Cardio-oncology is a growing field that encompasses managing cardiotoxic effects of oncologic therapies and preventing cardiovascular (CV) disease in patients with cancer and survivors. The development of novel treatments and the emergence of atypical CV complications has created a need for subspecialty care (1, 2, 3). However, training in cardio-oncology is limited. A nationwide survey of CV fellowships revealed that only 11% of institutions included cardio-oncology lectures in their curriculum (4). As of 2019, among a survey of 109 CV fellowship programs, only 9 had training opportunities in cardio-oncology (3).
To fulfill an educational gap, the American College of Cardiology (ACC) Cardio-Oncology Council recently published a statement outlining training requirements and core competencies for cardio-oncology subspecialty training among cardiologists and oncologists (5). This document provides a roadmap for levels I to III of training and highlights the necessary components, including didactics, research, institutional support, and an evaluation process. Level I training provides a basic understanding of the evaluation and treatment of cardio-oncology patients through a minimum of 2 to 4 weeks of exposure to cardio-oncology services (5). Level II subspecialty training is appropriate for cardiology fellows who want to independently deliver cardio-oncology care requiring 3 to 6 months of training, a total of 20 half-day cardio-oncology continuity clinics, 2 to 4 days of oncology clinics, and participation in 50 unique inpatient consultations (5). Level II training in other CV specialties, such as imaging, is typically attained during CV fellowship, and similarly, level II cardio-oncology training can be incorporated into a general fellowship. Level III training calls for 6 to 12 months of training, a total of 40 half-day continuity clinics, and participation in 100 unique inpatient consultations (5). In this Viewpoint, we describe how we built training experiences for cardiology trainees in cardio-oncology at 6 institutions, and we provide this perspective within the context of the structure outlined by the ACC Cardio-Oncology Council. Moreover, we review the challenges of creating a program and fulfilling the training requirements needed to educate clinicians in the diagnosis, management, and treatment of the various cardiotoxic effects of malignancies.
Achieving level I competency in cardio-oncology is feasible for internal medicine, cardiology, and hematology/oncology trainees who are participating in programs with established cardio-oncology services. Although often not formalized, general cardiology trainees across the United States all manage cardio-oncology patients through general cardiology clinics and inpatient services. In the United Kingdom, there has been a concerted effort by educators to ensure that all trainees achieve level I competency in cardio-oncology during general cardiology training.
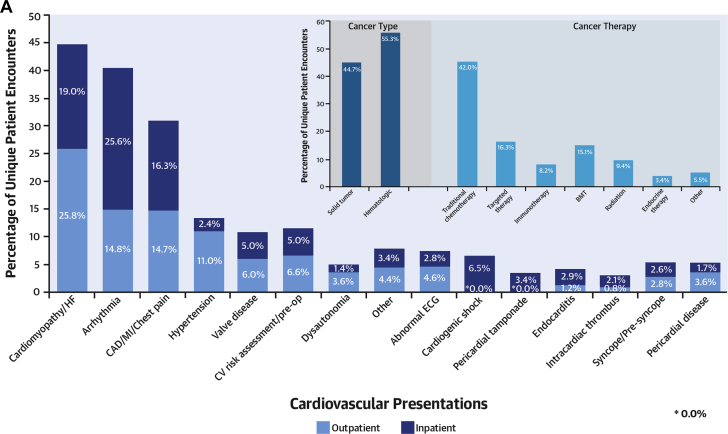
Sixteen graduated fellows from 6 institutions (Mayo Clinic, University of California Los Angeles [UCLA], Emory University, Lahey Hospital and Medical Center, the Ohio State University, and Vanderbilt University Medical Center [VUMC]) completed training commensurate with level II to III competency throughout a 3- to 4-year fellowship between 2014 and 2020. Four of the training institutions had established cardio-oncology programs (Mayo Clinic, UCLA, Lahey Hospital and Medical Center/Dana Farber Cancer Institute/Brigham and Women’s Hospital, and Vanderbilt University Medical Center). All 6 institutions have National Cancer Institute–designated cancer centers. All 16 fellows completed the obligations of a general CV fellow while also incorporating cardio-oncology experiences throughout the fellowship. Trainees met outpatient clinical requirements using different approaches. Some trainees included a half-day cardio-oncology clinic as their continuity clinic, exceeding the recommended 20 half-days of clinic. This offered continuity of care for patients with short- and long-term effects of cancer therapy (Figure 1A). For trainees with obligations at multiple training sites, they alternated the cardio-oncology clinic with other sites weekly. Some trainees pursued elective rotations in subspecialty clinics such as amyloidosis, survivorship, and various oncology services. Additional cardio-oncology clinic time was sought during research electives. Trainees were able to see approximately 100 or more unique patients throughout the fellowship.
