Abstract
The Seasonal Beliefs Questionnaire (SBQ) is a 26-item self-report measure of a winter seasonal affective disorder- (SAD-) specific cognitive vulnerability consisting of maladaptive thoughts about the seasons, light availability, and weather conditions. In a known groups comparison, currently depressed adults with SAD had significantly higher SBQ scores than currently depressed adults with nonseasonal Major Depressive Disorder (MDD) and healthy controls, and the MDD group had significantly higher SBQ scores than controls. Using that database, this study explored the predictive validity of using a SBQ cutoff score to differentiate SAD from MDD. Receiver operator characteristic curve analyses used SBQ total score to predict SAD vs. MDD, SAD vs. control, and MDD vs. control status. SBQ subscale combined score, derived from multivariable logistic regression with SBQ subscales, was examined as an alternative predictor. SBQ total score with a cutpoint of 132 had good predictive ability for distinguishing SAD from MDD (C-statistic = .792, sensitivity = .798, specificity = .794). SBQ subscale combination score slightly improved predictive ability for the SAD/MDD distinction (C-statistic = .813), with better sensitivity (.930) but worse specificity (.571). In contrast, score on a generic measure of depressogenic cognitive vulnerability, the Dysfunctional Attitudes Scale, was poor for differentiating SAD from MDD. SBQ total score was excellent in discriminating SAD cases from controls with a cutpoint of 121 (C-statistic = .962, sensitivity = .939, specificity .873), but had poor sensitivity for discriminating MDD cases from controls. Results support using the SBQ to screen for probable SAD in practice settings.
Keywords: seasonal beliefs, cognitive vulnerability, seasonal affective disorder screening, seasonal affective disorder detection, receiver operator characteristic curve analysis
The Seasonal Beliefs Questionnaire (SBQ) is a 26-item self-report inventory of maladaptive thoughts about the seasons, environmental light availability, and weather (Rohan et al., 2019). Based on the integrative cognitive-behavioral model of winter seasonal affective disorder (SAD; Rohan, Roecklein, & Haaga, 2009), the SBQ was designed to measure a SAD-specific cognitive vulnerability distinct from a more generic cognitive vulnerability to depression. Scale items were originally derived from a content analysis of thoughts reported during group cognitive-behavioral therapy for SAD (CBT-SAD; Rohan, 2008), including negative thoughts about the winter, short photoperiods, environmental cues signaling fall/winter, and inclement weather (e.g., snow, cold, cloud cover) and hyper-positive thoughts about the summer, long photoperiods, environmental cues signaling spring/summer, and temperate weather (e.g., sunshine, blue skies).
Preliminary evidence suggests that extreme seasonal beliefs, as measured by the SBQ, are SAD-specific. The original SBQ development paper (Rohan et al., 2019) included a known groups comparison of currently depressed adults with SAD vs. nonseasonal Major Depressive Disorder (MDD1) in the winter. The SAD group had significantly higher SBQ scores than both the MDD group and the never-depressed/low seasonality control group, and the MDD group had significantly higher SBQ scores than the control group. A generic measure of depressogenic cognitive vulnerability, the Dysfunctional Attitudes Scale (DAS; Weissman & Beck, 1978), showed the opposite pattern of depression group differences: the MDD group scored significantly higher than both the SAD and control groups, and the SAD group scored higher than controls. The group differences on SBQ total score (i.e., SAD > MDD > control) were replicated for four of five SBQ subscales: Global Winter Negativity (GW), Personal Deficiency Related to Winter (PD), Effects from Lack of Light (ELL), and Lack of Perceived Seasonal or Weather Effect (LPSWE)2. The fifth subscale, Global Summer Positivism (GS), appeared most SAD-specific, as the SAD group scored higher than both the MDD and control groups, but the MDD and control groups did not differ.
