Highlights
-
•
Published migration health research in the UK has focused primarily on infectious diseases and mental health.
-
•
Studies did not disaggregate by migrant sub-groups resulting in gaps for specific groups such as migrant workers and undocumented migrants.
-
•
Future research should ensure diverse geographic distribution of research, improve data disaggregation, and focus on how structures and systems impact migrant health.
-
•
Meaningful engagement, participatory approaches and co-production with migrants is critical to ensure research priorities and methodologies meet their needs and do not result in harm.
Keywords: Migration, Migrant, Health, United Kingdom, Scoping review
Abbreviations: EU, European Union; HIV, Human immunodeficiency virus; ICD-10, International Classification of Diseases - Tenth Revision; NHS, National Health Service; ONS, Office of National Statistics; PTSD, Post-traumatic stress disorder; SMR, Standardised mortality ratio; TB, Tuberculosis; UCL, University College London
Abstract
Background
One in seven people living in the United Kingdom (UK) is an international migrant, rendering migrants an important population group with diverse and dynamic health and healthcare needs. However, there has been no attempt to map contemporary trends within migration health research conducted in the UK. The aim of this scoping review was to describe trends within migration health research and identify gaps for future research agendas.
Methods
PubMed and Embase were systematically searched for empirical research with a primary focus on the concepts “health” and “migrants” published between 2001 and 2019. Findings were analysed using the UCL-Lancet Commission on Migration and Health Conceptual Framework for Migration and Health.
Results
In total, 399 studies were included, with almost half (41.1%; 164/399) published in the last five years of the study period between 2015 and 2019 and a third (34.1%; 136/399) conducted in London. Studies included asylum seekers (14.8%; 59/399), refugees (12.3%; 49/399), and undocumented migrants or migrants with insecure status (3.5%; 14/399), but most articles (74.9%; 299/399) did not specify a migrant sub-group. The most studied health topics were specific disease outcomes such as infectious diseases (24.1% of studies) and mental health (19.1%) compared to examining systems or structures that impact health (27.8%), access to healthcare (26.3%), or specific exposures or behaviours (35.3%).
Conclusions
There has been a growing interest in migration health. Ensuring a diverse geographic distribution of research conducted in the UK and disaggregation by migrant sub-group is required for a nuanced and region-specific understanding of specific health needs, interventions and appropriate service delivery for different migrant populations. More research is needed to understand how migration policy and legislation intersect with both the social determinants of health and access to healthcare to shape the health of migrants in the UK.
Background
In 2019, at least an estimated 14.2% of people (at least 9.34 million people) living in the United Kingdom (UK) were international migrants (Population of the UK by country of birth and nationality - Office for National Statistics, 2020). Here we define international migrants as people born outside of and residing within the UK. This includes people who come to work, study or join families, as well as those forced to migrate due to conflict, persecution or environmental disasters. The vast majority of people (71% of long-term migrants in 2018) migrate to the UK to work or study, compared to a much smaller proportion who come to accompany or join a family member (13%) or seek asylum or resettlement (6%) (Kierans, 2020).
Historically, migrants to the UK predominantly arrived from former British colonies and countries in close geographic proximity. There was a particular increase in migration to the UK after the second world war. Immigration regulations such as the 1962 Commonwealth Immigrants Act (amended in 1968) and the 1971 Immigration Act later restricted migration from former colonies and other non-European Union (EU) countries. The 2004 EU enlargement then led to a large increase in migration from Eastern Europe (Czaika and de Haas, 2020). Since the 2016 Brexit referendum, migration from EU countries has declined and migration from outside the EU has increased (Migration Statistics Quarterly Report: May 2020).
The conditions surrounding migration can improve or worsen an individual's health. Varying levels of risk, and resilience, during the migratory process are subject to multiple factors including migration status; national and multi-national migration policy; access to public services (including healthcare) and welfare; and broader socio-economic determinants of health (such as employment and housing). The respective magnitude of impact is often greater at the intersection of migration and gender, ethnicity, disability and poverty (Abubakar et al., 2018). Although research has shown that migrants have lower all-cause mortality in England and Wales when compared to the UK-born population (Wallace and Kulu, 2015), this aggregated mortality advantage conceals poorer health outcomes and barriers to healthcare experienced by more marginalised migrant groups (O'Donnell et al., 2007; Bradby et al., 2015).
In the UK, migration health research is a broad and varied field, appropriate for a heterogeneous population with diverse health needs and experiences. Methodological challenges such as culturally specific understandings of health (Napier et al., 2014), imperfect migrant categorisations (Abubakar et al., 2018) and limited data disaggregation by migration status (Burns et al., 2019; Migration Statistics Quarterly Report: May 2021) have made migration health research difficult to conduct, identify and synthesise. To date, there has been no attempt to map the research trends within the migration health published literature in the UK. The aim of this scoping review is two-fold: first, to describe trends within the published migration health literature; second, to identify gaps for future research on migration and health in the UK. As the UK, now outside of the EU, responds to shifts in global population mobility as a result of changing labour markets, geopolitics and climate change, this research provides an empirical catalogue to assist the formulation of migration health policy and future research agendas.
Methods
A scoping review of published literature on migration health in the UK was conducted. The aim of the review was to map published empirical research in the field rather than critically appraise the quality of the included studies. The choice of methodology allowed for a broader research question compared to a systematic review. Arksey and O'Malley's scoping review methodology (Arksey and O'Malley, 2005) was employed and the review was conducted in the following steps: determine a research question, identify relevant studies, select studies, chart the data, then collate, summarise and report the results. This study was done in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analysis extension for Scoping Reviews guidelines (Tricco et al., 2018) and can be found in Appendix A.
Research questions
This scoping review examined three research questions:
-
1
What are the publication trends (year of publication, journal, institution and country of first author, study location and study design) of migration health studies conducted in the UK between 2001 and 2019?
-
2
What are the most studied migrant typologies (migrant sub-group and country of origin) of migration health studies conducted in the UK between 2001 and 2019?
-
3
What are the most studied health topics of migration health studies conducted in the UK between 2001 and 2019?