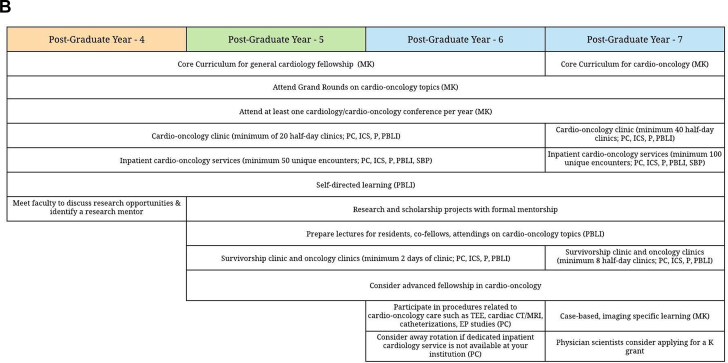
Figure 1.
Characteristics of Cardio-Oncology Clinical Encounters During Training and a Proposed Timeline to Achieve Competency in Cardio-Oncology Training
(A) Distribution of cardiovascular presentations, cancer type, and cancer therapy. Distribution of cardiovascular presentations seen during inpatient and outpatient encounters and the distribution of cancer type and therapy seen during outpatient encounters for 8 fellows at the Mayo Clinic, University of California Los Angeles, Emory University, Lahey Hospital and Medical Center, and The Ohio State University during cardio-oncology training in general cardiology fellowship. Percentages reflect the average percent contribution of each cardiovascular complaint, cancer type, and cancer therapy among all encounters across the 5 institutions. Trainees pursuing cardio-oncology training had a wide range of clinical exposures. (B) Cardio-oncology training sample roadmap. A proposed timeline of the roadmap to achieve level II and level III competency in cardio-oncology clinical care and research during general cardiology training (post-graduate years 4 to 6) and advanced training (post-graduate year 7). ACGME core competencies relevant to each training goal are listed in parentheses. BMT = bone marrow transplant; CAD = coronary artery disease; CHF = congestive heart failure; CT = computed tomography; CV = cardiovascular; ECG = electrocardiogram; EP = electrophysiology; HF = heart failure; ICS = interpersonal and communication skills; MI = myocardial infarction; MK = medical knowledge; MRI = magnetic resonance imaging; P = professionalism; PBLI = practice-based learning and improvement; PC = patient care; pre-op = pre-operative assessment; SBP = systems-based practice; TEE = transesophageal echocardiography.
As one example, VUMC started a formal cardio-oncology fellowship program with level III competency training in 2014 with a total of 8 individuals having completed training by 2020. Trainees rotated between 2 dedicated weekly cardio-oncology clinics, saw new consultations, and followed individual patients throughout the year. Trainees evaluated and devised a plan for at least 2 new consultations per clinic. Additionally, trainees attended rotations in subspecialty clinics such as heart failure and vascular medicine, along with oncology clinics. The additional CV subspecialty and oncology clinics were interspersed throughout the year and cumulatively resulted in at least level III training (5,6). At UCLA, clinic encounters occurred at a range of 1 to 3 different clinical sites, including a dedicated cardio-oncology clinic, a general clinic, and one affiliated with the Veterans Administration.