There is need for a simple scale that can aid in screening to differentiate SAD from MDD in practice settings with adequate sensitivity and specificity to inform whether further assessment is needed to guide clinical decision-making. We strongly suspect that SAD is more likely to be misdiagnosed as MDD than vice-versa because SAD is less prevalent than nonseasonal depression, with an estimated 10–20% of recurrent depressions following a seasonal pattern (Blazer, Kessler, & Schwartz, 1998; Magnusson, 2001), and individuals with SAD anecdotally report that self-awareness of their seasonal pattern developed gradually over time. In using SBQ score to inform the SAD/MDD distinction, sensitivity (i.e., the true positive rate for SAD) is deemed more important than specificity (i.e., the true positive rate for MDD). Diagnosing true SAD as MDD is problematic because certain depression treatments are more commonly used for SAD than for MDD, including light therapy, CBT-SAD, and bupropion hydrochloride extended release (bupropion HCl XL), which is U. S. Food and Drug Administration-approved for the prevention of SAD. Diagnosing true MDD as SAD on the basis of SBQ score is relatively less problematic because a patient with MDD with elevated seasonal beliefs would likely benefit from common SAD treatments, including CBT-SAD to directly address seasonal beliefs. Patients with MDD with elevated seasonal beliefs may have chronic depression that escalates in severity in the winter, termed “SAD with incomplete summer remission” (e.g., Lam et al., 2001).
Several self-report measures of seasonality are designed as brief screeners for SAD to determine if more definitive assessment (e.g., clinical diagnostic interview) is warranted, including the Seasonal Pattern Assessment Questionnaire (SPAQ; Rosenthal, Bradt, & Wehr, 1984), Seasonal Health Questionnaire (SHQ; Thompson & Cowan, 2001), Seasonality Assessment Form (Young et al., 2015), and Personal Inventory of Depression and SAD (Terman et al., 1998) and its self-assessment version (Terman & Williams, 1993). Of these, only the SPAQ and the SHQ have been administered to known samples of patients with SAD vs. MDD. In each case, scale scoring criteria for SAD were used to compare the proportions of true SAD cases correctly identified as having SAD (i.e., sensitivity) and the proportions of true MDD cases correctly identified as not having SAD (i.e., specificity).
Using SPAQ criteria for winter SAD, Mersch et al. (2004) compared 45 patients with SAD to 48 outpatients with a nonseasonal affective disorder, the majority of whom (41/48; 85%) had MDD. Sensitivity was only 44% (i.e., 20/45 SAD cases were correctly classified as having winter SAD), and specificity was 85% (i.e., 41/48 outpatients with a nonseasonal affective disorder were correctly classified as not having winter SAD). Thompson and Cowan (2001) compared 40 patients with SAD to 34 patients with MDD using SPAQ criteria and SHQ criteria that were designed to estimate DSM-IV diagnostic criteria for Major Depression with Seasonal Pattern. Sensitivity was better using SPAQ criteria (i.e., 90%, 36/40 patients with SAD were correctly classified) than SHQ criteria (i.e., 63%, 25/40 patients with SAD were correctly classified). Conversely, specificity was better using SHQ criteria (i.e., 94%, 32/34 patients with MDD were correctly classified) than SPAQ criteria (71%; 24/34 patients with MDD were correctly). Therefore, these measures are not ideal at making the SAD/MDD distinction. Using SPAQ winter SAD criteria, sensitivity was poor and specificity was good in Mersch et al. (2004), and sensitivity was excellent but specificity was fair in Thompson and Cowan (2001). Using the SHQ criteria had excellent specificity and poor sensitivity in Thompson and Cowan (2001). While longitudinal tracking of major depressive episode onset and remission across the seasons spanning multiple years should be predictive of a seasonal vs. a nonseasonal course of depression, no published study has examined this approach, which would be difficult to implement in practice settings.
Here, we test the utility of a one-time self-report measure in screening for SAD, particularly as distinct from MDD, for ease of use clinical settings to inform whether more definitive assessment is warranted. In contrast to prior work, this study tests the predictive ability of using an empirically-derived cutpoint score in making the SAD/MDD distinction and uses a scale designed to measure a SAD vulnerability, rather than SAD symptoms, as predictor. In a secondary analysis of the database used for the known groups comparison in Rohan et al. (2019), we used receiver operator characteristic (ROC) curve analyses to examine the predictive validity of SBQ score for distinguishing between SAD and nonseasonal MDD cases among currently depressed individuals, as well as between SAD cases and controls and MDD cases and controls. The current work makes an incremental contribution over Rohan et al. (2019) in determining optimal SBQ cutpoint for discriminating between groups and reporting sensitivity and specificity. To facilitate translation to screening in clinical practice, we examined total SBQ score as a predictor. We also explored the predictive validity of using a score based on linear combination of SBQ subscale scores to discriminate groups. If the latter metric improves sensitivity and specificity over total SBQ score, it might offset the costs associated with using an equation that weights subscales differently. We expected good predictive validity for SBQ scores in discriminating between SAD and MDD, and stronger predictive ability in making this distinction relative to DAS score. We expected excellent predictive validity in differentiating SAD cases from controls, with substantially better model fit, sensitivity, and specificity than for the MDD/controls distinction.
