Abstract
The aim of this study is to investigate whether or not delayed graft function (DGF) and pre-transplant sensitization have synergistic adverse effects on allograft outcome after deceased donor kidney transplantation (DDKT) using the Korean Organ Transplantation Registry (KOTRY) database, the nationwide prospective cohort. The study included 1359 cases between May 2014 and June 2019. The cases were divided into 4 subgroups according to pre-sensitization and the development of DGF post-transplant [non-pre-sensitized-DGF(−) (n = 1097), non-pre-sensitized-DGF(+) (n = 127), pre-sensitized-DGF(−) (n = 116), and pre-sensitized-DGF(+) (n = 19)]. We compared the incidence of biopsy-proven allograft rejection (BPAR), time-related change in allograft function, allograft or patient survival, and post-transplant complications across 4 subgroups. The incidence of acute antibody-mediated rejection (ABMR) was significantly higher in the pre-sensitized-DGF(+) subgroup than in other 3 subgroups. In addition, multivariable cox regression analysis demonstrated that pre-sensitization combined with DGF is an independent risk factor for the development of acute ABMR (hazard ratio 4.855, 95% confidence interval 1.499–15.727). Moreover, DGF and pre-sensitization showed significant interaction (p-value for interaction = 0.008). Pre-sensitization combined with DGF did not show significant impact on allograft function, and allograft or patient survival. In conclusion, the combination of pre-sensitization and DGF showed significant synergistic interaction on the development of allograft rejection after DDKT.
Subject terms: Medical research, Nephrology
Introduction
Delayed graft function (DGF) is a manifestation of acute kidney injury (AKI), which is more prevalent in deceased donor kidney transplantation (DDKT). The definition of DGF varies according to the study; however, it is mostly based on the use of dialysis within 1 week from transplant1–3. The mechanism underlying the development of DGF still needs to be unveiled, but it is suggested that post-ischemic acute tubular necrosis resulting from ischemia and reperfusion injury (IRI) developing during deceased donor management or recovery of organs, and calcineurin inhibitor (CNI) toxicity may be the major contributors4. The activation of adaptive immune system induced by DGF also increases the risk of allograft rejection.
Meanwhile, it is well known that the presence of preexisting donor-specific anti-human leukocyte antigen antibody (HLA-DSA), so-called “pre-sensitized state” is an important obstacle preventing successful kidney transplantation (KT)5–9. In such patients, HLA-DSA can increase the risk of acute or chronic antibody-mediated rejection (ABMR) resulting in worse allograft outcomes10,11. In the setting of DDKT, DGF combined with subclinical rejection resulted in far worse allograft outcomes. In addition, the detrimental impact of DGF on allograft was enhanced by the presence of pre-transplant HLA-DSA in DDKT12.
Based on the above background, it is possible that DGF in patients with pre-sensitization has a synergistic adverse impact on the allograft outcomes. However, it has yet to be fully investigated and only a single center study is available12. In this regard, the aim of this study is to investigate the combined impact of DGF and pre-sensitization on the development of allograft rejection using the well-established nationwide prospective cohort, Korean Organ Transplantation Registry (KOTRY).
Results
Baseline clinical and immunological patient characteristics
DGF developed in 10.7% (146/1359) out of the total DDKT recipients. Between pre-sensitized and non-pre-sensitized subgroups, no difference was detected in the frequency of DGF (9.6% vs. 13.0%, p = 0.188). Table 1 describes baseline characteristics of the donor and recipients of four subgroups. Baseline estimated glomerular filtration rate (eGFR) was significantly lower in donors of DGF(+) subgroups irrespective of pre-sensitization. Cold ischemic time showed a longer tendency in DGF(+) subgroups irrespective of pre-sensitization without statistical significance. However, donor age, gender, body mass index (BMI), underlying disease including DM or hypertension (HTN) and the proportion of donors after cardiac death (DCD) or donors after brain death (DBD) did not differ significantly across 4 subgroups. In our study, 3 had dual-kidney transplantation from expanded criteria donors, and 6 had en-bloc kidney transplantation from pediatric donors. All allocated in non-pre-sensitized-DGF(−) subgroup. There were no pre-emptive transplantation cases.
Table 1.
