Highlights
-
•
The psychological stress and past trauma of refugees often force them to misunderstand the severity of COVID-19.
-
•
The attempts of health care providers and aid agencies in the Rohingya refugee camps are limited to follow international/national guidelines to protect against the COVID-19 outbreak.
-
•
The roles of local mediators to integrate the healthcare policies and the voices of the refugees are crucial to tackling COVID-19.
Keywords: COVID-19, Rohingya refugee, Community resilience, Informality, Kutupalong
Abstract
Bangladesh Rohingya camps have hosted 65,000 refugees fled from Myanmar only since 2017. Their compromised living environment and limited physical and socioeconomic facilities make them highly sensitive to COVID-19. The Government of Bangladesh and international aid agencies have applied WHO's IPC (Infection, Prevention, and Control) guidelines to mitigate the transmission of COVID-19 outbreaks and enhance their resilience. However, Rohingyas often disregard these guidelines or become reluctant to follow them. Building on 10 in-depth interviews, 66 questionnaires, and observation, the study investigates the limitations and challenges of implementing these guidelines toward building community resilience. It assesses their resilience, focusingon Kutupalong camp, Cox's Bazar−one of the world's largest refugee camps. Findings reveal that Rohingya's past experience associated with their psychological trauma largely influences their current actions and demotivates them fromfollowing the health guidelines. Their deep mistrust of and disrespect to healthcare providers and aid agencies discourage them to follow the IPC. Also, insufficient built infrastructure and unhygienic living conditions, including improper WASH management, increase their risk to COVID-19. The study highlights a need for understanding their socio-psychological values and cultural narratives and recommends a set of guidelines for policymakers and aid agencies to build community resilience to COVID -19.
Introduction
COVID-19 pandemic is a stripping natural threat to humankind. Compared to similar past pandemics, which had controlled nature and limited geographical reach, COVID-19 has triggered extraordinarily unwarranted situations (Nahiduzzaman and Lai, 2020). Marginalized and displaced (refugees) populations (Ullah et al., 2021), in low-to-middle income countries (LMICs), are particularly vulnerable to COVID-19 (Wilkinson, 2020). LMICs host about 85% of global 79.5 million forcibly displaced people (UNHCR, 2019a). In general, the refugees in LMICs are experiencing a precarious living atmosphere and suffer from poor health infrastructure and services, including poor nutrition, and limited water, sanitation, and hygiene (WASH) facilities. Historically,the substandard livings historically make them vulnerable to disease outbreaks transmitted by the surface–person-air borne route (Wilkinson, 2020). Records show that between 2009 and 2017, 364 disease outbreak events occurred in 108 refugee camps (Altare et al., 2019). 134 host countries report that these camps are highly vulnerable only due to local transmission of SARS CoV-2 (UNCHR, 2020). However, unlike people in host communities, they are hardly prioritized for social and health privileges and urgencies, including vaccination and economic protection strategies (Gunst et al., 2019). This exclusion also makes difficult for early detecting, testing, diagnosing, and applying the preventive measures of COVID-19. Although the World Health Organization (WHO) recommends the “whole-of-government and whole-of-society approach” for everyone, in reality, the scenarios are different in refugee camps (San Lau et al., 2020). Consequently, refugees around the world are slurred and living with uncertainty.
Bangladesh has ranked as the second in South Asia in COVID-19 transmission as of late January 2021. Currently, the country has hosted more than one million forcibly displaced Rohingya refugees (FDMN); amongst them, 65,000 fled from Myanmar since 2017, resulting from the brutal persecution, rapes, and killingsby the Myanmar Military (Ullah et al., 2020). Until the end of December 2020, 366 confirmed cases and 10 casualties were reported (ISCG, 2020), although the record hardly represents the actual scenario. In addition, their pre-existing comorbidities and lack of knowledge, along with the congested living environments, inadequate WASH facilities, and insecure livelihoods have amplified their vulnerability to COVID-19 (Shammi et al., 2020; Ullah et al., 2020). In response to this crisis, the Government of Bangladesh (GoB), healthcare partners, and different aid agencies have implemented many strategies, which are predominantly guided by WHO's IPC1 (Infection, Prevention, and Controlling), to control the outbreak and enhance their resilience.
This study investigates to what extent Rohingya refugees are susceptible to COVID-19 socially, economically, and politically and how they could build resilience. To date, little literature investigates COVID-19 resilience in Rohingya camps and provides normative guidelines. For instance, Homaira et al. (2020) explore the normative challenges and mitigations strategies, focusing particularly on health and political commitments. Kamal et al. (2020) and Banik et al. (2020) illustrate the transitional strategies of IPC measures. However, the challenges of integrating Rohingya's socioeconomic dynamics, spatial dimensions, and indigenous ways of coping have yet to be revealed (Shammi et al., 2020). The study thus aims to a) identify Rohingya refugees’ vulnerabilities to COVID-19, b) examine community reactions or adaptation against building community resilience, and c) outline the challenges of planning management strategies for Rohingya refugees to build resilience against COVID −19.
The following section reviews the concept of resilience in association with COVID-19 in humanitarian settings. Then, this study proposes a conceptual framework for resilient planning under COVID-19, followed by the methodology. Next, it discusses the findings according to the objectives of this study. Finally, planning and management strategies for pandemics, in general are highlighted in the conclusions.
Pandemic, resilience and refugees
Vulnerability and resilience: Theoretical understanding
Vulnerability refers to the “insecurity and sensitivity in the well-being of individuals to withstand stresses and shocks in the cadence of daily living” (Moser, 1998, p.3). Vulnerability represents the degree to which a system (e.g., a household, community, or organization) is prone to and cannot adapt to the adverse effects of hazards (IPCC, 2014). Vulnerability is directly related to spatio-physical, economic, political, institutional, and governance dimensions, which ultimately act as a driver of the resilience capacity of a community against hazards or outbreaks (Guillard-Gonçalves and Zêzere, 2018; Hossain and Rahman, 2020).
Resilience, a socio-ecological concept, determines a “measure of the persistence of systems and their ability to absorb change and disturbance” (Holling, 1973, p. 14)). It refers to a system's ability to cope with the impacts of disturbance and shocks, highlighting its ability to self-organize, renew, and develop (Cutter et al., 2008; Dhar and Khirfan, 2017). Resilience also includes aspects like buffering impacts, bouncing back to pre-shock situations, shock-absorbing, evolving or transforming common themes that qualify resilience (Bene et al., 2012; Norris et al., 2008). It focuses on two aspects: the first, resilience is a process, not a product (Brown and Kulig, 1996; Pfefferbaum et al., 2008), and the second, resilience is adaptability, not stability (Handmer and Dovers, 1996; Waller, 2001). The COVID-19, albeit a result of a biological disaster, needs community awareness and resilience to control its outbreak. Community resilience highlights a community's ability to absorb disturbances.
Community resilience during pandemics
A community is not resilient if its resources are scarce or has limited capacity to recover or experience prolonged dysfunction with sustained negative socioeconomic impacts. Thus, resilience itself can be used as a measure of a community's physical/infrastructural (Cutter et al., 2008), socio-political (Kulig et al., 2013), economic (Leach, 2013), and psychological (Berkes and Ross, 2013) resources. Norris et al. (2008)’s set of networked capacities, and Cutter et al. (2008)’s Disaster Resilience of Place emphasize the importance of socioeconomic, institutional/organizational, infrastructural, and community competence2 as measurable indicators of community resilience, all of which are still pertinent to explain community resilience to COVID.
Spatio-physical infrastructures/resources include housing and water-sanitation-drainage infrastructure thatdirectly impact community resilience (Cutter et al., 2008). The lack of natural lighting, ventilation, and unhygienic conditions also influence COVID-19 transmission (Ghosh et al., 2020). This lacks increase COVID-19 vulnerability too and challenge the inherent3 and adaptive4 qualities of resilience in the context of dense and compromised living, like in a refugee camp. For example, the rapid increase of COVID-19 cases among Syrian Refugees housing in Lebanon is the consequence (Al Munajed et al., 2020). During the 2009 H1N1 outbreak in Taiwan (Kao et al., 2012) and 1918 influenza in the US (Garrett, 2007), a positive correlation between higher density and outbreak/death was also observed.
Alongside living places and inadequate WASH (water, sanitation, and hygiene), facilities and practices play a crucial role in virus transmission as well as decrease community resilience (Hung, 2003). Contaminated water and poor SWM (solid waste management) also pose higher transmission risk (Mathavarajah et al., 2021). Moreover, shared WASH facilities and prevailing sanitation habits contradict WHO's IPC guidelines (Wilkinson, 2020). This is also against SDGs 6 and 11, both of which prioritize the universal access to water and sanitation by 2030. In the case of COVID 19, such limited infrastructure makes refugees difficult to follow: “Wash your hands, self-isolate, social distancing.5” In addition, the lack of hospitals or health care facilities hinders a community's capacity to prepare for, respond to, and recover from similar disasters.
Economic resilience highlights the community's economic vitality, diversity, and equality. Savings, income security, and investments/ businesses increase the capacity of individuals/communities to absorb disaster impact and improve economic resilience (Norris et al., 2008). During the lockdowns, refugee communities deprived from their daily wage due to restricted movements and insufficient savings and were forced to depend on aids (San Lau et al., 2020). Many have lost up to 50% of their average wage (Teachout and Zipfel, 2020). In Lebanon, for example, 60% of refugees have been permanently laid off due to COVID-19 (Kebede et al., 2020). Economic uncertainty affects food consumption and healthy diets and thus reduces their immunity to fight against COVID-19.
Social resilience underscores people–and–place connection and social embeddedness within and outside of a community and increases their adaptive capacity (Aldrich and Meyer, 2015; Cutter et al., 2008). Longstaff et al. (2010) highlighted the importance of ‘super-connected’ networks to increase social resilience. Berkes and Ross (2013)’s integrated approaches of community resilience underscores values and beliefs, social networks, engaged governance (collaborative institutions), and readiness to accept changes and boost the recovery process of community resilience. Further, the lack of social relationship during disasters also decreases the social values and beliefs and increase internal violence, rumors, fear stigma, and psychological trauma especially among the poor. Evidence suggests that such crisis can often be translated into gender violence as happened during the Ebola outbreak in Liberia and Sierra Leone (Minor, 2017) and during COVID-19 (de Paz et al., 2020) as well.
Information and communication become vital in emergencies. A trusted source of information is the critical asset to build individual and community resilience (Longstaff et al., 2010). Norris et al. (2008) stated that reliable information and communication (e.g., Media, digital information, and connectivity) reduce health-related vulnerabilities during disasters. Trusted and transparent communication also gives people competence, invests in public outreach, and reflects the values and priorities of people (Pelling, 2010). For example, during SARS and Ebola, many died only due to the lack of communication, trust, and cooperation between volunteers and healthcare workers (San Lau et al., 2020). During the COVID-19 crisis, refugees also encounter administrative, financial, legal, and language barriers to access the trusted health information to protect themselves (Shadmi et al., 2020).