Methods
Participants
Participants in this study were cases used in the known groups analysis reported in Rohan et al. (2019). They were part of a larger study at the University of Pittsburgh, where this research was approved by the University’s Institutional Review Board. All participants were adults aged 18 or older and were screened with the Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Patient Edition with Psychotic Screen (SCID-I/P; First, Spitzer, Gibbon, & Williams, 2002). Exclusion criteria were: current substance use disorder and/or history of psychotic or bipolar disorders, PTSD, anorexia or bulimia nervosa, or somatic symptom disorders. Controls were additionally excluded for history of any mood disorder. Inclusion criteria were: Major Depressive Disorder, Recurrent with Seasonal Pattern (Currently in Episode) for the SAD group; Major Depressive Disorder (Currently in Episode) for the nonseasonal MDD group; and no history of Major Depressive Episodes and normal range scores on the SPAQ for controls. Participants were not assessed for other psychiatric disorders beyond these diagnostic inclusion/exclusion criteria.
The SAD group included 114 participants, with mean age = 39.3 (SD = 13.3) years, 83% females, 90% White, and 90% non-Hispanic. The MDD group consisted of 35 participants, with mean age = 39.7 (SD = 13.8) years, 57% females, 91% White, and 91% non-Hispanic. Healthy controls were 134 participants, with mean age = 34.0 (SD = 13.3) years, 75% female, 93% White, and 93% non-Hispanic. As reported in the known groups comparison (Rohan et al., 2019), the groups differed significantly on age, F(2, 282) = 5.60, p = .004, and sex distribution, X2(2) = 10.29, p = .0006, but group differences in SBQ scores were robust to adjusting for either age or sex. Both depressed groups were experiencing a current Major Depressive Episode, but the SAD group had significantly more severe symptoms than the MDD group (mean Beck Depression Inventory-Second Edition scores = 22.2 for SAD vs. 16.8 for MDD). However, this did not likely affect the current analyses because the SBQ is not a proxy measure of depression severity, given correlations between SBQ scores and two depression measures in a general sample (N = 536) were significant but small (r = .367 with the Structured Interview Guide for the Hamilton Rating Scale for Depression-Seasonal Affective Disorder Version-Self-Report and r = .403 with the Center for Epidemiologic Studies-Depression Scale; Rohan et al., 2019).
Measures
The following measures were administered as part of the parent study during the winter months, while SAD and MDD cases were experiencing a current major depressive episode.
Seasonal Beliefs Questionnaire (SBQ).
The SBQ (Rohan et al., 2019) is a 26-item self-report inventory of thoughts about the seasons, light availability, and weather conditions. The SBQ’s response format is a 7-point Likert scale based on “how you generally think: 1 = “strongly disagree,” 2 = “disagree very much,” 3 = “disagree slightly,” 4 = “neutral,” 5 = “agree slightly,” 6 = “agree very much,” 7 = “strongly agree.” After reverse-scoring eight items, items are summed for a total score (range = 26–182). The SBQ has five factors: Personal Deficiency Related to Winter (PD; e.g., “I’m a failure in the winter”), Global Summer Positivism (GS; e.g., “I’m always happier when it’s warmer”), Global Winter Negativity (GW; e.g., “I’m not a winter person”), Lack of Perceived Seasonal or Weather Effect (LPSWE; e.g., “Sunlight doesn’t affect my mood”), and Effects from Lack of Light (ELL; e.g., “It’s difficult to feel good on dark, dreary days”). SBQ scores have good internal consistency, convergent and divergent validity, and 2-week test-retest reliability (Rohan et al., 2019).
Dysfunctional Attitudes Scale-Form A (DAS).
The DAS (Weissman & Beck, 1978) is a 40-item measure of depressogenic attitudes, rules, and assumptions. Example items include: “If I don’t set the highest standards for myself, I am likely to end up a second rate person” and “My value depends greatly on what others think of me.” The response format (i.e., 7-point Likert scale for agreement) and scoring is the same as for the SBQ. DAS scores (range = 40–280) have good internal and test-retest reliability and concurrent validity (Weissman & Beck, 1978).
