respondent reported excellent/very good/good health 1-if the respondent reported fair/poor/and very poor health |
| Mental health | Based on the 6-item Kessler Screening Scale for Psychological Distress (K6). Scores range between 6-30. Coded as a binary variable: 0-Score of <19 (low risk of serious mental illness) 1-Score of >19 (high risk of serious mental illness) |
| Post-traumatic stress disorder (PTSD) | Based on the PTSD-8 short questionnaire. A score of 3 or 4 in at least three questions indicated increased risk of PTSD. Coded as a binary variable: 0-Did not meet criteria for increased risk of PTSD 1-Met criteria for increased risk of PTSD |
| Long term disability, illness or injury | 0-Respondent did not report an impairment which lasted or was likely to last at least 12 months. 1-Respondent reported an impairment which lasted or was likely to last at least 12 months |
| Key Explanatory Variables | |
| Financial hardship | Financial hardship was based upon responses to the following questions:
|
| Dose response financial hardship | Based upon responses to the individual financial hardships. Additional binary variables were created: 0-Did not report more than one financial hardship 1-Respondent reported between 2-3 financial hardships And 0-Did not report more than one financial hardship 1-Respondent reported more than 3 financial hardships |
| Additional Covariates: | |
| Age | Measured in years (continuous variables) |
| Gender | 0-Male 1-Female |
| Region of Origin | A series of binary variables for region of origin: 0-Not from region 1-North Africa and Middle East 0-Not from region 1-South East Asia 0-Not from region 1-Southern and Central Asia 0-Not from region 1-Sub-Sahara Africa 0-Not from region 1-Other regions (which included Oceania and Antarctica, North-West Europe, Southern and Eastern Europe, North-East Asia and the Americas) |
| Area level deprivation | Based on the SEIFA: Decile of Relative Socio-economic Advantage & Disadvantage 2011. Three binary variables 0-Not in decile of deprivation 1-Lives in an area of low deprivation (deciles 8-10) 0-Not in decile of deprivation 1-Lives in an area of medium deprivation (deciles 4-7) 0-Not in decile of deprivation 1-Lives in an area of high deprivation (deciles 1-3) |
| Time in Australia | Years (topcoded for anonymity) |
| English ability | English Ability was derived from variables measuring language proficiency in writing, speech, reading,and understanding 0-Does not report good or very good proficiency /comprehension writing, speech, reading or understanding 1-Reports good or very good proficiency/comprehension in writing, speech, reading, or understanding. |
| Type of housing arrangement | 0-Long term let 1-Temporary housing 2-Short term let 3-Other |
| Type of housing tenancy | 0-Does not pay rent 1-Pays rent privately 2-Pays rent to the Government 3-Pays loan or mortgage 4-Other type of payment |
| Employment Status | 0-Not currently employed 1-Currently employed |
2.5. Statistical analysis
We start by estimating simple descriptives for our study sample. These include the means, standard deviations, and sample sizes for each year of data. These are also calculated for the total sample.
Next, to estimate the relationship between financial hardship and health over time we employ a dynamic logistic model employing the Mundlak method Mundlak (1978) to proxy for fixed effects in STATA v.15 StataCorp (2017).
Formally the full model we estimate is:
| (1) |
| (2) |
Where is a binary variable for mental and physical health depending upon the model being estimated for individual i in period t. is lagged health. is the financial hardship variables (which are estimated separately). are time constant demographic variables. are variables related to housing tenure and area level deprivation of the individual. are variables relating to integration into Australian society. The means (denoted with the bar above the variable) of the time varying variables are included in the analysis to reduce omitted variable bias from time constant unobserved factors. The are the parameter of coefficients to be estimated. is the error term which includes a time constant component and an idiosyncratic component.
By using this estimation strategy, we can determine if there is an independent association of financial hardship with health beyond that of the social determinants of health and past health. In our model we assume that a one period lag should sufficiently capture the long-term relationship between health and financial hardship. This will remove some of the biases associated with cross-sectional analysis. Because of our relatively short panel of four years it is not feasible to test this assumption.
3. Results
Descriptive statistics for each wave and across the entire sample period are presented in Table 2. The mean age across all the waves was 40.1 (SD 13.2) years and 30.5% were female. The majority participants came from North Africa and the Middle East (51.1%) and Southern and Central Asia (38.5%). On enrolment in the study, most (78.5%) had only been in Australia for less than a year.
Table 2.
Descriptive Statistics.
