Abstract
The association of leisure time activities with specific mental disorders has mainly remained unclear because of lack of such research. This study analyzed the association of different levels of social leisure time activity during adolescence (ages 15–16 years) with the incidence of mental disorders during adolescence and young adulthood between the ages of 16–33 years. The study population consisted of 6838 (females 51.5%) participants from the longitudinal follow-up study, the Northern Finland Birth Cohort 1986, covering 72% of the total 1986 birth cohort. Psychiatric morbidity of the participants was followed through nationwide health registers until the end of the year 2018 when the participants were 33 years old. High social leisure time activity in adolescence associated with lower incidence of psychiatric disorders in general, and specifically, with affective, anxiety, and substance use disorders. Low social leisure time activity was related to increased incidence of any psychiatric disorder in general, and particularly to anxiety and behavioral disorders. In terms of prevention of mental disorders, these study findings encourage families, schools and other communities to continue to enhance and develop community-based social leisure time activities for children and adolescents.
Keywords: Adolescents, Mental disorder, Mental health, Social leisure time activity, Community
Introduction
Adolescence is a significant period for psychological development. During this period, leisure time activities make up a significant part of life and they are generally acknowledged to have positive impact on adolescents’ current mental wellbeing (e.g. Rodriguez et al., 2019) However, the relationship between leisure time activity and the development of specific mental disorders has remained unclear. This would be important information for planning and targeting preventive actions during adolescence. The current study examines the longitudinal associations between adolescents’ social leisure activities and the psychiatric diagnoses set in healthcare services by young adulthood.
Leisure time activity is commonly defined as having fun and relaxing activities (Torkildsen, 2005). Involvement in these activities has shown to strengthen adolescents’ physical health, mental well-being, relationship with parents, peer support and perception of academic well-being (e.g., Rochelle et al., 2013). Both cultural and physical activities have been found to be associated with improved self-esteem and psychosocial states, as well as with lower levels of current depressive symptoms and anxiety (Hansen et al., 2015). Accordingly, adolescents with low leisure time activity are reported to have significantly more mental health problems, such as depressive symptoms, anxiety (Bélair et al., 2018), increased substance use and risk behaviors (e.g. Agans et al., 2014), compared to adolescents with active leisure time. The social relationships in leisure time activities have also been emphasized as a possible mediator of the benefits of these activities (e.g., Oberle et al., 2019). Participation in meaningful social leisure time activities has been found to have a positive impact on current and future mental health (Ströhle et al., 2007; Hoegh Poulsen et al., 2016; Doré et al., 2018).
The results of previous studies on the effects of leisure time on mental health remain limited. Most are based on self-assessment questionnaires (see, for example, Badura et al., 2015; Tamminen et al., 2020; Ferreira et al., 2020) or are focus on current mental health issues (e.g. Doré et al., 2016). Research focusing on specific mental disorders conducted in longitudinal study settings is thus mainly lacking.
Limitations in existing research is particularly problematic. That research has demonstrated that different kinds of leisure time activities during adolescence are associated with mental health in general. This knowledge has been an incentive to develop various community-based leisure time models aiming to enhance mental health among youth. Examples of such models are the Icelandic model (Sigfúsdóttir et al., 2011), scout participation (Dibben et al., 2016) and cultural participation (Hansen et al., 2015). However, more research-based information of the relationship of leisure activity and mental health is needed to find effective preventive methods to reverse the alarming rise in the need of psychiatric care for young people.
Current Study
Research is still limited on whether leisure time activities during adolescence associate with later physician-diagnosed mental health disorders. This research-based information would be of great importance to recognize potential objectives for preventive actions for mental health disorders and thus reduce the need for the use of mental health services. The main objective of this longitudinal study was to examine at epidemiological level the association of socially different leisure time activities at ages 15–16 years with first-onset mental disorders diagnosed in clinical settings at ages 16–33 years. Three specific research questions were addressed. First, the level of social leisure time activity of the study participants was assessed based on a postal survey completed at ages 15–16 years. Second, the psychiatric diagnoses at 16–33 years were extracted from the health care registers. Third, the association of the level of social leisure time activity with first-onset mental disorders was examined after controlling for family-related factors of the study participants.
Methods
Study Population
The study population covers the members of the 1986 Northern Finland Birth Cohort Study (NFBC1986). It is an ongoing longitudinal follow-up study including children born in Northern Finland between July 1, 1985 and June 30, 1986. The study involved 99% of the age group of the children born in Northern Finland, of a total of 9432 live-born children. The focus of the NFBC1986 study is to assess morbidity, mortality, and social well-being as well as to identify high-risk groups and possible biological factors that enable risk prevention (Jokela et al., 2019). The NFBC1986 data consisted of postal surveys, clinical trials, and register-based data of the participants as well as parental data based on postal surveys and national registers.
