Introduction
Arthritis is well known in all cultures, with medical descriptions of inflammatory arthritis dating as early as the writings of Hippocrates,1 and paleontological evidence dating back 150 million years.2 Today, the data regarding the prevalence of these diseases remains scant, but suggest that close to 300 million people around the world live with arthritis.3 In terms of years lived with disability (YLD), arthritis and allied disorders account for 21.2%, second only to mental health issues.4 Though often associated with aging, in reality, arthritis can manifest at any age, even in childhood. In the US, approximately 300,000 children are affected by pediatric forms of arthritis.5
In the modern era, the term “arthritis” refers to more than 100 conditions that involve gradual erosion of and pain in joints. Arthritis remains the most prevalent cause of disability in the US, affecting 1 in 5 adults.6,7 This includes an estimated 52.5 million Americans with a doctor diagnosed arthritis, and 22.7 million with activity limitations due to the disease.7 In the next two decades, the number of people affected by arthritis is expected to approach a quarter of the population.8
Types of Arthritis
In general terms, the many types of arthritis can be grouped into a handful of broad classes, the most prevalent of which are osteoarthritis and a separate class of autoimmune disease types such as rheumatoid arthritis.
Osteoarthritis
Osteoarthritis (OA) is, by far, the most common form of arthritis, affecting as much as 13% of the population.9 On the basis of Framingham Study data, approximately a third of adults show radiographic signs of OA.10
At ages greater than 65, 80-90% of adults may show signs of OA, even if no symptoms are present.11 The prevalence of OA is increasing, consistent with aging of the baby boomer generation. Prevalence has risen by approximately 6 million people to 27 million since 1995.12
Whether associated with age, degeneration, secondary to trauma, or other conditions (such as rheumatoid arthritis), OA is characterized by progressive breakdown of cartilage and erosion of bone. OA can be found in any cartilaginous joint in the body, particularly those that bear weight or are subjected to trauma. Risk factors for OA include weight, age, genetics, and history of joint injuries. While several genes have been implicated in OA, the largest genetic risk factor for OA remains gender. Women are at approximately twice the risk as males for developing degenerative OA in any joint, though particularly the knee.13
Weight has been established as a risk factor in many studies, showing a dose dependent relationship to risk of knee and hip OA, but also hand.14 The relationship of weight to OA is thus not limited to weight bearing joints. Pro-inflammatory cytokines released from adipose tissue may account for half of the association between BMI and OA.15
Sports injuries are a notable risk in that they can result in secondary post-traumatic OA early in life.
Approximately half of young adults with knee injuries, often sustained in sports activities, will go on to develop radiographic evidence of OA in the affected knee. In a study of 1012 patients with a history of knee ligament injuries, injuries sustained before age 30 were associated with increased incident of post-traumatic OA 10-15 years after the injury. Those injuries that were sustained after age 30 had a reduced timeline (5 years) before observation of radiographic changes.16,17 Treatments are generally designed to alleviate pain and improve function, but are not necessarily curative. Treatments for both primary and secondary osteoarthritis generally include non-pharmacologic interventions such as weight loss, unloading and bracing of joints where possible18 chondroitin or the combination; and arthroscopic lavage or debridement.
Data Sources
We abstracted data from 42 randomized, controlled trials (RCTs). Exercise, self-management programs and education are also routinely used as evidence-based modalities. Of these, a recent meta-analysis performed by the Agency for Healthcare Research and Quality concludes exercise as the only intervention sufficiently backed by high quality evidence.19 There are no disease modifying pharmacological interventions for OA (though they under active investigation). Once disease has progressed significantly such that non-operative modalities show limited response, several surgical techniques are available to help both restore function to the joint and decrease the pain.
Rheumatoid Arthritis
Rheumatoid arthritis (RA) is the most common type of autoimmune inflammatory arthritis affecting 1.5 million US adults.20,21 RA is a systemic disease, affecting many organs and body systems. Tenderness at joint lines and symmetrical swelling are the most frequent symptoms of RA22 though fever, weight loss, and fatigue may also be present. If left untreated or inappropriately treated, RA can cause irreversible joint damage, reducing quality of life. Without active management, joint deformation may occur. Though not typically considered life-threatening, life expectancy in RA patients is generally 5-10 years less than population mean.23
Risk factors for RA and other autoimmune inflammatory arthritis likely involve both genetic and environmental factors. Having a family history of RA increases risk of developing RA by a factor of 3-5.24 As in osteoarthritis, women are more at risk for RA than men.25 Amongst environmental exposures, smoking is the best- documented environmental risk.26
Though diagnosing RA can be a difficult process, early diagnosis and treatment (within the first 6-months of symptom onset) is associated with better long-term health outcomes. Often, RA diagnosis is challenging, particularly in its early stages, because symptoms may share features with both other autoimmune diseases and many other musculoskeletal disorders (such as tendonitis or synovitis). As no one test is pathognomic for RA, physicians often rely on the history, physical examinations, blood tests, and radiographic imaging to diagnose RA. The 2010 American College of Rheumatology (ACR) and European League Against Rheumatism (EULAR) classification criteria for rheumatoid arthritis are the standard for diagnosis and study of RA.27
RA is often only one of multiple disease processes ongoing in a patient. According to the 2007 National Health Interview Survey, 47% of US adults with any form of arthritis have at least one additional comorbidity. Focusing on RA, on average, an established RA patient will commonly have two or more additional comorbid conditions.28 Chronic respiratory conditions, diabetes, cardiovascular disease, and mental health conditions are the most common comorbidities but autoimmune disorders and even osteoarthritis are not uncommon.
