Supplemental Digital Content is available in the text.
Keywords: COVID-19, cross-talk, oral dysbiosis, immune and metabolic dysregulation, Prevotella, vascular complications
Abstract
To date, coronavirus disease 2019 (COVID-19) has affected over 6.2 million individuals worldwide, including 1.46 million deaths. COVID-19 complications are mainly induced by low-grade inflammation-causing vascular degeneration. There is an increasing body of evidence that suggests that oral dysbiotic taxa are associated with worse prognosis in COVID-19 patients, especially the Prevotella genus, which was retrieved from nasopharyngeal and bronchoalveolar lavage samples in affected patients. Oral dysbiosis may act by increasing the likelihood of vascular complications through low-grade inflammation, as well as impairing respiratory mucosal barrier mechanisms against SARS-CoV-2. Salivary markers can be used to reflect this oral dysbiosis and its subsequent damaging effects on and the lungs and vasculature. Salivary sampling can be self-collected, and is less costly and less invasive, and thus may be a superior option to serum markers in risk stratification of COVID-19 patients. Prospective studies are needed to confirm such hypothesis.
Video Abstract: http://links.lww.com/CAEN/A28
Introduction
Coronavirus disease 2019 (COVID-19) is one of the largest public health pandemics since the Spanish flu of 1918. With a wide spectrum of clinical manifestations, COVID-19 has caused major setbacks in healthcare worldwide and challenged the capabilities of some of the most accomplished health care systems in the world. Although up to 80% of patients are initially asymptomatic, a nonnegligible percentage eventually require hospitalization and intensive care admission (ICU) [1].
Currently, the worst complication of COVID-19 is vascular inflammation and degeneration [2]. Dysbiosis, being closely related to vascular inflammation and degeneration, is one of the theories which may explain the interpersonal variability of COVID-19’s wide spectrum of manifestations [3]. Shen et al. [4] previously conducted serum proteomic profiling of COVID-19 patients and established a blood proteomic risk score (PRS) for the forecast of the patients’ clinical results. Kageyama et al. [5] showed that this proteomic profile is related to a particular set of proinflammatory intestinal microbiota. Chakraborty et al. [6] outlined the association of periodontopathic oral bacteria with unfavorable outcomes in COVID-19 patients.
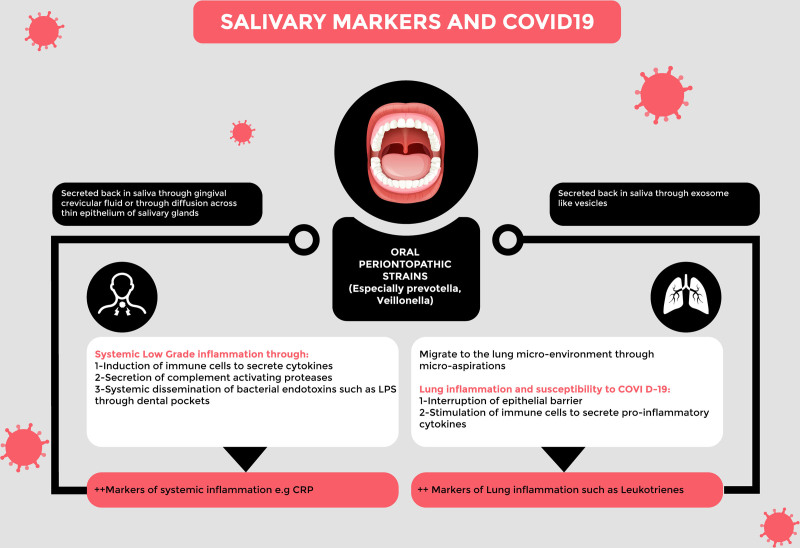
Salivary markers, such as C-reactive protein (CRP) and leukotrienes (exclusively perceptible in saliva), are simple and affordable tests that can be used to determine oral dysbiosis and periodontopathic strains. In this review, we summarize the available evidence, which suggests the role of oral microbiome dysbiosis in pulmonary and vascular inflammatory complications and the potential for salivary markers as a prognostic tool in COVID-19.
Low-grade inflammation association with coronavirus disease 2019 mortality and its relation to oral dysbiosis, the oral cavity-systemic inflammation axis
How oral microbiota contributes to low-grade inflammation?
