ABSTRACT
OBJECTIVE
Describe the expenditure resulting from hospitalizations for clinical treatment of users diagnosed with COVID-19 in the Unified Health System (SUS) between February and December 2020.
METHODS
This is a descriptive study based on data from the Hospital Information System about government expenditure on hospitalizations for clinical treatment of users diagnosed with COVID-19 and causes included in the ICD-10 chapters. We obtained the number of hospitalizations, average length of stay, lethality rate, and total expenditure considering hospital services, professional services and average expenditure per hospitalization.
RESULTS
In the period evaluated, SUS registered 462,149 hospitalizations, 4.9% of them for COVID-19 treatment. Total expenditure exceeded R$ 2.2 billion, with 85% allocated to hospital services and 15% to professional services. Expenditure for treating COVID-19 was distributed differently between the country’s regions. The Southeast region had the highest number of hospitalizations, highest total amount spent, highest average length of stay in days, and highest lethality rate; the South region, in turn, recorded the highest percentage of spending on non-profit hospitals (58%) and corporate hospitals (15%).
CONCLUSIONS
Hospitalizations for clinical treatment of coronavirus infection were more costly compared to those for treatment of acute respiratory failure and pneumonia or influenza. Our results show the disparities in hospitalization expenditure for similar procedures between the regions of Brazil, underlining the vulnerability and the need for strategies to reduce the differences in access, use, and distribution of SUS resources, ensuring equanimity, and considering the unfair inequalities between the country’s regions.
Keywords: Coronavirus Infections, Hospitalization, Hospital Costs, Public Expenditures on Health, Unified Health System
INTRODUCTION
SARS-CoV-2 infection has emerged as a major challenge for health systems. Since its outbreak in Wuhan, China in December 2019, the disease caused by the new coronavirus has totaled more than 161,513,458 confirmed cases and 3,352,109 deaths worldwide as of May 15, 20211 . Clinically, the infection can manifest in three distinct ways, which vary according to age group and associated clinical conditions: asymptomatic carrier, individual with acute respiratory disease (ARD) or patients with pneumonia at different degrees of severity2 .
COVID-19 is an acute respiratory infections (ARI), a group of clinical syndromes whose most common infectious agents are respiratory viruses, such as syncytial, or bacteria such as Streptococcus pneumoniae and Haemophilus influenzae 3 . The severity of the disease will depend on the infectious agent, the environment and host factors. Thus, according to the World Health Organization (WHO), ARI are among the infectious diseases with the highest morbidity and mortality rates worldwide4 . Data show that these infections are responsible for more than 4 million deaths per year, representing a major cause of death in developing countries5 .
In Brazil, in periods prior to the pandemic, such infections accounted for nearly one fifth of hospitalizations in the Unified Health System (SUS)6 . COVID-19 alone, as of May 15, 2021, recorded more than 432,000 deaths and 15,519,525 infected, but its impacts on the health sector and the national economy began to be noticed already in 20207 , 8 . Importantly, Brazil is among the few countries in the Americas to have a universal and free healthcare system, on which about 75% of the population depends exclusively, and which is recognized as one of the country’s most important public policies9 .
SUS is cited as an example of a successful healthcare system in Latin America, mainly for guaranteeing health as a right of all Brazilian citizens9 . On the other hand, the underfunding challenges have put the guarantee of this right at risk10 . In the context of the pandemic, the role played by SUS is significant, especially in hospital care. COVID-19 has resulted in additionally high hospitalization rates11 , and besides drawing attention to the added pressure on the health system, it is worth observing and analyzing SUS expenditure and how it is distributed throughout the territory.
In the scenario of the COVID-19 pandemic, developing analyses to estimate the direct medical-hospital costs required – including examinations, procedures, drugs, human resources, appointments, hospitalizations, rehabilitation and12 –, becomes indispensable to support decision-making, in terms of meeting the demands on services and development of operational strategies by national health systems13 .
Searches conducted on the Virtual Health Library (VHL), Scientific Electronic Library Online (SciELO) and PubMed, using the Descriptors in Health Sciences (DEcS/Mesh) in English and Portuguese, “hospital costs,” “health expenditures,” “public expenditures on health,” “public expenditures” and “public expenditures on private services” associated with the terms “COVID-19” and “Brazil,” using the Boolean operator AND, returned no prior study, of national scope, describing SUS expenditure on hospitalizations for clinical treatment of confirmed COVID-19 cases. Research on these expenditures, therefore, is minor in the literature, although addressing such a topic is extremely relevant to understand its toll on the public health system.
This study, thus, seeks to analyze the percentage of public expenditures on SUS hospitalizations for clinical treatment of COVID-19 patients in Brazil, between February and December 2020. To this end, we described and analyzed public expenditures on hospitalizations and how they are distributed according to the population characteristics. Our findings may contribute to adopting measures capable of avoiding complications and, consequently, the collapse of the healthcare system in a pandemic scenario.
METHODS
This is a descriptive study based on secondary data about government expenditures on hospitalizations for clinical treatment of users diagnosed with COVID-19 in Brazil, from February to December 2020.
Data on hospitalizations and their respective costs were collected from the Unified Health System’s Hospital Information System (SIH-SUS), available at the SUS Department of Information Technology (Datasus)14 website, through consolidated information on inpatient hospital authorizations (IHA), classified by country region.
The selected hospitalizations had as their main procedure code 03.03.01.022-3 (treatment of coronavirus infection) – which corresponds to the actions necessary to clinically treat hospitalized users diagnosed with coronavirus infection, in accordance with Ordinance No. 245, of March 24, 2020, and the Technical Guidelines for SIH-SUS operationalization during the coronavirus state of public health emergency, updated by the Ministry of Health on August 13, 202015 –, in hospital units linked to SUS (public and private associated).