Data Analysis
We conducted receiver operator characteristic (ROC) curve analyses using SBQ total score to predict SAD vs. MDD, SAD vs. control, and MDD vs. control status. For the primary distinction of SAD vs. MDD case status, DAS score was explored as a comparator predictor. As an alternative predictor to total SBQ score, we explored SBQ subscale combined score, derived from multivariable logistic regression with SBQ subscales. Combined score was generated by using the SBQ subscale data from each subject in the logistic regression prediction equations. For each predictive model, we generated the Area Under the Curve (AUC or C-statistic) as a measure of model fit and the optimal cutpoint score on the predictor for the distinction between groups (with sensitivity and specificity weighted equally). The optimal cutpoint score was determined as the score at which Youden’s Index (sensitivity + specificity − 1) was maximized (Pandey & Jain, 2016). In this analysis, sensitivity refers to the true positive rate (i.e., the proportion of true SAD cases correctly classified), and specificity refers to the true negative rate [i.e., the proportion of true comparator (MDD or control) cases correctly classified]. In discriminating between MDD and control cases, sensitivity refers to the true positive rate (i.e., the proportion of true MDD cases correctly classified), and specificity refers to the true negative rate (i.e., the proportion of controls correctly classified). We applied Carter et al.’s (2016) criteria to interpret C-statistics: 1.0 = perfect prediction (no false negatives and no false positives), 0.9–0.99 = excellent, 0.8–0.89 = good, 0.7–0.79 = fair, 0.51–0.69 = poor, and .50 = no better than chance. For our intended purpose of discriminating SAD from MDD, we considered a C-statistic ≥ .80 as sufficiently predictive to identify probable SAD cases for more definitive assessment, thereby potentially directing the clinician to SAD-specific treatment recommendations.
Results
C-statistics, SBQ total score and subscale combination score cutpoints, sensitivity, and specificity for predicting dichotomous group status are presented in Table 1. The prediction equations derived from multivariable logistic regression with all SBQ subscales as predictors vs. the three group comparison variables used to create “SBQ scale combined score” are:
Table 1.
Performance of receiver operating curve Seasonal Beliefs Questionnaire total score and subscale combination score cutpoint criteria in predicting seasonal affective disorder, nonseasonal Major Depressive Disorder, or control status
| Predictor | Group Outcome Variable | C-Statistic | Cutpoint (≥) | Sensitivity | Specificity |
|---|---|---|---|---|---|
| SBQ total | SAD vs. MDD | 0.792 | 132 | 0.798 | 0.714 |
| SBQ scale score | SAD vs. MDD | 0.813 | 808 | 0.930 | 0.571 |
| SBQ total | SAD vs. Control | 0.962 | 121 | 0.939 | 0.873 |
| SBQ scale score | SAD vs. Control | 0.976 | 1191 | 0.991 | 0.903 |
| SBQ total | MDD vs. Control | 0.789 | 118 | 0.600 | 0.858 |
| SBQ scale score | MDD vs. Control | 0.842 | 399 | 0.743 | 0.910 |
| DAS total | SAD vs. MDD | 0.636 |
Note. SBQ = Seasonal Beliefs Questionnaire, DAS = Dysfunctional Attitudes Scale-Form A, SAD = Seasonal affective disorder patient status, MDD = nonseasonal Major Depressive Disorder patient status, Control = healthy control status, defined as no history of Major Depressive Disorder and global seasonality score in the normal range. Sensitivity (i.e., the proportion of true positives correctly classified) and specificity (i.e., the proportion of true negatives correctly classified) is at or above the cutpoint score on the predictor.
In differentiating between SAD and nonseasonal MDD, total SBQ score had adequate predictive ability (C-statistic = .792), with good sensitivity [i.e., 79.8% true positive (SAD) cases were correctly classified] and reasonable specificity [i.e., 71.4% true negative (MDD) cases were correctly classified] using a cutpoint score of 132. The corresponding ROC curve is displayed in Figure 1. The optimal combination of maximum sensitivity and specificity, corresponding to an SBQ score of 132, is shown at the point in the curve that is closest to the upper left corner (i.e., the point with 1 - specificity value of 0.43). The diagonal represents the line of equality (i.e., random chance in predicting SAD vs. MDD case status). (See Supplemental Table for sensitivity and specificity across a range of total SBQ score cutpoints for distinguishing SAD vs. MDD case status). SBQ subscale combination score improved overall model fit (C-statistic = .813) and sensitivity (.930), but worsened specificity (.571). In contrast, DAS score was poor at discriminating SAD from MDD (C-statistic = .636).