Community competence/ human resources are often considered as one of the significant components of community resilience. Education and health quality/ability of a community increase community competence, where peoples’ knowledge and problem-solving skills serve as safety netsand determine their resilience (Aldrich and Meyer, 2015). For COVID-19, Knowledge, attitudes, and practice (KAP) are essential in dealing with fear, stigma, and the misinformation of virus transmission globally, including in Malaysia (Azlan et al., 2020), India (Pal et al., 2020), and Nigeria (Owhonda et al., 2020).
Physio-psychological wellness of communities directly impacts community resilience to disasters. It can build on the satisfaction of life (Cowen, 1994). Unfortunately, the level of satisfaction of refugees is substantially low due to their inadequate facilities of living and livelihoods. Persistent comorbidities, like CD (communicable disease) and NCD (non communicable diseases), largely influence Physio- psychological health illness of refugees. For instance, Abbara et al. (2020) noticed that the number of Syrians with chronic NCDs (e.g., diabetes, heart disease, cancer, and depression) are affected by COVID-19. Rubinson et al. (2013) argued that during the 2009 H1N1 influenza and the 2014–2016 Ebola epidemic, people who had NCDs were died more than those who did not have them.
In addition, Organizational resilience/emergency risk governance also affects community resilience. Institutional responses to promote leadership, preparedness of local authorities, emergency services, training, and public awareness enhance resilience to COVID −19 pandemic (Cutter et al., 2008; Wilkinson et al., 2020).
Conceptual framework
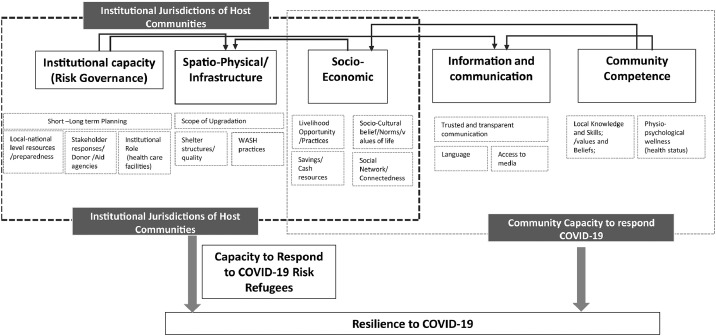
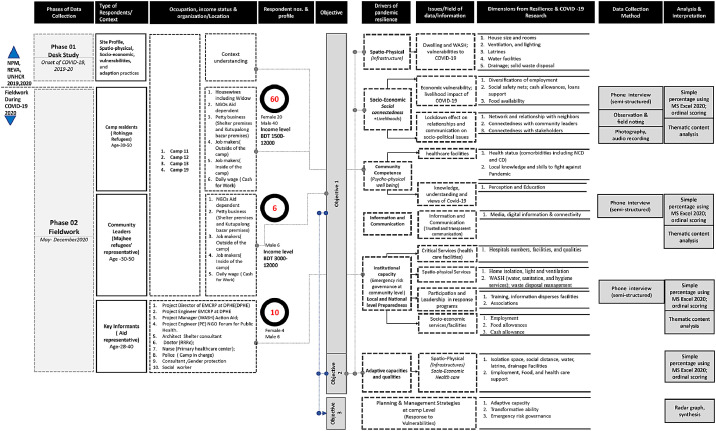
The discussion summarizes several attributes that influence communitys' resilience. Among them, spatio-physical, socioeconomic, and psycho-physical wellbeing affect the residents’ vulnerabilities and adaptability the most during COVID-19. Community resilience requires participatory and inclusive approaches (Masterson et al., 2016). Hence, a pandemic-resilient planning framework for refugees’ communities should start with investigating their vulnerabilities and adaptation practices that may vary by spaces and scales. For this, the proposed conceptual framework (Fig. 1), which is time, context, and hazard (COVID-19) specific, and multi-scalar (cutting across community, city, and national levels), and multi-dimensional.
Fig. 1.
The proposed conceptual framework for community resilience to COVID-19. (Source: Authors, 2020).
The framework builds on five interrelated dimensions of refugee living: spatio-physical, socioeconomic resources/infrastructure community competence/human resources, information and communication, and institutional capacity (risk governance) influenced by both intuitional polices and community responses. These dimensions also represent a complex and intertwined relationship between the host and refugee communities; however, are mostly governed by the local institutions (Fig. 1).
Case study: The Rohingya refugee camps in Bangladesh
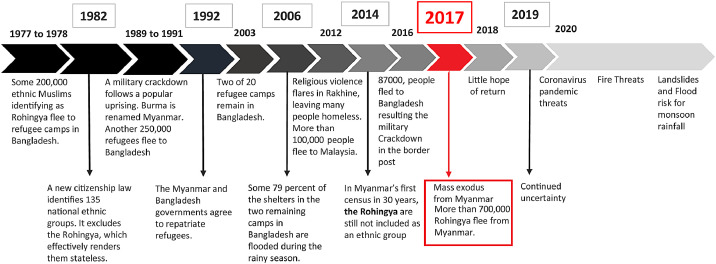
The Rohingya—a group of Muslim ethnic minority of Myanmar, have been housed in the Cox's Bazar, a small tourist city of Bangladesh, since 1977. Due to anti-Muslim violence that occurred in Myanmar in 1930 and 1938 and several times between 1990 and 2001 (Fig. 2), Rohingya civilians fled from Myanmar to Bangladesh (Ullah, 2016). Rohingyas were forced to leave for Bangladesh in four main periods (Fig. 2): (a)the late 1700s and early 1800s; (b)1977–1978, and the recent times; (c) in 1991 and 1992 (about 250,000), 2012; (d) and the most recent one was in 2017. Continuation of the socio-political violence, in August 2017, approximately 700,000 Rohingya refugees have fled from their host country to Bangladesh (Ahmed et al., 2021). Currently, 860,494 Rohingya live in 34 camps (2 registered and 32 un-registered) in Teknaf and Ukhia Upazila6 in Cox's Bazar. The majority of these camps are supported by the collaborative assistance of GoB( Goverment of Bangladesh) and other organizations, specifically the UN High Commission on Refugees (UNHCR) and the International Organization for Migration (IOM).
Fig. 2.
The history of Rohingya refugee in Bangladesh.
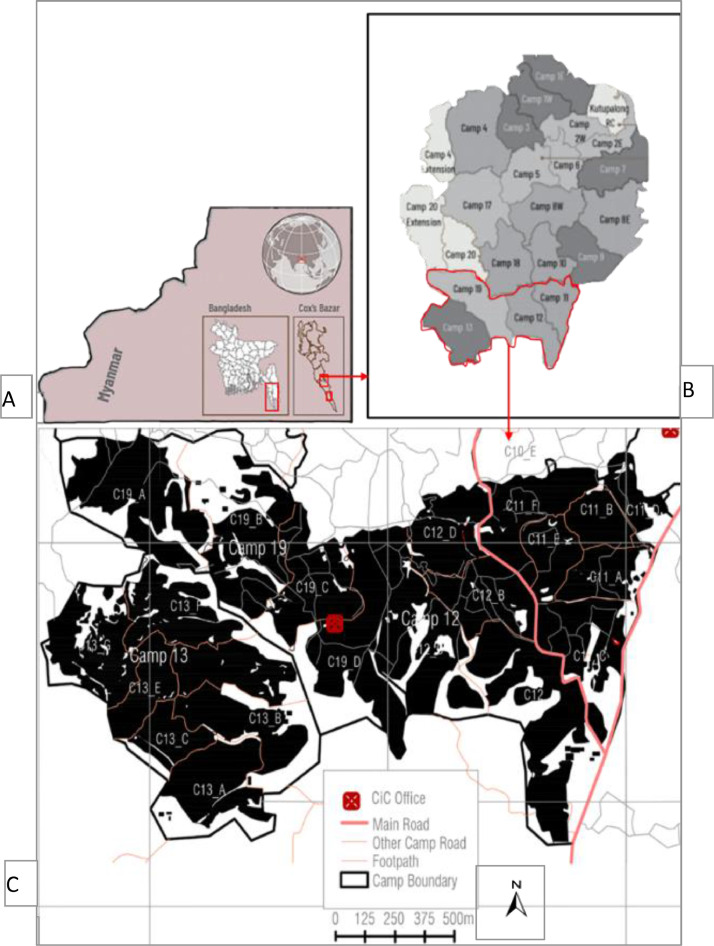
In 2017 GoB extended the Kutupalong area over surrounding 13 Sq.km areas, called “Kutupalong-Balukhali Expansion Site” (KBES). The KBES represents the world's largest “mega-camp” (Fig. 3b), includes 23 camps, and accommodates more than 600,000 refugees. The average household size is 4.6 in small makeshift shelters (of 11m2, one room) built with bamboo and tarpaulin (Khan et al., 2020). Sleeping on plastic clothes or papers on the muddy floor makes them vulnerable during rainy seasons. In addition, 10% of household is estimated have at least chronic disease or disability. Moreover, 17% of people living below the extreme poverty line, compared to the national average of 12.9%, can only 30% can read and write the Burmese language, 73% of households have a cell phone, and only 4% have a television (REVA, 2019).
Fig. 3.
(A) The location of Myanmar and Cox's Bazar, (B) KEBs “Mega-Camp”, the areas red-marked indicate the four camps:11,12,13, and 19, and (C) The figure ground map of four camps. (Source: Authors created based on various sources).
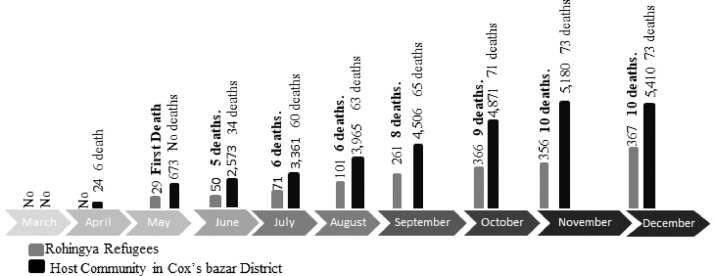
Since early 2020, although the COVID-19 outbreak has increased substantially across Bangladesh, Rohingya refugees have witnessed relatively low transmission (Fig. 4). But Truelove et al. (2020)’s model predicts a rapid outbreak even with low rates of transmission in Rohingya refugee camps. Such predictions hint at the long-term impact on Rohingya lives and livelihoods that would be amplified by their current insufficient and unhealthy living atmospheres. In addition, the lack of COVID-19 testing capacity, slow vaccination progress, and ineffective institutional responses have made the Rohingyas incredibly vulnerable to the virus attack (Ullah et al., 2020; UNCHR, 2020).
Fig. 4.
COVID-19 confirmation and death ratio of Rohingya refugees compared with the host community. Source: Author's created based on (ISCG, 2020; WHO, 2020a).
Among the 23 camps in KBES, this study considers camps 11, 12, 13, and 19 Table 1. We adopted three criteria of selecting these camps. First, we consider the camps to which aid workers/researchers have access since most camps are declared as Red Zones. We access these camps with the assistance ofthe Refugee Relief & Repatriation Commission (RRRC) and Action Aid Bangladesh (AAB). Second, the camps that have more COVID-19 cases, and third, the camps that represent a complex relationship of socioeconomic and spatial aspects (e.g., the highest household desity). These 4 camps, which satisfy this three criteria, represent the highest household density with a lack of saniation and water facilities. Demographically, children are counted as 51% of the total population, and 24% female 19% adult male, 1.5–2.5% widow and female-headed families, and 3–4% disable are estimated in the selected camps. Table 1 shows the camp profile.