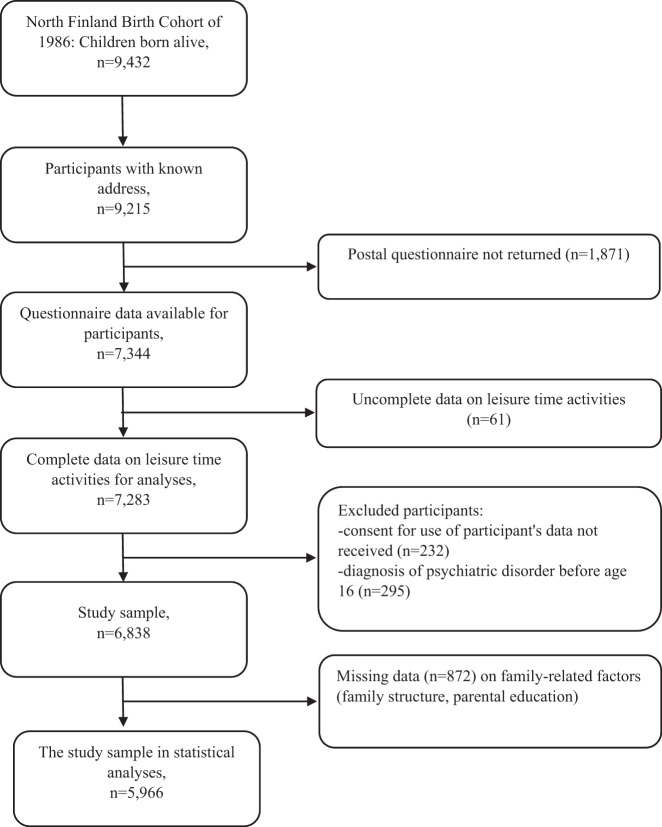
The original cohort study population consisted of 9423 subjects. For follow-up surveys, 9215 cohort members had a known mailing address. Of them, 7344 returned the postal survey administered at the age of 15–16 years. Questions related to hobbies were answered by 7283 cohort members, of whom 7051 gave permission to use their data for research purposes. Of 7051 cohort members, a total of 213 were excluded from this study because of mental disorder diagnoses set before 16 years of age. The most common diagnoses of the excluded participants were behavioral and emotional disorders, with onset usually occurring in childhood and adolescence (F90–F98) (35.2%), mood (affective) disorders (F30–F39) (23.9%), anxiety disorders (F40–F49) (17.4%), and disorders of psychological development (F80–F89) (17.4%).
The final study population contained 6838 participants, covering 72% of the total 1986 birth cohort (Fig. 1). In the current study, psychiatric morbidity of the participants was followed through health registers from 16 years of age until the end of the year 2018 when the participants were 33 years old.
Fig. 1.
Sampling of the data
Data Sources
The psychiatric disorders are based on the inpatient data from the Care Register for Health Care (CRHC) until 2018, and on the data of specialized level outpatient visits available for the years 1998–2018. The CRHC has been found to be a reliable source of information in scientific research. (Miettunen et al., 2011; Gissler and Haukka, 2004). The diagnoses recorded in the CRHC are always set by physicians. The main and secondary diagnoses were taken into account in the screening of psychiatric morbidity of the study participants.
The information of parents’ mental disorders (F00–F69, F80–F99, main and secondary diagnoses) were extracted from the following nationwide registers: inpatient treatments from the Care Register for Health Care (until 2018), specialized level outpatient visits (1998–2018) and primary care (2011–2018) from the Care Register for Health Care, and information of disability pensions from the Finnish Center for Pensions (until 2016).
Participants in the cohort study and their parents were asked for signed consent to use their data for research purposes. The study obtained approval from the Ethical Review Board of the National Institute for Health and Welfare (Section 28/2009), from the Ethics Committee of Northern Ostrobothnia Hospital District (EETTMK: 108/2017) and Oulu University, Faculty of Medicine, Oulu, Finland. In addition, official permission to use individual-level register-based data for scientific research was obtained from the administration of each register.
Measures
Psychiatric disorders of the study participants
The main outcomes of the current study were psychiatric disorders of the study subjects. In addition to any psychiatric disorders (ICD-10 codes: F00-F99), the following main diagnostic categories were analyzed: mental and behavioral disorders due to psychoactive substance use (F10–F19); schizophrenia, schizotypal, delusional and other non-mood psychotic disorders (F20–F29); mood (affective) disorders (F30–F39); anxiety, dissociative, stress-related, somatoform and other nonpsychotic mental disorders (F40–F49), and behavioral and emotional disorders with onset usually occurring in childhood and adolescence (F90–F98). These psychiatric diagnostic categories were chosen, because the preliminary evaluation (data not shown) showed those to be the most prevalent diagnostic categories for the purpose of the subsequent statistical analysis.
Social leisure time activity in adolescence
The survey for leisure time activities consisted of the following questions: How often (never, seldom, monthly, weekly, daily) do you do the following things: Meet friends, read, play, sing, recite poems, paint, write, etc., go to the movies, concerts, exhibitions, do handwork, crafts, and other similar activities, use computers, go to discos or dancing, participate in parish activities, go hiking, fishing, hunting, do scouting? Do you belong to a sports club (no; yes, but I do not attend the training sessions; yes, I attend the training sessions)? How often do you generally do the following types of physical exercise outside of school hours (never, once a month or less often, 2–3 times a month, once a week, 2–3 times a week, 4 times a week or more often)?