We also sought to compare the expenditures on hospitalizations for treatment of patients diagnosed with COVID-19, expenditures on hospitalizations for all causes considering the ICD-10 chapters, and expenditures on treatment of major respiratory system infections, such as pneumonia, influenza and acute upper and lower tract infections. For the latter, we selected procedures with code: 03.03.14.015-1 – treatment of pneumonia or influenza (flu), 03.03.14.010-0 – treatment of acute upper tract infections, and 03.03.14.014-3 – treatment of other acute lower tract infections16 .
Our study excluded data on treatments without scientific evidence for coronavirus infection. Hospitalization for treatment comprises actions and procedures necessary to stabilize and prevent the worsening of the user’s clinical picture. Such interventions, however, can vary substantially depending on the clinical picture of each user (considering associated comorbidities and degree of lung involvement), between the clinical protocols adopted by each state and municipality, and between the clinical practices chosen.
The chosen time frame comprises the months of February to December 2020 for hospitalizations for clinical treatment of users diagnosed with coronavirus. Such time frame is justified because the first case of SARS-CoV-2 infection in Brazil was confirmed on February 26, 2020; while December was the last month with data available in the SIH-SUS.
The variables of interest taken from the SIH-SUS comprised: number of hospitalizations, total cost of hospitalizations, cost of professional services, cost of hospital services, average cost of SUS hospitalization (by specialty or procedure, in a given geographical space, in the year considered), average length of stay (average total number of days for the IHA approved in the period) and lethality rate (ratio between the number of deaths and the number of approved IHA in the period, computed as hospitalizations, multiplied by 100)17 . All expenditures were calculated in reais, and the average length of stay was counted in days.
We also sought to identify the total amount paid by legal sphere, that is, the distribution of total government expenditures according to legal sphere, considering the categories of the National Registry of Health Establishments18 : “public hospitals,” “corporate hospitals,” and “non-profit hospitals.” The first group consists of those whose legal sphere is “federal public administration,” “state or Federal District,” “municipal” and “public administration – others.” Corporate are those whose legal sphere is “public company or mixed-capital company” and “other business entities.” Non-profit hospitals, in turn, are those registered in the legal sphere “non-profit entities”18 .
The number, proportion, ratio and amounts paid by hospitalizations, obtained from the SIH-SUS, were tabulated using the Microsoft Excel program and calculated by descriptive statistical analysis.
The analysis was performed on secondary data, of open access, without the possibility of individual identification of the information. Thus, according to the recommendations of the National Health Council (CNS) Resolution No. 466 of December 12, 2012, the ethical principles of research involving human beings were respected, and the research ethics committee approval waived.
RESULTS
Between February and December 2020, the SIH-SUS registered 462,149 hospitalizations, having as their main procedure the treatment of users with coronavirus, corresponding to a total expenditure of R$ 2,248,011,968.40. Importantly, SUS spent 85% of this amount on hospital services and 15% on professional services. Among all regions of the country, the Southeast accounted for the largest share of expenditures, representing about 45% of the total. The South and North regions presented, respectively, the highest and lowest average cost per hospitalization ( Table 1 ).
Table 1. Expenditures (in reais) of hospitalizations for clinical treatment of coronavirus infectiona according to region, Brazil, February – December 2020.
| Region | Total amount of expenditureb (R$) | Cost of hospital servicesc (R$) | Cost of professional servicesd (R$) | Average cost per hospital hospitalizatione (R$) |
|---|---|---|---|---|
| North | 133,723,986.43 | 111,708,340.36 | 22,015,646.07 | 3,157.96 |
| Northeast | 550,997,791.12 | 465,375,038.13 | 85,622,752.99 | 4,489.91 |
| Southeast | 1,010,529,436.45 | 857,747,748.55 | 152,776,809.87 | 5,154.34 |
| South | 381,184,490.20 | 324,887,362.21 | 56,297,127.99 | 6,165.64 |
| Midwest | 171,576,264.24 | 145,114,948.61 | 26,460,690.51 | 4,376.16 |
|
| ||||
| Total | 2,248,011,968.44 | 1,904,833,437.86 | 343,173,027.43 | 4,864.26 |
Source: Own elaboration, based on data from SIH-SUS.
a Hospitalizations of patients with COVID-19 registered with procedure code 03.03.01.022-3, compliant with Ordinance No. 245 of March 24, 2020 and Technical Guidelines for SIH-SUS operationalization during the coronavirus state of public health emergency published on August 13, 2020 by the Ministry of Health.
b Amount for IHA approved in the period. This amount does not necessarily correspond to the sum allocated to the establishment – depending on the situation of the units, they receive budgetary resources or there may be withholdings and incentive payments, not presented here. This amount should, therefore, be considered as the approved production sum.
c Cost of hospital services for IHA approved in the period.
d Cost of professional services for IHA approved in the period.
e Average cost per hospitalization in the Unified Health System (SUS), by specialty, in a given geographical space, in the period considered.
When considering all hospitalizations taken place in Brazil under SUS, in the analyzed period, 4.9% had as main procedure the treatment of COVID-19, corresponding to 15% of the expenditures with all hospitalizations in the country. By comparing the average length of stay (in days) between all hospitalizations and hospitalizations for coronavirus treatment, we found that the latter lasted longer ( Table 2 ).