Table 1.
explains the rationale the profile of these camps. Among these, the highest population was found in camp 13 and lowest in camp19.s.
| Camp | Blocks (including ub Blocks) | Total camp Area (Sq.m) | Average usable area per person (Sq.m.) | Total Households | Total Individuals |
Age and Gender Distribution |
Average monthly income | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Children | Female | Male | ||||||||||
| (0–17 years) | (18–59 Years) | (18–59 years) | BDT | |||||||||
| Camp 11 | 79 | 466,019 | 13 | 6146 | 29,671 | 15,270 | 7210 | 6088 | 3500–5000 | |||
| Camp 12 | 56 | 631,138 | 19 | 5303 | 25,659 | 13,321 | 6269 | 5056 | ||||
| Camp 13 | 94 | 753,767 | 16 | 8803 | 41,586 | 21,630 | 10,114 | 8244 | ||||
| Camp 19 | 66 | 766,669 | 25 | 4868 | 23,041 | 11,960 | 5715 | 4545 | ||||
Source: Author's created based on (ISCG, 2020; WHO, 2020a).
Research methodology
This research conducts a qualitative approach that combines empirical evidences and theoretical claims to produce arguments, as Schwandt (Schwandt, 2014) suggested. The key reason for adopting this approach was to comprehend Refugees’ lived experiences of coping with COVID-19. Data were collected in two phases. In the first phase, pre-COVID-19 data of Rohingya refugees were collected from secondary sources, including NPM7 (Needs and Population Monitoring), 2019, REVA (2019), and UNHCR (2020). This helped lay out the context and identify Rohingya refugees’ site profiles, pre-COVID-19 vulnerabilities, and adaptation practices. In the second phase, empirical data were obtained through interviews, questionnaires, and direct observation.
Interviews and questionnaires
We conducted our survey during May-December 2020–whether in-person with keeping 2 m physical distance or remotely–considering COVID restrictions and depending on the respondents’ preference and access to technology. For interviews, based on researchers’ professional networks along with purposive and snowballing approaches, ten NGO/local government officials, as key informants, who have been responsible to maintain/operate the health, shelter, education, WASH, roads, and drainage sectors in these camps, were initially selected. Fig. 5 illustrates five themes that guided the structure of each interview. Then, we used 66 questionnaires randomly with refugees: 60 with camp dwellers (i.e., the refugee victims) and 6 with local camp leaders (also called Majhee) (Fig. 5). At this stage, we invited two camp leaders (Rohingya volunteers) to assist us with their familiarity with Rohingyas' language and cultural background.
Fig. 5.
Analytical framework. (Source: Authors, 2020.).
Observation and mapping
We visited the campus while ensuring COVID-19 safety measures during August 2020. The ISCG (Inter Sector Coordination Group) guided us during observation, and we took notes and photographs (with respondents’ consent) to document the physical and socio-spatial environment of the camps. Also, to prepare the figure-ground maps, a few drone images that illustrate the physical condition of their built environments were collected from the NPM,17 (Needs and Population Monitoring) program of IOM Bangladesh.
Data analysis
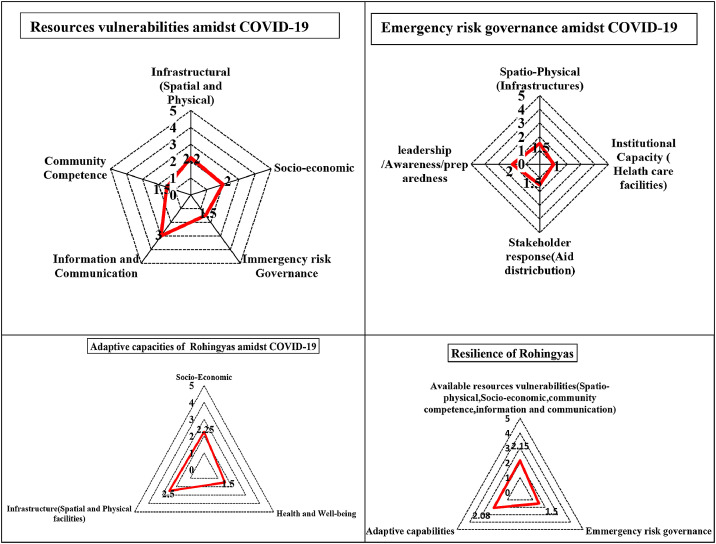
All information (from interviews, questionnaires, and observation notes) was transcribed into English for analysis. Thematic analysis of transcribed data is organized according to our objectives. The key intention was not to theorize but to highlight the phenomenon affecting communities’ resilience practices (and it's lack) during the pandemic. To interpret findings, an ordinal scale is used with scores for very poor (1), poor (2), fair (3), good (4), and very good (5), alongside simple “quasi-statistical” percentages without the intention to generalize (Maxwell, 2010). Scores from the ordinal scale were articulated in three summary matrices and three Radar Graphs in the discussion. This also helped to summarize the status of COVID-19 resilience of Rohingya refugees.
Rohingya refugees’ vulnerabilities during COVID‐19
Institutional capacity (Emergency risk governance)
Institutional capacity (Emergency risk governance) primarily includes healthcare planning and policy preparedness. The quality of the health care facilities and treatment strategies during COVID-19 are poor than required. For example, in the Kutupalong site, there are 0.31 physicians per 1000 people(Truelove et al., 2020), against the 4.5 minimum physicians/1000 as recommended by the WHO, and lower than the national average of 0.526 physicians/1000(WHO, 2020). Table 2 summarizes the gaps in meeting the health needs of the refugee communities.
Table 2.
Shows the evidence of Gaps and availability of preparedness.
| Availability of Healthcare facilities | Gaps in Preparedness | |
|---|---|---|
| At Rohingya Camp | 36 Primary health clinics (PHC) | (1 PHC/25,000 persons) are available in the camp settings, but the total number of functioning PHCs varies |
| 01 institutional quarantine center | 01 quarantine and testing center are inadequate for a one million Rohingya refugees. | |
| 01 testing facility available for Rohingya refugees in the camps | ||
| 14 SARI ITCs operational Severe Acute Respiratory Infection Isolation and Treatment Centers | 1292 (652 active and 579 standby beds) bed occupancy were ready at the end of the December,2020 was not sufficient for 01 million Rohingya refugees. No Intensive Care Unit (ICU) or ventilator capacity | |
| At Cox's Bazar District | 10 ICU beds in Cox's Bazar district | Without HEPA filter, Negative pressure facility merely can support critical patient of COVID-19 according to the WHO's IPC strategies. |
| 250 bed capacity are available in Cox's Bazar Sadar hospital in Cox's Bazar district | Typically treats between 400 and 600 inpatients daily; 50–60 of whom are estimated to be refugees available. | |
| Testing capacities | 1500 samples/day is inadequate | |
| 5 quarantine and 20 isolation facilities in Ukhiya and Teknaf Upazilas, with multi-sector support. | These facilities barely provide the sufficient facilities for all Rohingya refugees and host communities. |
(Source: Author prepared based on (IRC, 2020; Truelove et al., 2020; UNHCR, 2020) mainly
The estimation shows that the lack of the Severe Acute Respiratory Infection (SARI) treatment centers, isolation hub, and quarantine zones are acute in the camps. Further, limited beds, hygiene,waste management, less equipped ICUs (e.g., without negative pressure rooms), and ventilators are not capable to provide service to the critical ARI (Acute respiratory infected) patients. This lack forces patients to admit to Cox's Bazar district hospital, which is already overwhelmed by the patients of host communities.
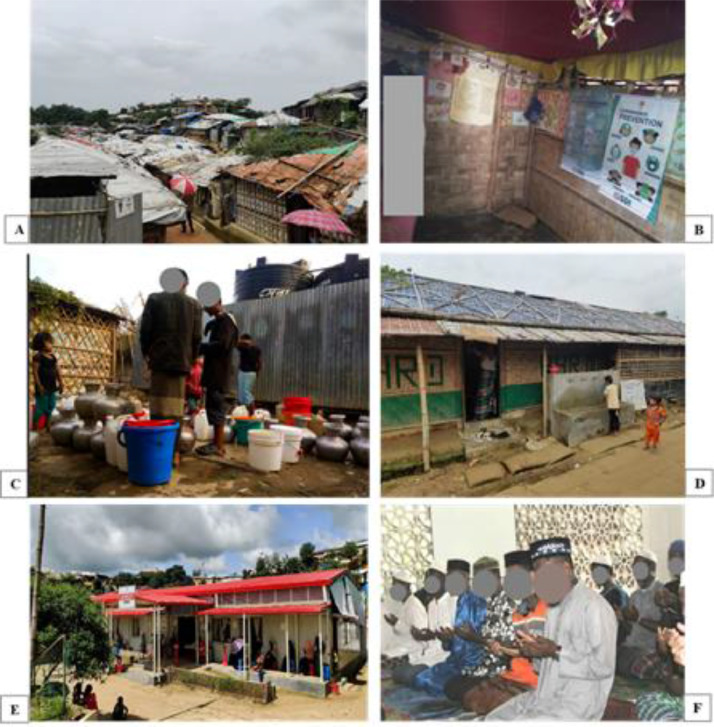
Moreover, PHCs (primary health care centers) in the camps are not well-functioning and limited in numbers to meet the demands of a large cohort of refugees.Long waiting times infornt of PHCs worsen the helath care vulnerabilities during COVID-19 (Fig. 6). Even they are limited to CD (Communicable disease) only, while non-communicable disease (NCD) management and specialized services (such as eye-care, oral healthcare, and services for people with disabilities and palliative needs, etc.). These lacks make Rohingyas vulnerable during COVID-19.
Fig. 6.
A) Crammed shelters; B) Lack of lighting and ventilation in shelter interior; B) Water scarcity resulted form limited water points; C) Roadside water sources; D) Long awaiting time in front of healthcare center; F) Communal prayer. (Source: Fieldwork, 2020).
Lack of trust and miscommunication with health caregivers induced Rohingyas drastic drop of taking treatment frequency than the pre-COVID-19 situation. For instance, the regular consultation serviced was dropped by 50% in 4 months (May-August 2020) due to fear and stigma of COVID-19. Our field work reveals that ARI (acute respiratory infections) has been decreased from 26.4% to 12.7% from week 12 to week 25, in 2020.The fear of being ‘killed’ and ‘isolated’ (if infected), lack of treatment diversities and extremely unprofessionalism by the healthcare workers (specifically staffs) and shortage of Rohingya medical staff also represented as main obstacle. A female Rohingya explained-
''These days, the healthcare workers behave rudely …. if we are infected (or suspected to be) by COVID-19. The guard man and other staff got violent. If we do not have fever, they even refuse to see us after keeping us waited for the whole day and give us only paracetamol [a medication used to treat fever] … We locally call it “paracetamol center”.