First, each leisure time activity was categorized to two groups based on its intensity: active leisure time (activity accomplished at least once a week) and non-active leisure time (activities accomplished less than once a week or not at all). Belonging to a sports club and participating in sports club training sessions were always defined to indicate active leisure time. Second, each activity was categorized according to the level of social activity related to it: an activity that could be done alone (etc. reading, swimming), activity where others need to be considered (etc. meeting friends, dancing, tennis), and belonging to a community (parish, scouts or sports club). After defining the intensity and level of social activity of each leisure time activity, the study participants were categorized to three hierarchical and mutually exclusive groups of social leisure activity (SLA): 1. High level of social leisure activity (high SLA), i.e. the participant belongs to a community or sports club, 2. Middle level of social leisure activity (middle SLA), i.e. the participant has leisure time activity where other people have to be considered, but he/she does not belong to a community or a sports club, and 3. Low level of social leisure activity (low SLA), i.e. the participant only has activities that can be done alone.
Family Related Factors
Information on family structure and parents’ education was collected from a questionnaire which the parents filled in when the cohort participants were aged 15–16 years. The parents, dichotomized to those who lived together and others, were asked: Do the child’s biological parents live together? (yes; no, because they are divorced; no, because they never lived together; no, because one of the parents has died). Parental educational level (less than 9 years of comprehensive school, comprehensive school/elementary school, matriculation examination) was dichotomized to indicate at least secondary level of education completed either by the mother or the father of the study participant.
Statistical Methods
Statistical significance of difference between groups was assessed with the Pearson Chi-square test. The association of leisure time activity (high level of social leisure activity, middle level of social leisure activity, low social leisure activity) in adolescence with diagnosed psychiatric disorders by young adulthood was analyzed with a logistic regression model. Both crude odds ratios (OR) and ORs adjusted for gender, biological parents living together, parental education level and parental psychiatric disorders are reported in the results.
Figure 1 shows the selection of the data for the current study. Initially, the 1986 Northern Finland Birth Cohort consisted of 9423 subjects. For the follow-up survey completed at the age of 15–16 years, 9215 (97.8% of initial population) cohort members had a known mailing address. Of them, 7344 (79.7% of eligible sample) returned the postal survey completed at the age of 15–16 years. The attrition analysis made in the follow-up survey at age 15–16 years showed that participation in the survey was less common among males (participants vs. attrition sample) (64 vs. 71%, p < 0.001), those living in urban areas (66 vs. 71%, p < 0.001) and those having a parent with a psychiatric disorder (58 vs. 69%, p < 0.001) (Miettunen et al., 2013) In the follow-up survey, questions related to leisure time activities were answered by 7283 (99.2% of survey participants) cohort members, of whom 7051 (96.0% survey participants) gave permission to use their data for research purposes. Of them, 213 were excluded due to mental disorder diagnoses set before 16 years of age. Furthermore, 872 participants had missing data on family-related factors (parents living together, etc.), and the final size of the study population in the statistical analyses was 5966 participants. The number of cases dropped from the adjusted model (in comparison to data available for SLA categorization) was 413 among males and 459 among females (12.5 v. 13.0%, p = 0.583), 345 among individuals with parental psychiatric disorders, and 527 among individuals without parental psychiatric disorders (13.7 v. 12.2%, p = 0.086).
Statistical analysis was performed using SPSS Statistics 25.
Results
Of all study participants, 2188 (32%) belonged to high level of social leisure activity (high SLA) group, 4502 (65.8%) to middle level of social leisure activity (middle SLA) group, and 218 (3.2%) to low level of social leisure activity (low SLA) group.
As Table 1 shows, of all study participants, 48.2% were males and 51.8% were females. As for parental characteristics, 78.3% of the participants had biological parents living together, and 38.0% of the parents had completed at least secondary level education. A total of 37.0% of the participants had at least one parent with a history of doctor-diagnosed psychiatric disorder.
Table 1.