| Variable | Wave 1 (n=1,509) | Wave 2 (n=1,288) | Wave 3 (n=1,181) | Wave 4 (n=1,242) | Mean Across the Waves |
|---|---|---|---|---|---|
| Gender | |||||
| Female | 447 (29.6) | 378 (29.3) | 365 (30.9) | 403 (32.4) | 398 (30.5) |
| Male | 1,062 (70.4) | 910 (70.1) | 816 (69.1) | 841 (67.6) | 907 (69.5) |
| Age (years) | 38.5 (13.0) | 39.4 (13.0) | 41.3 (13.1) | 41.6 (13.3) | 40.1 (13.2) |
| Region of Birth | |||||
| North Africa and the Middle East | 752 (49.8) | 655 (50.9) | 609 (51.6) | 651 (52.3) | 667 (51.1) |
| South-East Asia | 101 (6.7) | 85 (6.6) | 76 (6.4) | 86 (6.9) | 87 (6.7) |
| Southern and Central Asia | 593 (39.3) | 498 (38.7) | 455 (38.5) | 465 (37.4) | 503 (38.5) |
| Sub-Saharan Africa | 58 (3.8) | 46 (3.6) | 38 (3.2) | 39 (3.1) | 45 (3.5) |
| Other | 5 (0.3) | 4 (0.3) | 3 (0.3) | 3 (0.2) | 4 (0.3) |
| Level of Deprivation in Area of Settlement | |||||
| Low | 116 (7.7) | 95 (7.4) | 94 (8.0) | 99 (8.0) | 101 (7.7) |
| Medium | 353 (23.4) | 290 (22.5) | 267 (22.6) | 305 (24.6) | 304 (23.3) |
| High | 1,040 (68.9) | 903 (70.1) | 820 (69.4) | 838 (67.5) | 900 (69.0) |
| Time Since Arrival | |||||
| Less than a year | 1,184 (78.5) | 59 (4.6) | 0.0 (0.0) | 0.0 (0.0) | 311 (23.8) |
| Between 1 and 2 years | 253 (16.8) | 960 (74.5) | 58 (4.9) | 0.0 (0.0) | 318 (24.3) |
| Between 2 and 3 years | 34 (2.3) | 212 (16.5) | 910 (77.1) | 49 (3.9) | 301 (23.1) |
| 3 or more years | 38 (2.5) | 57 (4.4) | 213 (18.0) | 1,195 (96.1) | 376 (28.8) |
| Overall Health Poor over the past 4 weeks | 561 (37.2) | 501 (38.9) | 509 (43.1) | 511 (41.1) | 521 (39.9) |
| Overall K6 score (possible scores between 6 and 30) | 12.9 (5.9) | 12.8 (5.9) | 13.2 (6.1) | 11.8 (6.0) | 12.7 (6.0) |
| Probable serious mental health illness | 243 (16.6) | 215 (16.7) | 231 (19.8) | 185 (15.1) | 214 (17.0) |
| Long-term disability, injury or illness | 421 (28.3) | 412 (32.1) | 415 (35.4) | 412 (33.2) | 415 (32.0) |
| Likely to have PTSD | 487 (33.7) | 363 (28.7) | 372 (32.4) | 279 (23.0) | 375 (29.6) |
| Housing Arrangement | |||||
| Temporary housing | 202 (13.7) | 122 (9.6) | 110 (9.4) | 126 (10.3) | 140 (10.9) |
| Short-term let | 509 (34.5) | 243 (19.1) | 147 (12.6) | 131 (10.7) | 258 (20.0) |
| Long-term let | 729 (49.4) | 855 (67.2) | 845 (72.5) | 859 (70.1) | 822 (64.0) |
| Other | 37 (2.5) | 53 (4.2) | 64 (5.5) | 109 (8.9) | 66 (5.1) |
| Housing Tenure Type | |||||
| Pays Rent Privately | 1,304 (88.0) | 1,150 (90.3) | 1,024 (88.2) | 1,062 (85.9) | 1,135 (88.1) |
| Pays Government Rent | 109 (7.4) | 47 (3.7) | 58 (5.0) | 66 (5.3) | 70 (5.4) |
| Does Not Pay Rent | 33 (2.2) | 17 (1.3) | 19 (1.6) | 7 (0.6) | 19 (1.5) |
| Pays Loan or Mortgage | 7 (0.5) | 17 (1.3) | 38 (3.3) | 87 (7.0) | 37 (2.9) |
| Other Payment | 28 (1.9) | 42 (3.3) | 22 (1.9) | 15 (1.2) | 27 (2.1) |
| Good English Ability | 625 (41.9) | 626 (48.8) | 575 (49.3) | 674 (54.3) | 625 (48.3) |
| In paid employment | 135 (9.0) | 260 (20.2) | 311 (26.6) | 406 (32.8) | 278 (21.4) |
| Experiencing stress due to finances | 632 (43.2) | 739 (58.0) | 448 (39.8) | 575 (48.7) | 599 (47.4) |
| Number of economic hardships indicated | |||||
| 1 | 261 (23.5) | 273 (32.9) | 194 (22.6) | 196 (20.9) | 231 (24.7) |
| 2 | 170 (16.7) | 188 (25.3) | 134 (16.8) | 131 (15.0) | 156 (18.1) |
| 3 or more | 155 (15.4) | 257 (31.6) | 171 (20.5) | 168 (18.4) | 189 (21.1) |
| Experiencing at least one economic hardship | 659 (43.7) | 732 (56.8) | 517 (42.8) | 500 (40.2) | 602 (46.1) |
| Experiencing economic hardship | |||||
| Struggling to pay bills on time | 263 (18.3) | 395 (31.1) | 322 (27.7) | 314 (25.4) | 324 (25.3) |
| Could not pay rent/mortgage on time | 176 (12.1) | 168 (13.2) | 162 (13.9) | 149 (12.0) | 164 (12.8) |
| Went without meals | 120 (8.2) | 124 (9.7) | 82 (7.0) | 93 (7.5) | 105 (8.1) |
| Unable to heat or cool the home | 368 (25.4) | 534 (41.8) | 259 (22.2) | 332 (26.8) | 373 (29.1) |
| Pawned or sold something | 83 (5.7) | 85 (6.6) | 83 (7.1) | 78 (6.3) | 82 (6.4) |
| Needed help from welfare or charity | 214 (15.0) | 284 (22.6) | 222 (19.1) | 138 (11.2) | 215 (16.9) |
| Average number of economic hardships indicated | 0.83 (1.27) | 1.24 (1.44) | 0.96 (1.42) | 0.89 (1.39) | 0.9 (1.38) |
Notes: Results presented as n (%) except for age, K6 Score and Average number of economic hardships which are mean (SD)
A large majority (69.0%) of the migrants settled in areas of high deprivation, with only small numbers living in least deprived areas (7.7%). Half (49.4%) lived in long-term lets during wave one but this increased to 70.1% by wave four, with a subsequent fall in short-term lets (34.5% to 10.7%). Across the study period, the vast majority (88.1%) paid rent privately, with a notable few paying the government rent (5.4%) or a mortgage (2.9% across the study with 7% by wave four).