Stakeholder's response /Aid distribution/ infrastructure management
Rohingya refugees received various aid during the entire outbreak period (Table 9), but reduced aid (allocated for 931 BDT compared to the pre- COVID-19 1031 BDT (12.10 USD) during COVID-19 made them even vulnerable. Rohingya refugees even did not receive any cash allowances like the host communities received (e.g., a BDT 2500 cash support from the Prime Minister). Although a few elderlies (60 years old refugees) got 5000 BDT during pre-COVID-19 situations, none of the initiatives have even been continued during post- COVID-19 situation. Despite RRRC and NGO's efforts in distributing foods and NFI, no long-term planning was conceived–neither at camp, nor at shelter level–to adapt to the economic shocks as after losing income opportunities during COVID-19. To create alternative livelihoods and increase economic resilience to future pandemics, there was no skill development program.
During the pandemic, Rohingyas consider NGO services as very poor since all SWM and drain-cleaning services were ceased from them. Though WASH sector-partners and Government organizations, like RRRC and the Department of Public Health Engineering (DPHE), have provided facilities,8 including hand wash points and hygiene kits, all their supports are limited to ‘need-based’ and temporary, and no long-term planning was considered for future development. More than 100 different organizations are working to help the Rohingyas; however, all their facilities are discrete and short term biased, and failed to foresee the impact of COVID-19 vulnerabilities among Rohingyas.
The quality of the built environment was also insufficient to meet the COVID-19 needs. Neither RRRC nor NGOs helped Rohingyas reorganize/manage to improve indoor lightning and ventilation or improve community transmission-prevention infrastructure/facilities. 80% of refugee residents blamed the camp authorities and the site management for their negligence regarding shelter replacements,9 repairs, and infection prevention. In addition, 70% of refugees highlighted the lack of professionalism and extreme nepotism of community leaders ‘Mahjee’ regarding the allotment of better shelters, health, and employment services.
Leadership/Awareness/Preparedness
Respondents report that NGO-driven information/awareness sessions hardly encourage all to participate equally. It had gender-biased and lacked monitoring sessions, which make the refugee not to have proper understanding of WHO's IPC guidelines and their implementations. For instance, NGOs-hosted audio/video/poster sessions are entitled to only 4 to 5 Rohingya male participants in a single camp. Whether the representatives pass the information to the broad mass remains unchecked by the CwC (communication with the community) group. Male-female participation in various COVID-19 awareness programs represents about 10:1 that poses a severe risk for maintaining WHO's IPC at the household/community level. Due to unawareness of different strategies, such as women-friendly spaces and community feedback/complaint system, the female Rohingyas (representing 60%) remain reluctant to participate in the COVID-19 awareness programs.
Spatio‐Physical vulnerabilities
Inadequate shelter space
The unplanned camps, their ‘row house’ organization, and high ground coverage (over 80%) produce an extraordinarily cramped and unhealthy living environment (Fig. 6A). They have limited indoor lighting and ventilation( Fig. 6B). Typically, 10–11 officially allotted persons live in each of these tiny shelters occupying only an area, accounting for 1.6 sq m/person, which is not even close to recommended 4.5 sq m/person by the Humanitarian Charter (Sphere, 2018). Substandard shelters with conditions such as leaking walls and roofs, lack of weathering, or other hazards make them ever vulnerable. Narrow non-paved (Kacha) lanes/streets of 1 to 1.25 m wide with public gathering cater life-threatening residential overcrowding living, while exposing them airborne virus transmission. Rohingyas suffered from camp's low-elevation, chronic flooding/waterlogging, and maintaining non-permanent shelters. They were more concerned about monsoon flooding and seasonal calamities than Coronavirus.
The compact environment (indoor and outdoor spaces) hinders refugees to maintain COVID restrictions as recommended. A female respondent of camp, 11 argued:
“We cannot maintain social distancing in our shelter and outside as well. Our room becomes very hot during this hot summer due to the roofing materials, tarpaulin, insufficient solar fans, and natural ventilation. Therefore, we cannot stay a room for long, and can't stay outside also because of overcrowded people and the risk of Coronavirus.”
Insufficient Water, Sanitation, and Hygiene facilities
Shared water sources of the camp, including (52.08%) piped water (14.87%) and public taps/stand posts (6.69%), are also against the WHO's IPC. Most community leaders reported that only half of the households have access to water outlets (Fig. 6C). Also, because of inadequate water flow, refugees often wait 25 minutes more to collect water than of pre-COVID. Our fieldwork revealed that currently, 54% of the Rohingya refugees have access to chlorinated water supply through small and borehole-fed water networks, while 70% of household-water is contaminated. Inadequate water facilities and long waiting time pose the risk of surface-human transmission of SARS CoV-2. For instance, in camp 11, block E, one water collection point withfour taps serving 380 refugees is inadequate and contradicts the WHO's IPC again Fig. 6D. Typically, NGOs and local governments install community tube-wells/water taps in available empty spaces along/beside streets (Fig. 6D) without considering (travel) distance/time for all users. Regarding water deficiency, a female respondent in Camp 12 narrated:
''INGOs people tell us to drink plenty of water and wash our hands frequently for fighting against COVID 19, but we do not have enough water… we must go far away to collect the water while standing and waiting for over 15 min. As we have only one water collection point in each block, we cannot drink and use plenty of water after defecation and hand wash''.
Most (90%) Rohingyas use shared, and limited toilets/baths and tubewells – a situation that is common in camps but poses further challenges in the context of COVID-19. Our observation explained that camp 11 faces an acute shortage of toilet facilities. For instance, Block E of Camp 11 has only 1 latrine and 1 bathing cubicle for about 50 refugees.Besides lack 70% of toilets/baths and tubewells are nonfunctional. This shortage and non-functionality resulted in several people waiting and gathering in a narrow space and forced not to maintain the social distancing.
Our interviews reveal that 60–100 people queue at least twice a day at the points of shared WASH facilities and create transmission hotspots. During lockdowns, toilet usages increased significantly as Rohingyas queued about 20 min, doubled from pre-COVID-19 time. During peak hours (morning and noon), it grew to up to 25 min. Broken and unclean floors of shared latrines increase virus lifespan (2 h to 9 days), as suggested (WHO, 2020b). And, despite having community toilets, 70% of children use the makeshift toilets/tube-well-yards for defecating, which poses a significant risk of fecal-oral contamination. Further, many block leaders (Mahjee) reported that gender respective latrines are in crisis in the camps. During phone interviews, a female respondent argued-
"We cannot go to latrine easily during CORONA time, as all the males are roaming outside, we cannot maintain privacy and cannot do defecation on time. As a result, we feel physically unfit, we are now drinking less water; though volunteers told us to drink plenty of water; but we are not heeding their guidelines for reducing the frequency of latrines we needed. We must follow up when the latrine will become free".
Socio‐ Economic vulnerabilities
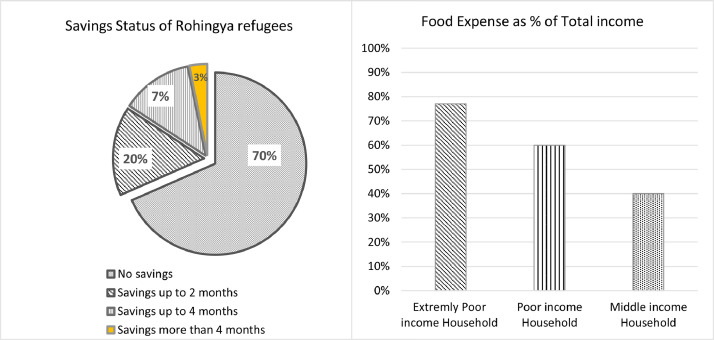
On average, 60% of Rohingya are unemployed (compared with 20% of host communities) and dependent on aids, and non-diversified income sources. Their income sources are limited to NGOs-provided-rations, daily wage earners, petty traders (smuggling also), and monthly salaried employment. Their average income ranges between BDT 3500–5000 (Table 3), almost 75% lower than the host communities. In contrast, 40% of Rohingya households that were evident highly vulnerable had the lowest average household income levels BDT 2736. Moreover, 80% of respondents claimed that they have no savings and spend 75% of their earnings for consuming food (Fig. 7), 10% for medical treatment, and the rest of the amount for availing NFI (communication/information, clothing, hygiene, and others). Home-based enterprises (HBE) like running small groceries, raising poultry, and sewing are almost absent in the camp settings.
Table 3.
Rohingya refugees’ occupation and income status.
| Types of Employment | Classifications of Occupations | Percentage of Respondents (%) | Monthly income (BDT) |
|---|---|---|---|
| Petty Traders(self-employed workers and services holders) | Selling rations (Pulse, salt, soap, rice, oil, sugar, eggs, dried fish) and NFI (light, fan, mattress) | 5 | 1000–1500 |
| Tailors, weavers | 4 | 3000–6000 | |
| Others (Importer from Myanmar, Bribe, Taking interest in credit) | |||
| Small shop/ business owner | 12 | 6000–8000 | |
| Hawker/ Vendor (outside of the camp) | |||
| Fishing at outside of the camp | 5 | 10,000–12,000 | |
| Driver (Auto Rickshaw/CNG) | 2 | 12,000–14,000 | |
| Wage Earners/ (Cash for work, 9 to 15 days per month) | Day labor (350 BDT per day) | 50 | 2770–5250 |
| Monthly Salaried Earned (26 days in a month) | Camp Volunteer | 10 | 2000–5000 |
| Human health and social worker | 10 | 3000–4000 | |
| Religious Teacher (Mowlana) | 2 | 5500–12,000 | |
| 100 (N = 66) |
(Source: Field Work, 2020).
Fig. 7.
Savings status and food expenses of Rohingya refugees. (Source: FieldWork, 2020).
Further, respondents specifically who had incomes before COVID-19become more financially stressed in COVID-19. 10 −12% of people in each block involve a program named “cash for work” for 50 takas/hour (0.6 US$/hour) run by humanitarian agencies. Though the programs are limited to specific categories (e.g., drain, road, shelter construction mainly), and limited working days (9–15days/week), these practices support the families in need; most of these are postponed due to the COVID-19 pandemic. Locals often claim that the program discriminates them by gender with a ratio of 70% male and 10% female. Inadequate and discriminated income limit their savings capacity and ‘safety nets’. Female Rohingyas thus remain economically more vulnerable. Their inconsistency and poor income cannot meet their monthly expenditures, which is around BDT 5000–7000 (USD58.95–82.53) per capita. A 30-year-old widow of Camp 13 shared her experience in COVID-19:
''I was able to earn only BDT 350 [USD 4.3] daily as a day labor under the “cash for works” program before the pandemic. Though it was very low, I could manage. But during post -COVID-19 situation, I have lost my work… I am now selling rations and taking loan from my neighbors to maintain my livelihoods''.
Their inconsistent and poor income opportunities make them food vulnerable (mostly disabled, elderly, and female-headed households). Nearly 70% of female-headedhouseholds suffered from food shortages compared to only 50% of male-headed ones. For instance, Camp 19 has 522 female-headed families who suffered a lot at the onset of the COVID-19 period. Only 2% had savings to obtain food beyond 4 months, while about 18% had limited savings to ensure food for 2–4months (Fig. 7). They can only afford “rice and lentil” for their children, which is inadequate and far from a balanced diet recommended building a strong immune system to combat COVID 19. A mother of four in Camp 11 spoke-
“My children have been crying for meat for last few days, but I could not afford it due to soaring price. I purchased two eggs and divided it among them.”