Psychiatric disorders by young adulthood and background characteristics of the study participants in relation to leisure time activity in adolescence, the 1986 Northern Finland Birth Cohort Study
| Total | Level of social leisure activity | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Low-SLAa (n = 218) | Middle-SLAa (n = 4502) | High-SLAa (n = 2118) | |||||||
| n | % | n | % | n | % | n | % | p-value | |
| Gender | |||||||||
| Male | 3298 | 48.2 | 104 | 47.7 | 2070 | 46.0 | 1124 | 53.1 | <0.001 |
| Female | 3540 | 51.8 | 114 | 52.3 | 2432 | 54.0 | 994 | 46.9 | |
| FAMILY RELATED FACTORS Biological parents living togetherb | |||||||||
| No | 1299 | 21.7 | 45 | 23.3 | 905 | 23.3 | 349 | 18.3 | <0.001 |
| Yes | 4687 | 78.3 | 148 | 76.7 | 2985 | 76.7 | 1554 | 81.7 | |
| Parental educationb | |||||||||
| Comprehensive school or less | 3781 | 62.0 | 120 | 61.2 | 2641 | 66.6 | 1020 | 52.7 | <0.001 |
| Secondary school graduate | 2316 | 38.0 | 76 | 38.8 | 1326 | 33.4 | 914 | 47.3 | |
| Parental psychiatric disorderc | |||||||||
| No | 4312 | 63.1 | 134 | 61.5 | 2787 | 61.9 | 1391 | 65.7 | 0.011 |
| Yes | 2526 | 36.9 | 84 | 38.5 | 1715 | 38.1 | 727 | 34.3 | |
| PSYCHIATRIC DISORDERS | |||||||||
| F00-F99: Any psychiatric disorder | 1003 | 14.7 | 49 | 22.5 | 704 | 15.6 | 250 | 11.8 | <0.001 |
| F10-F19: Substance use disorders | 206 | 3.0 | 8 | 3.7 | 154 | 3.4 | 44 | 2.1 | 0.010 |
| F20-F29: Psychotic disorders | 97 | 1.4 | 4 | 1.8 | 67 | 1.5 | 26 | 1.2 | 0.613 |
| F30-F39: Affective disorders | 522 | 7.6 | 25 | 11.5 | 378 | 8.4 | 119 | 5.6 | <0.001 |
| F40-F49: Anxiety | 539 | 7.9 | 33 | 15.1 | 379 | 8.4 | 127 | 6.0 | <0.001 |
| F90-F98: Behavioural disorders | 80 | 1.2 | 8 | 3.7 | 51 | 1.1 | 21 | 1.0 | 0.002 |
Participant can have diagnosis from several diagnose group. Levels of social leisure activity are mutually exclusive
aSLA social leisure activity
bWhen cohort members were 15–16 years old
cUntil the end of 2018
The results of comparisons between the three SLA groups showed higher prevalence of males in the high SLA group (53.1%) compared to the low SLA (47.7%) and middle SLA (46.0%) groups (p < 0.001). The proportion of biological parents not living together was significantly lower in the high SLA group (18.3%) compared to 23.3% in both the low- and middle SLA groups (p < 0.001). The proportion of parents who had completed at least secondary level education was lowest in the low SLA (38.8%) and middle SLA (33.4%) groups compared to the high SLA (47.3%) group (p < 0.001). The parental psychiatric disorders were less common in the high SLA group (34.3%) compared to the low SLA (38.5%) and middle SLA (38.1%) groups (p < 0.001).
The incidence of psychiatric disorders diagnosed for the first time when the study participants were 16–33 of age was 14.7%. The most common diagnostic groups were anxiety (7.6%), affective (7.9%) and substance use (3.0%) disorders. The level of SLA was statistically significantly associated with the incidence of any psychiatric disorder (p < 0.001), substance disorders (p = 0.010), affective disorders (p < 0.001), anxiety disorders (p < 0.001) and behavioral disorders (p = 0.002). Generally, the incidence of these psychiatric disorders was highest in the low SLA group and lowest in the high SLA group.
Table 2 shows the results of logistic regression analyses examining the association of social leisure time activity in adolescence with likelihood of physician-diagnosed psychiatric disorder by young adulthood. Low SLA was associated with increased likelihood of any psychiatric disorder (OR 1.61, 95% CI 1.13–2.30), anxiety disorders (OR 2.07, 95% CI 1.37–3.15) and behavioral disorders (OR 4.12, 95% CI 1.90–8.96). Furthermore, high SLA was associated with decreased likelihood of any psychiatric disorders (OR 0.78, 95% CI 0.66–0.93), substance use disorders (OR 0.53, 95% CI 0.36–0.78), affective disorders (OR 0.72, 95% CI 0.57–0.91) as well and anxiety disorders (OR 0.79, 95% CI 0.63–0.99). Social leisure time activity was not associated with psychotic disorders of the study participants.
Table 2.
Association of leisure time activity in adolescence with likelihood of psychiatric disorder diagnosed by young adulthood, the 1986 northern finland birth cohort study
| Likelihood for psychiatric disorder (outcome)a | Statistically significant covariates in adjusted model (OR and 95% CI) | ||||
|---|---|---|---|---|---|
| Low-SLAb | High-SLAb | ||||
| Outcome variable | OR | 95% CI | OR | 95% CI | |
| F00–F99: Any psychiatric disorder | |||||
| Crude model | 1.56 | 1.13–2.17 | 0.72 | 0.62–0.84 | Gender (1.40, 1.20–1.62), Biological parents living together (1.53, 1.30–1.80), Parental psychiatric disorder (1.74, 1.49–2.01) |
| Adjusted model | 1.61 | 1.13–2.30 | 0.78 | 0.66–0.93 | |
| F10–F19: Substance use disorders | |||||
| Crude model | 1.08 | 0.52–2.22 | 0.60 | 0.43–0.84 | Gender (0.53, 0.37–0.70), Biological parents living together (2.25, 1.64–3.08), Parental psychiatric disorder (1.91, 1.40–2.61) |
| Adjusted model | 1.21 | 0.58–2.52 | 0.53 | 0.36–0.78 | |
| F20–F29: Psychotic disorders | |||||
| Crude model | 1.24 | 0.45–3.42 | 0.82 | 0.52–1.30 | Gender (0.60, 0.38–0.92), Parental psychiatric disorder (2.14, 1.38–3.31) |
| Adjusted model | 1.34 | 0.48–3.74 | 0.79 | 0.49–1.29 | |
| F30–F39: Affective disorders | |||||
| Crude model | 1.41 | 0.92–2.17 | 0.65 | 0.52–0.80 | Gender (1.91, 1.55–2.34), Biological parents living together (1.55, 1.25–1.93), Parental psychiatric disorder (1.85, 1.52–2.26) |
| Adjusted model | 1.45 | 0.91–2.31 | 0.72 | 0.57–0.91 | |
| F40–F49: Anxiety disorders | |||||
| Crude model | 1.94 | 1.32–2.85 | 0.69 | 0.56–0.85 | Gender (1.63, 1.33–1.99), Biological parents living together (1.56, 1.26–1.93), Parental psychiatric disorder (1.77, 1.45–2.15) |
| Adjusted model | 2.07 | 1.37–3.15 | 0.79 | 0.63–0.99 | |
| F90–F98: Behavioural disorders | |||||