Table 2. Expenditures (in reais) and average length of stay (in days) of hospitalizations for ICD-10 chapters versus hospitalizations for clinical treatment of coronavirus infection according to region, Brazil, February – December 2020.
| Region | Hospitalizations for ICD-10 chaptersa | Hospitalizations for treatment of coronavirus infectionb | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||||
| Hospitalizations | Total amount of expenditurec (R$) | Average cost per hospital hospitalizationd | Average length of stay (in days)f | Hospitalizations | %e total hospitalizations | Total amount of expenditurec (R$) | %e total amount of expenditure on hospitalizations | Average cost per hospital hospitalizationd | Average length of stay (in days)f | |
| North | 758,143 | 819,819,970.59 | 1,081.35 | 4.7 | 42,345 | 5.6 | 133,723,986.4 | 16.3 | 3,157.96 | 7.4 |
| Northeast | 2,461,730 | 3,462,075,135.95 | 1,406.36 | 5.3 | 122,719 | 5.0 | 550,997,791.1 | 15.9 | 4,489.91 | 7.8 |
| Southeast | 3,772,966 | 6,511,672,543.21 | 1,725.88 | 5.9 | 196,054 | 5.3 | 1,010,529,436 | 15.5 | 5,154.34 | 8.6 |
| South | 1,646,796 | 3,055,201,666.37 | 1,855.24 | 5.2 | 61,824 | 3.7 | 381,184,490.2 | 12.5 | 6,165.64 | 8.5 |
| Midwest | 746,075 | 1,064,013,109.82 | 1,426.15 | 5.1 | 39,207 | 5.2 | 171,576,264.2 | 16.1 | 4,376.16 | 7.4 |
|
| ||||||||||
| Total | 9,385,710 | 14,912,782,425.94 | 1,588.88 | 5.4 | 462,149 | 4.9 | 2,248,011,968.44 | 15 | 4,864.26 | 8.2 |
Source: Own elaboration, based on data from SIH-SUS.
a All hospitalizations taken place under SUS, considering all ICD-10 chapters.
b All hospitalizations taken place under SUS with procedure code 245, compliant with Ordinance No. 24 of March 2020, 13 and Technical Guidelines for SIH-SUS operationalization during the coronavirus state of public health emergency published on August 2020, 2020 by the Ministry of Health.
c Amount for the IHAs approved in the period. This amount does not necessarily correspond to the sum allocated to the establishment – depending on the situation of the units, they receive budgetary resources or there may be withholdings and incentive payments, not presented here. This amount should, therefore, be considered as the approved production sum.
d Average cost per hospitalization in the Unified Health System (SUS), by specialty, in a given geographical space, in the period considered.
e Percentages calculated based on the cost of hospitalizations and total expenditures by region for all ICD-10 chapters.
f Average length of stay for approved IHA, computed as hospitalizations, in the period.
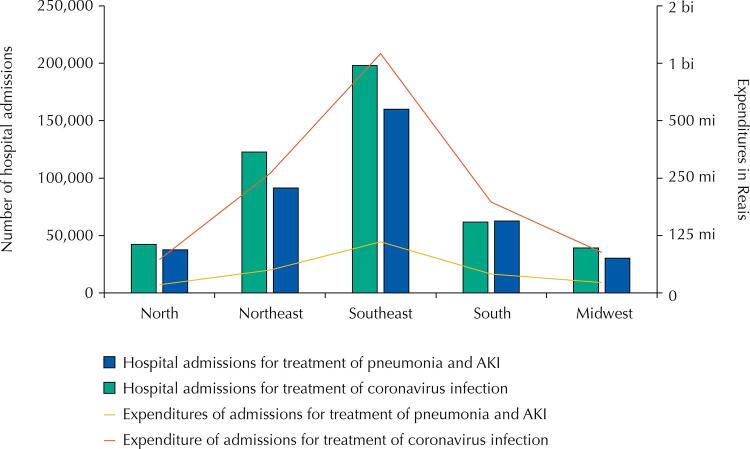
When comparing expenditures and the hospitalizations whose main procedure was treatment of acute upper and lower tract infections, pneumonia or influenza, with hospitalizations for coronavirus treatment, the higher expenses and number of hospitalizations found also refer to coronavirus infection ( Figure 1 ).
Figure 1. Hospitalizations and expenditures for treatment of coronavirus infectiona and for treatment of acute upper and lower tract infections, pneumonia or influenzab by region, Brazil, February – December 2020.
a Procedure with code 03.03.01.022-3 (treatment of coronavirus infection) – which corresponds to the actions necessary to clinically treat hospitalized patients diagnosed with COVID-19.
b Procedures with codes 03.03.14.015-1 – treatment of pneumonia or influenza (flu), 03.03.14.010-0 – treatment of acute upper tract infections, and 03.03.14.014-3 – treatment of other acute lower tract infections.
ARI: acute respiratory infections.
Regarding the expenditures associated with the average length of stay and lethality rate, comparing hospitalizations for COVID-19 treatment with hospitalizations for treatment of pneumonia or influenza, the Southeast region showed the highest number of hospitalizations, highest total amount spent, highest average length of stay in days, and higher lethality rate. The states of São Paulo and Minas Gerais had the highest expenditures for treatment of these conditions. The state of Roraima presented the longest length of stay for treatment, both of coronavirus infection and of pneumonia or influenza. The states of Paraíba and Rio de Janeiro had the highest lethality rates for coronavirus treatment and treatment of influenza or influenza, respectively ( Table 3 ).