According to recent studies, oral dysbiosis leads to chronic low-grade local and systemic inflammation. Periodontitis is one of the causes that increases the risk of cardiovascular disease, as well as contributes to the pathogenesis of atherosclerosis. Periodontitis patients have increased markers of systemic inflammation, including CRP, interleukin 6 (IL-6), haptoglobin and fibrinogen [7]. Rai et al. [8] found a link between oral dysbiosis and increased levels of interleukin 8 (IL-8), interleukin 6 (IL-6), tumor necrosis factor (TNF-α), granulocyte monocyte colony-stimulating factor (GM-CSF) and interferon γ (IFN-γ), which also increase the susceptibility to developing oral cancer.
Little is known about how oral dysbiosis induces systemic inflammation. The major depression model attempts to outline the systemic effects of dysbiosis [9]. Socransky et al. [10] investigated the mechanisms by which oral dysbiosis contributes to systemic inflammation. It is increasingly that a relationship between chronic periodontitis major depression exists. This relationship is the result of (1) stimulation of the immune system to secrete proinflammatory cytokines, mainly IL-6 and IL-8, (2) secretion of proteases that activate the associated complement system, (3) inflammation evoked by direct invasion of periodontal pathogen and their inflammatory products and (4) disturbances in the hypothalamic-pituitary-thyroid axis which alter periodontal status by affecting the immune system.
Within the periodontal pocket, bacteria exist in a stratified dental biofilm, which consists mainly of microorganisms and their components (endotoxins and lipopolysaccharides). When inflammation in the periodontal pocket occurs, it becomes a significant source of inflammatory and pathogen-derived mediators. In a healthy individual, the majority of bacteria are Gram-positive aerobes, whereas, in periodontitis individuals, around 85% of the bacteria are Gram-negative, according to Socransky et al. [10]. These bacteria invade the intact pocket epithelium and subsequently gain access to the circulation resulting in systemic dissemination of bacterial products.
Association of coronavirus disease 2019 complications with disease states related to low-grade inflammation
Low-grade inflammation (LGI), characterized by a chronic increase in inflammatory cytokines (IL-6, TNF-α and IL-1-β), is the cornerstone of all the high-risk classifications for developing severe COVID-19. Hyperglycemia, obesity and hypertension, all features of metabolic syndrome (MetS), are believed to increase the risk of cardiovascular disease and type 2 diabetes mellitus and are accompanied by LGI. In severe acute respiratory syndrome (SARS-CoV-2) patients, target tissues including the lungs, brain, gut and kidneys are infiltrated with proinflammatory macrophages and lymphocytes, which lead to hypercytokinaemia that supplements LGI in MetS patients. It has been found that patients with IL-6 levels of ≥80 pg/ml had a greater risk of developing respiratory failure by 22 times than that for patients with lower IL-6 level [11].
In high-risk patients with chronic LGI and SARS-CoV-2 infection, cellular immune response is mediated mainly by T-helper cells (Th) 1, Th-17, and proinflammatory macrophages. Therefore, a ‘normal’ proinflammatory response may intensify cytokine levels above those of the underlying LGI, increasing the risk of developing fatal forms of COVID-19. This suggests that in cases of SARS-Cov-2 infection, a ‘normal’ antiviral immune response in combination with LGI may trigger fatal consequences [12].
Evidence of association of oral dysbiosis with disorders characterized by low-grade inflammation such as obesity
Obesity and related complications
Evidence suggests that obesity may be induced by alterations in the oral microbiota. Data from Tam et al. [13] series revealed that there are discriminative features of microbiota between obese and nonobese patients. Bacteroidetes and Spirochaetes were more dominant in subgingival plaques on nonobese populations, while Proteobacteria, Chloroflexi and Prevotella/Firmicutes were more dominant in the obese population, with the noted absence of representatives from the phylum Bacteroidetes. The phylum Firmicutes was identified in obese patients as an independent, significantly discriminative feature, with an abundance of over four orders of magnitude. These findings in the oral cavity coincide with the observed microbiota of the gut in obese individuals, which is characterized by a reduced abundance of Bacteroidetes paralleled by an increased abundance of Firmicutes; a lower ratio of Bacteroidetes to Firmicutes (B:F) exists in obese patients [14,15]. Verdam et al. [16] demonstrated that the low B:F ratios and increased predominance of Prevotella observed in obese individuals contributed to intestinal inflammation (as shown by high levels of calprotectin), as well as increased the likelihood of systemic inflammation associated with obesity.