| Crude model | 3.32 | 1.56–7.10 | 0.87 | 0.52–1.46 | Biological parents living together (2.19, 1.33–3.61), Parental psychiatric disorder (1.73, 1.06–2.83) |
| Adjusted model | 4.12 | 1.90–8.96 | 1.12 | 0.65–1.93 | |
OR’s calculated with logistic regression with several outcomes. Crude model and model adjusted with gender, family structure and parental education when cohort members were 15–16, and parental psychiatric disorders until the end of 2018, has been built to examine associations between hierarchical hobby and psychiatric disorders. Participant can have a diagnosis from several diagnosis groups. Levels of social leisure activity are mutually exclusive
aReference category = Middle social leisure activity
bSLA social leisure activity
Discussion
Leisure time activities are known to have a positive effect on mental health. However, previous studies of this association have focused mainly on mental health symptoms but not on psychiatric disorders. Thus, in this respect, the research-based evidence of the impact of leisure time activities on psychiatric morbidity is still limited. This type of knowledge is needed to focus and to develop preventive actions for mental disorders. In this study, it was possible to analyze at the population level whether socially different leisure time activities during adolescence associate with first-onset mental disorders diagnosed between ages 16–33 years.
The main finding of the study was that socially active leisure time (high SLA) in adolescence was associated with a lower incidence of psychiatric disorders. Analogously, socially inactive leisure time (low SLA) was related to increased occurrence of psychiatric disorders. These findings remained significant even after controlling for commonly known family-related risk factors for psychiatric morbidity of young individuals, such as parents’ mental health disorders (Merikukka et al., 2018), parental educational level (Paananen et al., 2013), and living with a single parent (Amato, 2000). Thus, the findings of the current study can be interpreted to underline the importance of community in leisure activities as a protective factor against mental disorders. This is in line with previous studies reporting that community sport participation with improved physical health also has a positive effect on mental health among young people, seen as increasing positive psychological well-being and improving social health (e.g. Rochelle et al., 2013).
In this study, of the specific psychiatric disorders, socially active leisure time (high SLA) was found to decrease the likelihood for anxiety and affective disorders. One plausible explanation for this finding could be the role of environmental factors, which may either protect against or promote the development of these disorders (e.g. Beesdo et al., 2009). Epidemiological survey findings have also shown that anxiety disorders are the most prevalent mental disorders worldwide and are associated with significant comorbidity and morbidity (Stein et al., 2017). The development of depressive symptoms or anxious reactions to a diagnosed psychiatric disorder is usually a longer process. Commonly, it includes accumulation of various adverse experiences in everyday life of the adolescent. On the other hand, this time frame enables an individual to get support from the community, and consequently, to gather positive, rehabilitating experiences which may have a preventive impact on the development of potential mental disorders. The social interactions in the community can also provide alternative perspectives on stressors and challenges and give collaborative solutions for the difficulties an individual may have in his/her everyday life. Previous studies have acknowledged that on the individual level, interactions with close people within the community increase a sense of togetherness and lead to self-confidence and social skills (e.g. Ungar, 2012), which strengthens individuals’ mental health.
An important finding of this study was that high SLA was related to decreased likelihood of substance use disorders. In earlier studies, community-based activity, such as sports clubs, are shown to reduce the likelihood for substance abuse (Kristjansson et al. 2010). This can be seen as a result of the positive example of the community and the meaningful activity the community offers as an alternative to substance abuse. Also, the social pressure of an organized activity group and its rules of prohibiting substance use may affect individuals’ behavior. Overall, the high SLA findings of the current study give further support to the impact of leisure time activities on the positive mental health of young persons (e.g. Agans et al., 2014).
Socially inactive leisure time (low SLA) increased the incidence of anxiety and behavioral psychiatric disorders. One explanation for an excess of anxiety disorders might relate to the individuals themselves; for example, they may have a sensitive and introvert personality and therefore seek out leisure time activities that can be done alone (Whisman et al., 2000). Because of hobbies that are not social, adolescents may also have missed out on the potential protective effect of communities. Also, on community level, it is possible that some peer groups do not accept anxious or introverted persons as a group member. Accumulated experiences of being alone and left outside peer groups can be a source of anxiety and other mental health problems (Cantor-Graae and Selten, 2005). In this study, behavioral disorders were also associated with socially inactive leisure time. This may be due to decreased social capability, which is one typical characteristic of the disorder (Ogundele, 2018). Thus, the symptoms of these behavioral disorders may have been affecting the ability to be part of or to be approved by a peer group. This same phenomenon might be a plausible explanation for inactive social leisure time with other psychiatric disorders as well.