Like OA, RA imposes a significant impact on quality of life for those diagnosed. A study that examined self- reported quality of life for people with RA reported that people were 30% more likely to need help with personal care and twice as likely to have activity limitations when compared to controls.29 Several studies have documented significant negative impact on the work lives of people diagnosed with RA. Early and aggressive treatment of RA reduces risk of developing work disabilities - very much akin to the improved health incomes mentioned above.30
There are several treatments available for RA. To address the musculoskeletal symptoms, the non- pharmacologic mainstays used for OA are often also useful in RA (weight loss, joint bracing, self- management, education & exercise). In addition the same first line pharmacologic treatments used to for both primary and secondary OA (mostly NSAIDs) is often trialed for RA. However, the main recommended approach for the treatment of RA includes non-biologic DMARDs to reduce disease activity and prevent joint damage, usually prescribed within the first 3 months of diagnosis. If treatment with a non-biologic DMARD is unsuccessful, the ACR guidelines recommend graduating to a biologic DMARD.31 There are several biologic DMARDs available to patients; prescribers must consider disease activity, signs, symptoms, and patient preference when selecting a
Transition to a biologic is not curative but rather is an attempt to put the autoimmune disease process into remission for that specific patient. In fact, there is a high failure rate of biologic drugs in RA (and all autoimmune) patients. Of rheumatoid arthritis patients who took a first-generation biologic for at least 6 months, approximately 40-50% failed to meet the American College of Rheumatology criteria for 50% improvement. Of those patients who failed to meet this improvement criteria threshold on the initial on biologic, 40% were switched to another biologic by their rheumatologist.32 Overall, only a third of patients will achieve remission early in the course of the disease, necessitating frequent experimentation and switching between medications’ function and quality of life over the first two years of early rheumatoid arthritis (ERA).33
Economic Costs and Public Health Impact
In Delaware, 2015 data suggests approximately 193,000-207,000 people with arthritis, of whom 42% are inactive. This data positions Delaware as having an intermediate burden of arthritis relative to other states. Estimates of the total direct and indirect costs due to arthritis in Delaware total $363 Million annually.34,35
Across the nation, these estimated costs annually total more than $580 Billion for arthritis and related conditions.36 In general, these numbers suggest arthritis costs states about 1% of GDP,37 potentially limiting affected persons from walking a few blocks or climbing a flight of stairs. In reality, health care costs and volumes, particularly for pharmacologic treatment of inflammatory arthritis and surgical treatment of OA, have risen dramatically, and these numbers are likely to underestimate expenses. Direct costs related to arthritis and related disorders are staggering, accounting for as much as 7% of total aggregate hospital costs, and represent one of the most expensive conditions (OA) billed to private insurers.38 These hospital numbers also do not account for post-hospital costs such as nursing home, assisted living or home health costs. Severe osteoarthritis and mobility issues remain amongst core factors in decisions regarding nursing home placements.39 Indirect or secondary costs due to arthritis also contribute significantly to health care costs but are harder to track due the nature of coding for both diagnosis and treatment. For example, costs related to falls are a significant cost driver and data shows arthritis patients are substantially greater risk40 but which of those falls is primarily due arthritis complications versus other medical complications (such as syncope, hypoglycemia, arrhythmias) are harder to track.
Out of pocket expenses to patients are also costly. Evidence exists to show that increases in out-of-pocket expenses result in significant increases in abandonment of disease modifying RA therapies41 with clear implications for health outcomes. People with arthritis are also heavy consumers of complementary and alternative medicines (CAM). Approximately 41% of patients use some form of CAM, with a quarter of patients self-managing with vitamins, supplements, and other biologically based modalities,42 representing additional elective expenses related to arthritis self-management.