At Emory University and VUMC, fellows rotated on an inpatient cardio-oncology rotation, while cardio-oncology patients were cared for as part of the general CV consult service at the other institutions. At Emory University, the fellow completed 24 weeks of inpatient service in the bone marrow transplant, medical oncology, and hematology units, treating more than 50 unique patients. At VUMC, fellows rotated on the consultative service throughout the year, seeing 1 or 2 patients per week. The cases seen on the service ranged from immune checkpoint inhibitor–induced myocarditis and arrhythmias to acute heart failure in patients with breast cancer. General CV attendings staffed most of these consults. Without an established cardio-oncology inpatient service, achieving the recommended 3 to 6 months of dedicated cardio-oncology training is challenging. Some trainees participated in the inpatient oncology, hematology, and bone marrow transplant services to enhance their experience. Away rotations at institutions with established inpatient cardio-oncology services can help meet the training requirements.
Understanding the basics in acquisition and interpretation of advanced CV imaging modalities is integral to completing level II or III training in cardio-oncology. At all programs, trainees directly reviewed imaging of cancer treatment–related cardiotoxicity or cardiac tumors with expert readers to supplement their training. Fellows pursuing cardio-oncology training during their general cardiology fellowship were able to concurrently complete either level II or III competency in echocardiography. Many fellows also sought out level II training in cardiac CT, nuclear cardiac imaging, or vascular ultrasound. Two fellows pursued an additional year of advanced training in CV imaging.
Research is another integral part of cardio-oncology and was encouraged in training programs. Level III trainees were each expected to complete at least 1 research project (5). Across all institutions, fellows who completed cardio-oncology as part of their general CV fellowship averaged 5 to 6 months of research. Many of the fellows training at these various institutions were highly productive in manuscript publications and national meeting abstract presentations, and they have successfully launched careers in cardio-oncology.
The cardio-oncology curriculum for trainees seeking level II training during the CV fellowship can be integrated into the cardiology core curriculum. Lectures on multimodality imaging focused on cancer-related complications provide unique value because these are uncommonly encountered during CV training. Fellow-led case-based presentations and journal clubs are other opportunities to provide didactic instruction. Additional monthly or bimonthly dedicated sessions are feasible. Finally, supporting cardio-oncology faculty as grand rounds speakers can enhance the cardio-oncology curriculum and offer trainees the opportunity to network and build new collaborations.
A number of institutions have chosen to organize a fellow-based weekly didactic session covering topics including complications of cancer therapies and survivorship. Each case-based session has included discussing the mechanism of action, identification of cardiotoxicity, testing, and treatment with the cardio-oncology–based faculty participating in the conferences. Trainees at all institutions are encouraged to attend weekly tumor board sessions with oncology as a way for all programs to increase exposure to cancer management. With the increased use of teleconferencing due to the coronavirus disease 2019 pandemic, attendance at many of these conferences has expanded, providing an opportunity to expand didactic sessions to other programs. Beyond didactic instruction, attendance at cardio-oncology–focused national conferences and sessions offers educational and networking opportunities for trainees.
Fellows participating in cardio-oncology training should routinely be evaluated based on the Accreditation Council for Graduate Medical Education core competencies. All trainees are evaluated twice a year in medical knowledge, patient care, practice learning and improvement, interpersonal and communication skills, and professionalism. Trainees should maintain a log of patient encounters and review these with their program director, who can ensure exposure to a large and diverse number of patients.
The International Cardio-Oncology Society (ICOS) has recently developed a certification examination for cardio-oncology. Trainees who have met the requirements for at least level II training should be eligible and prepared to take the ICOS cardio-oncology certification examination following graduation, as is similarly done for other level II competencies. Because the ICOS examination is a recent development, only 1 trainee mentioned here took the test.
Competing clinical obligations were the biggest challenge to pursuing cardio-oncology training during general CV fellowship. Cardio-oncology specialty clinics and inpatient services are typically available only at large tertiary referral centers with comprehensive cancer centers. It can be challenging to maximize clinical time at the centers caring for patients with cancer while also meeting the clinical requirements at other training sites. During a general fellowship, research time is limited and must be pursued without affecting clinical obligations. Given these limitations, clinical research with short-term projects is more feasible than basic or translational science projects.
Funding currently remains a limitation for most institutions in starting a cardio-oncology fellowship. In most cases, incorporating a cardio-oncology year within the third year of the CV fellowship is a practical method to fund a trainee. This allows the trainee to have a clinical focus while using an established funding source. Potential downsides include taking time away from other core CV training, such as imaging rotations or research. Fellows must plan early and carefully to achieve multiple level II competencies during fellowship because pursuing a cardio-oncology track may supplant other concomitant goals.