The current study showed that first-onset psychotic disorders did not associate with either high or low social leisure time activity, although the occurrence of psychotic disorders was in line with general population rates (Moilanen et al., 2010). The explanation may be that psychiatric morbidity cannot be explained only by social or environmental factors, but also by genetic transmission (e.g. Kendler et al., 2003). The role of genetic factors is emphasized especially among the most severe disorders, such as psychosis (Holmans, 2020). However, in terms of preventing these disorders and according to the stress-vulnerability model (Myllyaho et al., 2021), meaningful social leisure time activities could be beneficial in reducing stress and providing tools to cope with them.
The present study has several strengths. Firstly, the cohort data is extensive and covers the entire birth cohort in Northern Finland. The follow-up of the subjects is based on register data that is monitored. Secondly, the Finnish Care Register has been found to be a reliable source of information in studies (Gissler and Haukka, 2004). In this study, it was possible to access the psychiatric diagnosis-related information far into adulthood. The registers utilized here provided the possibility to follow the accumulation of first onset of mental disorders occurring from 16 up to 33 years of age among the cohort members. The third strength of this study is that mental disorder diagnoses were extracted from the healthcare registers including all inpatient hospitalizations and specialized level outpatient visits of the study participants nationwide. The diagnoses in health care registers are always based on the ICD classification of diseases, which uses operational diagnostic criteria. Diagnosing a mental disorder always requires a thorough clinical examination (assessment of psychiatric status) of a patient, including differential diagnostics, not only between the psychiatric disorders, but also in relation to somatic illnesses. The clinical evaluation includes assessment of symptom criteria, not only symptoms informed by the patient, but also symptoms objectively observed by health care professionals. The severity (impact on distress and performance) and duration of the symptoms are also crucial criteria for mental disorder diagnosis. Research utilizing data on self-reported symptoms is often prone to subjective bias and, thus, caseness determination, i.e. a condition or fact the diagnostic criteria for a psychiatric disorder are satisfied, is unreliable.
There are some limitations attached to this study. The first limitation is that some mental disorder diagnoses were made by treating physician, not by a mental health specialist (psychiatrist), causing bias in the assessment of specific diagnosis of mental disorder. They have differences in their clinical practices because of differences in training and working experience. The second limitation in this study is that there is no information on whether structured methods have been used to set the diagnoses and also, it is not possible to control diagnostic practices between physicians. The third limitation of this study is the lack of information about undiagnosed mental health issues of the study participants. Some of the study participants’ mental health problems may have remained unrecognized and untreated in youth and the results can thus be biased due to undiagnosed mental health issues. The fourth limitation is that the small number of cases in the subgroup analyses may have caused lack of power in statistical analyses (Type II error). In addition, due to the many statistical comparisons performed in this study the possibility of chance findings (Type I error) cannot be excluded.
Conclusion
Research-based knowledge on whether the level of adolescent social leisure time activity is associated with specific physician-diagnosed mental disorders already by young adulthood has been limited. In this study, the main findings were that socially active leisure time in adolescence was associated with a lower incidence of psychiatric disorders in general, and, specifically, with affective, anxiety, and substance use disorders by young adulthood. Analogously, low social leisure time activity was related to increased incidence of any psychiatric disorder in general, and to anxiety and behavioral disorders in particular. Overall, our findings strongly indicate that socially active leisure time during adolescence is a protective factor against development of later psychiatric disorders. Social support of the community in the early phase is one way to prevent development of mental health symptoms into manifest psychiatric disorders. In terms of prevention of mental disorders, these study findings encourage families, schools and other communities to continue to enhance and develop community-based social leisure time activities for children and adolescents.
Biographies
Johanna Timonen
MSc, is a PhD student in the University of Oulu. Her major interests include leisure time activities and mental health prevention.
Mika Niemelä
PhD, is a professor of practice in the University of Oulu. His major interests cover implementation research and mental health prevention.
Helinä Hakko
PhD, is a biostatistician in Oulu University Hospital. Her major interests include statistics and psychiatric research.
Anni Alakokkare
MSc, is a biostatistician in the University of Oulu. Her major interests include statistics and psychiatric research.
Sami Räsänen
MD, PhD, is a professor of Psychiatry in the University of Oulu. His major interests include psychiatric research.
Authors’ Contributions
J.T. conceived of the study, contributed to study design, interpretations, and conducted analyses. S.R., H.H., A.A., and M.N. conceived and participated in the study design interpretation, conducted analyses and participated in drafting of the paper. All a read and approved the final paper.
Funding
This study was supported by the grant of ITLA Children’s Foundation (Researchers JT and MN). Open access funding provided by University of Oulu including Oulu University Hospital.
Data Sharing and Declaration
This manuscript’s data will not be deposited due to ethical reasons and administrative policy of the data owner.
Compliance with Ethical Standards
Conflict of Interest
The authors declare no competing interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants involved in the study. The study obtained approval from the Ethical Review Board of the National Institute for Health and Welfare (§28/2009), from the Ethics Committee of Northern Ostrobothnia Hospital District (EETTMK: 108/2017) and Oulu University, Faculty of Medicine, Oulu, Finland.