Despite the heavy costs of care, Federal spending on arthritis research in FY17 is estimated at $222 million.43 Conservatively, this suggests a ratio of only one dollar spent on therapeutic research for every 600 dollars spent on care. The public health implications of arthritis are not limited to physical manifestations. One third of patients experience significant anxiety or depression, with anxiety being approximately twice as prevalent as depression.44 In these patients, several factors may contribute to the depression, including reductions in physical activity and social support, as well as chronic pain and functional disabilities. Furthermore, the fact that arthritis affects juvenile populations markedly ties arthritis to other issues of national public health debate, namely sports safety and obesity.
Limited mobility creates a “vicious circle” in the context of arthritis, contributing to weight gain, which in turn is a risk factor for osteoarthritis. Modest weight loss may have dramatic consequence on pain and OA risk45 based on a sample of a defined population.
Long-term consequences of sports injuries are particularly pronounced. In women, knee injuries sustained in their late teens and early twenties place them at a 51% risk for secondary (post-traumatic) OA by the time they reach their 30s. This is equivalent to the risk of primary (degenerative) OA seen in women in their 70s and 80s.46
Public Health Priorities
In light of the soaring public health consequences of arthritis, the CDC and Arthritis Foundation (AF) partnered in 2010 with academic researchers to focus attention on specific public health recommendations related to osteoarthritis. “A National Health Agenda for Osteoarthritis 2010” makes 10 specific recommendations for public health policy following three main themes.47
Establish supportive policies, communication initiatives and strategic alliances for OA prevention and management;
Initiate needed research to better understand the burden of OA, its risk factors, and effective strategies for intervention; and
Ensure the availability of evidence-based intervention strategies-such as self- management education, physical activity, injury prevention, and weight management and healthy nutrition-to all Americans with OA.
Available Interventions
Providers have many opportunities to offer public health interventions in their communities. In general, most interventions focus on promoting self-management and arthritis appropriate exercise. The CDC provides a compendium of recommended evidenced based interventions, and a separate group of emerging programs with promising, but more limited supportive data (See Table 1 and Figure 1).48
Table 1. CDC Recommended and Promising Intervention Programs for Self-Management and Arthritis Appropriate Exercise48.
| Physical Activity | Self Management | |
|---|---|---|
| Recommended | Active Living Every Day | Arthritis Self-Management Program Chronic Disease Self-Management Program Tomando Control de su Salud (Spanish Chronic Disease Self-Man- agement Program) Programa de Manejo Personal de la Artritis (Spanish Arthritis Self- Management Program) |
| Enhance Fitness | ||
| Fit & Strong! | ||
| Walk With Ease (Group-Delivered) | ||
| Promising | Arthritis Foundation Aquatics Program | The Arthritis Toolkit |
| Walk with Ease (Self-Directed) | Better Choices, Better Health (Internet-delivered) | |
| Arthritis Foundation Exercise Program |
Figure 1.
Walk With Ease
The Arthritis Foundation Walk With Ease Program is an evidence-based self-guided or community exercise program recommended by the CDC.49 This multilingual program has been shown specifically to reduce pain associated with arthritis,.50 walk with ease, and improve work place activity limitations).51
While these tools may not be available in all communities, there are resources such as State Coordinators (https://www.cdc.gov/arthritis/partners/state_coordinators.htm) or the Arthritis Foundation “Arthritis Resource Finder” (http://resourcefinder. arthritis.org/) that have been developed to help providers and patients find local Arthritis Foundation and other community programs (Figure 2). In addition, the AF also provides both a rich resource of online information, including exercise and pain management toolkits to assist the patient community (http://www.arthritis.org/living-with-arthritis/tools-resources/) and a 24 hour seven day a week hotline (1-844-571-HELP), staffed by licensed social workers, to help connect patients with resources.
Figure 2.
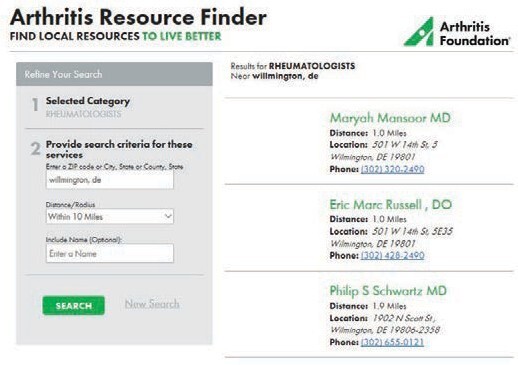
Arthritis Foundation Resource Finder Tool
The Arthritis Foundation Resource Finder tool for can be used to find local physicians, as well as arthritis appropriate community programs.