At the start of the study only 9% were in paid employment with this rising to 32.8% by wave four, despite all being eligible for work from the start of the study. English ability also improved throughout the course of the study from 41.9% reporting good or very good English to 54.3%.
On average across the four survey waves, 39.9% reported poor physical health in the last 4 weeks. In the Household Income and Labour Dynamics of Australia Survey, a nationally representative sample from Australia only 3% of respondents report poor health (Chen and Miller, 2013). Thus, the population in the BNLA survey has considerably worse health than the general population. 17% were likely to have a serious mental illness with the average score on the screening questionnaire being 12.7 (SD 6.0). The cut-off on the questionnaire for high risk of serious mental illness was over 19. The most common symptom reported was feeling like everything is an effort (64.9%). Around 30% were also likely to be suffering from PTSD and 32% reported a long-term disability, injury or illness.
Over the four waves of the study, the most commonly reported financial hardship was being unable to heat or cool the home (29.1%). Nearly half (46.1%) reported at least one financial hardship and a similar proportion (47.4%) experienced stress due to their finances. Of those who reported financial hardship, most only had one hardship (40.1%) but a third (32.8%) had 3 or more hardships. Notably, there was a rise in the number reporting economic hardship in wave two across all measures.
3.1. Estimation models
First, we will discuss the factors associated with poor health in our population. For all health outcomes, except limiting long term disability, illness or injury women are at increased risk compared to men. We also find for all outcomes except physical health, that migrants from North Africa and the Middle East and Sub-Sahara Africa are at a higher risk of poor health. For poor physical health and limiting long term disability there was a significant protective effect of employment. Past health for all health outcomes is significantly associated with current health. We will discuss the results in more detail in the following paragraphs.
3.2. Serious mental illness
In Table 3, the largest associated factor with serious mental illness was the region of birth. Participants from North Africa and the Middle East (OR 8.93, p<0.001, 95% CI 3.42 to 23.32), Sub-Saharan Africa (OR 6.04, p=0.003, 95% CI 1.88 to 19.47) and Southern and Central Asia (OR 4.83, p=0.001, 95% CI 1.86 to 12.52) were at a statistically significant higher risk compared to the South-East Asia cohort who were the base category. Being a woman compared to a man (OR 1.59, p < 0.001, 95% CI 1.23 to 2.05) and living in an area of high deprivation (OR 2.68, p=0.036, 95% CI 1.07 to 6.71) were both significantly associated with serious mental illness. Having serious mental illness in the previous year was strongly associated with having mental illness in the current wave (OR 4.88, p<0.001, 95% CI 3.57 to 6.65).
Table 3.
Mental Illness.
| Mental Illness | Odds Ratio | p-value | [95% Confidence Interval] |
|---|---|---|---|
| Previous Mental Illness | 4.88 | <0.001 | 3.57 to 6.65 |
| Age | 0.83 | 0.212 | 0.62 to 1.11 |
| Female | 1.59 | <0.001 | 1.23 to 2.05 |
| Region of Birth | |||
| South-East Asia | Reference | ||
| North Africa and the Middle East | 8.93 | <0.001 | 3.42 to 23.32 |
| Southern and Central Asia | 4.83 | 0.001 | 1.86 to 12.52 |
| Sub-Saharan Africa | 6.04 | 0.003 | 1.88 to 19.47 |
| Other | 3.19 | 0.317 | 0.33 to 30.95 |
| Deprivation in Area of Settlement | |||
| Low | Reference | ||
| Medium | 1.40 | 0.214 | 0.82 to 2.37 |
| High | 2.68 | 0.036 | 1.07 to 6.71 |
| Time since Arrival | 1.10 | 0.573 | 0.80 to 1.51 |
| Housing Arrangement | |||
| Long-term Let | Reference | ||
| Temporary Housing | 1.43 | 0.123 | 0.91 to 2.27 |
| Shorth-term Let | 1.12 | 0.526 | 0.79 to 1.61 |
| Other | 1.64 | 0.204 | 0.77 to 3.49 |
| Housing Tenure Type | |||
| Does Not Pay Rent | Reference | ||
| Pays Rent Privately | 1.03 | 0.962 | 0.34 to 3.08 |
| Pays Rent to Government | 0.74 | 0.637 | 0.21 to 2.59 |
| Pays Loan or Mortgage | 0.35 | 0.162 | 0.08 to 1.53 |
| Other Payment | 1.04 | 0.946 | 0.30 to 3.65 |
| Employed | 0.71 | 0.141 | 0.44 to 1.12 |
| Good English Ability | 0.76 | 0.122 | 0.54 to 1.08 |
3.3. Physical health
In Table 4, being female was associated with poor physical health (OR 1.27, p=0.033, 95% CI 1.02 to 1.59). Being employed compared to not being employed nearly halved the odds of poor health (OR 0.56, p=0.001, 95% CI 0.39 to 0.79). Poor health in the previous year was associated with poor health in the current year (OR 3.40, p<0.001, 95% CI 2.58 to 4.47).
Table 4.
