Prostate cancer is characterized clinically by slow growth and a relatively good prognosis, but its incidence is increasing rapidly in Japan (1,2). A recent retrospective analysis from the U.S. National Inpatient Sample also demonstrated that prostate cancer was among the most common malignant diseases in patients undergoing percutaneous coronary intervention (3). Early detection by prostate-specific antigen screening and advances in prostate cancer therapy have led to a relatively good prognosis and a lengthy clinical course. Accordingly, we can expect the number of prostate cancer survivors and persons living with prostate cancer to continue to grow.
Prostate cancer incidence increases with age. At the same time, older men demonstrate an increased prevalence of pre-existing lifestyle-related diseases, including cardiometabolic syndrome, resulting in an increased risk of comorbid cardiovascular disease (CVD). We expect that physicians are likely to encounter such conditions accompanying prostate cancer with increased frequency. Physicians, including cardiologists, primary care providers, oncologists, and urologists, need to realize that compared with other types of cancer, prostate cancer involves a long-term interaction with a cardiometabolic syndrome that is closely related to its clinical course. However, the links between prostate cancer and cardiometabolic disease have not been fully characterized, and no clear strategies for preventing and managing cardiometabolic syndrome in patients with prostate cancer have been established.
Therefore, we propose that the emerging link between prostate cancer and cardiometabolic syndrome will become increasingly important as a specialty in cardio-oncology and that greater research and development are needed. Although this link is clinically ceaseless and mutual, we summarize this issue here.
Understanding the Epidemiological Overlap Between Cardiometabolic Syndrome and Prostate Cancer
The causes of prostate cancer are still not fully understood, but some environmental factors are likely to contribute to a certain extent. Associations with factors such as obesity and hypertension that characterize metabolic syndrome have been documented; more specifically, a correlation between these factors and the grade of malignancy of prostate cancer has also been noted, although this relationship is controversial (4). We postulate that modifying these CVD risk factors may also decrease the risk for cancer (5). However, to our knowledge, no prospective study has investigated this exact question in prostate cancer.
In Japan, we have no recent nationwide surveillance or available clinical evidence defining the association between cardiometabolic syndrome and prostate cancer in the clinical setting. We propose that we need to gain a greater understanding of this association by updating real-world data, determining the actual frequency of metabolic syndrome and CVD in patients with prostate cancer, and defining the preventive effects of treatment for cardiometabolic syndrome on the development of prostate cancer. In addition, as has been reported by others, it may be clinically informative to survey the national prevalence of prostate cancer among patients with coronary disease, such as those undergoing percutaneous coronary intervention and/or presenting with acute coronary syndrome. To perform such research, it will be necessary to share relevant clinical information and for the oncologic, urologic, and cardiovascular communities to collaborate.
Cardiometabolic Disorders and Prostate Cancer Therapy
Lifestyle-related diseases, including metabolic syndrome, have been associated with the origins of prostate cancer, and recent evidence has also emerged on the associations between prostate cancer therapy and the onset of metabolic abnormalities and CVD. Androgen deprivation therapy (ADT), which is a major component of prostate cancer therapy, is known to increase several established cardiometabolic risk factors, such as dyslipidemia, body fat, and glycemic abnormalities (6). Therefore, medical providers need to understand that these factors must be carefully managed, especially in the setting of concurrent ADT.
There is still some disagreement, however, on the effects of ADT on the risk of cardiovascular events themselves. Although 1 meta-analysis reported no increased risk (7), more recent reports have determined an increased risk of CVD with ADT (8,9), and it has been noted that this relationship is particularly evident in patients with a prior history of CVD (10,11). Moreover, as with other cancers, the risk of deep vein thrombosis has also been reported (12,13); as such, the risk of CVD associated with ADT cannot be disregarded.
Thus, optimal cardiovascular risk management and prevention of CVD can potentially be beneficial in the delivery of prostate cancer therapy. A thorough assessment of such background risk factors is essential, especially with ADT. Collectively, pre-emptive and diligent management of cardiometabolic disease may be useful to avert the undesirable cardiometabolic effects and the development of CVD that may occur over the clinical course of prostate cancer therapy.