Table 3. Expenditures (in reais), average length of stay (in days), and lethality rate (per 100 inpatients) of hospitalizations for clinical treatment of coronavirus infection versus hospitalizations for treatment of pneumonia or influenza (flu) according to region, Brazil, February – December 2020.
| Regions | Hospitalizations for treatment of coronavirus infectiona | Hospitalizations for treatment of pneumonia or influenza (flu)b | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||||||||
| Hospitalizations | Total amount of expenditurec | Average cost per hospital hospitalization (in reais)d | Average length of stay (in days)e | Lethality ratef | Hospitalizations | Total amount of expenditurec | Average cost per hospital hospitalization (in reais)d | Average length of stay (in reais)e | Lethality ratef | |||||
|
|
|
|
|
|||||||||||
| (n) | (%) | (R$) | (%) | (n) | (%) | (R$) | (%) | |||||||
| North | 42,345 | 9 | 133,723,986,4 | 6 | 3,157.96 | 7.4 | 20.64 | 34,192 | 10 | 34,865,889.09 | 8 | 1,019.71 | 6.0 | 7.79 |
| Rondônia | 4,550 | 1 | 18,287,032.7 | 1 | 4,019.13 | 6.2 | 15.52 | 2,969 | 1 | 4,256,679.93 | 1 | 1,433.71 | 6.4 | 9.16 |
| Acre | 1,566 | 0 | 5,902,502.86 | 0 | 3,769.16 | 9.2 | 22.03 | 1,059 | 0 | 1,426,106 | 0 | 1,346.65 | 8.0 | 16.9 |
| Amazonas | 12,276 | 3 | 38,513,890.99 | 2 | 3,137.33 | 8.0 | 23.37 | 5,568 | 2 | 5,489,313.14 | 1 | 985.87 | 6.2 | 10.63 |
| Roraima | 1,699 | 0 | 6,162,828.14 | 0 | 3,627.33 | 9.7 | 25.13 | 1,686 | 0 | 2,066,920.29 | 0 | 1,225.93 | 9.4 | 10.74 |
| Pará | 18,509 | 4 | 54,212,642.19 | 2 | 2,928.99 | 7.2 | 19.12 | 19,326 | 6 | 18,065,351.26 | 4 | 934.77 | 5.3 | 6.12 |
| Amapá | 2,418 | 1 | 4,898,168.88 | 0 | 2,025.71 | 7.2 | 24.69 | 1,562 | 0 | 1,313,542.34 | 0 | 840.94 | 7.5 | 5.76 |
| Tocantins | 1,327 | 0 | 5,746,920.67 | 0 | 4,330.76 | 5.7 | 19.29 | 2,022 | 1 | 2,247,976.13 | 0 | 1,111.76 | 6.8 | 8.31 |
| Northeast | 122,719 | 27 | 550,997791.1 | 25 | 4,489.91 | 7.8 | 21.84 | 83,455 | 24 | 93,769,264.42 | 21 | 1,123.59 | 6.2 | 11.16 |
| Maranhão | 18,685 | 4 | 55,102,185.73 | 2 | 2,949.01 | 6.9 | 19.19 | 14,013 | 4 | 13,795,977.17 | 3 | 984,51 | 5.2 | 6.93 |
| Piauí | 9,868 | 2 | 46,716,983.14 | 2 | 4,734.19 | 7.4 | 17.73 | 9,005 | 3 | 7,060,563.32 | 2 | 784,07 | 4.9 | 6.36 |
| Ceará | 23,122 | 5 | 95,454,894.14 | 4 | 4,128.31 | 7.7 | 22.04 | 16,054 | 5 | 17,545,693.07 | 4 | 1,092.92 | 7.0 | 13.98 |
| Rio G. do Norte | 6,464 | 1 | 32,079,037.42 | 1 | 4,962.72 | 7.2 | 24.09 | 3,774 | 1 | 4,317,075.87 | 1 | 1,143.9 | 7.2 | 12.75 |
| Paraíba | 6,136 | 1 | 29,309,295.2 | 1 | 4,776.61 | 8.4 | 31.83 | 5,757 | 2 | 6,396,642.12 | 1 | 1,111.11 | 6.7 | 14.33 |
| Pernambuco | 29,866 | 6 | 133,019,014.1 | 6 | 4,453.86 | 8.1 | 22.34 | 9,632 | 3 | 1,607,5631.99 | 4 | 1,668.98 | 7.6 | 12.52 |
| Alagoas | 5,338 | 1 | 239,012,90.05 | 1 | 4,477.57 | 8.6 | 25.42 | 4,548 | 1 | 6,343,639.79 | 1 | 1,394.82 | 6.3 | 10.64 |
| Sergipe | 4,080 | 1 | 19,007,855.07 | 1 | 4,658.79 | 9.2 | 22.97 | 2,194 | 1 | 2,708,212.73 | 1 | 1,234.37 | 8.1 | 19.74 |
| Bahia | 19,160 | 4 | 116,407,236.3 | 5 | 6,075.53 | 8.2 | 20.34 | 18,478 | 5 | 19,525,828.36 | 4 | 1,056.71 | 5.7 | 11.35 |
| Southeast | 196,054 | 42 | 1,010,529,436 | 45 | 5,154.34 | 8.6 | 22.61 | 145,005 | 42 | 206,452,552.1 | 45 | 1,423.76 | 7.2 | 16.57 |
| Minas Gerais | 34,553 | 7 | 196,447,903.6 | 9 | 5,685.41 | 8.2 | 19.58 | 41,118 | 12 | 596,589,07.46 | 13 | 1,450.92 | 6.8 | 13.05 |
| Espírito Santo | 10,839 | 2 | 68,060,298.71 | 3 | 6,279.2 | 8.7 | 21.82 | 6,671 | 2 | 9,073,085.62 | 2 | 1,360.08 | 6.6 | 10.9 |
| Rio de Janeiro | 38,865 | 8 | 139,621,866.1 | 6 | 3,592.48 | 8.3 | 27.9 | 22,279 | 6 | 30,502,415.18 | 7 | 1,369.11 | 8.2 | 22.77 |
| São Paulo | 111,797 | 24 | 606,399,368 | 27 | 5,424.11 | 8.8 | 21.78 | 74,937 | 22 | 10,721,8143.8 | 23 | 1,430.78 | 7.1 | 17.16 |
| South | 61,824 | 13 | 381,184,490.2 | 17 | 6,165.64 | 8.5 | 19.25 | 58,222 | 17 | 77,888,586.08 | 17 | 1,337.79 | 6.0 | 13.74 |
| Paraná | 22,702 | 5 | 131,733,713.6 | 6 | 5,802.74 | 7.9 | 19.27 | 22,580 | 6 | 30,765,544.92 | 7 | 1,362.51 | 5.2 | 10.7 |
| Santa Catarina | 14,270 | 3 | 95,031,703,47 | 4 | 6,659.54 | 8.2 | 18 | 14,135 | 4 | 19,970,729.02 | 4 | 1,412.86 | 5.6 | 13.56 |