Education and Advocacy
Education
Improving the quality of life for people with arthritis in the United States is the top priority for CDC’s arthritis program.48 The CDC Arthritis Program recommends evidence-based programs that are proven to improve the quality of life for people with arthritis. The AF and the CDC work in tandem to disseminate life-changing information and resources, provide access to optimal care, create advancements in science, and facilitate robust community connections. Specific partner projects include providing consumer arthritis information and referral services through a toll-free helpline, collaborating with the National Council on Aging to market and promote evidence-based online arthritis and chronic disease self-management education programs, dissemination of the AF’s Walk with Ease program through large and multisite work site systems, and collaborating with the University of North Carolina and others to facilitate national public health action addressing Osteoarthritis through the Osteoarthritis Action Alliance.
Advocacy
People with arthritis face unique barriers to care including high costs of treatment, difficulty accessing medications, scarcity of specialists and coinsurance that limits access to treatment. It is hard for any patient to fight the battle alone. Advocacy can be a significant force for influencing health policy and increasing the understanding and visibility of the patient experience.
The topic of health is often a political endeavor as much as a medical one causing lawmakers to rethink their relationships with the populations they serve.52 Public health advocates need to ensure individual patient stories are being heard and told from the patient’s point of view.
Through the AF’s nationwide network of committed Advocates and annual events arthritis patients, caregivers, providers, and supporters learn to raise their visibility by addressing key policy issues on both the state and federal levels with lawmakers, insurers, employers and regulators. With the help of advocates AF fights to conquer all types of arthritis and make a positive impact on the lives of those affected, pushing for policies and laws that make health care more accessible.
Delaware Education and Advocacy
The Arthritis Foundation has widespread impact in the State of Delaware. With the help of almost 300 AF Delaware advocates, important patient-centric legislation has been successfully passed in the state. In 2013, Out of Pocket Cost Limits (Senate Bill 35) passed and went into effect in 2014. The law is significant because the specialty drug copayment or coinsurance limitation caps out of pocket costs to no more than $150 per month per specialty-tier medication (e.g., biologics). In 2014, DE Biosimilars (Senate Bill 118) was successfully passed and made effective in 2015. This law allows pharmacists to substitute biologic medications with new, interchangeable and potentially less expensive biosimilar medications when they arrive on the market. Bill 118 also ensures patients and their physicians are notified when a substitution occurs, resulting in a complete and accurate patient medical record. And, if a physician does not recommend a substitution for clinical reasons, they can stipulate that the prescription be dispensed as written. Both pieces of legislation increase access to life saving treatments for patients with arthritis and help lower the cost of arthritis care in Delaware. Through these kinds of advocacy efforts, arthritis patients now have access to these new life-changing medications and the arthritis cost curve has been bent in Delaware.
Additionally, the Arthritis Foundation is committed to providing educational tools to DE residents. In 2016, more than 7,830 individuals accessed the foundations online support tools and nearly 3,000 residents received Arthritis Today magazine. Further, specific to Delaware there are many local education and advocacy opportunities. The Arthritis Foundation hosts the Walk to Cure Arthritis, Juvenile Arthritis Family Days, and the annual Bone Bash gala in Delaware (Figure 3). Through Arthritis Foundation events, educational resources, and advocacy tools people living with arthritis learn how to get more involved, have a chance to connect with others, and effectively influence health policy that reduces barriers to care.
Figure 3.

Walk to Cure Arthritis
The Wilmington Delaware Walk to Cure Arthritis offers exercise and social engagement is support of arthritis community advocacy and research.
Recent Advances in Research.
• Tissue engineering offers significant promise for future patients. St. Louis researchers recently reported development of a resurfacing strategy for compromised joints. This strategy may offer patients alternatives to total joint replacement, and use adult stem cell technologies to control future inflammation.53 Future OA clinical trials will require novel biomarkers to monitor disease progression beyond radiographic data. Significant strides were recently reported for sports injury, where sophisticated MRI techniques were used for the first time to demonstrate early evidence of developing OA in high risk individuals.54,55
• In RA, two new drugs baricitinib (Eli Lilly) and sarilumab (Sanofi/Regeneron), are nearing final FDA review. If approved, these new drugs would offer new opportunities to the current panel of DMARDS, particularly for patients with difficult to treat disease.
Key Messages.
• Arthritis in the US is the second leading cause of disability (affecting 21.2% of the population) one of the most common, and most costly, chronic diseases (at a cost of over $796.3 billion or over 5.5% of the entire US GDP IN 2011 dollars).
• Whereas substantially improved medications are now available for rheumatoid and other inflammatory arthritis types, progress in osteoarthritis medications remains behind.
• A combination of self-management, weight loss, physical activity and pharmacologic interventions have been shown to be effective in managing symptoms of arthritis. Surgical treatment is both for mechanical symptom management and for joint death when non- operative treatments have failed.