Physical Health.
| Physical Health | Odds Ratio | p-value | [95% Confidence Interval] |
|---|---|---|---|
| Previous Poor Physical Health | 3.40 | <0.001 | 2.58 to 4.47 |
| Age | 0.83 | 0.132 | 0.64 to 1.06 |
| Female | 1.27 | 0.033 | 1.02 to 1.59 |
| Region of Birth | |||
| South-East Asia | Reference | ||
| North Africa and the Middle East | 1.20 | 0.364 | 0.81 to 1.79 |
| Southern and Central Asia | 0.75 | 0.159 | 0.50 to 1.12 |
| Sub-Saharan Africa | 0.75 | 0.159 | 0.50 to 1.12 |
| Other | 0.40 | 0.394 | 0.05 to 3.25 |
| Deprivation in Area of Settlement | |||
| Low | Reference | ||
| Medium | 1.13 | 0.600 | 0.72 to 1.76 |
| High | 0.97 | 0.964 | 0.45 to 2.10 |
| Time since Arrival | 1.26 | 0.100 | 0.96 to 1.66 |
| Housing Arrangement | |||
| Long-term Let | Reference | ||
| Temporary Housing | 1.00 | 0.985 | 0.67 to 1.50 |
| Shorth-term Let | 1.13 | 0.421 | 0.84 to 1.54 |
| Other | 1.67 | 0.096 | 0.91 to 2.07 |
| Housing Tenure Type | |||
| Does Not Pay Rent | Reference | ||
| Pays Rent Privately | 1.38 | 0.504 | 0.54 to 3.53 |
| Pays Rent to Government | 1.70 | 0.339 | 0.56 to 5.01 |
| Pays Loan or Mortgage | 0.79 | 0.603 | 0.16 to 2.87 |
| Other Payment | 1.93 | 0.208 | 0.69 to 5.37 |
| Employed | 0.56 | 0.001 | 0.39 to 0.79 |
| Good English Ability | 0.89 | 0.414 | 0.68 to 1.17 |
3.4. Long term disability, illness or injury
In Table 5, being born in North Africa and the Middle East (OR 3.05, p<0.001, 95% CI 1.96 to 4.75), Sub-Saharan Africa (OR 2.49, p=0.007, 95% CI 1.29 to 4.80) or Southern and Central Asia (OR 1.68, p=0.025, 95% CI 1.07 to 2.65) compared to Southeast Asia was associated with higher odds of long term impairment. Living in housing which is neither temporary, short-term let nor long-term let, which would include house owners or those living with family, was associated with a much reduced odds of long term disability, illness or injury (OR 0.46, p=0.017, 95% CI 0.25 to 0.87). Being in employment was also associated with decreased odds of long-term disability (OR 0.62, p=0.011, 95% CI 0.43 to 0.90). Having a long-term impairment in the previous year was significantly associated with having long term impairment in the current year (OR 5.29, p<0.001, 95% CI 4.42 to 6.32).
Table 5.
Long Term Disability, Illness or Injury.
| Long Term Disability, Illness or Injury | Odds Ratio | p-value | [95% Confidence Interval] |
|---|---|---|---|
| Previous Long Term Disability, Illness or Injury | 5.29 | <0.001 | 4.42 to 6.32 |
| Age | 0.85 | 0.188 | 0.67 to 1.08 |
| Female | 1.11 | 0.276 | 0.96 to 1.35 |
| Region of Birth | |||
| South-East Asia | Reference | ||
| North Africa and the Middle East | 3.05 | <0.001 | 1.96 to 4.75 |
| Southern and Central Asia | 1.68 | 0.025 | 1.07 to 2.65 |
| Sub-Saharan Africa | 2.49 | 0.007 | 1.29 to 4.80 |
| Other | 1.15 | 0.882 | 0.18 to 7.29 |
| Deprivation in Area of Settlement | |||
| Low | Reference | ||
| Medium | 0.81 | 0.351 | 0.53 to 1.26 |
| High | 0.79 | 0.542 | 0.37 to 1.69 |
| Time since Arrival | 1.23 | 0.128 | 0.94 to 1.61 |
| Housing Arrangement | |||
| Long-term Let | Reference | ||
| Temporary Housing | 0.87 | 0.505 | 0.58 to 1.30 |
| Shorth-term Let | 0.93 | 0.662 | 0.69 to 1.27 |
| Other | 0.46 | 0.017 | 0.25 to 0.87 |
| Housing Tenure Type | |||
| Does Not Pay Rent | Reference | ||
| Pays Rent Privately | 1.36 | 0.543 | 0.51 to 3.64 |
| Pays Rent to Government | 0.84 | 0.755 | 0.27 to 2.56 |
| Pays Loan or Mortgage | 1.41 | 0.580 | 0.42 to 4.71 |
| Other Payment | 0.83 | 0.744 | 0.27 to 2.55 |
| Employed | 0.62 | 0.011 | 0.43 to 0.90 |
| Good English Ability | 1.14 | 0.352 | 0.86 to 1.51 |
3.5. PTSD
In Table 6, the largest association with self-reporting of PTSD was seen with the region of birth. Being born in North Africa and the Middle East (OR 3.03, p<0.001, 95% CI 1.84 to 4.97) or in Sub-Saharan Africa was associated with increased reporting of PTSD symptoms (OR 2.07, p=0.043, 95% CI 1.02 to 4.17) compared to those from Southeast Asia. Being female was related to higher odds of self-reported PTSD by 27% (OR 1.27, p=0.023, 95% CI 1.03 to 1.56). As was the case, with the other health variables, lagged PTSD was significantly associated with reporting PTSD in the current year (OR 2.81, p<0.001, 95% CI 2.23 to 3.45).
Table 6.