Cardiometabolic Syndrome and Prostate Cancer
Although not specifically limited to prostate cancer, prevalent cardiometabolic disease may be an important factor that can determine the range of options for cancer therapy. Therefore, proper management of underlying metabolic derangements and the prevention of CVD are important to decrease toxicity of cancer therapy and to broaden treatment options maximally. In addition, a primary clinical concern in prostate cancer is the development of coexistent cardiovascular morbidity in parallel with standard prostate cancer therapy and resultant adverse cardiovascular outcomes.
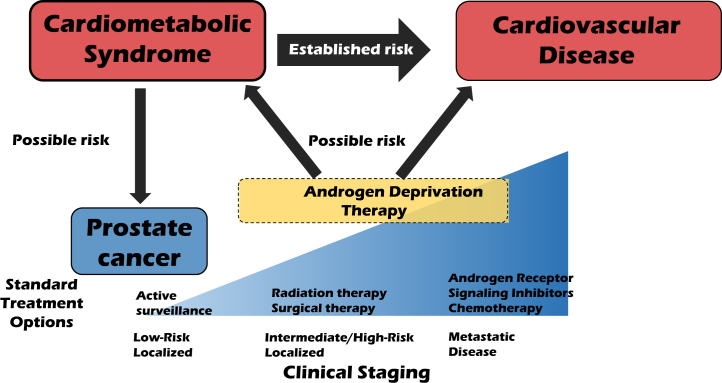
Cardiometabolic disease may potentially contribute to, at least in part, the causes of prostate cancer and may be unfavorably involved to some extent in its clinical course. Meanwhile, ADT may further worsen the metabolic derangements and potentially promote the development of comorbid CVD (Figure 1). More specifically, the natural history of metabolic derangements and consequent CVD and that of prostate cancer are more intimately related compared with other cancers. Thus, refined clinical practice and further studies that focus on the emerging and promising role of care for cardiometabolic disease will become increasingly important topics in cardio-oncology and prostate cancer.
Figure 1.
Clinical Link Between Cardiometabolic Disorders and Prostate Cancer
Components of the metabolic syndrome such as obesity and diabetes are established risk factors for cardiovascular disease and may be risk factors for prostate cancer. Androgen deprivation therapy, which is central to the treatment of prostate cancer, can promote metabolic derangements, although the direct link between androgen deprivation therapy and overt cardiovascular disease is somewhat controversial. We propose that the clinical course of cardiometabolic syndrome and that of prostate cancer care are closely related.
The greatest concern in promoting an understanding and accomplishing this goal may be that physicians, including cardiologists, oncologists, urologists, and primary care providers, do not have enough knowledge about the increased prevalence of prostate cancer and the link between cardiometabolic disorders and the clinical course of prostate cancer. However, because cardiometabolic disorders can be managed and treated, we need to become familiar with such disease links and appropriately screen and manage cardiometabolic disorders in patients with prostate cancer. Furthermore, the clinical and academic connections among cardiologists, oncologists, and urologists may not be sufficient thus far. Accordingly, we do not have enough knowledge to solve these clinical challenges. Given the close relationship between cardiometabolic disease and prostate cancer, however, the top priority is for specialists to collaborate and share accurate and precise information. To accomplish such goals, comprehensive strategies, such as multidisciplinary clinics, greater involvement of the primary care provider, patient education, and public service announcements, are needed. Furthermore, prostate cancer survivorship programs and collaborative studies on risk identification and mitigation are additional challenges. Thus, to promote collaboration among specialists and those strategies, physicians will be required to renew their awareness of why further enhancement and research in cardiometabolic syndrome are needed at each stage of prostate cancer prevention and treatment. Although the ultimate goal is still far away, it is important to take this first step.
Footnotes
Dr. Tanaka has received modest honoraria from Astellas, AstraZeneca, Boehringer Ingelheim, Daiichi-Sankyo, Kowa, Merck, Mitsubishi Tanabe, Novo Nordisk, Taisho Toyama, Takeda, and Teijin. Dr. Node has received honoraria from Eli Lilly, Astellas, Ono, Takeda, Daiichi-Sankyo, Boehringer Ingelheim, MSD (Merck Sharp & Dohme), Mitsubishi Tanabe, and AstraZeneca; has received research grants from Amgen, Teijin, Terumo, Mitsubishi Tanabe, Asahi Kasei, Astellas, Boehringer Ingelheim, and Bayer; and has received scholarships from Bayer, Daiichi-Sankyo, Teijin, Astellas, Takeda, and Bristol-Myers Squibb.