References
- 1.Entezami, P., Fox, D. A., Clapham, P. J., & Chung, K. C. (2011, February). Historical perspective on the etiology of rheumatoid arthritis. Hand Clinics, 27(1), 1–10. 10.1016/j.hcl.2010.09.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sassoon, J., Noe, L. F., & Benton, M. J. (2012). Cranial anatomy, taxonomic implications and palaeopathology of an upper jurassic pliosaur (Reptilia: Sauropterygia) from Westbury, Wiltshire, UK: upper jurassic pliosaur from wiltshire. Palaeontology, 55(4), 743–773. 10.1111/j.1475-4983.2012.01151.x [DOI] [Google Scholar]
- 3.Briggs, A. M., Cross, M. J., Hoy, D. G., Sànchez-Riera, L., Blyth, F. M., Woolf, A. D., & March, L. (2016, April). Musculoskeletal health conditions represent a global threat to healthy aging: A report for the 2015 World Health Organization world report on ageing and health. The Gerontologist, 56(Suppl 2), S243–S255. 10.1093/geront/gnw002 [DOI] [PubMed] [Google Scholar]
- 4.March, L., Smith, E. U. R., Hoy, D. G., Cross, M. J., Sanchez-Riera, L., Blyth, F., et al. Woolf, A. D. (2014, June). Burden of disability due to musculoskeletal (MSK) disorders. Best Practice & Research. Clinical Rheumatology, 28(3), 353–366. 10.1016/j.berh.2014.08.002 [DOI] [PubMed] [Google Scholar]
- 5.Sacks, J. J., Helmick, C. G., Luo, Y.-H., Ilowite, N. T., & Bowyer, S. (2007, December 15). Prevalence of and annual ambulatory health care visits for pediatric arthritis and other rheumatologic conditions in the United States in 2001-2004. Arthritis and Rheumatism, 57(8), 1439–1445. 10.1002/art.23087 [DOI] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention (CDC) . (2009, May 1). Prevalence and most common causes of disability among adults—United States, 2005. MMWR. Morbidity and Mortality Weekly Report, 58(16), 421–426. [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention (CDC) . (2013, November 8). Prevalence of doctor-diagnosed arthritis and arthritis-attributable activity limitation—United States, 2010-2012. MMWR. Morbidity and Mortality Weekly Report, 62(44), 869–873. [PMC free article] [PubMed] [Google Scholar]
- 8.Hootman, J. M., Helmick, C. G., Barbour, K. E., Theis, K. A., & Boring, M. A. (2016, July). Updated projected prevalence of self-reported doctor-diagnosed arthritis and arthritis-attributable activity limitation among US adults, 2015-2040: Projected prevalence of arthritis in the US, 2015-2040. Arthritis & Rheumatology (Hoboken, N.J.), 68(7), 1582–1587. 10.1002/art.39692 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cisternas, M. G., Murphy, L., Sacks, J. J., Solomon, D. H., Pasta, D. J., & Helmick, C. G. (2016, May). Alternative methods for defining osteoarthritis and the impact on estimating prevalence in a US population-based survey. Arthritis care & research, 68(5), 574–580. 10.1002/acr.22721 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Felson, D. T., Couropmitree, N. N., Chaisson, C. E., Hannan, M. T., Zhang, Y., McAlindon, T. E., et al. Myers, R. H. (1998, June). Evidence for a Mendelian gene in a segregation analysis of generalized radiographic osteoarthritis: The Framingham Study. Arthritis and Rheumatism, 41(6), 1064–1071. [DOI] [PubMed] [Google Scholar]
- 11.Roberts, J., & Burch, T. A. (1966, June). Osteoarthritis prevalence in adults by age, sex, race, and geographic area. Vital and Health Statistics. Series 11, Data from the National Health Survey, (15): 1–27. [PubMed]
- 12.Lawrence, R. C., Felson, D. T., Helmick, C. G., Arnold, L. M., Choi, H., Deyo, R. A., . . .. Wolfe, F., & the National Arthritis Data Workgroup. (2008, January). Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part II. Arthritis and Rheumatism, 58(1), 26–35. [DOI] [PMC free article] [PubMed]
- 13.Srikanth, V. K., Fryer, J. L., Zhai, G., Winzenberg, T. M., Hosmer, D., & Jones, G. (2005, September). A meta-analysis of sex differences prevalence, incidence and severity of osteoarthritis. Osteoarthritis and Cartilage, 13(9), 769–781. 10.1016/j.joca.2005.04.014 [DOI] [PubMed] [Google Scholar]