PTSD.
| PTSD | Odds Ratio | p-value | [95% Confidence Interval] |
|---|---|---|---|
| Previous PTSD | 2.81 | <0.001 | 2.23 to 3.54 |
| Age | 1.00 | 0.976 | 0.79 to 1.26 |
| Female | 1.27 | 0.023 | 1.03 to 1.56 |
| Region of Birth | |||
| South-East Asia | Reference | ||
| North Africa and the Middle East | 3.03 | <0.001 | 1.84 to 4.97 |
| Southern and Central Asia | 1.41 | 0.174 | 0.86 to 2.30 |
| Sub-Saharan Africa | 2.07 | 0043 | 1.02 to 4.17 |
| Other | 3.17 | 0.156 | 0.64 to 15.57 |
| Deprivation in Area of Settlement | |||
| Low | Reference | ||
| Medium | 1.28 | 0.260 | 0.83 to 1.99 |
| High | 1.48 | 0.311 | 0.70 to 3.14 |
| Time since Arrival | 0.81 | 0.117 | 0.62 to 1.05 |
| Housing Arrangement | |||
| Long-term Let | Reference | ||
| Temporary Housing | 1.19 | 0.369 | 0.81 to 1.75 |
| Shorth-term Let | 1.20 | 0.226 | 0.89 to 1.61 |
| Other | 1.33 | 0.350 | 0.73 to 2.41 |
| Housing Tenure Type | |||
| Does Not Pay Rent | Reference | ||
| Pays Rent Privately | 1.50 | 0.413 | 0.57 to 3.92 |
| Pays Rent to Government | 1.79 | 0.292 | 0.60 to 5.32 |
| Pays Loan or Mortgage | 1.52 | 0.495 | 0.45 to 5.12 |
| Other Payment | 2.32 | 0.110 | 0.83 to 6.52 |
| Employed | 1.06 | 0.728 | 0.75 to 1.51 |
| Good English Ability | 0.99 | 0.954 | 0.75 to 1.31 |
3.6. Relationship between financial hardship and health and dose response of financial hardship
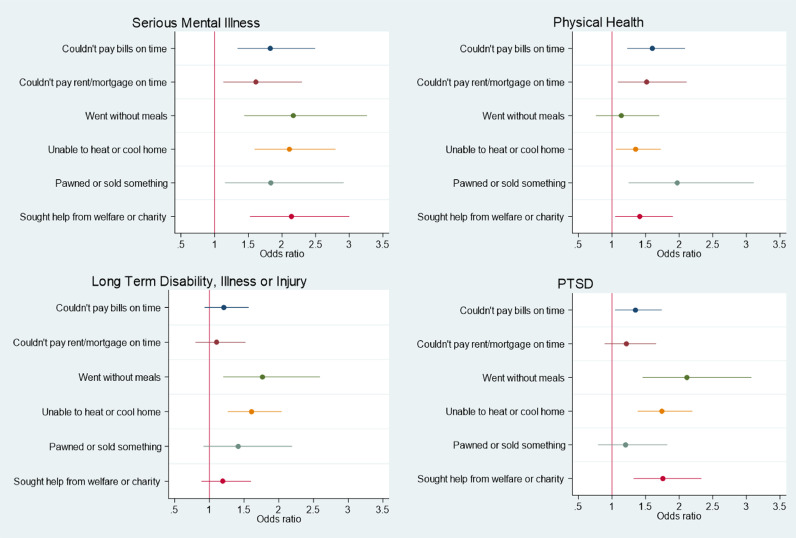
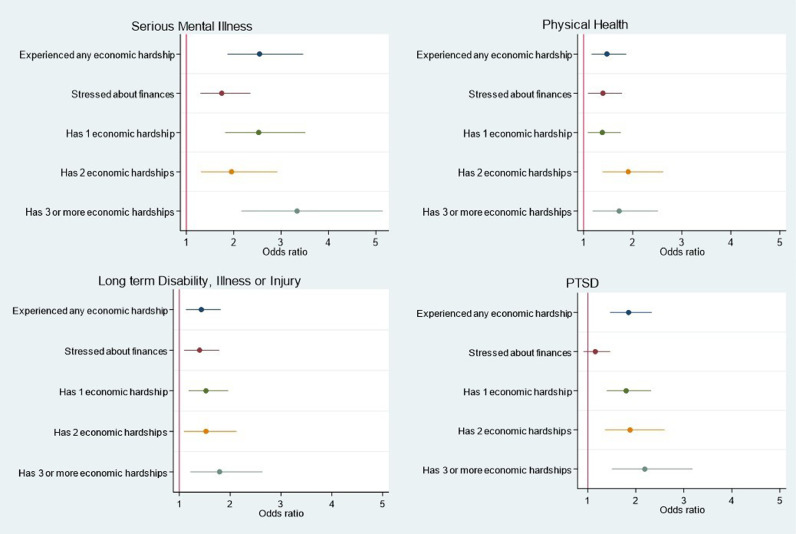
Next, we will discuss the relationship between financial hardship and poor health in HMs to Australia which are presented in Figs. Fig. 1, Fig. 2. For all measures of health, we find a significant association with financial hardship independent of the social determinants of health. The largest associations between financial hardship and health was found for mental health measures. The element of financial hardship with the largest association with all measures of health except physical health was going without meals. For physical health the largest association was found for having to pawn or sell something. Being unable to heat or cool one's home was the only element of financial hardship correlated with all health outcomes. We found some evidence of a dose response of suffering from multiple elements of financial hardship with limiting long term disability. However, this dose response was stronger for PTSD. We did not find a dose response for increasing financial hardship with mental illness and physical health.