Comparison of clinical and laboratory parameters among the 4 subgroups according to DGF and pre-sensitization status.
| Non-pre-sensitized (n = 1224) | Pre-sensitized (n = 135) | p-value | |||
|---|---|---|---|---|---|
| DGF(−) (n = 1097) | DGF(+) (n = 127) | DGF(−) (n = 116) | DGF(+) (n = 19) | ||
| Donors | |||||
| Age (years) | 47.6 ± 14.9 | 48.7 ± 14.8 | 49.2 ± 13.6 | 47.1 ± 13.0 | 0.615 |
| Male (n, %) | 772 (70.4%) | 92 (72.4%) | 83 (71.6%) | 10 (52.6%) | 0.361 |
| BMI (kg/m2) | 23.2 ± 3.7 | 23.4 ± 3.8 | 22.9 ± 3.6 | 23.4 ± 4.9 | 0.743 |
| HTN (n, %) | 260 (25.3%) | 36 (29.0%) | 21 (18.9%) | 3 (17.6%) | 0.284 |
| DM (n, %) | 120 (11.6%) | 13 (10.4%) | 12 (10.8%) | 1 (5.6%) | 0.852 |
| DBD (n, %) | 1056 (96.3%) | 123 (96.9%) | 112 (96.6%) | 19 (100.0%) | 0.838 |
| DCD (n, %) | 41 (3.7%) | 4 (3.1%) | 4 (3.4%) | 0 (0.0%) | 0.838 |
| eGFR (CKD-EPI) (ml/min/1.73 m2) | 77.5 (43.3–107.1) | 32.6 (20.6–63.9)* | 72.2 (45.9–103.8)† | 47.8 (25.5–103.0) | < 0.001 |
| Cold ischemic time (min) | 290.3 ± 138.0 | 324.8 ± 135.8 | 284.4 ± 124.7 | 322.9 ± 146.0 | 0.061 |
| KDPI (%) | 66.0 (44.0–84.0) | 71.0 (51.0–89.0) | 64.0 (51.0–81.0) | 67.0 (48.0–82.0) | 0.221 |
| Recipients | |||||
| Age (years) | 51.3 ± 10.6 | 52.7 ± 11.1 | 51.1 ± 9.8 | 50.1 ± 12.1 | 0.502 |
| Male (n, %) | 678 (61.8%) | 75 (59.1%) | 38 (32.8%)*,† | 8 (42.1%) | < 0.001 |
| BMI (kg/m2) | 23.0 ± 3.3 | 22.9 ± 3.3 | 22.0 ± 2.9* | 23.0 ± 2.8 | 0.022 |
| HTN (n, %) | 986 (90.0%) | 115 (90.6%) | 97 (84.3%) | 19 (100.0%) | 0.111 |
| DM (n, %) | 311 (28.4%) | 37 (29.1%) | 17 (14.7%)*,† | 4 (21.1%) | 0.014 |
| Dialysis modality (n, %) | |||||
| Hemodialysis | 857 (78.1%) | 112 (88.2%)* | 97 (83.6%) | 18 (94.7%) | 0.011 |
| Peritoneal dialysis | 240 (21.9%) | 15 (11.8%)* | 19 (16.4%) | 1 (5.3%) | 0.011 |
| Dialysis duration (months) | 84.5 (53.7–113.4) | 90.8 (50.2–114.6) | 103.7 (68.5–136.0)*,† | 130.5 (108.6–164.9)*,† | < 0.001 |
| Previous KT history (n, %) | 92 (8.4%) | 14 (11.0%) | 31 (26.7%)*† | 3 (15.8%) | < 0.001 |
| Mismatch number (n) | 3.4 ± 1.8 | 3.5 ± 1.6 | 3.8 ± 1.3* | 3.7 ± 1.6 | 0.023 |
| Induction therapy (n, %) | |||||
| ATG | 309 (28.2%) | 58 (45.7%)* | 69 (59.5%)*,† | 12 (63.2%)* | < 0.001 |
| Basiliximab | 803 (73.3%) | 84 (66.1%) | 59 (50.9%)*,† | 14 (73.7%) | < 0.001 |
| Main immunosuppressant (n, %) | |||||
| Tacrolimus | 1076 (98.1%) | 126 (99.2%) | 115 (99.1%) | 18 (94.7%) | 0.436 |
| Cyclosporin | 16 (1.5%) | 0 (0.0%) | 0 (0.0%) | 1 (5.3%) | 0.115 |
| Sirolimus | 8 (0.7%) | 3 (2.4%) | 1 (0.9%) | 1 (5.3%) | 0.073 |
| PRA > 50% | 325 (29.6%) | 39 (30.7%) | 95 (81.9%)*,† | 14 (73.7%)*,† | < 0.001 |
| Follow-up period (months) | 38.2 (25.3–50.9) | 37.5 (24.9–51.8) | 37.8 (24.7–48.0) | 36.0 (17.7–44.1) | 0.651 |
Continuous variables are shown as mean ± standard deviation or median with interquartile range. Categorical variables are shown as number (proportions).
DGF delayed graft function, BMI body mass index, HTN hypertension, DM diabetes mellitus, DBD donor after brain death, DCD donor after cardiac death, eGFR estimated glomerular filtration, CKD-EPI chronic kidney disease-epidemiology collaboration, KDPI kidney donor profile index, KT kidney transplantation, ATG anti-thymocyte globulin, PRA panel reactive antibody, DSA donor-specific antibody.