Figure 1.
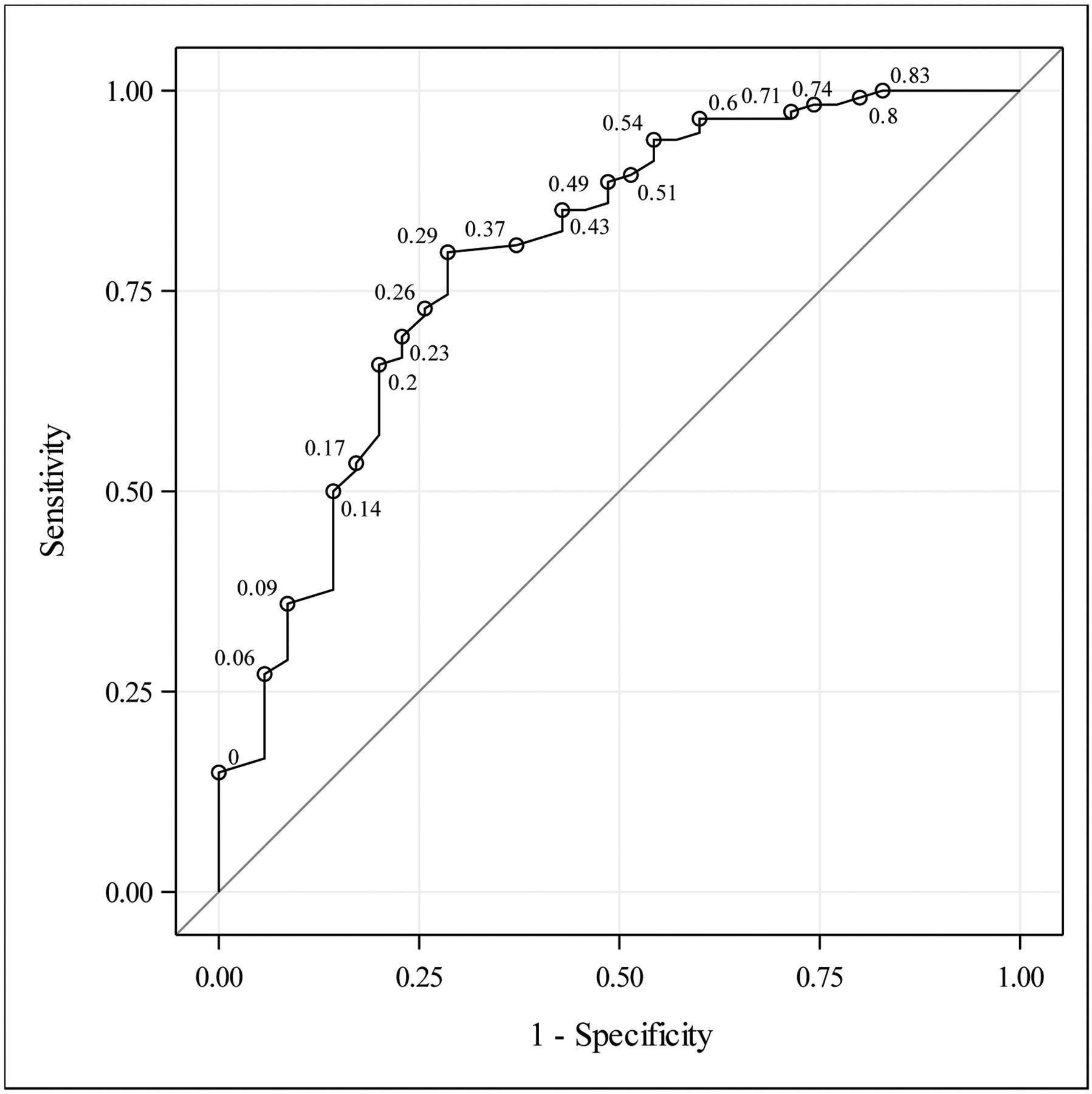
The receiver under the operating characteristic (ROC) curve for predicting seasonal affective disorder vs. nonseasonal Major Depressive Disorder case status using Seasonal Beliefs Questionnaire total scores. Points labeled by (1 - specificity) value.