Vascular degeneration and oral dysbiosis
The severity of COVID-19 has been linked to a state of vascular degeneration, as evidenced by the increased risk of thromboembolic events seen in severely ill patients. Evidence suggests that oral dysbiosis is associated with a greater risk of vascular degeneration [17].
Grau et al. [18] found that individuals with periodontitis had a greater risk of developing stroke by 400% than those with caries. Another study found a correlation between intimal thickening (used as a surrogate measure of atherosclerosis) and periodontal pathogens, but not health-compatible organisms [19]. Systemic antibody levels have been linked to periodontal pathogens, as well as the incidence of coronary heart disease and subclinical atherosclerosis. This data suggests a connection between periodontal pathogens and the incidence of cardiovascular disease [19].
Chhibber-Goel et al. [20] used next-generation sequencing to analyze bacterial species in atherosclerotic plaques; the most characteristic taxa were Prevotella and Veillonella.
Periodontal bacteria can contribute to atherogenesis by destabilization of the atherosclerotic plaque. Prevotella gingivalis infection is associated with the proliferation of smooth muscle cell tissue in developing aneurysms, especially aortic aneurysms [21].
The concentrations of IL-18 and IFN-γ are reduced by 90% at 12 months post periodontal therapy. This finding is of special importance as levels of IL-18 are used to predict (1) acute myocardial infarction in coronary artery disease patients, (2) major cardiovascular events seen 6 months after hospitalization in individuals with acute coronary syndrome and (3) IL-18 independently predicts congestive heart failure, myocardial infarction, cardiovascular death, as well as all-cause non-CVD death [22].
Status of lung microbiome in coronavirus disease 2019 and relationship to oral microbiome: oral-lung axis
The pathway to which microbes reach the lungs is believed to originate from the oral cavity, through microaspiration as taxonomic profiles showed identical organisms. The use of culture-independent techniques concluded that the mouth and lung microbiota are similar, which suggests that saliva does not only reflect low-grade systemic inflammation but gives an idea about the lung environment as well. One of the major periodontopathic strains, Prevotella, has been associated with negative outcomes in the lungs [23–25].
Shen suggests that there is an association between microbiota, COVID-19 and some opportunistic infectious agents. Prevotella significantly coexists with COVID-19, alongside Capnocytophaga and Veillonella [26,27].
These findings were confirmed by Chakraborty et al. [6] by identifying the interplay between Prevotella and SARS-CoV-2 in the lung microenvironment, leading to the development of severe acute symptoms and the persistence of chronic lung injury in affected patients. Lung epithelium and proximal and distal airways play a pivotal role in maintaining immune homeostasis, mainly as a first line of defense against inhaled bacterial, fungal and viral pathogens. Culture supernatant fluids of P intermedia are cytotoxic to airway epithelial cells, resulting in their destruction and subsequently the loss of the barrier that protects against viral infections, which may explain the link between Prevotella and SARS-CoV-2 in the Shen and Chakraborty series [28].
A major function of lung microbiota is to mitigate the inflammatory response located within the lungs (alternatively termed ‘tolerance’). The presence of high bacterial load and predominant taxa derived from the upper respiratory tract has been associated with an attenuated immune response of alveolar macrophages to lipopolysaccharide. This suggests the role of microbiota in regulating inflammatory responses at the pulmonary mucosal surface. The presence of members of the Bacteroidetes phylum decreases lung inflammation, while Prevotella spp. and Veillonella spp. increase Th-17 cell-mediated lung inflammation, as demonstrated by other human studies [29,30].
Prevotella and Veillonella species are associated with low-grade systemic inflammation, defective lung epithelial barriers and increased likelihood of exaggerated pulmonary inflammation. Evidently, these two taxa gain access to the lungs through the oral cavity, as they are predominant periodontopathic strains. Table 1 summarizes the above-mentioned evidence of Prevotella and its reported systemic and pulmonary proinflammatory roles.
Table 1.