Identifying relevant studies
The search strategy was based on the terms used in a systematic review on international migrant mortality conducted by the authors (Aldridge et al., 2018). A librarian at University College London was consulted about the adaption of the search terms. Two bibliographic databases were systematically searched: PubMed and Embase for studies published between January 1, 2001 and December 10, 2019. Full search terms are provided in Appendix B. We chose to search for studies that included data from January 1, 2001 in order to capture contemporary trends of research in this area.
Study selection
The inclusion criteria were adapted from a similar scoping review of migration health research conducted in the Republic of Ireland (Villarroel et al., 2019) and developed through an iterative process with the co-authors. We included empirical research with a primary aim or focus on the health of migrants in the UK. For example, if the study did not make an explicit link between its rationale or objectives and migration health, it was not included in the review. Health was defined holistically as the state of physical, mental and social well-being, taking into account the impact of a range of personal, social, economic and environmental factors (World Health Organization 2006). The definition for migrants used was defined in the previous section. All migrant sub-groups, study designs and health outcomes were included. Detailed inclusion criteria can be seen in Appendix C. Three reviewers (RB, CZ, PP) double screened all titles and abstracts using Covidence systematic review software. Two reviewers (RB and IE) screened the full texts. Any discrepancy was resolved in a panel discussion between the authors involved.
Charting, collating, summarising and reporting the results
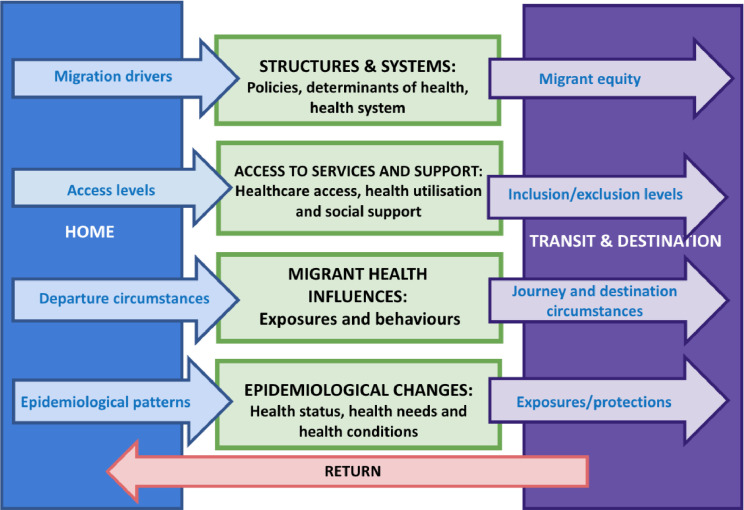
Two reviewers (RB, IE) independently double extracted data on the following fields: study location (country, National Health Service (NHS) region of England, and city where available), study design and size, year of publication, journal, institution and country of first author, migrant sub-group, migrant country of origin, health domain and outcome. Consensus was reached collaboratively between reviewers. We used the stated study rationale, aims and/or objectives of each paper to identify the migrant sub-groups and main health research groupings. The health outcomes were then mapped onto the four domains (green boxes in Fig. 1) of an adapted version of the University College London(UCL)-Lancet Commission on Migration and Health Conceptual Framework on Migration and Health: (1) structures and systems (policies, determinants of health and health system, 2) access to services and support (healthcare access, healthcare use and behaviour, 3) migrant health influences (exposures and behaviours), and (4) epidemiological changes (health status and health needs) (Abubakar et al., 2018). Outcomes were placed into multiple domains where relevant. For example, a study about mental trauma would be categorised into both ‘migrant health influences’ as an exposure and ‘epidemiological changes’ as a mental health outcome. For year of publication, study location and migrant country of origin, the number of studies included in the review were compared to the UK Office of National Statistics (ONS) migrant population size estimates over the study period. Similarly, the number of studies on specific International Classification of Disease - Tenth Revision (ICD-10) disease categories were compared to their corresponding standardised mortality ratios (SMR) estimates from a systematic review and meta-analysis on mortality for international migrants (Aldridge et al., 2018).
Fig. 1.
Four domains (green boxes) adapted from the UCL-Lancet Commission Conceptual Framework of Migration and Health. Blue arrows represent the migration-related influences from place of origin or home. Purple arrows represent migration-related influences that emerge or change at a transit stage and/or in the destination. Health topics for this study were only assessed in the UK as the destination country.
Results
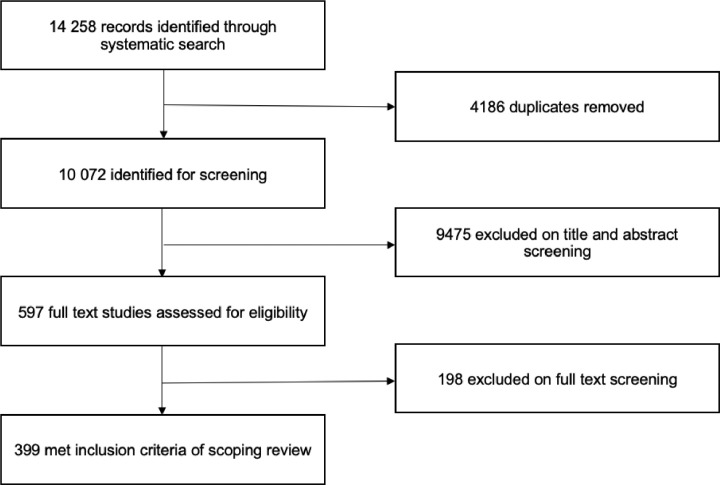
We identified 14 258 articles, of which 4186 studies were duplicates, leaving 10 072 studies to be screened. 597 full text articles were reviewed for eligibility (14 studies could not be assessed), of which 399 met the full inclusion criteria (Fig. 2). References for all included studies are listed in Appendix D. No studies published in 2001 were included as all used data collected before 2001.
Fig. 2.
Study selection.