Informed Consent
Informed consent was obtained from all individual participants involved in the study.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Agans JP, Champine RB, DeSouza LM, Mueller MK, Johnson SK, Lerner RM. Activity involvement as an ecological asset: profiles of participation and youth outcomes. Journal of Youth and Adolescence. 2014;43:919–932. doi: 10.1007/s10964-014-0091-1. [DOI] [PubMed] [Google Scholar]
- Amato P. The consequences of divorce for adults and children. Journal of Marriage & Family. 2000;62:1269–1287. doi: 10.1111/j.1741-3737.2000.01269.x. [DOI] [Google Scholar]
- Badura, P., Madarasova Geckova, A., Sigmundova, D., van Dijk, J. P. & & Reijneveld, S. A. (2015). When children play, they feel better: Organized activity participation and health in adolescents. BMC Public Health, 1090 10.1186/s12889-015-2427-5. [DOI] [PMC free article] [PubMed]
- Bélair, M. A., Kohenn, D. E., Kingsbury, M. & & Colman, I. (2018). Relationship between leisure time physical activity, sedentary behaviour and symptoms of depression and anxiety: evidence from a population-based sample of Canadian adolescents. BMJ Open, 8, e021119. 10.1136/bmjopen-2017-021119. [DOI] [PMC free article] [PubMed]
- Beesdo K, Knappe S, Pine DS. Anxiety and anxiety disorders in children and adolescents: developmental issues and implications for DSM-V. Psychiatric Clinics of North America. 2009;32:483–524. doi: 10.1016/j.psc.2009.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cantor-Graae E, Selten JP. Schizophrenia and migration: a meta-analysis and review. The American Journal of Psychiatry. 2005;162:12–24. doi: 10.1176/appi.ajp.162.1.12. [DOI] [PubMed] [Google Scholar]
- Dibben C, Playford C, Mitchell R. Be(ing) prepared: Guide and Scout participation, childhood social position and mental health at age 50-a prospective birth cohort study. Journal of Epidemiology and Community Health. 2016;71:275–281. doi: 10.1136/jech-2016-207898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doré I, Sabiston CM, Sylvestre M-P, Brunet J, O’Loughin J, Nader PA, Gallant F, Bélanger M. Years participating in sports during childhood predicts mental health in adolescence: a 5-year longitudinal study. Journal of Adolescent Health. 2018;64:790–796. doi: 10.1016/j.jadohealth.2018.11.024. [DOI] [PubMed] [Google Scholar]
- Doré I, O’Loughlin JL, Beauchamp G, Martineau M, Fournier L. Volume and social context of physical activity in association with mental health, anxiety and depression among youth. Preventive Medicine. 2016;91:344–350. doi: 10.1016/j.ypmed.2016.09.006. [DOI] [PubMed] [Google Scholar]
- Ferreira VR, Jardim TV, Póvoa TIR, Viana RB, Sousa ALL, Jardim PCV. Physical inactivity during leisure and school time is associated with the presence of common mental disorders in adolescence. Revista de saude publica. 2020;54:128. doi: 10.11606/s1518-8787.2020054001888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gissler M, Haukka J. Finnish health and social welfare registers in epidemiological research. Norsk Epidemiologi. 2004;14(1):113–120. [Google Scholar]
- Hansen E, Sund E, Knudtsen MS, Krokstad S, Holmen T. Cultural activity participation and associations with self-perceived health, life-satisfaction and mental health: the Young HUNT Study, Norway. BMC Public Health. 2015;15(1):1–8. doi: 10.1186/s12889-015-1873-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoegh Poulsen, P., Biering, K. & & Andersen, J. H. (2016). The association between leisure time physical activity in adolescence and poor mental health in early adulthood: A prospective cohort study. BMC Public Health, 16, 3. 10.1186/s12889-015-2658-5. [DOI] [PMC free article] [PubMed]
- Holmans P. Using genetics to increase specificity of outcome prediction in psychiatric disorders: prospects for progression. American Journal of Psychiatry. 2020;177:884–887. doi: 10.1176/appi.ajp.2020.20081181. [DOI] [PubMed] [Google Scholar]
- Jokela, M., Ruddock, M., Ylitalo, T. (2019) Pohjois-Suomen syntymäkohortit 1966 ja 1986. Historiikki yli 50 vuoden taipaleelta. https://juuli.fi/Record/0337723219.