Examples of the oral, systemic and pulmonary pathogenic roles of Prevotella species
| Oral dysbiosis | Low-grade systemic inflammation |
|
|---|---|---|
| Prevotella is a major pathogen of periodontitis reflecting oral dysbiosis [23] | Prevotella has been fund as a component of atherosclerotic plaques [20] | |
| Pulmonary effects | Prevotella is linked to higher obesity risk, and higher rates of obesity related complications [15] | |
| Prevotella is linked to lung disorders associated with increased leukotrienes such as asthma [30] | ||
| Prevotella in BAL has been linked to severe lung injury in influenza patients [25] | Prevotella in nasopharyngeal samples and BAL has been linked to severity of COVID-19 [6,26] | |
BAL, bronchoalveolar lavage; COVID-19, coronavirus disease 2019.
Salivary markers: a mirror of systemic and pulmonary proinflammation
Mechanism of secretion of salivary markers: saliva is a mirror of the serum markers
One of the most important diagnostic tools for detecting salivary pathologies is salivary analysis. It is simple, noninvasive, inexpensive and easy to store. Salivary analysis has become a very popular laboratory investigation for the diagnosis of oral and systemic diseases.
The use of saliva has been appreciated as it can determine the normal internal characteristics and disease state of an individual 7, due to the fact that it is exchanged with different substances that are components of plasmatic liquid. This is as a result of the presence of a thin layer of epithelial cells, which separates the salivary ducts from the systemic circulation. Substances could be transferred to the saliva through (1) active carriage, (2) diffusing through the membrane (ultrafiltration) or (3) through passive diffusion via a concentration gradient [31].
The oral cavity can host many types of oral microbiota, which are inducers of inflammatory mediators such as cytokines. Additionally, there are other forms of microbiota that can gain access to the serum via inflamed and disrupted periodontal pocket.
Therefore, the link between saliva and blood appears bidirectional, whereby the composition of both these body compartments affect and reflect each other.
Salivary markers and lung inflammation
Saliva reflects the systemic markers of inflammation. There is increasing evidence that suggests a continuous migration of pulmonary inflammatory markers to the oral cavity. One of the most important markers of decreased epithelial integrity and lung inflammation is leukotrienes. Ono et al. [32] proved that salivary leukotrienes are can be relied upon as sensitive indicators of airway inflammation in asthma. The mechanism by which the lung microenvironment confers its markers to the oral cavity is not completely understood. However, one of the suggested mechanisms is the exchange of exosome-like vesicles between different organs. The infrastructure of extracellular vehicles has been extensively investigated. Extracellular vehicles carry bioactive compounds (proteins, nucleic acids, lipids and metabolites like leukotriene) within their inner core or in their lipid bilayer, which may suggest that the source of salivary leukotrienes is partly conveyed by such vesicles [7].
Implication: use of salivary biomarkers for risk stratification of coronavirus disease 2019
The detection of certain bacterial taxa in the oral cavity is associated with low-grade systemic and pulmonary inflammation in the context of COVID-19, as discussed in section II. These periodontopathic taxa, namely Prevotella and Veillonella, have been found to overpopulate the lung microenvironment.
A major prognostic predictor for COVID-19 associated complications is the detection of such strains in the oral cavity. The use of salivary biomarkers may serve as an alternative prognostic tool for COVID-19 disease.
Research has yet to point out an association of these bacterial taxa in the oral cavity with the elevation of particular biomarkers, but several studies have compared the incidence of periodontitis (associated with the same strains) with the elevation of salivary biomarkers.
Salivary C-reactive protein
Salivary testing has recently gained much interest, as it is noninvasive, inexpensive and can be self-sampled as compared to serum markers. This interest has extended the use of saliva-based screening for COVID-19 in place of the traditional nasopharyngeal swab; saliva was equal to swab testing in the diagnostic accuracy of COVID-19 [33].
Salivary CRP, initially produced by the liver, enters the saliva via gingival crevicular fluid as one of its components or through the salivary glands. According to the study done by Savitha and Shasmitha, salivary CRP concentrations were higher in periodontitis patients compared to healthy individuals, which suggests that salivary CRP is increased in inflammatory conditions of the oral cavity [34]. Salivary inflammatory markers were also identified by Labat et al. [35] to aid in cardiovascular disease and risk factors prediction. High salivary CRP levels correlating to plasma CRP levels were associated with inflammatory conditions such as arterial stiffness, atherosclerosis and metabolic syndrome. The suggestion arises that salivary CRP is used as a prognostic marker during the earliest encounter with the COVID-19 patient.