| Rio G. do Sul | 24,852 | 5 | 154,419,073,2 | 7 | 6,213.55 | 9.1 | 19.95 | 21,507 | 6 | 27,152,312.14 | 6 | 1,262.49 | 7.2 | 17.04 |
| Midwest | 39,207 | 8 | 171,576,264.2 | 8 | 4,376.16 | 7.4 | 18.37 | 27,445 | 8 | 43,362,970.17 | 10 | 1,580.00 | 6.5 | 11.96 |
| Mato G. do Sul | 4,408 | 1 | 21,722,376.9 | 1 | 4,927.94 | 8.1 | 19.44 | 6,897 | 2 | 9,825,686.84 | 2 | 1,424.63 | 6.4 | 14.21 |
| Mato Grosso | 9,328 | 2 | 41,813,431.57 | 2 | 4,482.57 | 7.1 | 19.83 | 5,813 | 2 | 8,298,784.8 | 2 | 1,427.63 | 6.0 | 10.87 |
| Goiás | 16,100 | 3 | 70,691,166.46 | 3 | 4,390.76 | 6.5 | 18.8 | 10,795 | 3 | 18,489,557.09 | 4 | 1,712.79 | 6.1 | 12.24 |
| Distrito Federal | 9,371 | 2 | 37,349,289.31 | 2 | 3,985.62 | 8.9 | 15.68 | 3,940 | 1 | 6,748,941.44 | 1 | 1,712.93 | 8.4 | 8.88 |
|
| ||||||||||||||
| Total | 462,149 | 100 | 2,248,011,968.44 | 100 | 4,864.26 | 8.2 | 21.42 | 348,319 | 100 | 456,339,261.8 | 100 | 1,310.12 | 6.6 | 13.57 |
Source: Own elaboration, based on data from SIH-SUS.
a Hospitalizations of patients with COVID-19 registered with procedure code 03.03.01.022-3, compliant with Ordinance No. 245 of March 24, 2020 and Technical Guidelines for SIH-SUS operationalization during the coronavirus state of public health emergency published on August 13, 2020 by the Ministry of Health.
b Hospitalizations of patients registered on the Inpatient Hospital Authorization (IHA) with procedure code 03.03.14.015-1.
c Amount for the IHAs approved in the period. This amount does not necessarily correspond to the sum allocated to the establishment – depending on the situation of the units, they receive budgetary resources or there may be withholdings and incentive payments, not presented here. This amount should, therefore, be considered as the approved production sum.
d Average cost per hospitalization in the Unified Health System (SUS), by specialty, in a given geographical space, in the period considered.
e Average length of stay for approved IHA, computed as hospitalizations, in the period.
f Ratio between the number of deaths and the number of approved IHA, computed as hospitalizations, in the period, multiplied by 100.
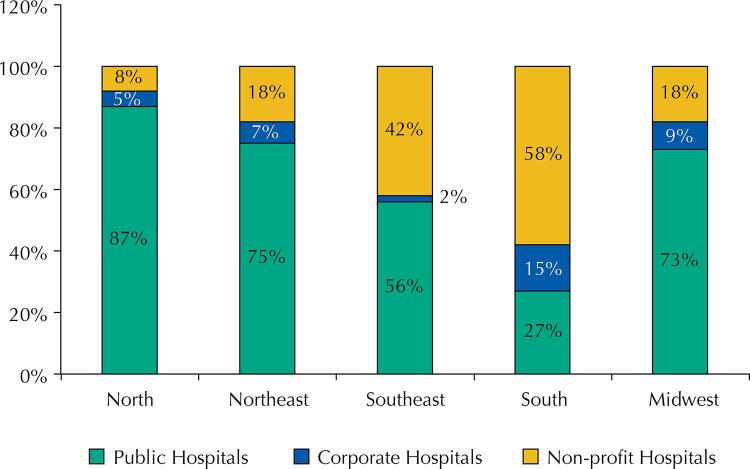
As for the percentage of distribution of total hospitalization expenditure for COVID-19 treatment between the legal spheres of SUS hospitals, we found a higher percentage of expenditures with non-profit hospitals (58%) and corporate hospitals (15%) in the South region ( Figure 2 ).
Figure 2. Distribution of expenditures on hospitalizations for clinical treatment of coronavirus infection between the legal spheres of SUS hospitals by region, Brazil, February – December 2020.
Source: Own elaboration, based on data from SIH-SUS.
DISCUSSION
Our findings showed that the public expenditures of hospitalizations for COVID-19 treatment were distributed differently between the country’s regions.
Considering the volume of hospitalizations for clinical treatment of coronavirus-infected users in the period analyzed, it is evident the impact that such hospitalizations generate on the health system. Although the hospitalizations born by SUS do not account for all hospitalized cases, the progressive evolution of the patient’s clinical picture confers great care coverage to SIH-SUS for these hospitalizations.
Previous studies have also reported on the geographical variations of the average amount paid per hospitalization in Brazil, verified by the significant differences in regional expenditure, regardless of the COVID-19 pandemic20 . The average cost of hospitalization is higher for this treatment when compared to all causes of hospitalization and, more specifically, when compared to cases of treatment for pneumonia or influenza. Such fact indicates that hospitalizations for clinical treatment of COVID-19 are more expensive than those for other causes. Importantly, the variations between the average cost of hospitalization and the average length of stay result from socioeconomic, epidemiological and demographic factors, which determine the profile of hospital demand by SUS, as well as public healthcare policies21 .