Findings
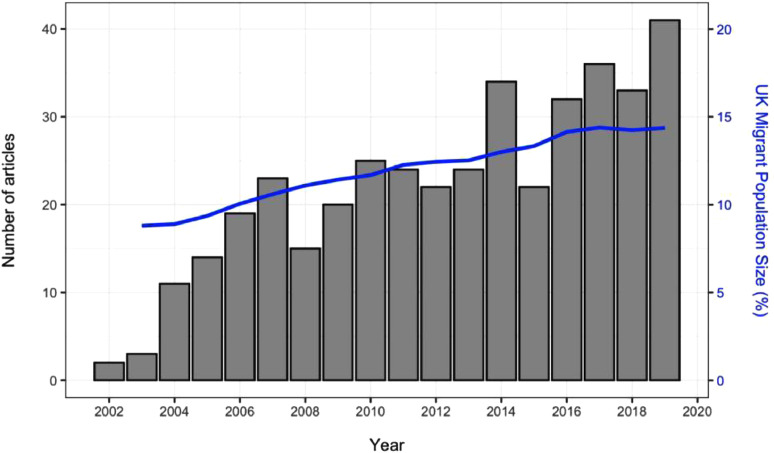
Publication trends in UK migration health research
The publication rate of migration health research in the UK has steadily increased since 2001, reflecting the national trend of an increasing proportion of migrants in the total UK population (Fig. 3). More than a third of the studies (41.1%; 164/399) were published in the final five years of our 19-year study period (2015 and 2019).
Fig. 3.
Migration health research publications in the UK between 2001 and 2019. Migrant population size as a percentage of the total UK population is marked in the blue line.
Migration health research was published in a diverse range of journals. In total, 208 different journals published UK migration health research from 2001 to 2019. This heterogeneity can be seen in the top ten most published in journals shown in Table 1.
Table 1.
Top 10 journals publishing migration health research by number and percentage of articles (n = 399) in the UK between 2001 and 2019.
| Journal | Number of articles N (%) |
|---|---|
| Public Health | 14 (3.5) |
| Social Science and Medicine | 11 (2.7) |
| Ethnicity and Health | 9 (2.3) |
| European Journal of Public Health | 9 (2.3) |
| Journal of Public Health | 9 (2.3) |
| PLOS One | 9 (2.3) |
| BMC Health Services Research | 8 (2.0) |
| International Journal of STD and AIDS | 8 (2.0) |
| BMJ Open | 7 (1.8) |
| Clinical Child Psychology and Psychiatry | 7 (1.8) |
Research was predominantly conducted by first author researchers with at least one affiliation at an institution in England (90.0%; 359/399), with a few exceptions including Scotland (8.5%; 34/399), the United States of America (4.8%; 19/399) and the Netherlands (4.3%; 17/399). Although migration health research was conducted by a wide range of different first author institutions (214 in total), half of the top ten were based in London. The most active institutions were University College London (9.5%; 38/399), King's College London (6.3%; 25/399), the London School of Hygiene and Tropical Medicine (4.3 17/399) and Imperial College London (3.3%; 13/400) (Table 2). Most first authors were based at a university (76.9%; 307/399) while a minority were from an NHS trust or hospital (8.0%; 32/399) or associated with both a university and an NHS trust or hospital (4.5%; 18/399).
Table 2.
Top 10 first author institutions publishing migration health research by number and percentage of articles (n = 399) in the UK between 2001 and 2019.
| Institution* | Number of articles N (%) |
|---|---|
| University College London | 38 (9.5) |
| King's College London | 25 (6.3) |
| The London School of Hygiene and Tropical Medicine | 17 (4.3) |
| Imperial College London | 17 (4.3) |
| University of Oxford | 13 (3.3) |
| Queen Mary University | 12 (3.0) |
| University of Manchester | 12 (3.0) |
| University of Amsterdam | 11 (2.8) |
| University of Edinburgh | 10 (2.5) |
| University of Birmingham | 9 (2.3) |
Each affiliation of multi-affiliated first authors was included separately.
Migration health research in the UK
The majority of studies were conducted in England (72.9%; 291/399), with 8.5% (34/399) in Scotland, 7.3% (29/399) in Wales and 1.5% (6/399) in Northern Ireland. One in five studies (19.1%; 76/399) did not specify a location more specific than the United Kingdom. The distribution of study locations varied in how well they related to the proportion of migrants living in the country or region between 2001 and 2019 (Table 3). While a third of studies were conducted in London, where one in three migrants in the UK lived, a majority of other regions in England such as the North West, West Midlands, South East, East of England, the East Midlands and the South West were underrepresented in the literature, meaning they had comparatively less migration health research but higher proportions of migrants to the total migrant population and the total UK population of each region during the study period. Scotland and Wales were overrepresented in the literature while Northern Ireland had an equal proportion of articles to migrant population size but not to total population size.
Table 3.
Country and region in the UK where migration health research was conducted by number and percentage of articles (n = 399), average migrant population size as a percentage of the total UK migrant population and average migrant population size as a percentage of the total population in each location between 2001 and 2019.
| Country | Region | Number of articles* N (%) | Migrant pop. of total UK migrant pop.⁎⁎% | Migrant pop. of total pop. in each location⁎⁎% |
|---|---|---|---|---|
| England | 291 (72.9) | 92.1 | 12.7 | |
| London | 137 (34.3) | 38.0 | 34.0 | |
| Yorkshire & Humberside | 22 (5.5) | 5.7 | 7.9 | |
| North West | 21 (5.3) | 7.2 | 7.5 | |
| West Midlands | 19 (4.8) | 8.1 | 10.5 | |
| South East | 12 (3.0) | 12.7 | 10.8 | |
| East | 9 (2.3) | 8.0 | 10.0 | |
| East Midlands | 8 (2.0) | 5.7 | 9.2 | |
| North East | 8 (2.0) | 1.6 | 4.6 | |
| South West | 7 (1.8) | 5.1 | 7.1 | |
| Scotland | 34 (8.5) | 4.5 | 6.2 | |
| Wales | 29 (7.3) | 2.0 | 4.9 | |
| Northern Ireland | 6 (1.5) | 1.4 | 5.8 |
Percentages in the number of articles column do not add up to 100% because each article could have recorded more than one study location.
Data from the UK Office of National Statistics between 2001 and 2019.