Although humanitarian agencies provide basic food and groceries (Table 4), they hardly ensure daily protein and minerals intake as required. Thus, malnutrition and deficiencies of minerals10 (e.g., calcium) expose them to COVID-19 and sever-malnutrition again. In addition, food price hike (about double), unavailability of sufficient camp ration and inaccessibility to ‘Kutupalong’ bazar during the lockdown impacted them severely.
Table 4.
Summary of Aids to Rohingyas.
| Aid provided | Categories and quantities of Aids | Aid agencies |
|---|---|---|
| Food Items (FI) | Rice (13 kg /per person), lentil (2/ per person kg), salt, flour (2 kg), edible oil (1liter), Sugar (1 kg) mainly. | NGOs |
| Pulses (1 kg/per person and Potatoes 2 kg/per person Cabbage, fish (1 kg) | NGOs | |
| Non-food items (NFI) | 2/3 pieces of soap and 1/2 kg detergent powder (disinfectant liquid) etc. | NGOs |
| Water storage containers and basins | NGOs | |
| Tissue paper, Hygiene kit | NGOs | |
| Surgical Mask mainly | NGOs | |
| Financial support | Cash | No cash allowances |
Source: (Filed Work,2020).
Information and communication vulnerabilities
Radio and NGO workers were identified as the most reliable media for receiving COVID-19 information and scored as ‘fair’ in terms of trusted information and sources. 40% of respondents reported that obtaining information from friends, family, or neighbors is more valuable than that from internet. Misperception and misinterpretation often create rumors and spread quickly across the settlements. This study identified three vulnerable sources of information during COVID: 1) lack of internet connectivity, 2) reduced office time and accessibility, and 3) information disperse strategies.
Besides, the difference in language, socio-cultural norms, and religious beliefs between the refugees and the host communities (i.e., the NGO people) further impeded communication effectiveness. A female respondent from Camp 11 clearly explained one such barrier,
''The language barrier remains one of the challenges. I do not understand what the ICU nurses and doctors say because they speak Bengali and Chittagonian [Cox's Bazar's local dialect]. I get scared to ask them again. The Bangladeshi translator also misunderstands us and fails to convey our experiences to the doctor accurately. [During the last meeting,]I couldn't understand any word that the doctor said , and the doctor went away without giving me an appropriate description''.
Community competence (Psycho‐physical wellbeing)
Two measures of community competence are essential. The first is related to their health quality in terms of psycho-physical wellbeing. About 60% of Rohingya refugees have pre-existing comorbidities. Acute Respiratory Infections (ARIs) (70%), Diarrheal Diseases (60%) and Unexplained Fever/ Malaria, and skin diseases are the three most communicable diseases (CD) among all refugees (Table 5). 70% of Rohingyas, women, and children, are suffering from anemia and malnutrition. 80% of Rohingya women are susceptible to posttraumatic stress disorder (PTSD) resulted from prolonged displacement, family segregation, and primarily political humiliation in their previous lives. This experience discourages the Rohingyas’ to even the COVID-19 screening test. A doctor from the humanitarian agency stated as follows,
Most female Rohingyas have mental trauma resulted from their present and past life. Since they arrived in 2017, they have had notrust in us. They dont even want to get vaccinated. They think that we are experimenting with medicines on them and keeping them on trial - a similar situation that they used to face in Myanmar.
Table 5.
Health condition and disease classification of Rohingya refugees.
| Disease classification | Common health conditions | Percentage (%) | Reasons |
|---|---|---|---|
| Non- communicable diseases (NCD) | Hypertension/High blood pressure | 60 | Trauma earned from Rakhine state experiences |
| Diabetes | 40 | Lack of Health care knowledges and Hypertension earned from Myanmar violence's. | |
| Unexplained pain /Arthritis/Bone weakness | 80 | Trauma earned from Rakhine state experiences | |
| Stroke/Heart-related issues | 30 | Lack of healthy life both in Mayanmar and Bangladesh | |
| Gastric problem/Ulcer | 60 | ||
| Drug addictions | 30 | Trauma earned from Rakhine state experiences and uncertainty life in Bangladesh | |
| Communicable diseases (CD) | Acute Respiratory illness /Cough/Tuberculosis | 70 | Lack of healthy life both in Mayan mar and Bangladesh |
| Fever/Malaria | 60 | Malnutrition and lack of healthy life | |
| Food poison/Diarrhea | 60 | Malnutrition and lack of healthy life | |
| Cholera/Waterborne disease | 40 | Lack of healthy life | |
| Measles/Skin infections | 50 | ||
| Hepatitis | 30 |
(Source: Fieldwork, 2020).
Though the actual morbidity and mortality rate of COVID-19 among Rohingya refugees is still low (2.39% till October 2020) comparing with the 14.41% in Cox's Bazar district, 45% of them had the three common COVID-19 symptoms (i.e., fever, cough, and unexplained pain), compared with the 30% of the host communities.
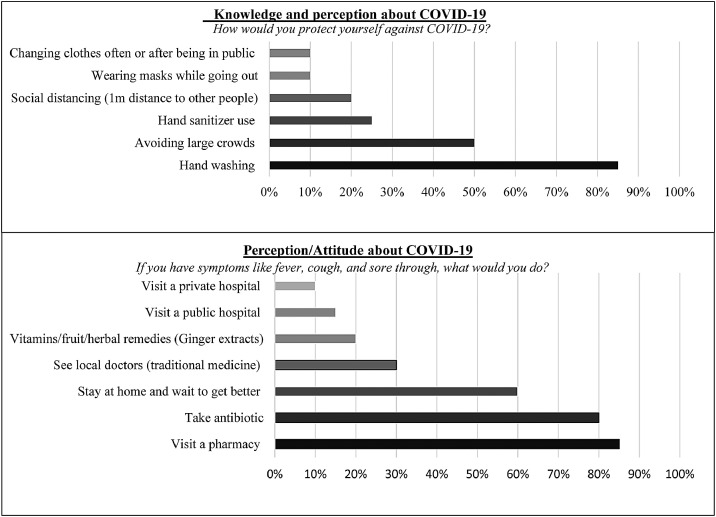
The second measure is about the knowledge, attitudes, and perceptions (KAP) that are influenced by the Rohingyas’ experience/ memory, lack of baseline education, and religious belief and cultural norms, are against the COVID-19 responses( Fig. 8). Pre-COVID-19 vulnerabilities make refugee's life even more challenging and reduce adaptive capacities during the COVID-19 situation. Lack of basic education has also hindered the learning of WHO's IPC guidelines. For example, 90% Rohingyas have misconceptions about the meaning of “Quarantine” and “isolation”. Further, none is fully aware of the actual symptoms of COVID-19, and it transmits. An old resident shared his belief:
"Coronavirus? I do not know about it, and I think we do not have that here. But I have heard that some people in the foreign countries are infected, who are non-Muslim. It is a punishment by Allah. We believe that everything is happened by Allah's instructions. If Allah wants, we will die or be alive".
Fig. 8.
KAP studies of Rohingyas. (Source: Fieldwork,2020).
Religious beliefs and cultural values often influence the knowledge and awareness of COVID-19. 80% of respondents believe that “Allah would keep us safe”, as 70% considered COVID-19 a disease of the rich people (Boroloker rog). They also felt that communal prayer and religious hymns (dua) would safeguard them from the virus (Fig. 6F). 80% of them perceived it as a ‘choyache rog’ (contagious disease) that transmits through touch, cough, or sneezes. Although a few have adequate knowledge of COVID- 19, they did not follow any preventive/protective measures due to unaffordability, illiteracy, and lack of healthcare facilities. A community leader (Block Mahjee) reported –
''Yes, NGOs have instructed us to avoid praying (saying namaj) in mosques, but we did not follow them. We pray in mosques regularly. We try to keep 1.5 to 2 feet distance from others in mosque while praying, but sometimes we forget to maintain distance''.
Moreover, refugees perceived the COVID-19 as deadlier than the actual morbidity levels and rate of COVID-19. The majority consider that ‘they will be killed by NGOs if they tested as positive symptoms of COVID-19 (female and male respondents).” Further, lack of knowledge on COVID-19 and mistrust forces refugees to be reluctant to allow their female partners and girls to go to isolation centers during COVID-19. An older female respondent shared her belief as follows,
"The isolation centeris a “Jail” and Sira- zaga” (separate land/place) … “Being sent to die alone.” In the isolation center NGOs behave rudely, do not give food properly, and do not allow phone calls . They even do not give proper medicines for COVID-19".
Surprisingly, respondents acquired helpful knowledge of the benefits of handwashing (accounting 85% of respondents), staying home (60%), poor practices (i.e., face mask and hand protection - 10%) were found and maintaining a minimum 1 m inter-distance (20%) were considered in successful COVID-19 prevention (Fig. 8). Coughing and sneezing were recognized as significant reasons, while surface-person communication was deemed least responsible for transmission. Interestingly, 85% of respondents still believe that taking medicine from the local pharmacy would cure virus infection. Yet, most Rohingyas are unwilling to visit NGO-led hospitals due to a lack of healthcare facilities and trust in healthcare providers.
Adaptive practices/ copying mechanism
Socioeconomic adaptation
To improve economic freedom, about 70% of refugees used three coping mechanisms during COVID-19: (1) selling rations; (2) borrowing from friends, relatives or loan sharks starting from April-May; and (3) relying on NGO's support. About 90% dealt with the worst food crisis during May-July 2020. About 60% of households reduced meal portion size, skipped meals, and relied on low nutrition meals. 60% sold FI (Food items), 25% sold NFI (Non-food items, e.g., soap, light, bucket, etc.), and 15% spending savings to meet food-related expenditure and had to rely on the scant aid supplied by NGOs. 80% of female- headed families and many families with a disability or lack of persons with income adopted debt habits to purchase food mainly. 88% of respondents claimed the ‘food’ was the most prioritized needs during COVID-19.
Phyco-physical wellbeing adaptation
Rohingya refugees adopted a negative coping11 mechanism during the COVID-19 situation to remain in good health and compensate the health care facilities. They include i) employing the isolation practices at home followed by prayer and ‘Dua’, ii) religious song and home remedies followed by taking medicine from nearby drug stores, iii) visiting quack doctors, and iv) cutting down other household necessities to buy medicine during COVID-19 outbreak. Whereas in the pre- COVID-19 situation, refugees were accustomed to visit doctors from non-governmental organizations (NGOs) and NGO health workers.