This scenario is compounded by fiscal austerity measures and the strong restriction of revenues by the federal level – the main source of resources for service provision in the SUS. Although the transfer of specific federal financial resources so that states and municipalities can fund public actions and services related to combating COVID-19 was regulated, recent regulatory changes in financing, with no discretion in the allocation of resources by state and municipal entities, have intensified regional inequality in the supply of actions and services by the SUS, including outpatient and hospital services. With the approval, in 2016, of Constitutional Amendment No. 95, which established a spending ceiling for the Federal Government, SUS lost almost 22.5 billion reais between 2018 and 202022 . In this respect, the pandemic imposed new challenges to the system, due to the community transmissibility characteristics of the disease23 and, according to the data presented here, the higher cost of hospitalizations.
Research shows that most COVID-19 patients evolve with few symptoms or even asymptomatic. According to the WHO24 , however, 14% of the identified cases develop severe disease, requiring hospitalization and oxygen therapy, 5% require hospitalization in Intensive Care Units (ICU), and most ICU patients require ventilatory support24 .
For data analysis and decision making, one must consider the heterogeneous distribution, between the country’s regions, of the population’s age structure and mobility, the percentage of people in vulnerable situations, and the prevalence of comorbidities, as these factors can determine more severe conditions of SARS-CoV-2 infection. Added to this scenario are the effects of the coping measures enacted by each state, which are directly related to the incidence of cases25 .
The inequalities in public expenditure for clinical treatment of COVID-19 observed in this study refer to the different scenarios, from the care and epidemiological standpoints, faced by the Brazilian regions and that constitute historical differences in the capacity and coverage of the health system. In this study, the Southeast region had the highest number of hospitalizations and highest total expenditure of hospitalizations for treatment of coronavirus infection. Possible explanations are associated with the higher numbers of infected people concentrated in this region and the greater availability of beds11 . Nevertheless, in a country marked by inequalities, including in the provision of health services, Noronha et al.11 highlight the presence of care gaps, which can lead local systems to collapse.
The analysis of lethality among COVID-19 inpatients for clinical treatment shows that four of the five states in the Southeast, four of the seven states in the North, and six of the nine states in the Northeast exceeded the average lethality for the country, while the remaining states showed lethality below the national average. The states that registered the higher lethality rate (Paraíba, Alagoas and Roraima) and higher average length of stay (Roraima, Sergipe and Acre) are in the North and Northeast regions. Such data can reveal, to some extent, economic, social and welfare inequalities that, to be solved, require policies that account for regional singularities25 .
The availability of resources in certain regions, for example, of dialysis machines and non-invasive and invasive ventilation equipment, may be related to the increased cost of hospitalizations in the others. A detailed mapping of the number of ICU beds and of ventilators and respirators showed that Brazil has a ratio of 15.6 ICU beds per 100,000 inhabitants, with a 7.1 average in the SUS and enormous regional heterogeneity, besides the scarcity of resources in most locations20 . These findings corroborate analyses26 , 27 conducted by Brazilian researchers regarding the relationship between higher levels of vulnerability to the pandemic and a combination of ICU bed infrastructure below the minimum, mortality from COVID-19-like conditions above the national median20 , and increased effects of the disease in poorer regions, such as the North and Northeast28 .
In the Brazilian health system, the relationship between public and private becomes even more complex when analyzing the State’s participation in financing supplementary healthcare, regarding the percentage borne by SUS to non-profit and corporate hospitals in the Southern region. It becomes thus urgent to expand the availability of beds by SUS with equitable availability, so that certain areas are prioritized by government investment before the emergency situation established by the COVID-19 pandemic29 .
Among the findings presented here, two are most significant. First, the significant impact that COVID-19, in terms of public health expenditures, represents for the burden of hospitalizations for acute respiratory diseases in the country, given the increase in total expenditure on hospitalizations in the analyzed period. Second, and perhaps more important, are the disparities in inpatient expenditure for similar procedures between regions of the country. That said, it is important to analyze the gaps in the process of standardizing clinical and care practices and to elucidate the difficulties and differences found in each location that justify such disparities. Moreover, we must understand which strategies, in the medium and long term, can be implemented to reduce the differences in access, use, and distribution of resources, aiming to lessen the financial impact on the public health system’s accounts.
Some limitations of this study must be emphasized. First, the fact that the data from the last six months available from SIH-SUS are subject to update; but this is the only public domain hospital information system in the country19 . The second concerns the evaluation of the system’s coverage, which covers only hospitalizations carried out in the public network and that associated with SUS, excluding hospitalizations conducted privately and by health plans19 . Nevertheless, we consider it an important system for analyzing the morbidity profile, since 80% of hospitalizations in Brazil are covered by SIH-SUS, varying according to the level of complexity and procedure required19 . Its third important limitation encompasses the absence of an approach on the profile of hospitalized users, considering gender, race/color, age, associated comorbidities, among other aspects that could help evaluating the SUS hospital network during the pandemic. The non-performance of these analyses is due to the unavailability of such variables by SIH-SUS, when working with consolidated IHA data.
The available data do not allow a more detailed approach on the characteristics of users hospitalized for coronavirus treatment. Moreover, the statistics related to hospital morbidity present selective restrictions, providing information only on users whose clinical picture required hospitalization, and partial restrictions, such as users who would need hospitalization but, for some reason, were not admitted19 , 30 .
CONCLUSIONS
The data presented here refer to a specific time frame, which allows us to evaluate the onset of the pandemic in Brazil. Our findings show that the public expenditure represented by hospitalizations for coronavirus treatment, between February and December 2020, cost more than R$ 2.2 billion. Moreover, the results presented here allow us to infer that hospitalizations for this purpose were more costly when compared with those for treating ARI and pneumonia or influenza.