Salivary leukotrienes (LBT4)
Leukotrienes are lipid inflammatory mediators that are suggested markers of airway hypersensitivity. Multiple extrapulmonary negative outcomes have been tied to Leukotrienes. LTB4 is highly linked to periodontitis and was proven by Emingil et al. [36] to be a periodontitis marker.
Leukotrienes were shown to be involved in the arterial stiffness pathogenesis. In atherosclerosis, some inflammatory alterations involve the endothelial monolayer, which cannot resist leucocyte contact compared to the normal state. In subclinical atherosclerosis, leukotrienes have been proposed to be mediators, biomarkers and therapeutic targets. Their role in the pathogenesis of COVID-19-related complications was initially discarded until Funk et al. [37] pointed out the principal role of leukotrienes in the pathogenesis of acute respiratory distress syndrome (ARDS) in COVID-19. Leukotrienes were not previously considered due to undetectable levels in serum. Since the comparison of bronchoalveolar lavage (BAL) leukotrienes levels across patients with variable severity is nearly inapplicable, it became difficult to define their exact role in COVID-19. However, oral samples have been shown to include readily measurable LTB4 concentrations, which then decreased after oral treatment with an antiasthmatic leukotriene synthesis inhibitor. Widegren et al. [38] proved that LTB4 utilizes specific neutrophil chemoattractant properties and virucidal effects against Coronaviridae.
More studies are needed to confirm the association of salivary markers with the predominance of Prevotella and Veillonella in the oral and lung microenvironment.
Figure 1 summarizes the connection between oral microbiome, LGI and lung damage, as well as the implications for the use of salivary makers in risk stratification of COVID-19 cases.
Fig. 1.
Salivary markers and COVID-19. COVID-19, coronavirus disease 2019; CRP, C-reactive protein.
Conclusion
Periodontopathic strains, namely Prevotella and Veillonella, have the potential to induce low-grade systemic inflammation, increasing the likelihood of vascular degeneration and metabolic complications such as obesity. They can also compromise the lung mucosal barrier, thus facilitating SARS-CoV-2 entry. These taxa have been persistently found in BAL and nasopharyngeal samples of COVID-19 patients, and their retrieval has been associated with a worse prognosis. The use of next-generation sequencing to detect the presence of these species in the oral cavity would be a useful but a costly strategy for prediction of vascular complications of COVID-19. Alternatively, salivary biomarkers can predict the presence of these periodontopathic strains and are sensitive markers of vascular degeneration as well as pulmonary inflammation. Their use is superior to serum sampling due to the possibility of self-sampling, thus minimizing contact with infected patients. Their use can also better reflect the ongoing damage in the lungs as sensitive markers of lung damage (such as leukotrienes) are retrievable from the saliva while being almost undetectable in the blood. Prospective studies should be conducted by working groups globally to determine the exact salivary signature of COVID-19 and to test its feasibility as prognostic tool for the risk stratification of patients.
Acknowledgements
I want to thank as a first author, the parents of my junior co-authors, they have definitely played a crucial role in raising their critical thinking and in developing their abilities. I also wanted to thank all the co-founders and key mentors of “Research accessibility team” initiative. This idea involved, to date, 412 students and created 11 international publications in less than 10 months. Finally, yet importantly, I want to thank the Cardiovascular Endocrinology and Metabolism team, for their contribution to the success of our research initiative.
Supplementary Material
Footnotes
Supplemental Digital Content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's website, www.cardiovascularendocrinology.com.