- 14.Reyes, C., Leyland, K. M., Peat, G., Cooper, C., Arden, N. K., & Prieto-Alhambra, D. (2016, August). Association between overweight and obesity and risk of clinically diagnosed knee, hip, and hand osteoarthritis: A population-based cohort study. Arthritis & Rheumatology (Hoboken, N.J.), 68(8), 1869–1875. 10.1002/art.39707 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fowler-Brown, A., Kim, D. H., Shi, L., Marcantonio, E., Wee, C. C., Shmerling, R. H., & Leveille, S. (2015, January). The mediating effect of leptin on the relationship between body weight and knee osteoarthritis in older adults. Arthritis & Rheumatology (Hoboken, N.J.), 67(1), 169–175. 10.1002/art.38913 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Roos, E. M. (2005, March). Joint injury causes knee osteoarthritis in young adults. Current Opinion in Rheumatology, 17(2), 195–200. 10.1097/01.bor.0000151406.64393.00 [DOI] [PubMed] [Google Scholar]
- 17.Roos, H., Adalberth, T., Dahlberg, L., & Lohmander, L. S. (1995, December). Osteoarthritis of the knee after injury to the anterior cruciate ligament or meniscus: The influence of time and age. Osteoarthritis and Cartilage, 3(4), 261–267. 10.1016/S1063-4584(05)80017-2 [DOI] [PubMed] [Google Scholar]
- 18.Samson, D. J., Grant, M. D., Ratko, T. A., Bonnell, C. J., Ziegler, K. M., & Aronson, N. (2007, September). Treatment of primary and secondary osteoarthritis of the knee. Evidence Report/technology Assessment, (157): 1–157. [PMC free article] [PubMed]
- 19.Agency for Healthcare Research and Quality. (2016). Treatment of osteoarthritis of the knee: An update (research protocol). Retrieved from http://effectivehealthcare.ahrq.gov/index.cfm/search-for- guides-reviews-and-reports/?pageaction=displayproduct&productid=2247
- 20.Helmick, C. G., Felson, D. T., Lawrence, R. C., Gabriel, S., Hirsch, R., Kwoh, C. K., . . .. Stone, J. H., & the National Arthritis Data Workgroup. (2008, January). Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part I. Arthritis and Rheumatism, 58(1), 15–25. [DOI] [PubMed]
- 21.Myasoedova, E., Crowson, C. S., Kremers, H. M., Therneau, T. M., & Gabriel, S. E. (2010, June). Is the incidence of rheumatoid arthritis rising?: Results from Olmsted County, Minnesota, 1955-2007. Arthritis and Rheumatism, 62(6), 1576–1582. 10.1002/art.27425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Neogi, T., & Felson, D. (2013). Osteoarthritis and Rheumatoid Arthritis. In Wall & Melzack’s Textbook of Pain (6th ed., pp. 645-657). Philadelphia, PA. Retrieved from https://www-clinicalkey-com. ezp.welch.jhmi.edu/#!/content/book/3-s2.0-B9780702040597000474?scrollTo=%23hl0000543
- 23.Pincus, T., Callahan, L. F., Sale, W. G., Brooks, A. L., Payne, L. E., & Vaughn, W. K. (1984, August). Severe functional declines, work disability, and increased mortality in seventy-five rheumatoid arthritis patients studied over nine years. Arthritis and Rheumatism, 27(8), 864–872. 10.1002/art.1780270805 [DOI] [PubMed] [Google Scholar]
- 24.Jiang, X., Frisell, T., Askling, J., Karlson, E. W., Klareskog, L., Alfredsson, L., & Källberg, H. (2015, February). To what extent is the familial risk of rheumatoid arthritis explained by established rheumatoid arthritis risk factors? Arthritis & Rheumatology (Hoboken, N.J.), 67(2), 352–362. 10.1002/art.38927 [DOI] [PubMed] [Google Scholar]
- 25.Kvien, T. K., Uhlig, T., Ødegård, S., & Heiberg, M. S. (2006, June). Epidemiological aspects of rheumatoid arthritis: The sex ratio. Annals of the New York Academy of Sciences, 1069, 212–222. 10.1196/annals.1351.019 [DOI] [PubMed] [Google Scholar]
- 26.Källberg, H., Ding, B., Padyukov, L., Bengtsson, C., Rönnelid, J., Klareskog, L., & Alfredsson, L., & the EIRA Study Group . (2011, March). Smoking is a major preventable risk factor for rheumatoid arthritis: Estimations of risks after various exposures to cigarette smoke. Annals of the Rheumatic Diseases, 70(3), 508–511. 10.1136/ard.2009.120899 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Aletaha, D., Neogi, T., Silman, A. J., Funovits, J., Felson, D. T., Bingham, C. O., III, et al. Hawker, G. (2010, September). 2010 rheumatoid arthritis classification criteria: An American College of Rheumatology/European League Against Rheumatism collaborative initiative. Annals of the Rheumatic Diseases, 69(9), 1580–1588. 10.1136/ard.2010.138461 [DOI] [PubMed] [Google Scholar]