SBQ total score had excellent predictive validity for distinguishing SAD cases from controls (C-statistic = .962), with excellent sensitivity [i.e., 93.9% true positive (SAD) cases correctly classified] and good specificity [i.e., 87.3% true negative (control) cases correctly classified] using a cut score of 121. SBQ combination score improved model fit (C-statistic = .976), sensitivity (.991), and specificity (.903).
Although model fit was adequate for differentiating MDD cases from controls on the basis of SBQ total score (C-statistic = .789) and specificity was good [i.e., 85.8% true negative (control) cases correctly classified] using a cutpoint of 118, sensitivity was poor with only 60% of true MDD cases correctly classified. The predictive model fit (C-statistic = .842), sensitivity (.743), and specificity (.910) were all improved by using the SBQ combination score.
Discussion
These results support the predictive validity of score on a one-time self-report measure, the SBQ, to aid in identifying true cases of SAD among patients presenting with depression in clinical settings. Accurately detecting cases of seasonal (vs. nonseasonal) Major Depressive Disorder guides the clinician to implement first-line SAD treatments, such as light therapy, CBT-SAD, and preventive bupropion HCl XL. Using SBQ total score to predict SAD vs. MDD patient status, model fit was very close to our a priori threshold for sufficient predictive validity to identify likely SAD cases for more definitive assessment to inform decision-making about depression treatment recommendations (observed C-statistic = .792 vs. threshold ≥ .80), with good sensitivity for detecting true SAD cases and reasonable specificity for detecting true negative (MDD) cases using a cutpoint score ≥ 132. Using a linear combination of SBQ subscale scores, derived from multivariable logistic regression, improved model fit above our threshold (C-statistic = .813), but due to the accompanying loss in specificity for differentiating MDD from SAD, we recommend using SBQ total score as the better predictor. Clinical utility for the SBQ as an initial SAD screen is high, given that the SBQ is a freely available, 26-item self-report questionnaire that takes approximately 5 minutes to complete and is simple to score. Patients could potentially complete the SBQ in the waiting room to help inform whether further assessment for SAD is warranted. The accepted diagnostic standard for SAD is clinical diagnostic interview focused on the temporal course of major depressive episode recurrence and remission, according to DSM-5 criteria for the Seasonal Pattern course specifier. SBQ score can help clinicians identify cases for whom the benefits of conducting a diagnostic interview (i.e., accurate SAD diagnosis to guide treatment) outweigh the costs (e.g., investment of time and resources).
SBQ total score easily distinguished SAD cases from never-depressed, low seasonality controls and, therefore, could be used in both research and clinical settings for this purpose. Given that combined SBQ subscale score conferred little improvement for this purpose beyond already excellent model fit, sensitivity, and specificity using the total score, we recommend using SBQ total score for simplicity in differentiating SAD cases from controls. As expected, SBQ score is substantially better at distinguishing patients with SAD from patients with MDD and controls than it is at differentiating MDD cases from controls. This aligns with the face validity of the SBQ as a measure of SAD-specific cognitions. We do not recommend the SBQ for distinguishing MDD from controls because it had poor sensitivity for that purpose (i.e., only 60% of true MDD cases correctly classified).
Using SBQ total score to discriminate SAD from nonseasonal MDD appears to represent an improvement over using the Seasonal Pattern Assessment Questionnaire (SPAQ) or the Seasonal Health Questionnaire (SHQ) for this purpose. Future research should subject these previously used screening measures and other measures to ROC curve analysis. The ROC approach empirically derives cutpoint scores to differentiate groups with the best combined sensitivity and specificity, which represents an improvement over comparing groups on the proportions that meet the scale’s (possibly arbitrary) criteria for winter SAD. Another candidate for this type of ROC analysis is the unpublished Seasonal Attitudes Scale (SAS; Sigmon, Rohan, Boulard, Whitcomb, & Dorhofer, 2000), which, like the SBQ, discriminated between a sample of currently depressed patients with SAD, currently depressed patients with nonseasonal MDD, and never-depressed controls (i.e., SAD > MDD > controls on SAS scores; Sigmon et al., 2007).