*p < 0.05 compared with non-pre-sensitized-DGF(−) subgroup, †p < 0.05 compared with non-pre-sensitized-DGF(+) subgroup.
Among recipient factors, there was a significantly longer dialysis vintage and also additional number of female patients in both pre-sensitized subgroups than in non-pre-sensitized subgroups. As expected, pre-sensitized subgroups had higher HLA mismatch number. In addition, a previous KT history and the proportion of anti-thymocyte globulin (ATG) use as induction therapy were higher in the pre-sensitized subgroups than in the non-pre-sensitized subgroups. The proportion of DM as the primary renal disease was lower in the pre-sensitized subgroups than in the non-pre-sensitized subgroups. A significantly higher proportion of patients undergoing hemodialysis as the dialysis modality prior to KT were selected from the non-pre-sensitized-DGF(+) subgroup, when compared with the non-pre-sensitized-DGF(−) subgroup. Although the majority of patients received tacrolimus as the main immunosuppressant, more patients in DGF(+) subgroups showed a tendency to take sirolimus compared with DGF(−) subgroups.
Comparison of overall biopsy-proven allograft rejection (BPAR) and acute ABMR
The median time to BPAR and ABMR from transplant showed no significant difference across 4 subgroups (BPAR, p = 0.357; ABMR, p = 0.318). Despite the incidence of overall BPAR was not significantly different across 4 subgroups, pre-sensitized-DGF(+) subgroup tended to be higher compared with other 3 subgroups. The incidence of acute ABMR was higher in pre-sensitized-DGF(+) subgroup (21.1%, 4/19) than in other 3 subgroups. Totally, acute ABMR occurred in 53 kidney transplantation recipients (KTRs), and of these, 3 had de novo DSA at the time of biopsy. 1 was in non-pre-sensitized-DGF(−) subgroup, 1 in non-pre-sensitized-DGF(+) subgroup, the other in pre-sensitized-DGF(+) subgroup. The incidence of chronic ABMR was higher in pre-sensitized subgroups compared to non-pre-sensitized subgroups. In contrast, acute and chronic T-cell mediated rejection (TCMR) rate showed no statistically significant difference across 4 subgroups (Table 2).
Table 2.
Comparison of rejection-related outcomes among the 4 subgroups according to DGF and pre-sensitization status.
| Non-pre-sensitized (n = 1224) | Pre-sensitized (n = 135) | p-value | |||
|---|---|---|---|---|---|
| DGF (−) (n = 1097) | DGF (+) (n = 127) | DGF (−) (n = 116) | DGF (+) (n = 19) | ||
| Overall BPAR (n, %) | 139 (12.7%) | 17 (13.4%) | 17 (14.7%) | 6 (31.6%) | 0.107 |
| Acute ABMR (n, %) | 35 (3.2%) | 5 (3.9%) | 9 (7.8%)* | 4 (21.1%)*,† | < 0.001 |
| Acute TCMR (n, %) | 107 (9.8%) | 10 (7.9%) | 9 (7.8%) | 4 (21.1%) | 0.284 |
| Chronic active ABMR (n, %) | 3 (0.3%) | 2 (1.6%) | 5 (4.3%)* | 1 (5.3%) | < 0.001 |
| Chronic active TCMR (n, %) | 10 (0.9%) | 3 (2.4%) | 1 (0.9%) | 1 (5.3%) | 0.152 |
| Repeated acute rejection within 1 year (n, %) | 41 (3.7%) | 3 (2.4%) | 5 (4.3%) | 2 (10.5%) | 0.363 |
Categorical variables are shown as number (proportions).
DGF delayed graft function, BPAR biopsy-proven allograft rejection, ABMR antibody-mediated rejection, TCMR T-cell mediated rejection.
*p < 0.05 compared with non-pre-sensitized-DGF(−) subgroup, †p < 0.05 compared with non-pre-sensitized-DGF(+) subgroup.
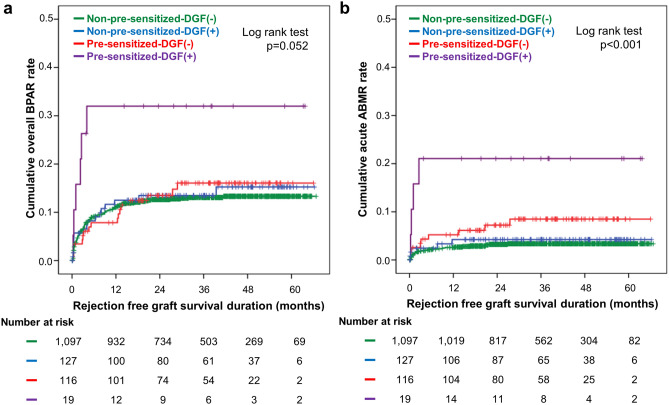
Although not significant, the Kaplan–Meier curve showed that cumulative overall BPAR rate had a tendency to be higher in pre-sensitized-DGF(+) subgroup (log rank p = 0.052) (Fig. 1a). Cumulative acute ABMR rate was significantly highest in the pre-sensitized-DGF(+) subgroup [log rank; p < 0.001 vs. non-pre-sensitized-DGF(−), p = 0.004 vs. non-pre-sensitized-DGF(+), p = 0.052 vs. pre-sensitized-DGF(−)] (Fig. 1b).