The spatial distribution of study locations at the city-level was skewed towards larger urban centres. Out of a total of 33 cities identified in the studies which specified a location, a third of studies were conducted in London (34.1%; 136/399), followed by Birmingham, Manchester and Glasgow (Table 4). With the exception of London, the proportion of migrants out of the total population living in each city did not consistently reflect where research activity was focused. Notably, almost one in three people living in Luton was a migrant where only 4 studies were conducted during the study period. Eight of the top 10 cities with the most research had a higher proportion of migrants than the UK national average (11.6%), however all bar London had less than 5 percent of the total migrant population.
Table 4.
Top 10 UK cities where migration health research was conducted by number and percentage of articles (n = 399), average migrant population size as a percentage of the total UK migrant population and average migrant population size as a percentage of the total population in each city between 2001 and 2019. Data from the UK Office of National Statistics and National Records of Scotland.
| City | Number of articlesN (%) | Migrant pop. of total UK migrant pop⁎⁎% | Migrant pop. of total pop. in each city⁎⁎% |
|---|---|---|---|
| London | 136 (34.1) | 38.0 | 34.0 |
| Birmingham | 12 (3.0) | 3.1 | 20.8 |
| Manchester | 11 (2.8) | 4.0 | 11.04 |
| Glasgow | 9 (2.8) | 0.9 | 12.2 |
| Bradford | 7 (1.8) | 1.0 | 14.5 |
| Edinburgh | 6 (1.5) | 0.9 | 15.0 |
| Leeds | 5 (1.3) | 1.1 | 10.7 |
| Bristol | 4 (1.0) | 0.7 | 12.3 |
| Dunstable* | 4 (1.0) | 0.3 | 7.5 |
| Luton | 4 (1.0) | 0.8 | 29.0 |
Data for Bedfordshire as Dunstable not available.
Data from the UK Office of National Statistics between 2001 and 2019.
Migration health research methodology shifted to include more qualitative and mixed method study designs and more multi-country comparative studies over the study period. Although in total there were less qualitative (33.8%; 135/399) and mixed methods (11.0%; 44/399) studies than quantitative studies (55.1%; 220/399) over the entire study period, almost half of the qualitative (46.7%; 63/135) and mixed method (41.0%; 18/44) studies were published in the last five years (2015 - 2019) of the study period compared to a third of quantitative studies (37.0%; 83/221). Similarly, more than half of multi-country comparative studies (60.3%; 44/73), where the target migrant population in the UK or any one of its devolved nations is compared to other countries, were published in the last five years of the study period.
When examining research study size, the number of study participants included in each study was skewed towards smaller numbers (Table 5). Almost a third (35.8%; 143/399) of the studies had less than 50 research participants. Large size datasets with more than 10,000 participants were less common (10.5%; 42/399).
Table 5.
Number of study participants by number of articles and percentage of articles (n = 399).
| Number of study participants | Number of articles N (%) |
|---|---|
| <50 | 143 (35.8) |
| 50–100 | 52 (13.0) |
| 101–500 | 107 (26.8) |
| 501–1500 | 26 (6.5) |
| 1501–10,000 | 20 (5.0) |
| >10,000 | 42 (10.5) |
| Missing or not relevant* | 9 (2.3) |
No participants in study or total not recorded.
Typology of migrants
In terms of how studies classified their target migrant population, the majority of studies (74.9%; 299/399) used a broad term for ‘migrant’ (e.g., immigrant, foreign-born, or first-generation) rather than a specific migrant sub-group categorisation. Where migrant sub-group classifications were available, forced migrants were the most commonly specified type of migrant. This includes asylum seekers (14.8%; 59/399), refugees (12.3%; 49/399), and unaccompanied asylum-seeking minors (3.3%; 13/399). The least specified sub-groups were those detained in immigration detention, labour migrants and family visa migrants (Table 6). Examining the studies by sex, one in five studies focused only on female migrants (20.8%; 83/399) while few studies (4.5%; 18/399) were on male migrants only.
Table 6.
Migrant sub-group specified as study population by number and percentage of articles (n = 399).
| Migrant group | Number of articles* N (%) |
|---|---|
| Unspecified migrant^ | 299 (74.9) |
| Asylum seeker | 59 (14.8) |
| Refugee | 49 (12.3) |
| Undocumented or insecure status | 14 (3.5) |
| Unaccompanied asylum-seeking children | 13 (3.3) |
| Trafficked | 11 (2.8) |
| International student | 9 (2.3) |
| Detainee | 7 (1.8) |
| Migrant worker | 4 (1.0) |
| Family | 1 (0.25) |
Percentages do not add up to 100% because each article could have specified more than one migrant sub-group.
Unspecified migrant was used in the studies to classify those described as international migrant, immigrant, born abroad, new entrant, foreign-born, foreign national, first-generation migrant, or by their country of birth.
While migrant study populations originated from a wide range of countries (156 in total), most studies included participants from a limited number of countries - Pakistan (17.3% of studies; 69/399), India (16.8%; 67/399), Somalia (15.3%; 61/399), Bangladesh (15.3%; 61/399,400), Nigeria (12.3%; 49/399) and Poland (11.3%; 45/399). More broadly, almost half of the studies involved migrants from Africa (44.9%; 179/399) and a third involved migrants from South Asia (34.1%; 136/399) and Europe and Central Asia (33.6%; 134/399) (Table 7).
Table 7.
World Bank region of origin for migrants by number and percentage of articles (n = 399).
| Region^ | Number of articles* N (%) |
|---|---|
| Africa | 179 (44.9) |
| South Asia | 136 (34.1) |
| Europe and Central Asia | 134 (33.6) |
| East Asia and Pacific | 67 (16.8) |
| Middle East and North Africa | 65 (16.3) |
| Caribbean | 46 (11.5) |
| South and Central America | 43 10.8) |
| Asia | 35 (8.8) |
| North America | 12 (3.0) |
Percentages do not add up to 100% because each article could have more than one migrant region of origin.
Eastern Mediterranean and Stateless regions were removed as totals were less than 10.
