Graphical Abstract
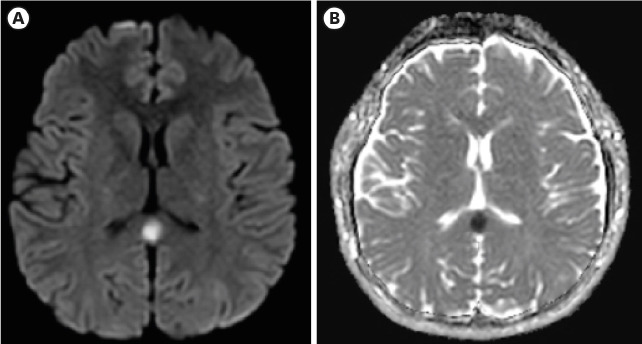
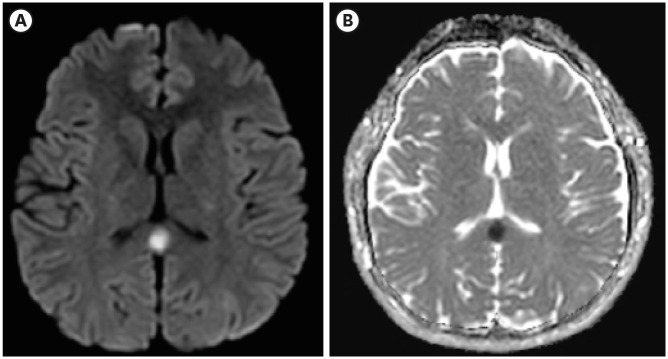
A 22-year-old previously healthy man visited the emergency department. He received the first dose of SARS-CoV-2 mRNA vaccine (BNT162b) 3-days prior coming to the hospital. He complained of febrile sensation and headache around the eyes and forehead. Upon admission, he was alert and neurologic examination showed that cranial nerves were grossly intact with both deep tendon reflexes and muscle strength being normal. There were signs of suspicious mild nuchal rigidity but not evident. SARS-CoV-2 polymerase chain reaction (PCR) that was performed due to fever turned out to be negative. Initial chemistry results showed leukopenia (3200/uL) and thrombocytopenia (141000/uL) with serum sodium being in the normal range (142mmol/L). There was no pleocytosis (WBC 2/uL) or other abnormalities in the CSF study. The patient's brain magnetic resonance imaging (MRI) showed an oval shaped restricted diffusion in the corpus callosum with low apparent diffusion coefficient (ADC) values and lack of contrast mediated enhancement (Fig. 1). He was transferred to a tertiary hospital emergency department and admitted, being diagnosed with cytotoxic lesion of the corpus callosum (CLOCCs) after SARS-CoV-2 mRNA vaccination. After that, the patient's symptoms improved and he was discharged 2 days later with no notable changes to be mentioned in the following outpatient check-up a week later.
Fig. 1. The brain magnetic resonance imaging (MRI) of a 22-year-old patient who received the first dose of SARS-CoV-2 mRNA vaccine (BNT162b) 3-days prior coming to the hospital. (A, B) The brain images show an oval-shaped restricted diffusion in the corpus callosum with low apparent diffusion coefficient (ADC) values. The patient was diagnosed with cytotoxic lesion of the corpus callosum (CLOCCs) after SARS-CoV-2 mRNA vaccination.
CLOCCs are associated with many disease entities including malignancy, infections, subarachnoid hemorrhage, metabolic abnormality, trauma and vaccination.1 Corpus callosal lesions with low abnormal diffusion restriction and low ADC values are known to be caused by cytotoxic edema.2 It has been generally agreed that cytotoxic edema is related to glutamate releasing from astrocytes that are stimulated by cytokines, culminating in the influx of water within cells.3 Important differential diagnoses of CLOCCs include ischemic stroke of anterior cerebral artery distal branch and acute disseminated encephalomyelitis (ADEM). However, lesions of stroke and ADEM tend to be asymmetric and more aggressive than CLOCCs.1 Furthermore, because of redundant blood supply to the corpus callosum, ischemic infarction is rare in the region.4 Recently a few cases have reported relationship between COVID-19 and CLOCCs.5 Also, multisystem inflammatory syndrome has recently been demonstrated to result in CLOCCs among the children suffering from cytokine storms.6 This is a limited single neuroimaging finding of the patient who received the first jab of SARS-CoV-2 mRNA vaccine (BNT162b) with the underlying mechanism needing further investigation. However, to our knowledge, CLOCCs after all types of COVID-19 vaccination has not yet been reported and we would like to share a single adverse event. A mRNA vaccine is a novel type protecting from COVID-19 with indisputable efficacy, however its adverse effects must not be overlooked when patients seek medical attention after vaccination. Clinicians should be aware of not only the common side effects of COVID-19 vaccination but also uncommon adverse effects resulting from SARS-CoV-2 vaccination.
Ethics statement
Ethic approval for this study was waived by Institutional Review Board (IRB) of Aerospace Medical Center (IRB No. ASMC-21-IRB-010). The images are published under the agreement of the patient.
Footnotes
Disclosure: The authors have no potential conflicts of interest to disclose.
- Conceptualization: Yang H.
- Data curation: Youn T.
- Writing - original draft: Yang H, Youn T.
- Writing - review & editing: Yang H.
References
- 1.Starkey J, Kobayashi N, Numaguchi Y, Moritani T. Cytotoxic lesions of the corpus callosum that show restricted diffusion: mechanisms, causes, and manifestations. Radiographics. 2017;37(2):562–576. doi: 10.1148/rg.2017160085. [DOI] [PubMed] [Google Scholar]
- 2.Moritani T, Smoker WR, Sato Y, Numaguchi Y, Westesson PL. Diffusion-weighted imaging of acute excitotoxic brain injury. AJNR Am J Neuroradiol. 2005;26(2):216–228. [PMC free article] [PubMed] [Google Scholar]
- 3.Matute C, Alberdi E, Domercq M, Sánchez-Gómez MV, Pérez-Samartín A, Rodríguez-Antigüedad A, et al. Excitotoxic damage to white matter. J Anat. 2007;210(6):693–702. doi: 10.1111/j.1469-7580.2007.00733.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kasow DL, Destian S, Braun C, Quintas JC, Kagetsu NJ, Johnson CE. Corpus callosum infarcts with atypical clinical and radiologic presentations. AJNR Am J Neuroradiol. 2000;21(10):1876–1880. [PMC free article] [PubMed] [Google Scholar]
- 5.Rasmussen C, Niculescu I, Patel S, Krishnan A. Covid-19 and involvement of the corpus callosum: potential effect of the cytokine storm? AJNR Am J Neuroradiol. 2020;41(9):1625–1628. doi: 10.3174/ajnr.A6680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lin J, Lawson EC, Verma S, Peterson RB, Sidhu R. Cytotoxic lesion of the corpus callosum in an adolescent with multisystem inflammatory syndrome and SARS-CoV-2 infection. AJNR Am J Neuroradiol. 2020;41(11):2017–2019. doi: 10.3174/ajnr.A6755. [DOI] [PMC free article] [PubMed] [Google Scholar]