Fig. 1.
Odds Ratios for the Association between Financial Hardship and Health.
Fig. 2.
Odds Ratios for the Association between Number of Elements of Financial Hardship and Health.
3.7. Mental illness
In Fig. 1, having at least one element of financial hardship increased the odds of mental illness by two-fold (OR 2.55, p<0.01, 95% CI 1.87 to 3.46). The highest odds were going without meals (2.17, p<0.001, 95% CI 1.44 to 3.26), followed by seeking help from welfare or charity (OR 2.14, p<0.001, 95% CI 1.53 to 3.00), being unable to heat or cool the home (OR 2.11, p<0.001, 95% CI 1.59 to 2.79), needing to pawn or sell something (OR 1.84, p=0.01, 95% CI 1.16 to 2.91), not being able to pay the bills on time (OR 1.83, p<0.001, 95% CI 1.34 to 2.49) and finally, not being able to pay rent/mortgage on time (OR 1.61, p=0.008, 95% CI 1.13 to 2.30). Feeling stressed about finances, regardless of whether this resulted in financial hardship was associated with poor mental health (OR 1.75, p<0.001, 95% CI 1.30 to 2.35).
3.8. Physical health
In Fig. 1, needing to pawn or sell something had the highest odds ratio (OR 1.97, p=0.003, 95% CI 1.25 to 3.11) of poor physical health, followed by not being able to afford to pay the bills (OR 1.60, p=0.003, 95% CI 1.23 to 2.09) and rent or mortgage on time (OR 1.52, p=0.013, 95% CI 1.09 to 2.11). Being unable to heat or cool the home (OR 1.35, p=0.015, 95% CI 1.06 to 1.72) and needing to seek help from welfare or charity (OR 1.41, pp=0.023, 95% CI 1.05 to 1.90) were also associated with increased odds of poor physical health. Experiencing stress about finances also increased the odds of poor physical health (OR 1.39, p=0.008, 95% CI 1.09 to 1.78).
3.9. Long term disability, illness or injury
In Fig. 1 we can see that going without meals was associated with the highest odds of long-term disability, illness or injury (OR 1.76, p=0.004, 95% CI 1.20 to 2.59). Also significantly associated with the risk of having a long-term impairment was being unable to heat or cool the home (OR 1.61, p<0.001, 95% CI 1.27 to 2.04). Having at least one element of financial hardship (OR 1.43, p=0.003, 95% CI 1.13 to 1.81) and experiencing stress due to finances (OR 1.40, p=0.007, 95% CI 1.10 to 1.78) were positively and significantly associated with long term disability, illness or injury.
In Fig. 2, 3 or more financial hardships increased the odds ratio by 0.27 (OR 1.79, p=0.003, 95% CI 1.22 to 2.63) compared to one (OR 1.52, p=0.001, 95% CI 1.18 to 1.96) or two (OR 1.52, p=0.013, 95% CI 1.09 to 2.12) financial hardships.
3.10. PTSD
In Fig. 1, we can see that the highest odds ratio for PTSD was going without meals (OR 2.11, p<0.001, 95% CI 1.46 to 3.07). Needing to seek help from welfare or charity (OR 1.76, p<0.001, 95% CI 1.32 to 2.33) and being unable to heat or cool the home (OR 1.74, p<0.001, 95% CI 1.38 to 2.19) had very similar associations with PTSD. This was then followed by not being able to afford bills (OR 1.35, p=0.021, 95% CI 1.05 to 1.74). Having at least one economic hardship was associated with PTSD (OR 1.85, p<0.001, 95% CI 1.47 to 2.33) (Fig. 2).
In Fig.2, PTSD showed the clearest dose-response to financial hardship with 3 or more economic hardships having the strongest association (2.19, p<0.001, 95% CI 1.50 to 3.18), then two hardships (OR 1.88, p<0.001, 95% CI 1.38 to 2.60) and finally one hardship (OR 1.80, p<0.001, 95% CI 1.40 to 2.32).
4. Discussion
This is the first study to explore the relationship between health, the social determinants of health and financial hardship over time in a vulnerable migrant population (HM-refugees). We find that women and migrants from North Africa, Middle East, and Sub-Sahara Africa are at a higher risk for poor health. Employment was linked to better outcomes when considering physical health and long-term impairment but not mental health or PTSD and living in an area of high deprivation was associated with higher likelihood of mental illness. We also find an independent association of financial hardship with health after controlling for the social determinants of health. For all health outcomes, except physical health, going without meals has the largest negative association with health. For physical health, having to pawn or sell something has the largest negative association with health. Being unable to heat or cool one's home was the only component of financial hardship that was correlated with all health outcomes. We find a dose response with increasing financial hardship and PTSD. In all our estimation models, past health is important.
An important contribution of this study is that we were able to follow a cohort of HM as they settle into their host country to understand how their health and circumstances evolve over time. Many refugees saw a deterioration in their finances over time. Our odds ratios are higher than those reported using a cross-section from the first year of the BNLA data (Chen et al., 2017). This may be because financial hardship of study participants increased after the first year of the study when they could no longer use the Humanitarian Settlement Programme where health is already worse than the general population, and remains so four years after arrival, more must be done to tackle poor health and the causes of poor health. Compared to data from the Australian HILDA survey (Department of Social Services 2017), the association between poor mental health and financial hardship was slightly lower (OR 2.13 vs 2.55) in the BNLA, when adjusted for similar factors. Whilst the relationship is similar, the prevalence in 2013 of economic hardship in refugees was around double that of the general Australian population (38.8% and 17.1%) (Department of Social Services 2017). This creates a double risk, with mental illness as likely to occur with financial hardship than the general public, but with financial hardship being more widespread in the refugee population.