Unfortunately, we did not code for single versus recurrent MDD in the nonseasonal MDD group. Future studies should examine the predictive validity of SBQ score in distinguishing SAD from recurrent vs. single episode MDD. Given that participants were assessed in the winter, future work should also determine whether SBQ score discriminates between groups in other seasons. Although the SBQ is designed as a trait-like measure of “how you generally think,” the degree of fluctuation in scores from the depressed to the remitted state is not known.
These results, coupled with the prior known groups comparison of patients with SAD, patients with nonseasonal MDD, and controls (Rohan et al., 2019), lend further support that extreme seasonal beliefs are a SAD-specific cognitive construct. As an advantage over symptom-based measures for distinguishing SAD vs. nonseasonal MDD, seasonal beliefs, as measured by the SBQ, represent a malleable treatment target and potentially a cognitive vulnerability to SAD. A recent clinical trial comparing CBT-SAD to light therapy in 177 adults with SAD found evidence that seasonal beliefs mediate acute outcome in CBT-SAD (Rohan, Burt, Camuso, Perez, & Meyerhoff, 2020). Using parallel-process growth models, CBT-SAD promoted greater decreases in SBQ scores during treatment than light therapy, and these changes were related to decreases in symptoms only in CBT-SAD (Rohan et al., 2020). In contrast, depressogenic attitudes (DAS scores) improved comparably during CBT-SAD and light therapy, and the DAS did not mediate acute outcome in CBT-SAD. The SBQ development study (Rohan et al., 2019) reported that greater change in SBQ scores during CBT-SAD was associated with a lower risk of depression recurrence following CBT-SAD two winters later, whereas change in SBQ score was unrelated to risk of recurrence two winters later following light therapy. In contrast, DAS change during treatment was unrelated to recurrence following either treatment. It is theoretically meaningful that the SBQ both discriminates SAD from MDD cases and is at least a mediator, and potentially a mechanism, of CBT-SAD’s effects.
In conclusion, we advocate use of the SBQ as a simple initial screen for SAD in practice and research settings with adequate sensitivity and specificity for differentiating SAD from MDD to determine whether more definitive assessment with clinical interview is warranted. The resulting algorithm, “If SBQ total score ≥ 132, conduct clinical interview for Seasonal Pattern course specifier,” should increase efficiency in guiding clinicians to SAD-specific treatment options. This strategy should help guard against misdiagnosing SAD as MDD, shortening time to accurate diagnosis and implementing effective treatment for individuals with SAD.
Supplementary Material
Public Significance Statement.
This study tested the predictive ability of Seasonal Beliefs Questionnaire (SBQ) score in differentiating between cases of seasonal vs. nonseasonal major depression. Results support using SBQ total score with a cutpoint ≥ 132 in initial screening for making this distinction in clinical practice, based on sufficient sensitivity (i.e., 79.8% true positive rate) and specificity (i.e., 79.4% true negative rate) to warrant further assessment.
Acknowledgments
This work was supported by the National Institute of Mental Health (grants R03MH096119-01A1 and R01MH103313-02 awarded to Kathryn A. Roecklein). Jonah Meyerhoff was supported by a grant from the National Institute of Mental Health (T32 MH115882). Jonah Meyerhoff was supported by a grant from the National Institute of Mental Health (T32 MH115882). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The authors have no financial or nonfinancial competing interests.
Footnotes
The abbreviation “MDD” is used to refer to nonseasonal major depressive disorder from this point forward.
LPSWE subscale items reflect lack of attention to, and perceived irrelevance of, weather and season cues with respect to mood. Subscale items are reverse-scored, such that SAD cases attribute the largest effects of season and weather on mood.
Contributor Information
Kelly J. Rohan, Department of Psychological Science, University of Vermont
Jonah Meyerhoff, Department of Preventive Medicine, Northwestern University Feinberg School of Medicine.