- 28.Michaud, K., & Wolfe, F. (2007, October). Comorbidities in rheumatoid arthritis. Best Practice & Research. Clinical Rheumatology, 21(5), 885–906. 10.1016/j.berh.2007.06.002 [DOI] [PubMed] [Google Scholar]
- 29.Dominick, K. L., Ahern, F. M., Gold, C. H., & Heller, D. A. (2004, January 13). Health-related quality of life among older adults with arthritis. Health and Quality of Life Outcomes, 2, 5. 10.1186/1477-7525-2-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.ter Wee, M. M., Lems, W. F., Usan, H., Gulpen, A., & Boonen, A. (2012, February). The effect of biological agents on work participation in rheumatoid arthritis patients: A systematic review. Annals of the Rheumatic Diseases, 71(2), 161–171. 10.1136/ard.2011.154583 [DOI] [PubMed] [Google Scholar]
- 31.Singh, J. A., Saag, K. G., Bridges, S. L., Jr., Akl, E. A., Bannuru, R. R., Sullivan, M. C., . . .. McAlindon, T., & the American College of Rheumatology. (2016, January). 2015 American College of Rheumatology guideline for the treatment of rheumatoid arthritis: ACR RA treatment recommendations. Arthritis care & research, 68(1), 1–25. [DOI] [PubMed]
- 32.Consumer Reports Health. (2013). best buy drugs - using biologics to treat: rheumatoid arthritis. comparing effectiveness, safety, side effects, and price. Retrieved February 20, 2017, from https://www.consumerreports.org/health/resources/pdf/best-buy-rugs/BBD_Rheumatoid_Arthritis.pdf
- 33.Barnabe, C., Sun, Y., Boire, G., Hitchon, C. A., Haraoui, B., Thorne, J. C., . . .. Bykerk, V. P., & the CATCH Investigators. (2015, August 24). Heterogeneous disease trajectories explain variable radiographic, function and quality of life outcomes in the canadian early arthritis cohort (CATCH). PLoS One, 10(8), e0135327. [DOI] [PMC free article] [PubMed]
- 34.Barbour, K. E., Helmick, C. G., Boring, M., Zhang, X., Lu, H., & Holt, J. B. (2016, May 20). Prevalence of doctor-diagnosed arthritis at state and county levels-United States, 2014. MMWR. Morbidity and Mortality Weekly Report, 65(19), 489–494. Retrieved from https://www.cdc. gov/mmwr/volumes/65/wr/mm6519a2.htm 10.15585/mmwr.mm6519a2 [DOI] [PubMed] [Google Scholar]
- 35.Centers for Disease Control and Prevention. (n.d.). State data tables, data and statistics, arthritis Retrieved February 17, 2017, from https://www.cdc.gov/arthritis/data_statistics/state-data-list-current.htm
- 36.Arthritis and Joint Pain. (n.d.). Retrieved February 20, 2017, from http://www.boneandjointburden.org/2014-report/ivh11/arthritis-and-joint-pain
- 37.Centers for Disease Control and Prevention (CDC) . (2007, January 12). National and state medical expenditures and lost earnings attributable to arthritis and other rheumatic conditions—United States, 2003. MMWR. Morbidity and Mortality Weekly Report, 56(1), 4–7. [PubMed] [Google Scholar]
- 38.Torio, C. M., & Moore, B. J. (2016). National inpatient hospital costs: The most expensive conditions by payer, 2013: Statistical Brief #204. In Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Rockville (MD): Agency for Healthcare Research and Quality (US). Retrieved from http://www.ncbi.nlm.nih.gov/books/NBK368492/ [PubMed] [Google Scholar]
- 39.Van Rensbergen, G., & Nawrot, T. (2010, July 14). Medical conditions of nursing home admissions. BMC Geriatrics, 10(1), 46. 10.1186/1471-2318-10-46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Barbour, K. E., Stevens, J. A., Helmick, C. G., Luo, Y.-H., Murphy, L. B., Hootman, J. M., . . .. Sugerman, D. E., & the Centers for Disease Control and Prevention (CDC). (2014, May 2). Falls and fall injuries among adults with arthritis—United States, 2012. MMWR. Morbidity and Mortality Weekly Report, 63(17), 379–383. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/24785984 [PMC free article] [PubMed]
- 41.Hopson, S., Saverno, K., & Liu, L. Z. AL-Sabbagh, A., Orazem, J., Costantino, M. E., & Pasquale, M. K. (2016, February). Impact of out-of-pocket costs on prescription fills among new initiators of biologic therapies for rheumatoid arthritis. Journal of Managed Care & Specialty Pharmacy, 22(2), 122–130. [DOI] [PMC free article] [PubMed]