To our knowledge, this is the first study to estimate the cost of SUS hospitalizations for COVID-19 treatment, and may add necessary reflections before the impending collapse of the health care system in most of the country. New cost analysis studies that consider other approaches are needed to monitor the long-term economic impact of the pandemic on the national health system, in addition to the organization and provision of responses that consider local, social, and demographic characteristics. Given this scenario and the role played by SUS in ensuring the lives of thousands of Brazilians during the pandemic, health cannot be seen as an expense, but rather as an investment in defense of the lives of the Brazilian people.
REFERENCES
- 1.1. Organização Pan-Americana da Saúde. Folha informativa COVID-19-. Brasília, DF: OPAS-Brasil; 2021 [cited 2021 Feb 12]. Available from: https://www.paho.org/pt/covid19
- 2.2. Xavier AR, Silva JS, Almeida JPCL, Conceição JFF, Lacerda GS, Kanaan S. COVID-19: manifestações clínicas e laboratoriais na infecção pelo novo coronavírus. J Bras Patol Med Lab. 2020;56(1):1-9. 10.5935/1676-2444.20200049 [DOI]
- 3.3. Cardoso AM. A persistência das infecções respiratórias agudas como problema de Saúde Pública. Cad Saude Publica. 2010;26(7):1270-1. 10.1590/S0102-311X2010000700001 [DOI]
- 4.4. World Health Organization. Pandemic and epidemic diseases. Infection prevention and control of epidemic and pandemic-prone acute respiratory infections: WHO guidelines. Geneva (CH): WHO; 2014 [cited 2021 Feb 13]. Available from: http://apps.who.int/iris/bitstream/10665/112656/1/9789241507134_eng.pdf?ua=1 [PubMed]
- 5.5. Fórum das Sociedades Respiratórias Internacionais. Doenças respiratórias no mundo: realidades de hoje – oportunidades para o amanhã. Sheffield (UK): European Respiratory Society Publications Office; 2013 [cited 2021 Feb 22]. Available from: https://www.thoracic.org/about/global-public-health/firs/resources/FIRS-in-Portuguese.pdf
- 6.6. Godoy DV, Dal Zotto C, Bellicanta J, Weschenfelder F, Nacif SB. Doenças respiratórias como causa de internações hospitalares de pacientes do Sistema Único de Saúde num serviço terciário de clínica médica na região nordeste do Rio Grande do Sul. J Pneumol. 2001;27(4):193-8. 10.1590/S0102-35862001000400005 [DOI]
- 7.7. Ministério da Saúde (BR). COVID-19: Painel Coronavirus Brasil. Brasília, DF; 2021 [cited 2021 May 5]. Available from: https://covid.saude.gov.br/
- 8.8. Marinelli NP, Albuquerque LPA, Sousa IDB, Batista FMA, Mascarenhas MDM, Rodrigues MTP. Evolução de indicadores e capacidade de atendimento no início da epidemia de COVID-19 no Nordeste do Brasil, 2020. Epidemiol Serv Saude. 2020;29(3):e2020226. 10.5123/s1679-49742020000300008 [DOI] [PubMed]
- 9.9. Andrade RO. Covid-19 is causing the collapse of Brazil’s national health service. BMJ. 2020;370:m3032. 10.1136/bmj.m3032 [DOI] [PubMed]
- 10.10. Souza DO. O subfinanciamento do Sistema Único de Saúde e seus rebatimentos no enfrentamento da Covid-19. Physis Rev Saude Coletiva. 2020;30(3):1-6. 10.1590/S0103-73312020300313 [DOI]
- 11.11. Noronha KVMS, Guedes GR, Turra CM, Andrade MV, Botega L, Nogueira D, et al. Pandemia por COVID-19 no Brasil: análise da demanda e da oferta de leitos hospitalares e equipamentos de ventilação assistida segundo diferentes cenários. Cad Saude Publica. 2020;36(6):e00115320. 10.1590/0102-311x00115320 [DOI] [PubMed]
- 12.12. Rocha R, Rache B, Nunes L, Massuda A. Estimação de custos de hospitalizações em UTI por COVID-19 no SUS: limite inferior por cenários populacionais de infecção. São Paulo, SP: Instituto de Estudos para Políticas de Saúde; 2020 [cited 2021 Feb 20]. (Nota Técnica; nº 2). Available from: https://ieps.org.br/wp-content/uploads/2020/03/NT2_Corona.pdf
- 13.13. Arredondo R. Why revisit your cost-accounting strategy. Healthc Financ Manage. 2014;68(7):68-73. [PubMed]
- 14.14. Ministério da Saúde (BR), Departamento de Informática do Sistema Único de Saúde. Sistema de Informação Hospitalar Descentralizado - SIHD. Brasília, DF: DATASUS; c2016 [cited 2021 Feb 12]. Available from: http://sihd.datasus.gov.br/principal/index.php
- 15.15. Ministério da Saúde (BR), Secretaria de Atenção Especializada à Saúde. Portaria Nº 245 de 24 de março de 2020. Inclui procedimento na Tabela de Procedimentos, Medicamentos, Órteses, Próteses e Materiais Especiais do SUS, para atendimento exclusivo de pacientes com diagnóstico clínico de COVID-19 e altera o Sistema de Informação Hospitalar do SUS (SIH/SUS) para permitir o registro de ações relativas ao enfrentamento da COVID-19. Brasília, DF; 2020 [cited 2021 Feb 12]. Available from: http://bvsms.saude.gov.br/bvs/saudelegis/saes/2020/prt0245_15_06_2020_rep.html