Pakistan, India, Bangladesh, Nigeria, Poland and China were in the top ten countries of origin when ranked by both the number of articles and the average ONS population size of migrants from each country of origin in the UK between 2001 and 2019 (Fig. 4). Eight of the top ten countries of origin in the ranking by number of articles were found to have a lower rank when ordered by population size in the UK (blue lines), meaning more research was conducted on migrants from these countries relative to their proportionate population size. Conversely, large migrant population sizes from countries of origin such as Ireland, Germany, South Africa and the United States of America were underrepresented in research production (red lines).
Fig. 4.
Comparison of the top ten rank position of migrant country of origin when ordering by number of articles and ONS average population size between 2001 - 2019. Blue lines correspond to a higher rank position in the number of articles compared to population size. Red lines correspond to a lower rank position when ordering by the number of articles compared to population size.
Health outcomes in migration health research
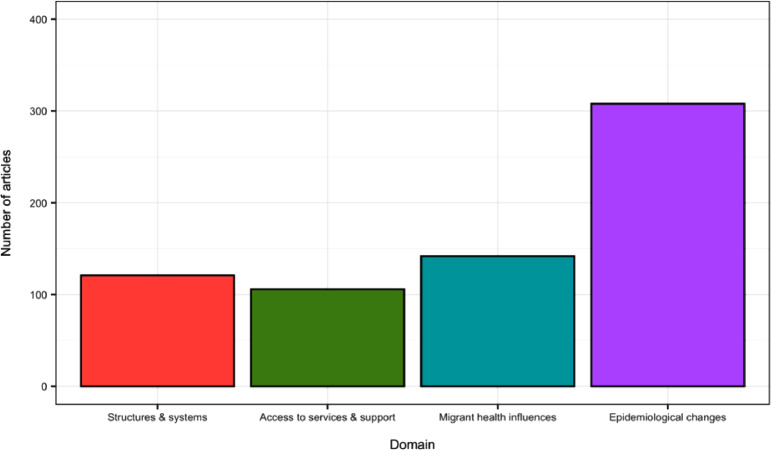
Although a diverse number of outcomes were identified (102 in total), a majority of studies (81.9%; 327/399) included at least one outcome in the epidemiological changes domain (Fig. 5), which were predominately classified by ICD-10 categories. Over a quarter of all studies included at least one outcome in structures and systems (27.8%; 111/399) and access to services and support (26.3%; 105/399) while a third of studies included one outcome in migrant health influences (35.3%; 141/399).
Fig. 5.
Number of articles with at least one outcome in each of the four domains. Note: Studies often included outcomes in more than one domain.
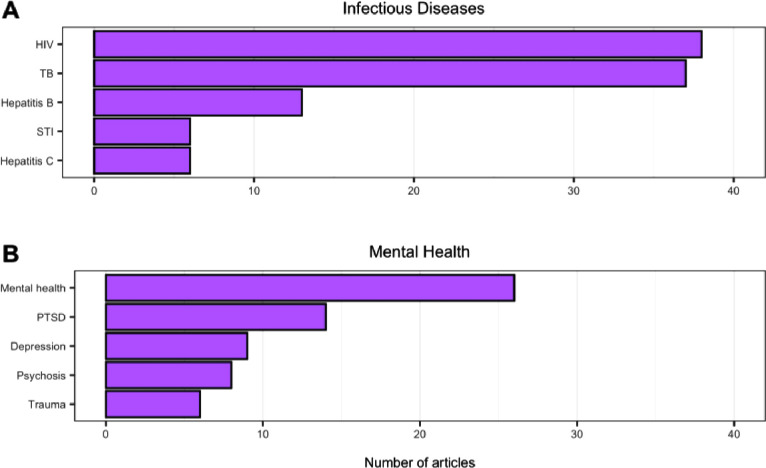
The most studied health topics in migration health research were specific disease outcomes compared to systems or structures that impact health, access to healthcare, or specific exposures or behaviours (Fig. 6). Notably, infectious diseases and mental health, comprising 24.3% (97/399) and 19.1% (76/399) of studies respectively, were the highest researched outcomes in the epidemiological changes domain as well as in the entire review (Fig. 6D). This was also reflected within the systems and structures domain (Fig. 6A), whereby the first and third most researched outcomes (screening and testing respectively) involved health system components associated with the control of infectious diseases within migrants.
Fig. 6.
Top 5 health outcomes within each domain. Note that panel D has a different x-axis scale to panels A - C.
The infectious disease studies were skewed towards specific conditions while the mental health studies were often not further classified. Human Immunodeficiency Virus (HIV) and tuberculosis (TB) were the most studied infectious diseases and outcomes in the entire study (Fig. 7A) while mental health (not classified further) was the most researched mental health outcome and third most studied outcome in any domain (Fig. 7B). The remaining top mental health outcomes included conditions associated with trauma such as post-traumatic stress disorder (PTSD) and measuring mental trauma itself.
Fig. 7.
Top 5 infectious disease (A) and mental health (B) outcomes in terms of number of articles. Note that the outcome of mental health in 7B is a general measure of mental health.
Infectious disease studies predominantly focused on populations classified as unspecified ‘migrants’ while studies on mental health tended to concentrate on forced migrants. For example, almost all studies on infectious diseases were on unspecified ‘migrants’ (89.5%, 85/95) with a limited number of studies on asylum seekers (11.5%, 11/96) and refugees (3.1%, 3/96). Conversely, a majority of studies on unaccompanied asylum-seeking children (76.9%, 10/13), more than half of the studies on refugees (51.0%, 25/49) and more than a third on asylum seekers (39.0%, 23/59) focused on at least one mental health outcome with only 33 studies (11.0%, 33/299) on unspecified ‘migrants’ including a mental health outcome.