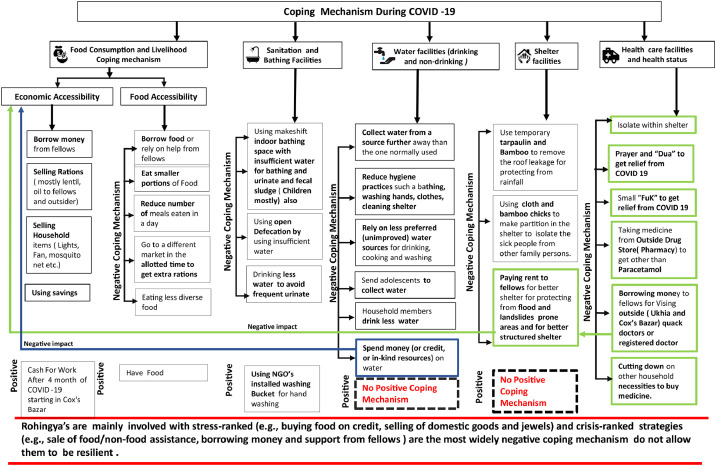
The most positive health outcome of COVID-19 is probably Rohingyas’ adaptation to hand-wash- a habit that has increased 85% compared to the 10% of pre- COVID-19 time. Due to the shortage of face masks, female Rohingyas use their scarves/shawls or niqab as an alternative, which approach was not certainly meet the WHO's IPC. Fig. 9 explains the adaptation practices by the Rohingya refugees.
Fig. 9.
Copying mechanism of Rohingya refugees during COVID-19. (Source: Fieldwork,2020).
Spatio-Physical (Infrastructures) adaptation
For isolation, 70% preferred home isolation. For example, all the 20 affected people (mostly male and aged between 40 and 60) (carrying COVID-19 symptoms) in camp19 got isolated and treated at home. But due to space constraints, 80% of Rohingyas had to share a single room (16.72sq.m.)12 using temporary partitions like untreated bamboo and cloths. Crammed camp settings merely have the community space for community isolation, as female Rohingyas feel reluctant to get admitted in the NGO-led isolation centers.
Despite continuous NGO supports to upgrade WASH infrastructure since 2017, all their supports have been limited to ‘need-based’ and sectorial WASH initiatives that did not have the capacity to tackle a crisis like COVID-19. In the scarcity of toilets, baths, and water supplies, only 20% of refugees could build makeshift attached toilets mostly used for urination and defecation – especially for females and adolescents. Still, 40% of female dwellers consume less water to avoid frequent trips to community toilets. Reducing food intake limit ordinary defecation habits, which pose threats at morbidity obviously amidst COVID-19. Our fieldwork reveals that copying approaches of Rohingyas were primarily negative in sense and in few positve whcih even have exacerbated the COVID-19. Fig. 9 highlights the negative and positive coping mechanism and their interconnection.
Resilience and challenges: Summary and discussion
Overall, Rohingya refugees demonstrate poor resilience to the pandemic (Fig. 10) When ranked, the study discovered the following three scores of their resilience. The first was the refugees’ lack of community competence due to socio-phycological ill-being relates to the economic uncertainty. The second includes poor living conditions, including improper WASH management, due to the limitation of global approaches or prescriptions to reduce COVID −19. The third and the last includes mistrust, disrespect/unsatisfaction toward health care facilities driven by the weak institutional capacity (risk governance). Comparing to the endogenous practices, many of the vulnerabilities and risks seem exogenous – mostly beyond the control of Rohingya refugees’ – especially those in the Government and Non-government sections. Although adaptation, as a process of adjustment to actual or expected adversities (IPCC, 2014), Rohingyas have proved fractional and delimited by both external and internal issues.
Fig. 10.
Rohingyas’ pandemic vulnerabilities, risk governance, and adaptive capacities. (Source: Fieldwork, 2020).
Despite continuous counseling of NGOs since 2017, the Rohingyas still remain susceptible to mental stigma, fear, and xenophobia and lost their community competence. ‘Very poor’ community competence ofdisplaced Rohingyas mainly originated from poor mental health / physiological disturbance is significant (Fig. 10). Predominant negative flashbacks and memories resulting from the massacre, anxiety, and acute stress Rohingya's past experiences from Myanmar broadly impact their mental health. Many consider this as ‘undefined pain’ that is even a hundred times more than COVID-19 stress or vulnerability. Even sexual and domestic violence increase in the camps during COVID-19. They are looking for humanitarian assistance for their survival strategies mainly because of food and other necessities but not building their resistance to COVID-19. Existing comorbidities, malnutrition, unwillingness to avail health care facilities were identified as other obstacles limiting the community competence. Poor mental health situations hinder the improvement of the individual or household resilience and maintenance of COVID-19-related precautionary practices (Cutter et al., 2008; Kulig et al., 2013). NGOs should consider that mental health first aid on the frontlines of the Rohingya crisis during COVID-19.
Very poor economic capital/resources (economic opportunity within and outside of the camp territories and food security) posed high economic vulnerability and food insecurity (buying capacity and inadequate ration) despite the current levels of humanitarian assistance (Fig. 10). This also catered the mental ill-being amidst COVID-19. The'Statelesstitle' becomes the main socioeconomic vulnerability here. Informal/non-permanent employment and lack of alternative livelihoods, savings/HBE, social safety nets, and credit facilities were identified as Rohingyas’ key economic vulnerabilities, which force them to adopt stress and criss ranked copying mechanism13 also stated in (REVA 2019) ’s study.
Very poor institutional capacity (risk governance) routed from lack of COVID-19 health care infrastructures and inadequate aid distribution mostly, which were even coupled with scant WASH facilities, poorly managed SWM and FSM, insufficient household space,and proper lighting/ventilation often cap Rohingya refugee's resilience power (Fig. 10) acknowledge the other study (Ghosh et al., 2020). The Mental Health and Psychosocial Support Working Group (MHPSS WG) (co-chaired by IOM and UNHCR) failed to help Rohingyas eliminate COVID-19 trauma at the onset (May-August) of the pandemic primarily. Despite their extensive support to the community health working group (CHWG) for implementing community health activities in the camps, limited numbers of CHWGs and unprofessional healthcare services create negligence and inequality that hinder the COVID-19 emergency services for the Rohingya refugees. These often contributed to higher ‘mistrust and disrespect’ and ‘miscommunication’ towards health care facilities, also illustrated in acaps (2020)'s study. The care providers do not consider refugee's past experiences and mental conditions. Instead they force refugees to adopt locally available healthcare treatments from local drug stores and home remedies. Neither adaptation strategy, nor any emergency risk management scheme was devised during the pandemic, even the world has limited knowledge on the potential risk plan, and their impacts on the refugees and displaced (Sen, 2020), inconsequence lack of adaptation, Rohingyas’ failed to adjust to actual or expected adversities (IPCC, 2014).
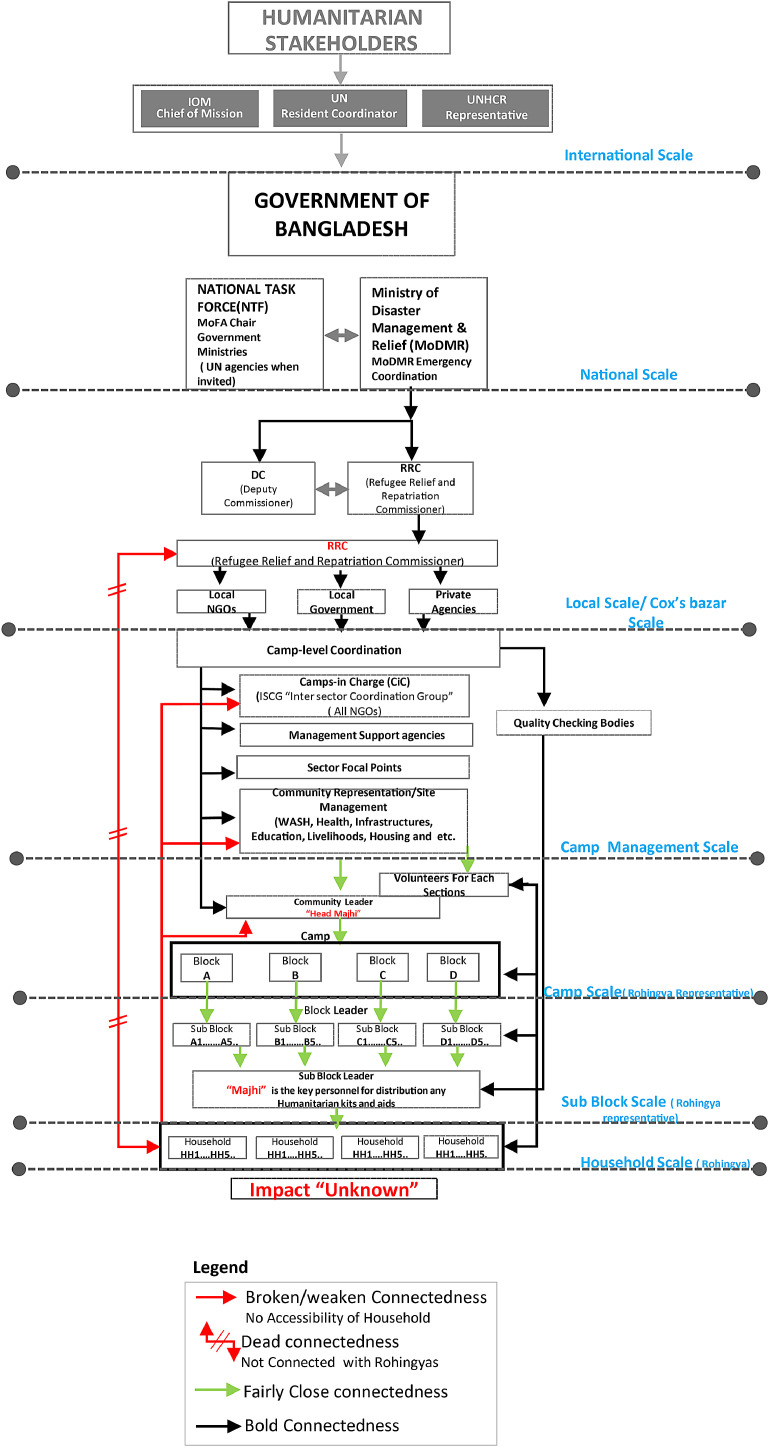
Despite continuous up-gradation, Rohingyas became susceptible to microbial transmission during COVID-19. ‘Poor’ and ‘very poor’ (shared) WASH facilities in all camps resulted from a lack of long-term planning methods integrated with risk governance. Short-term and sectoral-based provisions of WASH sectors out rightly halted Rohingyas’ mental well-being and reduce adaptive capacity. Highly top-down approaches have been evident in every sphere of policies and actions(Fig.11). Humanitarian agencies who work under RRRC maintain robust connectivity with Rohingyas' in aid distribution; coordinate with others. Yet, discrete or segmental aids (e.g., food, testing kits, sanitation, and water) disperse often poses inadequacy and non-justified amongst Rohingyas during COVID-19. Supply-demand mismatch and lack of preparedness administered by the NGOs and local governments during COVID-19. However, The Ministry of Disaster Management and Relief (MoDMR) and International humanitarian agencies (e.g., IOM, UNHCR, and UN) coordinated well to ensure inter-ministerial support and maintained robust connectivity at the national scale. However, at the local scale, the lack of community-led approaches and the absence of a local mediator to negotiate local victims and NGOs people are the main reasons that affect refugees' resilience. At the local scale, Rohingyas and camp representatives (e.g., camp in charge and site management) maintain a reciprocal relationship. Camp representatives (CRs) maintain robust connectivity with the Camp Majhees14 (CMs) to manage the camps with the widespread support of CMs but rarely reach the doorsteps of individuals/households. While Block Majhee (BM)15 – a leader who act as a mediator between CMs and individual Rohingya/household to disperse the information to each other. However, despite the involvement of BMs, Rohingyas' can rarely place their needs and urge to the CRs and CMs directly, and they maintain a weakened relationship. NGOs’ only kept providing every day and emergency supports through BMs, but rarely investigates the outcome of their aids or activities, which pose a 'feedback gap' from Rohingyas' side.This gap makes Rohingyas' even vulnerable during COVID-19 while nepotism/unprofessionalism from the site management/camp authorities and even from BMs often increases both economic and mental health vulnerability, even worsened the COVID-19 vulnerabilities again.Fig. 11 highlights this interelation and identify bold and weak connectedness among Rohingyas' and all stakeholders during COVID-19. To resolve this, disaster preparedness and response should be built more comprehensively by involving inter-sectoral coordination, information sharing, monitoring and evaluations, and adaptive learning (ISCG, 2020).