References
- 1.Johns Hopkins Coronavirus Resource Center. COVID-19 Map. Johns Hopkins Coronavirus Resource Center-Johns Hopkins University & Medicine. 2020. [Google Scholar]
- 2.AbdelMassih AF, Kamel A, Mishriky F, Ismail H, El L, Malak L, et al. Is it infection or rather vascular inflammation? Game-changer insights and recommendations from patterns of multi-organ involvement and affected subgroups in COVID-19. Cardiovasc Endocrinol Metab 2020; 9:110–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ma J, Li H. The role of gut microbiota in atherosclerosis and hypertension. Front Pharmacol. 2018; 9:1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shen B, Yi X, Sun Y, Bi X, Du J, Zhang C, et al. Proteomic and metabolomic characterization of COVID-19 patient sera. Cell. 2020; 182:59–72.e15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kageyama Y, Akiyama T, Nakamura T. Intestinal dysbiosis and probiotics in COVID-19. J Clin Trials. 2020; 10:2167–2870. [Google Scholar]
- 6.Chakraborty S. SARS-Cov2 enables anaerobic bacteria (Prevotella, et al) to colonize the lungs disrupting homeostasis, causing long-drawn chronic symptoms, and acute severe symptoms (ARDS, septic shock, clots, arterial stroke) which finds resonance, with key differences. OSF Preprints 2020:2019–2021. [Epub ahead of print]
- 7.Kirk P, Carpenter JP, Tanner MA, Pennell DJ. Low prevalence of fibrosis in thalassemia major assessed by late gadolinium enhancement cardiovascular magnetic resonance. J Cardiovasc Magn Reson. 2011; 13:8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rai AK, Panda M, Das AK, Rahman T, Das R, Das K, et al. Dysbiosis of salivary microbiome and cytokines influence oral squamous cell carcinoma through inflammation. Arch Microbiol. 2020. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 9.Hashioka S, Inoue K, Hayashida M, Wake R, Oh-Nishi A, Miyaoka T. Implications of systemic inflammation and periodontitis for major depression. Front Neurosci. 2018; 12:483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Socransky SS, Haffajee AD. Dental biofilms: difficult therapeutic targets. Periodontol 2000. 2002; 28:12–55. [DOI] [PubMed] [Google Scholar]
- 11.Ciornei RT. Prevention of severe coronavirus disease 2019 outcomes by reducing low-grade inflammation in high-risk categories. Front Immunol. 2020; 11:1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tay MZ, Poh CM, Rénia L, MacAry PA, Ng LFP. The trinity of COVID-19: immunity, inflammation and intervention. Nat Rev Immunol. 2020; 20:363–374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tam J, Hoffmann T, Fischer S, Bornstein S, Gräßler J, Noack B. Obesity alters composition and diversity of the oral microbiota in patients with type 2 diabetes mellitus independently of glycemic control. PLoS One. 2018; 13:e0204724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Goodson JM, Groppo D, Halem S, Carpino E. Is obesity an oral bacterial disease? J Dent Res. 2009; 88:519–523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hjorth MF, Blædel T, Bendtsen LQ, Lorenzen JK, Holm JB, Kiilerich P, et al. Prevotella-to-Bacteroides ratio predicts body weight and fat loss success on 24-week diets varying in macronutrient composition and dietary fiber: results from a post-hoc analysis. Int J Obes (Lond). 2019; 43:149–157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Verdam FJ, Fuentes S, de Jonge C, Zoetendal EG, Erbil R, Greve JW, et al. Human intestinal microbiota composition is associated with local and systemic inflammation in obesity. Obesity (Silver Spring). 2013; 21:E607–E615. [DOI] [PubMed] [Google Scholar]
- 17.AbdelMassih AF, Mahrous R, Taha A, Saud A, Osman A, Kamel B, et al. The potential use of ABO blood group system for risk stratification of COVID-19. Med Hypotheses. 2020; 145:110343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Grau AJ, Becher H, Ziegler CM, Lichy C, Buggle F, Kaiser C, et al. Periodontal disease as a risk factor for ischemic stroke. Stroke. 2004; 35:496–501. [DOI] [PubMed] [Google Scholar]
- 19.Kumar PS. Oral microbiota and systemic disease. Anaerobe. 2013; 24:90–93. [DOI] [PubMed] [Google Scholar]