The fact that we estimate longitudinal models, means that our results are not the same as other studies exploring the relationship between financial hardship and health in a vulnerable migrant population. The associations we find are smaller than those reported by Maharaj et al. (Maharaj et al., 2017). Potentially because they do not control for past health which may bias their coefficents upwards. Unlike Blair (Blair, 2000), we find a significant and large association between PTSD and financial hardship. But, this may partially be attributed to how the author defined financial hardship compared to the measure used in this study.
In order for countries to meet their SDG objectives of ‘ensuring healthy lives and promoting well-being for all at all ages’ (SDG 3) and reducing health inequalities (SDG 10) (Tulloch et al., 2016), countries must enact a clear plan to help this vulnerable group.
We do find some protective association of employment suggesting that supporting HM to find work in their host country may help to reduce financial hardship and improve health (Waddell and Burton, 2006). This suggests that policies that help refugees integrate into the host country and find meaningful and well-paid work can reduce the health and economic burden in this vulnerable population. Our results also suggest that women refugees and those from the North Africa, Middle East, and Sub-Sahara Africa are more likely to suffer from poor health so should be targeted for additional support.
Going without meals due to a shortage of money had the largest association with all measures of health except for physical health. The inability to afford culturally appropriate food may make the participants feel alienated from their home country and friends and family, compounding feelings of loneliness and worry which results in poor mental health. This may also be a contributing factor to PTSD, with feelings of hunger or worry about family serving as stark reminders of painful experiences. Practically, going without meals suggests a high level of poverty. This is likely to increase social isolation, lack of autonomy over decisions and inequality. This agrees with work done by Butterworth et al. who theorised, using a neo-material explanation, food insecurity is associated with “the most profound mental health effects of hardship” (Butterworth et al., 2012). All these factors are known to increase susceptibility to mental disorders. Furthermore, poverty and disability have been shown to have a mutually reinforcing relationship. Those with the worst financial hardship, which may be compounded by illiteracy or lack of education, are the least able to afford preventative healthcare or navigate the health care system leading to long term health problems.
As with all studies relating to refugees, our results may not translate between countries, hindering generalisability. Refugee support and experience is country specific and the results may not translate to other countries’ approaches. Finally, whilst initial causal inferences can be made, it is impossible to determine definitive causation from the analysis. The lagged health and longitudinal analysis method begins to examine the direction of the effect; however, the data was only collected around once a year and the onset of financial hardship and health within the previous years is beyond the scope of the data, therefore we are not be able to completely control for past behaviour.
5. Conclusion
Women and immigrants from North Africa, Middle East, and Sub-Sahara Africa need additional support to reduce the risk of poor health. Refugees are more likely to have financial hardship and these hardships increase the likelihood of poor health. To help this vulnerable group to integrate into the host country it is important to provide long term economic support to reduce the risk of both financial hardship and poor health. Our findings can be used to help develop long term strategies to promote the health and economic well-being of a vulnerable population of HM, contributing to international SDGs of reducing health inequalities (SDG 10) and improving the health and well-being of all people (SDG 3).
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Funding
This work was undertaken as a Masters dissertation project for a MPH at Newcastle University but did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Footnotes
As defined by the 1951 Convention Relating to the Status of Refugees, a refugee is
“someone who is unable or unwilling to return to their country of origin owing to a well-founded fear of being persecuted for reasons of race, religion, nationality, membership of a particular social group, or political opinion.” (United Nations High Commissioner for Refugees 2010)
An asylum seeker, on the other hand, is in the process of having their asylum application reviewed. This does not grant them the same privileges as a refugee and they often are unable to work, access healthcare and receive less financial support (Refugee Council of Australia 2018).
Unauthorised maritime arrivals or those arriving without a visa as of July 2013 were sent to offshore regional processing centres and ineligible for resettlement in Australia. Onshore asylum seekers without a valid visa when they entered Australia between 13 August 2012 and 1 January 2014 are subject to a different “fast-track” review process for deciding their resettlement status. See https://www.kaldorcentre.unsw.edu.au/publication/refugee-status-determination-australia
According to government figures “The Australian Government usually allocates around 13,750 places to refugees and others with humanitarian needs under its planned Humanitarian Program. Historically, the majority of these places are granted to offshore refugees referred to Australia by the UNHCR, but some are given to refugees who arrived by air or boat and were granted protection visas onshore”. See https://www.aph.gov.au/about_parliament/parliamentary_departments/parliamentary_library/pubs/rp/rp1415/asylumfacts
Contributor Information
Viviana Albani, Email: Viviana.albani@ncl.ac.uk.
Heather Brown, Email: heather.brown@ncl.ac.uk.