Fig. 11.
Interrelation among Rohingya and all stakeholders during COVID-19.
Although Rohingyas ranked ‘fair’ in their adaptive capabilities (Fig. 9, Fig. 10), more than 60% Rohingya households reported not having any means of coping with an emergency expense or pandemic, which even became proved negative in sense has also highlighted by REVA (2019), and such status cannot be able to generate any transformative strategies to be resilient (IPCC, 2014). Furthermore, ignoring mental health conditions by the financial hardship due to lack of legal refugee status or stateless challenged the refugees’ coping strategies and increased the instability stated by (ISCG, 2019; Ullah et al., 2020). Therefore, Governments, IOM, UNHCR, and aid agencies ought to work collaboratively and act to anticipate the spread of COVID-19 in refugees to fight against the outbreak and increase their resilience against hazards (Guillard-Gonçalves and Zêzere, 2018). The study determines all vulnerabilitiesfacilitating the impact of SARS CoV-2 with existing policies and human rights issues to enhance resilience.
Conclusions
The study reveals Rohingyas' indigenous attempts to escalate their resilience. COVID-19 awareness and aid agencies’ advice – forcing them to believe that they are vulnerable to COVID 19 – have hardly influenced these attempts to enhance their resilience. However, it becomes a fact when the number of affected cases along with casualties is not that significant and consistent. For example, our record shows that 10 death cases reported in the refugees’ camp compared to the host communities 73 death during the second web.
Aid agencies and professional services failed to consider and prioritize Rohingyas’ socio-psychological trauma from their past lives and thus failed to optimize the pandemic risk. As a result, their roles become ineffective, and they may lose the moral support and trust of Rohingyas. The problem is about linking two sides of a coin – one side represents WHO's IPC guidelines, a global and general framework that aims to fit all, and the other side belongs to the Rohingya refugees that have unique past experience entirely different from other refugees in the world. To minimize the gap, an intermediate or negotiable attribute is thus important to integrate community-based coping approaches and global health prescriptions. The study finds the potential role of ‘Majhee’ to become such an attribute. For the emergency management planning at the camp level, the role of Majhee can be more prioritized to make balance top-down and community-based approaches as a part of planning systems of refugees’ development, but needs popular selection or election process for avoiding Majhee favourtision and corruption. Further, enhancing mental well-being along with the better infrastructure that can also ensure a sense of safety and food security would be the most desirable for the refugee victims in the context of COVID −19 and similar outbreaks. Aid programs, despite criticisms, saved dwellers from starvation and proved to be a key coping element.
This study investigates the baseline capacity of Rohingya camps to identify the limitations and challenges of building community resilience. Rohingya refugees, like others across the world, are already vulnerable to their precarious living atmosphere, stateless identification, and uncertainty of livelihoods. However, for Rohingya, nothing can be as vulnerable as they had in their past lives. Thus, COVID-19 impacts and risks are hardly made refugees having a feeling of vulnerability. To develop theresilience capacity of refugee camps, the Government and humanitarian agencies should work on a long-term basis while appreciating the role of community leaders (Majhee and religious leaders) as a negotiated attribute to fight against COVID-19.
Authors’ contribution
All authors contributed differently to the content. Salma Akter conceptualized and drafted the manuscript, conducted interviews, and coordinated the overall project. Dr. Tapan K. Dhar conceptualized the research, took care of the methodology, provided critical comments, and edited the manuscript. Abid Ibna A. Rahman conducted the fieldwork and coordinated with studied Rohingya refugees. Md. Kamal Uddin conducted tele-data collection (phone –correspondence) procedures with the Rohingya refugees in their native language. All authors approved the final version of the manuscript.
Declaration of competing interests
The authors declare that they have no competing interests.
Acknowledgments
Funding
The authors received no financial support for the research, authorship and/or publication of this article.
Acknowledgements
We express our gratitude to the editor and reviewers for their suggestions and feedback. We especially thank Dr. Syed Muhaiminur Rahman, IRC (International Rescue Committee), Md Elias Khan, Police Inspector, and Rebeka Ahsan, Deputy Project Director of EMCRP (Emergency Multi-Sector Rohingya Crisis Response Project) at DPHE, Cox's Bazar, for the logistic support. Lastly, we extend our gratitude to the Rohingya refugees who participated in our study despite their urgency and language barriers.
Footnotes
IPC refers to infection, prevention, and control measures for COVID 19 describing general guidelines for maintaining social distancing, isolation, and quarantine (WHO 2020).
An intangible measure that determines how well a community's collective actions (through mutual trust and shared willingness) help it cope with post-disaster events by applying its pre-disaster knowledge and skills.
Well-functioning in non-crisis times
Flex-ability in response during disasters.
A motto of WHO to protect COVID outbreak.
Upazila refers to 'sub-district', formerly called Thana, representing a territorial administrative region next to ‘District’ in Bangladesh.
NPM is a part of the IOM's global Displacement Tracking Matrix (DTM) programming. The purpose of DTM programming is to develop the process for tracking and monitoring population displacement during crises.
As of August 2, WASH sectors installed 1,489 hand-washing stations, 203 stools with a bucket and taps at
household- level at public places, and 1,286 tippy taps (a cost-effective hands-free device for hand washing). (ISCG,2020).
Between 21to 27 August 2020, ta total of 515 Rohingya refugees affected by 82 slope failures 10,172 Rohingya refugees affected by 68 events of wind/storms/rain 61 Rohingya refugees affected by 4 floods (NPM, ISCG, Site Management Sector, 2020).
The crisis of food shortage force refugees to skip regular meal habits, and consumption of less balanced food are associated with topmost challenges faced by the refugee's communities in the pandemic situation, also these are linked with at least one symptom (fever and weakness) of COVID −19.
According to (REVA,2019) negative coping means the approach that temporally benefit them but for long run have negative impact on their health.
According to Rohingyas the room is comprised 8-10/10-12 hand, where 1 hand is estimated as 1.5 feet.
crisis-ranked strategies (e.g., sale of food/non-food assistance, borrowing money, ask for support from relatives and friends) are the most widely adopted ones (REVA,2019)
Every Camp has one/two camp leaders called Camp Majhee/ head majhee. 1camp is comprised of 4-5 Blocks.
Every Block has block majhee or leader who works under camp majhee's. Every block has 4-5 sub block. Each Sub-block has subblock majhee or leader who directly connected with individual Rohingya's.
Contributor Information
Salma Akter, Email: surma.arch@gmail.com.
Tapan Kumar Dhar, Email: dhar@ku.ac.bd.
Reference
- acaps. (2020). COVID-19 EXPLAINED, FOUR MONTHS OF COVID-19 PROGRAMMING RESTRICTIONS. Retrieved from https://www.acaps.org/country/bangladesh/special-reports#container-1484.
- Abbara, A., Rayes, D., Fahham, O., Alhiraki, O.A., Khalil, M., Alomar, A., et al. (2020). Coronavirus 2019 and health systems affected by protracted conflict: the case of Syria. 96, 192–195. [DOI] [PMC free article] [PubMed]
- Ahmed S., Simmons W.P., Chowdhury R., Huq S. The sustainability–peace nexus in crisis contexts: how the Rohingya escaped the ethnic violence in Myanmar, but are trapped into environmental challenges in Bangladesh. Sustain. Sci. 2021:1–13. doi: 10.1007/s11625-021-00955-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Munajed Al, D. Ekren, M. E.J.J.o., Health Exploring the impact of multidimensional refugee vulnerability on distancing as a protective measure against COVID-19. The case of Syrian refugees in Lebanon and Turkey. 2020;1 doi: 10.1016/j.jmh.2020.100023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aldrich D.P., Meyer M.A. Social capital and community resilience. Am. Behav. Sci. 2015;59(2):254–269. [Google Scholar]
- Altare C., Kahi V., Ngwa M., Goldsmith A., Hering H., Burton A. Infectious disease epidemics in refugee camps: a retrospective analysis of UNHCR data (2009-2017) J. Global Health Rep. 2019;3 [Google Scholar]
- Azlan A.A., Hamzah M.R., Sern T.J., Ayub S.H., Mohamad E. Public knowledge, attitudes and practices towards COVID-19: a cross-sectional study in Malaysia. PLoS ONE. 2020;15(5) doi: 10.1371/journal.pone.0233668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Banik R., Rahman M., Hossain M.M., Sikder M.T., Gozal D. COVID-19 pandemic and Rohingya refugees in Bangladesh: what are the major concerns? Glob. Public Health. 2020:1–4. doi: 10.1080/17441692.2020.1812103. [DOI] [PubMed] [Google Scholar]
- Bene, C., Wood, R.G., Newsham, A., & Davies, M.J. (2012). Resilience: new utopia or new tyranny?Reflection about the potentials and limits of the concept of resilience in relation to vulnerability reduction programmes (1353–6141). Retrieved from
- Berkes F., Ross H. Community resilience: toward an integrated approach. Soc. Nat. Resour. 2013;26(1):5–20. [Google Scholar]
- Brown D.D., Kulig J.C. Vol. 4. University of Lethbridge; 1996. pp. 29–52. (The Concepts of Resiliency: Theoretical Lessons from Community Research). [Google Scholar]
- Cowen E.L. The enhancement of psychological wellness: challenges and opportunities. Am. J. Commun. Psychol. 1994;22(2):149–179. doi: 10.1007/BF02506861. [DOI] [PubMed] [Google Scholar]
- Cutter S.L., Barnes L., Berry M., Burton C., Evans E., Tate E. A place-based model for understanding community resilience to natural disasters. Global Environ. Change. 2008;18(4):598–606. [Google Scholar]
- de Paz C., Muller M., Munoz Boudet A.M., Gaddis I. World Bank. 2020. Gender dimensions of the COVID-19 Pandemic. [Google Scholar]
- Dhar T.K., Khirfan L. Vol. 19. Urban Climate; 2017. pp. 72–91. (A Multi-Scale and Multi-Dimensional Framework for Enhancing the Resilience of Urban Form to Climate Change). [Google Scholar]
- Garrett, T.A.J.F.R.B.o.S.L. (2007). Economic effects of the 1918 influenza pandemic. 26.