- 16.16. Secretaria de Saúde do Estado de São Paulo. Orientações AIH Covid-19. São Paulo, SP; 2020 [cited 2021 Feb 21]. (Circular; nº 320/2020). Available from: http://www.fehosp.com.br/files/circulares/5003fad52d33fc622273f3e3b911298b.pdf
- 17.17. Ministério da Saúde (BR), Departamento de Informática do Sistema Único de Saúde. Informações de Saúde: morbidade hospitalar do SUS por local de residência. Notas Técnicas. Brasília, DF: DATASUS; s.d. [cited 2021 Feb 10]. Available from: http://tabnet.datasus.gov.br/cgi/sih/nrdescr.htm
- 18.18. Ministério da Saúde (BR), Departamento de Informática do Sistema Único de Saúde. Informações de Saúde: Cadastro Nacional de Estabelecimentos de Saúde CNES. Notas Técnicas. Brasília, DF: DATASUS; s.d. [cited 2021 Feb 10]. Available from: http://tabnet.datasus.gov.br/cgi/cnes/NT_RecursosF%C3%ADsicos.htm
- 19.19. Lessa FJD, Mendes ACG, Farias SF, Sá DA, Melo Filho DA. Novas metodologias para vigilância epidemiológica: uso do Sistema de Informações Hospitalares - SIH/SUS. Inf Epidemiol SUS. 2000;9 Supl 1:3-27. 10.5123/S0104-16732000000500001 [DOI]
- 20.20. Rache B, Rocha R, Nunes L, Spinola P, Malik AM, Massuda A. Necessidades de infraestrutura do SUS em preparo ao COVID-19: leitos de UTI, respiradores e ocupação hospitalar. São Paulo, SP: Instituto de Estudos para Políticas de Saúde; 2020 [cited 2021 Feb 20]. (Nota Técnica; nº 3). Available from: https://ieps.org.br/pesquisas/necessidades-de-infraestrutura-do-sus-em-preparo-ao-covid-19-leitos-de-uti-respiradores-e-ocupacao-hospitalar/
- 21.21. REDE Interagencial de Informação para a Saúde Indicadores e Dados Básicos para a Saúde no Brasil. Brasília, DF: OPAS-Brasil; 2008 [cited 2021 Feb 20]. Capítulo 3, Fichas de Qualificação de Indicadores -E- Recursos: valor médio pago por internação hospitalar no SUS (AIH); p. 256. Available from: https://www.paho.org/bra/dmdocuments/indicadores.pdf
- 22.22. Menezes APR, Moretti BR, Reis AAC. O futuro do SUS: impactos das reformas neoliberais na saúde pública – austeridade versus universalidade. Saude Debate. 2019;43 Nº Espec 5:58-70. 10.1590/0103-11042019S505 [DOI]
- 23.23. Fernandes GAAL, Pereira BLS. Os desafios do financiamento do enfrentamento à COVID-19 no SUS dentro do pacto federativo. Rev Adm Publica. 2020;54(4):595-613. 10.1590/0034-761220200290 [DOI]
- 24.24. World Health Organization. Clinical management of severe acute interim guidance, 13 March 2020. Geneva (CH): WHO; 2020; [cited 2021 Feb 22]. Available from: https://apps.who.int/iris/handle/10665/331446
- 25.25. Cavalcante JR, Cardoso-dos-Santos AC, Bremm JM, Lobo AP, Macário EM, Oliveira WK, et al. COVID-19 no Brasil: evolução da epidemia até a semana epidemiológica 20 de 2020. Epidemiol Serv Saude. 2020;29(4):e2020376. 10.5123/s1679-49742020000400010 [DOI] [PubMed]
- 26.26. Rache B, Nunes L, Rocha R, Lago M, Fraga A. Como conter a curva no Brasil? Onde a epidemiologia e a economia se encontram. São Paulo, SP: Instituto de Estudos para Políticas de Saúde; 2020 [cited 2021 Feb 26]. (Nota Técnica; nº 4). Available from: https://ieps.org.br/pesquisas/como-conter-a-curva-no-brasil-onde-a-epidemiologia-e-a-economia-se-encontram/
- 27.27. Rache B, Rocha R, Nunes L, Spinola P, Massuda A. Para além do custeio: necessidades de investimento em leitos de UTI no SUS sob diferentes cenários da Covid-19. São Paulo, SP: Instituto de Estudos para Políticas de Saúde; 2020 [cited 2021 Feb 26]. (Nota Técnica; nº 7). Available from: https://ieps.org.br/pesquisas/para-alem-do-custeio-necessidades-de-investimento-em-leitos-de-uti-no-sus-sob-diferentes-cenarios-da-covid-19/
- 28.28. Kerr L, Kendall C, Silva EM, Pescarini JM, Almeida RLF, Ichihara MY, et al. COVID-19 no Nordeste brasileiro: sucessos e limitações nas respostas dos governos dos estados. Cienc Saude Coletiva. 2020;25 Supl 2:4099-120. 10.1590/1413-812320202510.2.28642020 [DOI] [PubMed]
- 29.29. Costa NRA. A disponibilidade de leitos em Unidade de Tratamento Intensivo no SUS e nos planos de saúde diante da epidemia da COVID-19 no Brasil. Rio de Janeiro, RJ: Observatorio Hospitalar Fiocruz; 2020 [cited 2021 Feb 25]. Available from: http://observatoriohospitalar.fiocruz.br/sites/default/files/biblioteca/ESTUDO%20NILSON_0.PDF
- 30.30. Ranzani OT, Bastos LSL, Gelli JGM, Maechesi JF, Baião F, Hamacher S, et al. Characterisation of the first 250,000 hospital admissions for COVID-19 in Brazil: a retrospective analysis of nationwide data. Lancet Respir Med. 2021;9(4):407-18. 10.1016/S2213-2600(20)30560-9 [DOI] [PMC free article] [PubMed]