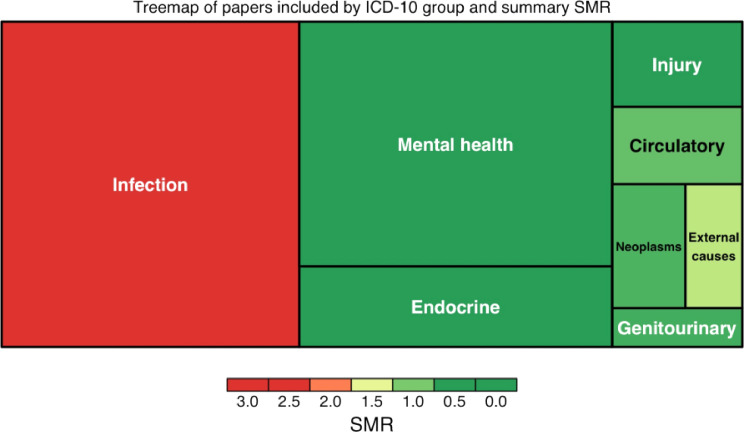
To assess how the research priorities (i.e. the number of studies by disease outcome) related to the relative burden of disease in migrants, we compared the number of studies on specific ICD-10 disease categories with their corresponding summary SMR estimates by ICD-10 category for international migrants (Aldridge et al., 2018) (Fig. 8). Two ICD-10 disease categories had SMR estimates higher than 1, infectious diseases (2.38) and external causes of mortality (1.28), suggesting migrants had higher mortality than the host population. Infectious diseases were the most researched outcome in this review and the highest cause of mortality for international migrants globally, suggesting a good balance between its prioritisation within the research landscape and its relative impact on the health of migrants. However, even with an elevated SMR, external causes of mortality were less researched compared to other ICD-10 categories with lower SMRs such as neoplasms, circulatory and endocrine outcomes.
Fig. 8.
Treemap of studies included by ICD-10 group and summary SMR. Area represents the number of studies in each ICD-10 category. Colour corresponds to previously published SMRs specific to migrants for each ICD-10 category.
Discussion
Migration health research and publication trends in the UK
Almost half of the studies concerning migration health in the UK were published between 2015 and 2019, demonstrating a linear increase in the rate of research generation that is consistent with global migration health research trends (Sweileh et al., 2018). This progression is likely due to an increase in both research production in the UK and levels of national and global international migration (Migration Statistics Quarterly Report: May 2020; Indicators, 2018). While this growth in research is promising, ensuring a diverse geographic distribution across the UK is important for a nuanced and region-specific understanding of migration health. Our findings highlight a need for more research in most regions of England especially the South East, the East, the East Midlands and the South West where migrant populations have been understudied compared to the proportion of each region's migrant population to both the total UK migrant population and the region's total population. At the city-level, research was predominantly conducted in larger urban settings where most migrants tend to live, revealing a gap in the evidence-base about the health of migrants in more rural contexts. Clearly, relative migrant population size should not be the only consideration for research prioritisation. It is also important to take into account the distinct health needs of migrants and their access to healthcare in different settings, for example, rural and urban contexts or areas with new and established migrant communities.
Migrant typologies
Most studies did not disaggregate the studied migrant population by migrant sub-group, as has been found in several other scoping or systematic reviews on migrants (Villarroel et al., 2019; Sweileh et al., 2018). This is problematic given important differences in the experience of the migration process between migrant sub-groups. This finding supports the call to standardise migrant sub-group definitions to improve comparability between contexts while still recognising the nuances inherent in human mobility (Abubakar et al., 2018; Wickramage et al., 2018). Disaggregation of migration data by migrant sub-group status as well as sex and age are needed to strengthen the evidence-base on the specific health needs, interventions and appropriate service delivery for different migrant populations (Gazard et al., 2015). Furthermore, evidence disaggregated by migration sub-group is better suited to inform policy generation as policies tend to target migrant groups according to their immigration status. When migrant sub-group was specified, the most common classification was asylum seekers and refugees. Few studies explicitly focused on undocumented migrants and even fewer on migrant workers. This finding highlights a need for further research and more comprehensive (yet secure) reporting on these underrepresented migrant groups as seen in reviews (Sweileh et al., 2018).
Health outcomes in migration health research
The most researched health outcomes for migrants were infectious diseases, specifically HIV and TB, as found in similar reviews conducted in Europe and globally (Sweileh et al., 2018; Roura et al., 2015). This finding reflects a complex relationship between infectious diseases and migration. Research over the past 20 years has revealed how dominant discourses framing migrants as vectors of disease could have driven the volume of infectious disease research (World Health Organization 2016). Evidence shows that some migrants may have a significant burden of infectious diseases depending on disease prevalence in their country of origin and exposure to adverse conditions prior to and after arrival in the UK (Wagner et al., 2014). However, migrants pose a negligible risk of spreading infectious diseases into the general host population (Aldridge et al., 2016). Future research and evidence-based policy action should therefore focus on improving health outcomes for migrants with infectious diseases given the significant burden and higher risk of mortality while also extending their studies to explore larger barriers to healthcare and structural determinants of health.
Mental health was the second most researched health outcome, specifically PTSD, depression, psychosis and trauma. The majority of studies examining mental health in the UK focused on forced migrants. This is expected given the adverse impacts of escaping conflict or persecution, the conditions surrounding the migration journey and navigating the socioeconomic, legal and structural barriers in the UK on an individual's mental health status (Heptinstall et al., 2004; Palmer and Ward, 2007; Sen et al., 2018). However, there was an absence of mental health research on other migrant sub-groups like migrant workers who potentially experience some of these barriers upon arriving and living in the UK. A systematic review found that migrant workers experience anxiety, depression and alcohol and substance abuse due to marginalisation and strenuous work (Mucci et al., 2020). As most people migrate to the UK to work, it is essential to understand their current burden of mental health conditions, access to mental health services and the role of occupational health medicine.
The prevailing focus on specific disease outcomes by the studies included in this review reveals how migration health research in the UK has concentrated less on exposures and behaviours that influence migrant health as well as on examining migrants’ access to services. A minority of studies (less than 5%) explored health behaviour, health beliefs and traditional medicine despite their importance for the provision of culturally competent healthcare (Napier et al., 2014) and understanding healthcare usage. Although healthcare utilisation was the third most studied outcome in the review, its domain overall (access to services and support) was the least researched. This is surprising given how understanding migrant healthcare access and experience is critical to planning health services and reducing barriers to access. Despite all residents in England regardless of immigration status being entitled to access primary care, a few studies showed that some migrants struggle to register with a General Practice, lack knowledge of their entitlement or even fear arrest when accessing NHS services (Fang, 2015; Kang et al., 2019; Weller et al., 2019). In terms of secondary care where non-urgent treatment is chargeable for those who cannot prove their entitlement, research has shown that some migrants have been denied urgent care or received delayed treatment (Potter et al., 2020; Doctors of the World 2020). To bridge the gap between policy and practice, future research is needed to build a stronger evidence base on both the facilitators and barriers to migrant healthcare access at all levels.