- Kendler KS, Prescott CA, Myers J, Neale MC. The structure of genetic and environmental risk factors for common psychiatric and substance use disorders in men and women. Archives of General Psychiatry. 2003;60(9):929–937. doi: 10.1001/archpsyc.60.9.929. [DOI] [PubMed] [Google Scholar]
- Kristjansson AL, James JE, Allegrante JP, Sigfusdottir ID, Helgason AR. Adolescent substance use, parental monitoring, and leisure-time activities: 12-year outcomes of primary prevention in Iceland. Preventive Medicine. 2010;51(2):168–171. doi: 10.1016/j.ypmed.2010.05.001. [DOI] [PubMed] [Google Scholar]
- Merikukka, M., Räsänen, S., Hakko, H., Ristikari, T., Gissler, M., Niemelä, M. (2018) Association between parental hospital-treated somatic illnesses in childhood and later mental disorders among offspring up to early adulthood: An explorative study in the 1987 Finnish Birth Cohort. Scandinavian Journal of Public Health, 1–10. 10.1177/1403494818774729 [DOI] [PubMed]
- Miettunen, J., Murray, G. K., Jones, P. B., Mäki, P., Ebeling, H., Taanila, A., Joukamaa, M., Savolainen, J., Törmänen, S., Järvelin, M.-R., Veijola, J., Moilanen, I. (2013). Longitudinal associations between childhood and adulthood externalizing and internalizing psychopathology and adolescent substance use. Psychological Medicine, 1–12. 10.1017/S0033291713002328 [DOI] [PubMed]
- Miettunen J., Suvisaari J., Haukka J., & Isohanni M. (2011). Use of register data for psychiatric epidemiology in the Nordic Countries. In M. Tsuang, M. Tohen & P. Jones (Eds.), Textbook of Psychiatric Epidemiology, 17-131. Wiley-Blackwell. 10.1002/9780470976739.ch8
- Moilanen K, Jokelainen J, Jones P, Hartikainen A-L, Järvelin M-R, Isohanni M. Deviant intrauterine growth and risk of schizophrenia: A 34-year follow-up of the Northern Finland 1966 Birth Cohort. Schizophrenia research [Schizophr Res] 2010;124:223–30. doi: 10.1016/j.schres.2010.09.006. [DOI] [PubMed] [Google Scholar]
- Myllyaho, T., Siira, V., Wahlberg, K. E., Hakko, H., Tikkanen, V., Läksy, K., Roisko, R., Niemelä, M., Räsänen, S. (2021) Dysfunctional family functioning in high socioeconomic status families as a risk factor for the development of psychiatric disorders in adoptees: the Finnish Adoptive Family Study of Schizophrenia. Social Psychiatry and Psychiatric Epidemiology. 10.1007/s00127-020-02016-2 [DOI] [PubMed]
- Oberle, E., Xuejun, R. J., Guhn, M., Schonert-Reichl, K. A. & & Gadermann, A. M. (2019). 2019). Benefits of extracurricular participation in early adolescence: associations with peer belonging and mental health. Journal of Youth and Adolescence, 48, 2255–2270. 10.1007/s10964-019-01110-2. [DOI] [PubMed]
- Ogundele MO. Behavioural and emotional disorders in childhood: A brief overview for paediatricians. World J Clin Pediatr. 2018;7(1 Feb):9–26. doi: 10.5409/wjcp.v7.i1.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paananen R, Santalahti P, Merikukka M, Rämö A, Wahlbeck K, Gissler M. Socioeconomic and regional aspects in the use of specialized psychiatric care—a Finnish nationwide follow-up study. European Journal of Public Health. 2013;23:372–377. doi: 10.1093/eurpub/cks147. [DOI] [PubMed] [Google Scholar]
- Rodriguez A, Sánchez C, López E, et al. Role of physical activity and sedentary behavior in the mental health of preschoolers, children and adolescents: a systematic review and meta-analysis. Sports Medicine (Auckland, N.Z.) [Sports Med] 2019;49(9 Sep):1383–1410. doi: 10.1007/s40279-019-01099-5. [DOI] [PubMed] [Google Scholar]
- Rochelle M, Young J, Harvey J, Charity M, Payne W. A systematic review of the psychological and social benefits of participation in sport for children and adolescents: informing development of a conceptual model of health through sport. International Journal of Behavioral Nutrition & Physical Activity. 2013;10:98–118. doi: 10.1186/1479-5868-10-98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sigfúsdóttir I, Kristjánsson A, Gudmundsdottir M, Allegrante JP. Substance use prevention through school and community-based health promotion: A transdisciplinary approach from Iceland. Global Health Promotion. 2011;18:23–6. doi: 10.1016/S0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- Ströhle, A., Höfler, M., Pfister, H., Müller, A. G., Hoyer, J., Wittchen, H. U. & & Lieb, R. (2007). Physical activity and prevalence and incidence of mental disorders in adolescents and young adults. Psychological Medicine 37, 1657–1666. 10.1017/S003329170700089X. [DOI] [PubMed]
- Stein DJ, Scott KM, de Jonge P, Kessler RC. Epidemiology of anxiety disorders: from surveys to nosology and back. Dialogues Clin Neurosci. 2017;19:127–136. doi: 10.31887/DCNS.2017.19.2/dstein. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tamminen N, Reinikainen J, Appelqvist-Schmidlechner K, Borodulin K, Mäki-Opas T, Solin P. Associations of physical activity with positive mental health: A population-based study. Mental Health and Physical Activity. 2020;18(Mar):100319. doi: 10.1016/j.mhpa.2020.100319. [DOI] [Google Scholar]
- Torkildsen G. Recreation and leisure management. 5th ed. London and New York, NY: Routledge, Taylor and Francis Group; 2005. [Google Scholar]
- Ungar, M. (2012). The social ecology of recilience. a handbook of theory and practice. New York, NY: Springer. 10.1007/978-1-4614-0586-3_2.
- Whisman MA, Sheldon CT, Goering P. Psychiatric disorders and dissatisfaction with social relationships: Does type of relationship matter? Journal of Abnormal Psychology. 2000;109:803–808. doi: 10.1037//0021-843x.109.4.803. [DOI] [PubMed] [Google Scholar]