- 42.Quandt, S. A., Chen, H., Grzywacz, J. G., Bell, R. A., Lang, W., & Arcury, T. A. (2005, October 15). Use of complementary and alternative medicine by persons with arthritis: Results of the National Health Interview Survey. Arthritis and Rheumatism, 53(5), 748–755. 10.1002/art.21443 [DOI] [PubMed] [Google Scholar]
- 43.National Institutes of Health. (n.d.) NIH categorical spending - NIH research portfolio online reporting tools (RePORT). Retrieved February 13, 2017, from https://report.nih.gov/categorical_spending.aspx
- 44.Murphy, L. B., Sacks, J. J., Brady, T. J., Hootman, J. M., & Chapman, D. P. (2012, July). Anxiety and depression among US adults with arthritis: Prevalence and correlates. Arthritis care & research, 64(7), 968–976. 10.1002/acr.21685 [DOI] [PubMed] [Google Scholar]
- 45.Felson, D. T., Zhang, Y., Anthony, J. M., Naimark, A., & Anderson, J. J. (1992, April 1). Weight loss reduces the risk for symptomatic knee osteoarthritis in women. The Framingham Study. Annals of Internal Medicine, 116(7), 535–539. 10.7326/0003-4819-116-7-535 [DOI] [PubMed] [Google Scholar]
- 46.Lohmander, L. S., Ostenberg, A., Englund, M., & Roos, H. (2004, October). High prevalence of knee osteoarthritis, pain, and functional limitations in female soccer players twelve years after anterior cruciate ligament injury. Arthritis and Rheumatism, 50(10), 3145–3152. 10.1002/art.20589 [DOI] [PubMed] [Google Scholar]
- 47.Lubar, D., White, P. H., Callahan, L. F., Chang, R. W., Helmick, C. G., Lappin, D. R., et al. Waterman, M. B. (2010, April). A national public health agenda for osteoarthritis 2010. Seminars in Arthritis and Rheumatism, 39(5), 323–326. 10.1016/j.semarthrit.2010.02.002 [DOI] [PubMed] [Google Scholar]
- 48.Centers for Disease Control and Prevention (CDC). (n.d.). Intervention Programs, Arthritis. Retrieved February 17, 2017, from https://www.cdc.gov/arthritis/interventions/
- 49.Centers for Disease Control and Prevention (CDC). (n.d.). Physical activity programs, intervention programs, arthritis. Retrieved February 16, 2017, from https://www.cdc.gov/arthritis/interventions/physical-activity.html
- 50.Callahan, L. F., Shreffler, J. H., Altpeter, M., Schoster, B., Hootman, J., Houenou, L. O., et al. Schwartz, T. A. (2011, August). Evaluation of group and self-directed formats of the Arthritis Foundation’s Walk With Ease Program. Arthritis care & research, 63(8), 1098–1107. 10.1002/acr.20490 [DOI] [PubMed] [Google Scholar]
- 51.Nyrop, K. A., Charnock, B. L., Martin, K. R., Lias, J., Altpeter, M., & Callahan, L. F. (2011, December). Effect of a six-week walking program on work place activity limitations among adults with arthritis. Arthritis care & research, 63(12), 1773–1776. 10.1002/acr.20604 [DOI] [PubMed] [Google Scholar]
- 52.Wallack, L., Dorfman, L., Jernigan, D., & Themba, M. (1993). Media advocacy and public health: Power for prevention. 1st ed. Sage Publications, Inc.: Atlanta, Ga. [Google Scholar]
- 53.Moutos, F. T., Glass, K. A., Compton, S. A., Ross, A. K., Gersbach, C. A., Guilak, F., & Estes, B. T. (2016, August 2). Anatomically shaped tissue-engineered cartilage with tunable and inducible anticytokine delivery for biological joint resurfacing. Proceedings of the National Academy of Sciences of the United States of America, 113(31), E4513–E4522. 10.1073/pnas.1601639113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Gallo, M. C., Wyatt, C., Pedoia, V., Kumar, D., Lee, S., Nardo, L., et al. Majumdar, S. (2016, August). T1ρ and T2 relaxation times are associated with progression of hip osteoarthritis. Osteoarthritis and Cartilage, 24(8), 1399–1407. 10.1016/j.joca.2016.03.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Russell, C., Pedoia, V., Amano, K., Potter, H., & Majumdar, S. (2016). Baseline cartilage quality is associated with voxel-based T1e and T2 following ACL reconstruction: A multicenter pilot study. ]ournal of Orthopaedic Research: Official Publication of the Orthopaedic Research Society. 10.1002/jor.23277 10.1002/jor.23277 [DOI] [PMC free article] [PubMed]