Examining how structures and systems impact migrants’ health has become increasingly important within the context of England's growing number and breadth of policies aiming to embed immigration control within public services like the NHS (Griffiths and Yeo, 2021). Sharing data between the Home Office and public services (e.g., a patient's hospital bill, a victim's report of a crime, or a worker's report of employer abuse) for immigration enforcement has garnered distrust and fear within some migrant communities (Weller et al., 2019; Delvino, 2020). Furthermore, migrants without recourse to public funds cannot receive welfare such as income support, school lunch subsidies or homelessness assistance (Weller et al., 2020, Delvino, 2020). Future research on migration health should work to disentangle how these policies impact health and how they both foster and reinforce barriers to health and social care through human rights based, intersectional and transdisciplinary approaches to research (Spitzer et al., 2019).
Implications for future migration health research
Future migration health research must work to address the methodological challenges and research gaps identified in this review to better understand the health needs of migrants in the UK. First, research should use the globally accepted definitions of migrant sub-groups in data collection, with a recognition that these categorises are dynamic. More broadly, further disaggregation of data on migrants based on socio-demographic factors (e.g., gender and livelihood) and migration indicators (e.g., length of residence in host country and entry visa category) will allow for improved comparability between contexts and a more holistic understanding of an individual's migration trajectory. Second, researchers should ensure a diverse geographic distribution of research in the UK to capture the region-specific health profiles and service delivery requirements. Third, health research on migrants must address the paucity of evidence on the social determinants of health, access to and use of healthcare and exposures and behaviours that influence migrant health. Future studies must work to better understanding the structural and social factors that place some migrants at risk but also those that facilitate resilience and good health. Lastly, meaningful engagement, participatory research approaches and co-production with migrant communities throughout the entire research process is critical to ensure priorities and methodologies meet their needs and do not result in harm. Collaborative research approaches offer the opportunity to jointly identify research gaps, co-produce knowledge through the establishment of funded peer researcher roles and disseminate findings in ways that create sustainable change.
Limitations
There are a few limitations of this scoping review. We only searched two databases and were thus limited to the studies included within our search capacity. The databases searched did not include grey literature. As a result, there may be research on migration health that we have not identified. The review only included studies with a primary focus on migrants as stated explicitly in its aims, rationale or objectives. Therefore, studies that examined migrants as part of secondary analyses or stratified by migration were not included. Similarly, only health topics that were specifically mentioned in the aims, rationale or objectives sections of included studies were extracted. Other health topics or outcomes mentioned in other sections of a study (e.g., an outcome not described in the study's aim or rationale but was included in results) were not extracted.
Conclusion
Our scoping review identifies important research trends over the last 20 years and provides an evidence-base for future research prioritisation of migration health in the UK. We found that much of the research has focused on specific health outcomes while structural and systemic determinants of health were under-researched. These findings will enable researchers, policy makers and non-governmental organisations to embed evidence within their practice and policy formation. It will also help them to critically engage with the body of migration health evidence in the UK to understand why some areas of migration health research are over or underrepresented.
Declaration of Competing Interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Footnotes
This figure does not account for undocumented migrants in the UK, for whom no accurate population estimate exists.
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jmh.2021.100061.
Appendix. Supplementary materials
References
- 1.Population of the UK by country of birth and nationality - Office for National Statistics n.d. https://www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/internationalmigration/datasets/populationoftheunitedkingdombycountryofbirthandnationality, 2020.
- Kierans D., Who migrates to the UK and why? n.d. https://migrationobservatory.ox.ac.uk/resources/briefings/who-migrates-to-the-uk-and-why/, 2020.
- Czaika M., de Haas H., Determinants of Migration to the UK n.d. https://migrationobservatory.ox.ac.uk/resources/briefings/determinants-of-migration-to-the-uk/, 2020.
- Migration Statistics Quarterly Report: May 2020. Office of National Statistics; n.d.
- Abubakar I., Aldridge R.W., Devakumar D., Orcutt M., Burns R., Barreto M.L. The UCL-lancet commission on migration and health: the health of a world on the move. Lancet. 2018;392:2606–2654. doi: 10.1016/S0140-6736(18)32114-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallace M., Kulu H. Mortality among immigrants in England and Wales by major causes of death, 1971-2012: a longitudinal analysis of register-based data. Soc. Sci. Med. 2015;147:209–221. doi: 10.1016/j.socscimed.2015.10.060. [DOI] [PubMed] [Google Scholar]
- O'Donnell C.A., Higgins M., Chauhan R., Mullen K. “They think we're OK and we know we're not”. A qualitative study of asylum seekers’ access, knowledge and views to health care in the UK. BMC. Health Serv. Res. 2007;7:75. doi: 10.1186/1472-6963-7-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradby H., Humphris R., Newall D., Phillimore J., Public health aspects of migrant health: a review of the evidence on health status for refugees and asylum seekers in the European Region. 2015. [PubMed]
- Napier A.D., Ancarno C., Butler B., Calabrese J., Chater A., Chatterjee H. Culture and health. Lancet. 2014;384:1607–1639. doi: 10.1016/S0140-6736(14)61603-2. [DOI] [PubMed] [Google Scholar]
- Burns R., Pathak N., Campos-Matos I., Zenner D., Katikireddi S.V., Muzyamba M.C. Million Migrants study of healthcare and mortality outcomes in non-EU migrants and refugees to England: analysis protocol for a linked population-based cohort study of 1.5 million migrants. Wellcome Open Res. 2019;4 doi: 10.12688/wellcomeopenres.15007.1. 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Migration and health n.d. https://migrationdataportal.org/themes/migration-and-health accessed March 4, 2021.