Kathryn A. Roecklein, Department of Psychology, University of Pittsburgh
References
- Blazer DG, Kessler RC, & Schwartz MS (1998). Epidemiology of recurrent major and minor depression with a seasonal pattern: The National Comorbidity Survey. British Journal of Psychiatry, 172(2), 164–167. 10.1192/bjp.172.2.164 [DOI] [PubMed] [Google Scholar]
- Carter JV, Pan J, Rai SN, & Galandiuk S (2016). ROC-ing along: Evaluation and interpretation of receiver operating characteristic curves. Surgery, 159(6), 1638–1645. 10.1016/j.surg.2015.12.029 [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, & Williams JBW (2002). Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Patient Edition with Psychotic Screen (SCID-I/P). New York State Psychiatric Institute. [Google Scholar]
- Lam RW, Tam EM, Yatham LN, Shiah I-S, & Zis AP (2001). Seasonal depression: The dual vulnerability hypothesis revisited. Journal of Affective Disorders, 63, 123–132. 10.1016/S0165-0327(00)00196-8 [DOI] [PubMed] [Google Scholar]
- Magnusson A (2000). An overview of epidemiological studies on seasonal affective disorder. Acta Psychiatrica Scandinavica, 101(3), 176–184. 10.1034/j.1600-0447.2000.101003176.x [DOI] [PubMed] [Google Scholar]
- Pandey M, & Jain A (2016). ROC curve: Making way for correct diagnosis. PharmaSUG 2016 Conference Proceedings. https://www.pharmasug.org/proceedings/2016/SP/PharmaSUG-2016-SP11.pdf [Google Scholar]
- Rohan KJ (2008). Coping with the seasons: A cognitive-behavioral approach to seasonal affective disorder. Therapist guide. In the Treatments that Work™ Series. New York, NY: Oxford University Press. https://www.oxfordclinicalpsych.com/view/10.1093/med:psych/9780195341089.001.0001/med-9780195341089 [Google Scholar]
- Rohan KJ, Burt KB, Camuso J, Perez J, & Meyerhoff J (2020). Applying experimental therapeutics to examine cognitive and chronological vulnerabilities as mediators of acute outcomes in CBT-SAD and light therapy for winter depression. Journal of Consulting and Clinical Psychology, 88(8), 786–797. 10.1037/ccp0000499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rohan KJ, Meyerhoff J, Ho S, Roecklein KA, Nillni YI, Hillhouse JJ, DeSarno MJ, & Vacek PM (2019). A measure of cognitions specific to seasonal depression: Development and validation of the Seasonal Beliefs Questionnaire. Psychological Assessment, 31(7), 925–938. 10.1037/pas0000715 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rohan KJ, Roecklein KA, & Haaga DAF (2009). Biological and psychological mechanisms of seasonal affective disorder: A review and integration. Current Psychiatry Reviews, 5(1), 37–47. 10.2174/157340009787315299 [DOI] [Google Scholar]
- Rosenthal NE, Bradt GH, & Wehr TA (1984). Seasonal Pattern Assessment Questionnaire. Bethesda, MD: National Institute of Mental Health. [Google Scholar]
- Sigmon ST, Rohan KJ, Boulard NE, Whitcomb SR, & Dorhofer DM (2000). Development and validation of the Seasonal Attitudes Scale. Paper presented at the meeting of the Association for the Advancement of Behavior Therapy, New Orleans, LA. [Google Scholar]
- Sigmon ST, Whitcomb-Smith S, Boulard NE, Pells JP, Hermann BA, Edenfield TM, LaMattina SM, & Shartell JG (2007). Attentional bias and psychophysiological arousal in seasonal and nonseasonal depression. Cognitive Therapy and Research, 31, 619–638. 10.1007/s10608-006-9029-6 [DOI] [PubMed] [Google Scholar]
- Terman M, Terman JS, & Williams JBW (1998). Seasonal affective disorder and its treatments. Journal of Practical Psychiatry and Behavioral Health, 5, 287–303. [Google Scholar]
- Terman M & Williams JBW (1993). Personal Inventory for Depression and SAD—Self-Assessment Version (PIDS-SA). New York, NY: New York State Psychiatric Institute and Department of Psychiatry. [Google Scholar]
- Thompson C, & Cowan A (2001). The Seasonal Health Questionnaire: A preliminary validation of a new instrument to screen for Seasonal Affective Disorder. Journal of Affective Disorders, 64(1), 89–98. 10.1016/S0165-0327(00)00208-1 [DOI] [PubMed] [Google Scholar]
- Weissman A, & Beck AT (1978). Development and validation of the Dysfunctional Attitude Scale: A preliminary investigation. Paper presented at the annual meeting of the American Educational Research Association, Toronto, Ontario, Canada. [Google Scholar]
- Young MA, Hutman P, Enggasser JL, & Meesters Y (2015). Assessing usual seasonal depression symptoms: The Seasonality Assessment Form. Journal of Psychopathology and Behavioral Assessment, 37(1), 112–121. 10.1007/s10862-014-9440-3 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