References
- 1.Cancer Registry and Statistics Cancer Information Service, National Cancer Center, Japan. Cancer statistics in Japan. 2017. https://ganjoho.jp/data/reg_stat/statistics/brochure/2017/cancer_statistics_2017_fig_E.pdf Available at:
- 2.Torre L.A., Bray F., Siegel R.L., Ferlay J., Lortet-Tieulent J., Jemal A. Global cancer statistics, 2012. CA Cancer J Clin. 2015;65:87–108. doi: 10.3322/caac.21262. [DOI] [PubMed] [Google Scholar]
- 3.Potts J.E., Iliescu C.A., Lopez Mattei J.C. Percutaneous coronary intervention in cancer patients: a report of the prevalence and outcomes in the United States. Eur Heart J. 2019;40:1790–1800. doi: 10.1093/eurheartj/ehy769. [DOI] [PubMed] [Google Scholar]
- 4.Bhindi B., Locke J., Alibhai S.M.H. Dissecting the association between metabolic syndrome and prostate cancer risk: analysis of a large clinical cohort. Eur Urol. 2015;67:64–70. doi: 10.1016/j.eururo.2014.01.040. [DOI] [PubMed] [Google Scholar]
- 5.Koene R.J., Prizment A.E., Blaes A., Konety S.H. Shared risk factors in cardiovascular disease and cancer. Circulation. 2016;133:1104–1114. doi: 10.1161/CIRCULATIONAHA.115.020406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Melloni C., Roe M.T. Androgen deprivation therapy and cardiovascular disease. Urol Oncol. 2019 Mar 14 doi: 10.1016/j.urolonc.2019.02.010. [E-pub ahead of print] [DOI] [PubMed] [Google Scholar]
- 7.Nguyen P.L., Je Y., Schutz F.A. Association of androgen deprivation therapy with cardiovascular death in patients with prostate cancer: a meta-analysis of randomized trials. JAMA. 2011;306:2359–2366. doi: 10.1001/jama.2011.1745. [DOI] [PubMed] [Google Scholar]
- 8.Carneiro A., Sasse A.D., Wagner A.A. Cardiovascular events associated with androgen deprivation therapy in patients with prostate cancer: a systematic review and meta-analysis. World J Urol. 2015;33:1281–1289. doi: 10.1007/s00345-014-1439-6. [DOI] [PubMed] [Google Scholar]
- 9.Agarwal M., Canan T., Glover G. Cardiovascular effects of androgen deprivation therapy in prostate cancer. Curr Oncol Rep. 2019;21:91. doi: 10.1007/s11912-019-0841-z. [DOI] [PubMed] [Google Scholar]
- 10.Gupta D., Salmane C., Slovin S., Steingart R.M. Cardiovascular complications of androgen deprivation therapy for prostate cancer. Curr Treat Options Cardiovasc Med. 2017;19:61. doi: 10.1007/s11936-017-0563-1. [DOI] [PubMed] [Google Scholar]
- 11.Margel D., Peer A., Ber Y. Cardiovascular morbidity in a randomized trial comparing GnRH-agonist and GnRH-antagonist among patients with advanced prostate-cancer and pre-existing cardiovascular disease. J Urol. 2019;202:1199–1208. doi: 10.1097/JU.0000000000000384. [DOI] [PubMed] [Google Scholar]
- 12.Guo Z., Huang Y., Gong L. Association of androgen deprivation therapy with thromboembolic events in patients with prostate cancer: a systematic review and meta-analysis. Prostate Cancer Prostatic Dis. 2018;21:451–460. doi: 10.1038/s41391-018-0059-4. [DOI] [PubMed] [Google Scholar]
- 13.Nead K.T., Boldbaatar N., Yang D.D., Sinha S., Nguyen P.L. Association of androgen deprivation therapy and thromboembolic events: a systematic review and meta-analysis. Urology. 2018;114:155–162. doi: 10.1016/j.urology.2017.11.055. [DOI] [PubMed] [Google Scholar]