References
- Andrew, Kaldor Renata. Centre for international refugee law. Factsheet Australia's Refugee Policy. 2020 https://www.kaldorcentre.unsw.edu.au/sites/default/files/Factsheet_Australian%20Refugee%20Policy_Apr2019.pdf Available from: Accessed: November. [Google Scholar]
- Australian Government Department of Home Affairs. Humanitarian Settlement Programme: About the programme. 2020; Available from: https://immi.homeaffairs.gov.au/settling-in-australia/humanitarian-settlement-program/about-the-program. Accessed November 2020
- Blair R.G. Risk Factors associated with PTSD and major depression among Cambodian refugees in Utah. Health & Social Work, 2000;25(1):23–30. doi: 10.1093/hsw/25.1.23. [DOI] [PubMed] [Google Scholar]
- Butterworth P., Olesen S.C., Leach L.S. The role of hardship in the association between socio-economic position and depression. Australian & New Zealand J. Psychiatry. 2012;46(4):364–373. doi: 10.1177/0004867411433215. [DOI] [PubMed] [Google Scholar]
- Chen E., Miller G.E. Socioeconomic status and health: mediating and moderating factors. Annual Rev. Clin. Psychol. 2013;Mar 28(9):723–749. doi: 10.1146/annurev-clinpsy-050212-185634. [DOI] [PubMed] [Google Scholar]
- Chen W. Pre-migration and post-migration factors associated with mental health in humanitarian migrants in Australia and the moderation effect of post-migration stressors: findings from the first wave data of the BNLA cohort study. The Lancet Psychiatry. 2017;4(3):218–229. doi: 10.1016/S2215-0366(17)30032-9. [DOI] [PubMed] [Google Scholar]
- Chen W., Ling L., Renzaho A.M.N. Building a new life in Australia: an analysis of the first wave of the longitudinal study of humanitarian migrants in Australia to assess the association between social integration and self-rated health. BMJ Open. 2017;7(3) doi: 10.1136/bmjopen-2016-014313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Department of Home Affairs and Department of Social Services . Australian National Audit Office; Canberra: 2019. Delivery of the Humanitarian Settlement Program. Available from: https://www.anao.gov.au/sites/default/files/Auditor-General_Report_2019-2020_17.pdf Accessed: November 2020. [Google Scholar]
- Department of Social Services . Department of Social Services; Canberra: 2017. Building a New Life in Australia (BNLA): The Longitudinal Study of Humanitarian Migrants — Findings from the first three waves. [Google Scholar]
- Department of Social Services; Melbourne Institute of Applied Economic and Social Research, 2017, "The Household, Income and Labour Dynamics in Australia (HILDA) Survey, GENERAL RELEASE 16 (Waves 1-16)", doi:10.4225/87/VHRTR5, ADA Dataverse, V5
- Edwards B. Cohort Profile: building a new life in Australia (BNLA): the longitudinal study of humanitarian migrants. Int. J. Epidemiol. 2017;47(1):20. doi: 10.1093/ije/dyx218. -20h. [DOI] [PubMed] [Google Scholar]
- Heptinstall E., Sethna V., Taylor E. PTSD and depression in refugee children. Eur. Child Adolesc. Psychiatry. 2004;13(6):373–380. doi: 10.1007/s00787-004-0422-y. [DOI] [PubMed] [Google Scholar]
- Maharaj V. Food Insecurity and risk of depression among refugees and immigrants in South Africa. J. Immigrant Minority Health. 2017;19(3):631–637. doi: 10.1007/s10903-016-0370-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mundlak Y. On the pooling of time series and cross section data. Econometrica. 1978;46(1):69–85. [Google Scholar]
- Parliament of Australia . 2015. Asylum Seekers and Refugees: What are the Facts? Research paper series, 2014–15Available from: https://www.aph.gov.au/about_parliament/parliamentary_departments/parliamentary_library/pubs/rp/rp1415/asylumfacts Accessed: November 2020. [Google Scholar]
- Refugee Council of Australia . 2018. Australia's Asylum Policies. Available from: https://www.refugeecouncil.org.au/asylum-policies/ Accessed: April 2020. [Google Scholar]
- Simich L., Hamilton H., Baya B.K. Mental distress, economic hardship and expectations of life in Canada among Sudanese Newcomers. Trans. Psychiatry. 2006;43(3):418–444. doi: 10.1177/1363461506066985. [DOI] [PubMed] [Google Scholar]
- StataCorp . StataCorp LLC; College Station, TX: 2017. Stata Statistical Software: Release 15. [Google Scholar]
- Tulloch O., Machingura F., Melamed C. Overseas Development Institute; London: 2016. Health, migration and the 2030 Agenda for Sustainable Development. [Google Scholar]
- UNDESA (United Nations, Department of Economic and Social Affairs) United Nations; New York: 2020. International Migrant Stock 2019: Ten Key Facts.https://www.un.org/en/development/desa/population/migration/publications/migrationreport/docs/MigrationStock2019_TenKeyFindings.pdf [online] available. [Google Scholar]
- United Nations High Commissioner for Refugees . 2010. Convention and Protocol Relating to the Status of Refugees. Available from: https://www.unhcr.org/3b66c2aa10.html. Accessed: April 2020. [PubMed] [Google Scholar]
- Vonnahme L.A. Factors associated with symptoms of depression among bhutanese refugees in the United States. J. Immigrant Minority Health. 2015;17(6):1705–1714. doi: 10.1007/s10903-014-0120-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waddell G, Burton AK. Is work good for your health and well-being? The Stationery Office. 2006 Sep 6. [Google Scholar]
- World Health Organization Regional Office for Europe . 2018. Fact Sheets on Sustainable Development Goals: Health Targets. Migration and Health. Available from: https://www.euro.who.int/__data/assets/pdf_file/0014/352130/10.7-SDG-Fact-sheet-Migration-and-Health_FINAL.pdf?ua=1 Accessed: November 2020. [Google Scholar]
- World Health Organization . 2018. Report on the Health of Refugees and Migrants in the WHO European Region: no Public Health Without Refugee and Migrant Health. Available from: https://www.euro.who.int/en/publications/html/report-on-the-health-of-refugees-and-migrants-in-the-who-european-region-no-public-health-without-refugee-and-migrant-health-2018/en/index.html#head08 Accessed: November 2020. [Google Scholar]