- 20.Chhibber-Goel J, Singhal V, Bhowmik D, Vivek R, Parakh N, Bhargava B, Sharma A. Linkages between oral commensal bacteria and atherosclerotic plaques in coronary artery disease patients. NPJ Biofilms Microbiomes. 2016; 2:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Salhi L, Rompen E, Sakalihasan N, Laleman I, Teughels W, Michel JB, Lambert F. Can periodontitis influence the progression of abdominal aortic aneurysm? A systematic review. Angiology. 2019; 70:479–491. [DOI] [PubMed] [Google Scholar]
- 22.Borgnakke WS. Does treatment of periodontal disease influence systemic disease? Dent Clin North Am. 2015; 59:885–917. [DOI] [PubMed] [Google Scholar]
- 23.Torrungruang K, Jitpakdeebordin S, Charatkulangkun O, Gleebbua Y. Porphyromonas gingivalis, aggregatibacter actinomycetemcomitans, and Treponema denticola/prevotella intermedia co-infection are associated with severe periodontitis in a Thai population. PLoS One. 2015; 10:e0136646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Xu N, Wang L, Li C, Ding C, Li C, Fan W, et al. Microbiota dysbiosis in lung cancer: evidence of association and potential mechanisms. Transl Lung Cancer Res. 2020; 9:1554–1568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hanada S, Pirzadeh M, Carver KY, Deng JC. Respiratory viral infection-induced microbiome alterations and secondary bacterial pneumonia. Front Immunol. 2018; 9:2640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shen Z, Xiao Y, Kang L, Ma W, Shi L, Zhang L, et al. Genomic diversity of severe acute respiratory syndrome–coronavirus 2 in patients with coronavirus disease 2019. Clin Infect Dis. 2020; 71:713–720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bao L, Zhang C, Dong J, Zhao L, Li Y, Sun J. Oral microbiome and SARS-CoV-2: beware of lung co-infection. Front Microbiol. 2020; 11:1840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ulrich M, Beer I, Braitmaier P, Dierkes M, Kummer F, Krismer B, et al. Relative contribution of Prevotella intermedia and pseudomonas Aeruginosa to lung pathology in airways of patients with cystic fibrosis. Thorax. 2010; 65:978–984. [DOI] [PubMed] [Google Scholar]
- 29.Sommariva M, Le Noci V, Bianchi F, Camelliti S, Balsari A, Tagliabue E, Sfondrini L. The lung microbiota: role in maintaining pulmonary immune homeostasis and its implications in cancer development and therapy. Cell Mol Life Sci. 2020; 77:2739–2749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lopes MP, Cruz ÁA, Xavier MT, Stöcker A, Carvalho-Filho P, Miranda PM, et al. Prevotella intermedia and periodontitis are associated with severe asthma. J Periodontol. 2020; 91:46–54. [DOI] [PubMed] [Google Scholar]
- 31.Yoshizawa JM, Schafer CA, Schafer JJ, Farrell JJ, Paster BJ, Wong DT. Salivary biomarkers: toward future clinical and diagnostic utilities. Clin Microbiol Rev. 2013; 26:781–791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ono E, Taniguchi M, Higashi N, Mita H, Yamaguchi H, Tatsuno S, et al. Increase in salivary cysteinyl-leukotriene concentration in patients with aspirin-intolerant asthma. Allergol Int. 2011; 60:37–43. [DOI] [PubMed] [Google Scholar]
- 33.Pasomsub E, Watcharananan SP, Boonyawat K, Janchompoo P, Wongtabtim G, Suksuwan W, et al. Saliva sample as a non-invasive specimen for the diagnosis of coronavirus disease 2019: a cross-sectional study. Clin Microbiol Infect. 2020. https://linkinghub.elsevier.com/retrieve/pii/S1198743X20302780. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lurie N, Saville M, Hatchett R, Halton J. Developing Covid-19 vaccines at pandemic speed. N Engl J Med. 2020; 382:1969–1973. [DOI] [PubMed] [Google Scholar]
- 35.Oz F, Cizgici AY, Ucar A, Karaayvaz EB, Kocaaga M, Bugra Z, et al. Doppler-derived strain imaging detects left ventricular systolic dysfunction in children with Turner syndrome. Echocardiography. 2014; 31:1017–1022. [DOI] [PubMed] [Google Scholar]
- 36.Emingil G, Çinarcik S, Baylas H, Çoker I, Hüseyinov A. Levels of leukotriene B 4 in gingival crevicular fluid and gingival tissue in specific periodontal diseases. J Periodontol. 2001; 72:1025–1031. [DOI] [PubMed] [Google Scholar]
- 37.Funk CD, Ardakani A. A novel strategy to mitigate the hyperinflammatory response to COVID-19 by targeting leukotrienes. Front Pharmacol. 2020; 11:1214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Widegren H, Andersson M, Borgeat P, Flamand L, Johnston S, Greiff L. LTB4 increases nasal neutrophil activity and conditions neutrophils to exert antiviral effects. Respir Med. 2011; 105:997–1006. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.