- Ghosh S., Seth P., Tiwary H. How does Covid-19 aggravate the multidimensional vulnerability of slums in India? A Commentary. Soc. Sci. Human. Open. 2020;2(1) [Google Scholar]
- Guillard-Gonçalves C., Zêzere J.L. Combining social vulnerability and physical vulnerability to analyse landslide risk at the municipal scale. Geosciences (Basel) 2018;8(8):294. [Google Scholar]
- Gunst M., Jarman K., Yarwood V., Rokadiya S., Capsaskis L., Orcutt M. Healthcare access for refugees in Greece: challenges and opportunities. Health Policy (New York) 2019;123(9):818–824. doi: 10.1016/j.healthpol.2019.06.003. [DOI] [PubMed] [Google Scholar]
- Handmer J.W., Dovers S.R. A typology of resilience: rethinking institutions for sustainable development. Ind. Environ. Crisis Q. 1996;9(4):482–511. [Google Scholar]
- Holling C.S. Resilience and stability of ecological systems. Annual Rev. Ecol. Syst. Sust. 1973;4(1):1–23. [Google Scholar]
- Homaira N., Islam M., Haider N. COVID-19 in the Rohingya refugee camps of Bangladesh: challenges and mitigation strategies. Global Biosecur. 2020;(4):1. [Google Scholar]
- Hossain M.Z., Rahman M.M. Climate change vulnerability and resilience of urban poor in Khulna, Bangladesh: the role of asset-based community development approach. Int. J. Urban Sustain. Dev. 2020:1–17. [Google Scholar]
- Hung L.S. The SARS epidemic in Hong Kong: what lessons have we learned? J. R. Soc. Med. 2003;96(8):374–378. doi: 10.1258/jrsm.96.8.374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- IPCC . Geneva:Intergovernmental Panel on Climate Change. 2014. Climate change 2014: synthesis report. [Google Scholar]
- IRC. (2020). International Rescue Committee Report COVID-19 in humanitarian crises: a double emergency. Accessed on: May, 17.
- ISCG. (2019). ISCG monsoon response in Rohingya refugee camps weekly update.Retrieved from https://relie fweb. int/ report/ bangl adesh/ iscg- monsoon- respo nse-r ohing ya- refug ee- camps- weekly-u pdate- 6- 12- september- 2019.
- ISCG ISCG situation report: rohingya Refugee Crisis. Cox’s Bazar |. 2020 https://reliefweb.int/report/bangladesh/iscg-situation-report-rohingya-refugee-crisis-cox-s-bazar-september-2020 September 2020. [Google Scholar]
- Kamal, A.-H., Huda, M., Dell, C., Hossain, S., Ahmed, S. J.G.B. (2020). Translational strategies to control and prevent spread of COVID-19 in the Rohiynga refugee camps in Bangladesh. 1(4).
- Kao, C.-.L., Chan, T.-.C., Tsai, C.-.H., Chu, K.-.Y., Chuang, S.-.F., Lee, C.-.C., et al. (2012). Emerged HA and NA mutants of the pandemic influenza H1N1 viruses with increasing epidemiological significance in Taipei and Kaohsiung, Taiwan, 2009–10. 7(2). [DOI] [PMC free article] [PubMed]
- Kebede T.A., Stave S.E., Kattaa M. May; 2020. Facing Multiple Crises: Rapid Assessment of the Impact of COVID-19 on Vulnerable Workers and Small-Scale Enterprises in Lebanon. [Google Scholar]
- Khan, M.N., Islam, M.M., & Rahman, M.M.J.P.H.i.P. (2020). Risks of COVID19 outbreaks in Rohingya refugee camps in Bangladesh. 1, 100018. [DOI] [PMC free article] [PubMed]
- Kulig J.C., Edge D.S., Townshend I., Lightfoot N., Reimer W. Community resiliency: emerging theoretical insights. J. Community Psychol. 2013;41(6):758–775. [Google Scholar]
- Leach K. Community economic development: localisation, the key to a resilient and inclusive local economy? Local Econ. 2013;28(7–8):927–931. [Google Scholar]
- Longstaff P.H., Armstrong N.J., Perrin K., Parker W.M., Hidek M.A. Building resilient communities: a preliminary framework for assessment. Homeland Secur. Affair. 2010;6(3):1–23. [Google Scholar]
- Masterson J.H., Peacock W.G., Van Zandt S.S., Grover H., Schwarz L.F., Cooper Jr, J. T. Planning for community resilience: a handbook for reducing vulnerability to disasters. J. Am. Plann. Assoc. 2016;82(2):214–215. [Google Scholar]
- Mathavarajah S., Stoddart A.K., Gagnon G.A., Dellaire G. Pandemic danger to the deep: the risk of marine mammals contracting SARS-CoV-2 from wastewater. Sci. Total Environ. 2021;760 doi: 10.1016/j.scitotenv.2020.143346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maxwell J.A. Using numbers in qualitative research. Qual. Inquiry. 2010;16(6):475–482. [Google Scholar]
- Minor O.M. Ebola and accusation: gender dimensions of stigma in Sierra Leone’s Ebola response. Anthropol. Action. 2017;24(2):25–35. [Google Scholar]
- Moser C. The asset vulnerability framework: reassessing urban poverty reduction strategies. World Devel. 1998;26(1):1–19. [Google Scholar]
- Nahiduzzaman K.M., Lai S.-.K. What does the global pandemic COVID-19 teach us? Some reflections. J. Urban Manag. 2020 [Google Scholar]
- Norris F.H., Stevens S.P., Pfefferbaum B., Wyche K.F., Pfefferbaum R.L. Community resilience as a metaphor, theory, set of capacities, and strategy for disaster readiness. Am. J. Community Psychol. 2008;41(1–2):127–150. doi: 10.1007/s10464-007-9156-6. [DOI] [PubMed] [Google Scholar]
- Owhonda G., Maduka O., Nwadiuto I., Tobin-West C., Azi E., Ojimah C. Awareness, perception and practice of COVID 19 prevention among residents of a state in the South-South Region of Nigeria: implications for public health control efforts. medRxiv. 2020 doi: 10.1093/inthealth/ihab046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pal R., Yadav U., Grover S., Saboo B., Verma A., Bhadada S.K. Knowledge, attitudes and practices towards COVID-19 among young adults with Type 1 Diabetes Mellitus amid the nationwide lockdown in India: a cross-sectional survey. Diabetes Res. Clin. Pract. 2020;166 doi: 10.1016/j.diabres.2020.108344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pelling M. 2010. Adaptation to Climate Change: from Resilience to Transformation: Routledge. [Google Scholar]
- Pfefferbaum B.J., Reissman D.B., Pfefferbaum R.L., Klomp R.W., Gurwitch R.H. Handbook of Injury and Violence Prevention. Springer; 2008. Building resilience to mass trauma events; pp. 347–358. [Google Scholar]
- REVA. (2019). Refugee influx emergency vulnerability assessment. Retrieved from Cox's Bazar, Bangladesh: https://www.humanitarianresponse.info/en/operations/bangladesh/assessment/refugee-influx-emergency-vulnerability-assessment-reva-2-0
- Rubinson, L., Mutter, R., Viboud, C., Hupert, N., Uyeki, T., Creanga, A., et al. (2013). Impact of the fall 2009 influenza A (H1N1) pdm09 pandemic on US hospitals. 51(3), 259. [DOI] [PMC free article] [PubMed]
- Lau San, L. Samari, G. Moresky, T. R., Casey S.E., Kachur S.P., Roberts L.F. COVID-19 in humanitarian settings and lessons learned from past epidemics. Nat. Med. 2020;26(5):647–648. doi: 10.1038/s41591-020-0851-2. [DOI] [PubMed] [Google Scholar]
- Schwandt T.A. Sage publications; 2014. The Sage Dictionary of Qualitative Inquiry. [Google Scholar]
- Sen, S.J.W.D. (2020). The pandemic under siege: a view from the Gaza Strip. 135, 105063. [DOI] [PMC free article] [PubMed]
- Shadmi E., Chen Y., Dourado I., Faran-Perach I., Furler J., Hangoma P. Health equity and COVID-19: global perspectives. Int. J. Equity Health. 2020;19(1):1–16. doi: 10.1186/s12939-020-01218-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shammi M., Robi M.R., Tareq S.M. COVID-19: socio-environmental challenges of Rohingya refugees in Bangladesh. J. Environ. Health Sci. Eng. 2020:1–3. doi: 10.1007/s40201-020-00489-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teachout M., Zipfel C. International Growth Centre; 2020. The Economic Impact of COVID-19 Lockdowns in Sub-Saharan Africa. [Google Scholar]
- Truelove S., Abrahim O., Altare C., Lauer S.A., Grantz K.H., Azman A.S. The potential impact of COVID-19 in refugee camps in Bangladesh and beyond: a modeling study. PLoS Med. 2020;17(6) doi: 10.1371/journal.pmed.1003144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ullah A.A. Rohingya crisis in Myanmar: seeking justice for the “stateless. J. Contemp. Crim. Justice. 2016;32(3):285–301. [Google Scholar]
- Ullah A.A., Hossain M.A., Chattoraj D. Covid-19 and Rohingya Refugee Camps in Bangladesh. Intellect. Discourse. 2020;28(2):793–806. -793–806. [Google Scholar]
- Ullah, A.A., Nawaz, F., Chattoraj, D.J.S.S., & Open, H. (2021). Locked up under lockdown: the COVID-19 pandemic and the migrant population. 3(1), 100126. [DOI] [PMC free article] [PubMed]
- UNCHR. (2020). Refugee health workers lead COVID-19 battle in Bangladesh camps. Retrieved December 2020 https://www.unhcr.org/en-us/news/stories/2020/7/5f198f1f4/refugee-health-workers-lead-covid-19-battle-bangladesh-camps.html
- UNHCR. (2019a). Retrieved June 2019 https://www.unhcr.org/figures-at-a-glance.html
- UNHCR CAMP Profiles: Rohingya Refugee Response bangladesh. 2020 [Google Scholar]
- Waller M.A. Resilience in ecosystemic context: evolution of the concept. Am. J. Orthopsychiatry. 2001;71(3):290–297. doi: 10.1037/0002-9432.71.3.290. [DOI] [PubMed] [Google Scholar]
- WHO . 2020. Rohingya Crisis, Situation Report #34. Retrieved from https://www.who.int/docs/default-source/searo/bangladesh/bangladesh—rohingya-crisis—pdf-reports/sitreps/sitreps-2020/who-situation-report-34.pdf?sfvrsn=baa8dff8_7. [Google Scholar]
- WHO . 2020. Sanitation, Hygiene and Waste Management for the COVID-19 Virus. Retrieved from. [Google Scholar]
- WHO. (2020). THE GLOBAL HEALTH OBSERVATORY, Explore a world of health data. https://www.who.int/data/gho/data/indicators/indicator-details/GHO/medical-doctors-(per-10-000-population).
- Wilkinson A. Local response in health emergencies: key considerations for addressing the COVID-19 pandemic in informal urban settlements. Environ. Urban. 2020:503–522. doi: 10.1177/0956247820922843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilkinson A., Conteh A., Macarthy J. Chronic conditions and COVID-19 in informal urban settlements: a protracted emergency. Citie Health. 2020:1–4. [Google Scholar]