- Arksey H., O'Malley L. Scoping studies: towards a methodological framework. Int. J. Soc. Res. Methodol. 2005;8:19–32. [Google Scholar]
- Tricco A.C., Lillie E., Zarin W., O'Brien K.K., Colquhoun H., Levac D. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann. Intern. Med. 2018;169:467–473. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- Aldridge R.W., Nellums L.B., Bartlett S., Barr A.L., Patel P., Burns R. Global patterns of mortality in international migrants: a systematic review and meta-analysis. Lancet. 2018;392:2553–2566. doi: 10.1016/S0140-6736(18)32781-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Villarroel N., Hannigan A., Severoni S., Puthoopparambil S., MacFarlane A. Migrant health research in the Republic of Ireland: a scoping review. BMC Public Health. 2019;19:1–10. doi: 10.1186/s12889-019-6651-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . WHO; Geneva, Switzerland: 2006. Constitution of the World Health Organization-Basic Documents, Supplement. October 2006. [Google Scholar]
- Sweileh W.M., Wickramage K., Pottie K., Hui C., Roberts B., Sawalha A.F. Bibliometric analysis of global migration health research in peer-reviewed literature (2000-2016) BMC Public Health. 2018;18:777. doi: 10.1186/s12889-018-5689-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Indicators G.M. International Organization for Migration; Berlin: 2018. Global Migration Data Analysis Centre. [Google Scholar]
- Wickramage K., Vearey J., Zwi A.B., Robinson C., Knipper M. Migration and health: a global public health research priority. BMC Public Health. 2018;18:1–9. doi: 10.1186/s12889-018-5932-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gazard B., Frissa S., Nellums L., Hotopf M., Hatch S.L. Challenges in researching migration status, health and health service use: an intersectional analysis of a South London community. Ethn. Health. 2015;20:564–593. doi: 10.1080/13557858.2014.961410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roura M., Domingo A., Leyva-Moral J.M., Pool R. Hispano-Americans in Europe: what do we know about their health status and determinants? A scoping review. BMC Public Health. 2015;15:472. doi: 10.1186/s12889-015-1799-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization The migration and health. Lancet Infect. Dis. 2016;16:867. doi: 10.1016/S1473-3099(16)30218-3. [DOI] [PubMed] [Google Scholar]
- Wagner K.S., Lawrence J., Anderson L., Yin Z., Delpech V., Chiodini P.L. Migrant health and infectious diseases in the UK: findings from the last 10 years of surveillance. J. Public Health. 2014;36:28–35. doi: 10.1093/pubmed/fdt021. [DOI] [PubMed] [Google Scholar]
- Aldridge R.W., Zenner D., White P.J., Williamson E.J., Muzyamba M.C., Dhavan P. Tuberculosis in migrants moving from high-incidence to low-incidence countries: a population-based cohort study of 519 955 migrants screened before entry to England, Wales, and Northern Ireland. Lancet. 2016;388:2510–2518. doi: 10.1016/S0140-6736(16)31008-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heptinstall E., Sethna V., Taylor E. PTSD and depression in refugee children. Eur. Child Adolesc. Psychiatry. 2004;13:373–380. doi: 10.1007/s00787-004-0422-y. [DOI] [PubMed] [Google Scholar]
- Palmer D., Ward K. “Lost”: listening to the voices and mental health needs of forced migrants in London. Med. Confl. Surviv. 2007;23:198–212. doi: 10.1080/13623690701417345. [DOI] [PubMed] [Google Scholar]
- Sen P., Arugnanaseelan J., Connell E., Katona C., Khan A.A., Moran P. Mental health morbidity among people subject to immigration detention in the UK: a feasibility study. Epidemiol. Psychiatr. Sci. 2018;27:628–637. doi: 10.1017/S2045796017000269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mucci N., Traversini V., Giorgi G., Tommasi E., De Sio S., Arcangeli G. Migrant workers and psychological health: a systematic review. Sustain. Sci. Pract. Policy. 2020;12:120. [Google Scholar]
- Fang M.L., Experiencing “pathologized presence and normalized absence”; understanding health related experiences and access to health care among Iraqi and Somali asylum seekers, refugees and persons without legal status 2015:12. [DOI] [PMC free article] [PubMed]
- Kang C., Tomkow L., Farrington R. Access to primary health care for asylum seekers and refugees: a qualitative study of service user experiences in the UK. Br. J. Gen. Pract. 2019;69:e537–e545. doi: 10.3399/bjgp19X701309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weller S.J., Crosby L.J., Turnbull E.R., Burns R., Miller A., Jones L. The negative health effects of hostile environment policies on migrants: a cross-sectional service evaluation of humanitarian healthcare provision in the UK. Wellcome Open Res. 2019;4:109. doi: 10.12688/wellcomeopenres.15358.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weller et al., 2020. Assessing and Supporting children and families who have no recourse to public funds (NRPF) n.d, 2020. http://guidance.nrpfnetwork.org.uk/reader/practice-guidance-families/eligibility-for-other-services/.
- Potter J.L., Burman M., Tweed C.D., Vaghela D., Kunst H., Swinglehurst D. The NHS visitor and migrant cost recovery programme-a threat to health? BMC Public Health. 2020;20:1–9. doi: 10.1186/s12889-020-08524-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doctors of the World. Delays & Destitution: an Audit of Doctors of the World's Hospital Access Project (July 2018-20). 2020.
- Griffiths M., Yeo C. The UK's hostile environment: deputising immigration control. Crit. Soc. Policy. 2021 0261018320980653. [Google Scholar]
- Delvino N., When a crime victim is an irregular migrant: “safe reporting of crime” or “leap of faith”?, https://www.compas.ox.ac.uk/2019/when-a-crime-victim-is-an-irregular-migrantsafe-reporting-of-crime-or-leap-of-faith/, 2020.
- Spitzer D.L., Torres S., Zwi A.B., Khalema E.N., Palaganas E. Towards inclusive migrant healthcare. BMJ. 2019;366:l4256. doi: 10.1136/bmj.l4256. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.