For trainees interested in pursuing a career in research and level III training, funding through institutional grants may be feasible. At VUMC, trainees were funded through a National Institutes of Health T32 Institutional Award held by both the CV and Oncology Divisions. The benefits of funding through this source are a strong focus on research, with approximately 20% of the time available for clinical work. Despite only 20% of the time available for clinical work, trainees can meet the patient experience criteria recommended by the ACC perspective. Individuals who apply for the T32 Institutional Award can be current CV fellows or individuals who have completed CV or oncological subspecialty training. The limitations of funding through the T32 Institutional Award include the need for a pre-established award at the institution and U.S. citizenship.
Cardio-oncology continues to grow as a field and will benefit from standardization of training (Figure 1B). We have discussed the components of cardio-oncology fellowship at 6 institutions in this Viewpoint. These trainees were able to meet the clinical, research, and evaluation of competency requirements outlined by the perspective with 1 exception: for fellows with no inpatient cardio-oncology service at their institution, it was challenging to accomplish 3 to 6 months of cardio-oncology rotations. However, established continuity of a patient with cancer under cardio-oncology care allows for general fellows to have more exposure through other inpatient general rotations. All fellows had access to a cardio-oncology clinic, trained at institutions with a National Cancer Institute–designated cancer center, and had opportunities to attend multidisciplinary conferences, participate in research, and gain expertise in multimodality imaging. These pre-existing institutional components are essential to comprehensive and robust cardio-oncology training. Securing a source of funding and competing clinical obligations, particularly for trainees who are combining cardio-oncology training with CV training, remain challenges to the cardio-oncology practice. As Hayek et al. (3) discussed, barriers to forming these programs include institutional and financial support, designing an optimal educational curriculum, and varying access to imaging technologies and research programs (3). Although we cannot determine these in other institutions, we believe it is important to begin these discussions today.
Author Disclosures
Dr. Yang has received research funding from CSL Behring. Dr. Moslehi has served a consultant for Bristol Myers Squibb, Takeda, Deciphera, AstraZeneca, Nektar, Audentes Therapeutics, TripleGene, Boston Biomedical, ImmunoCore, Janssen, and Myovant; and is supported by grants from the National Institutes of Health (R01HL144146 and R01HL155990). Dr. Hayek is supported by the National Heart, Lung, and Blood Institute (1R01HL153384-01). All other authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Footnotes
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
Contributor Information
Sherry-Ann Brown, Email: shbrown@mcw.edu.
Eiman Jahangir, Email: Eiman.jahangir@vumc.org.
References
- 1.Miller K.D., Nogueira L., Mariotto A.B. Cancer treatment and survivorship statistics, 2019. CA Cancer J Clin. 2019;69:363–385. doi: 10.3322/caac.21565. [DOI] [PubMed] [Google Scholar]
- 2.Sturgeon K.M., Deng L., Bluethmann S.M. A population-based study of cardiovascular disease mortality risk in US cancer patients. Eur Heart J. 2019;40:3889–3897. doi: 10.1093/eurheartj/ehz766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hayek S.S., Ganatra S., Lenneman C. Preparing the cardiovascular workforce to care for oncology patients: JACC review topic of the week. J Am Coll Cardiol. 2019;73:2226–2235. doi: 10.1016/j.jacc.2019.02.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Barac A., Murtagh G., Carver J.R. Cardiovascular health of patients with cancer and cancer survivors: a roadmap to the next level. J Am Coll Cardiol. 2015;65:2739–2746. doi: 10.1016/j.jacc.2015.04.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Alvarez-Cardona J.A., Ray J., Carver J. Cardio-oncology education and training: JACC council perspective. J Am Coll Cardiol. 2020;76:2267–2281. doi: 10.1016/j.jacc.2020.08.079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lenihan D.J., Hartlage G., DeCara J. Cardio-oncology training: a proposal from the International Cardioncology Society and Canadian Cardiac Oncology Network for a New Multidisciplinary Specialty. J Card Fail. 2016;22:465–471. doi: 10.1016/j.cardfail.2016.03.012. [DOI] [PubMed] [Google Scholar]