Figure 1.
Kaplan–Meier estimates of withdrawal-censored allograft rejection according to DGF and pre-sensitization status. (a) Overall BPAR rate, (b) acute ABMR rate. The numbers below the figures denote the number of KTRs at risk in each subgroup. DGF delayed graft function, BPAR biopsy-proven allograft rejection, ABMR antibody-mediated rejection, KTR kidney transplantation recipient.
Risk factors of overall BPAR and acute ABMR
In cox regression analysis, pre-sensitization and DGF individually were not independent risk factors of overall BPAR [pre-sensitization, hazard ratio (HR) 1.353, 95% confidence interval (CI) 0.874–2.097, p = 0.176; DGF, HR 1.292, 95% CI 0.834–2.001, p = 0.252]. However, when pre-sensitization and DGF were taken together, it became an independent risk factor for overall BPAR (unadjusted HR 2.933, 95% CI 1.299–6.619, p = 0.010, adjusted HR 2.663, 95% CI 1.087–6.525, p = 0.032) (Table 3a).
Table 3.
Multivariable Cox regression for independent predictors of (a) overall BPAR and (b) acute ABMR.
| Unadjusted HR (95% CI) | p-value for interaction | Adjusted HR (95% CI) | p-value for interaction | |
|---|---|---|---|---|
| (a) | ||||
| KDPI | 1.006 (1.000–1.013) | |||
| Recipient BMI | 1.057 (1.015–1.102) | |||
| Mismatch number | 1.136 (1.039–1.242) | 1.100 (0.988–1.225) | ||
| Cold ischemic time | 0.998 (0.997–1.000) | 0.998 (0.997–1.000) | ||
| Non-pre-sensitization | Reference | |||
| Pre-sensitization | 1.353 (0.874–2.097) | |||
| DGF (−) | Reference | |||
| DGF ( +) | 1.292 (0.834–2.001) | |||
| Pre-sensitization and DGF | 2.933 (1.299–6.619) | 0.010 | 2.663 (1.087–6.525) | 0.032 |
| (b) | ||||
| PRA > 50% | 1.864 (1.088–3.195) | |||
| Previous KT history | 2.291 (1.180–4.450) | 3.265 (1.641–6.496) | ||
| Dialysis duration | 1.004 (1.000–1.008) | |||
| Non-pre-sensitization | Reference | |||
| Pre-sensitization | 2.977 (1.592–5.566) | |||
| DGF(−) | Reference | |||
| DGF(+) | 1.787 (0.872–3.660) | |||
| Pre-sensitization and DGF | 6.666 (2.404–18.481) | < 0.001 | 4.855 (1.499–15.727) | 0.008 |
(a) Multivariable regression model was adjusted with parameters showing significant differences in univariable analysis or known to affect overall BPAR. Parameters were as follows: donor factors (cold ischemic time, KDPI), recipient factors (BMI, dialysis duration, previous KT history, mismatch number, PRA > 50%). 1021 (75.1%) recipients were included.
(b) Multivariable regression model was adjusted with parameters showing significant differences in univariable analysis or known to affect acute ABMR. Parameters were as follows: donor factors (cold ischemic time, KDPI), recipient factors (dialysis duration, previous KT history, mismatch number, PRA > 50%). 1,023 (75.3%) recipients were included.
BPAR biopsy-proven allograft rejection, ABMR antibody-mediated rejection, HR hazard ratio, CI confidence interval, KDPI kidney donor profile index, BMI body mass index, DGF delayed graft function, PRA panel reactive antibody, KT kidney transplantation.
In respect of acute ABMR, while DGF alone was not an independent risk factor (HR 1.787, 95% CI 0.872–3.660, p = 0.113), pre-sensitization was associated with a significant HR (HR 2.977, 95% CI 1.592–5.566, p = 0.001). In interaction analysis, the combination of pre-sensitization and DGF had much higher HR (unadjusted HR 6.666, 95% CI 2.404–18.481, p < 0.001, adjusted HR 4.855, 95% CI 1.499–15.727, p = 0.008) (Table 3b).
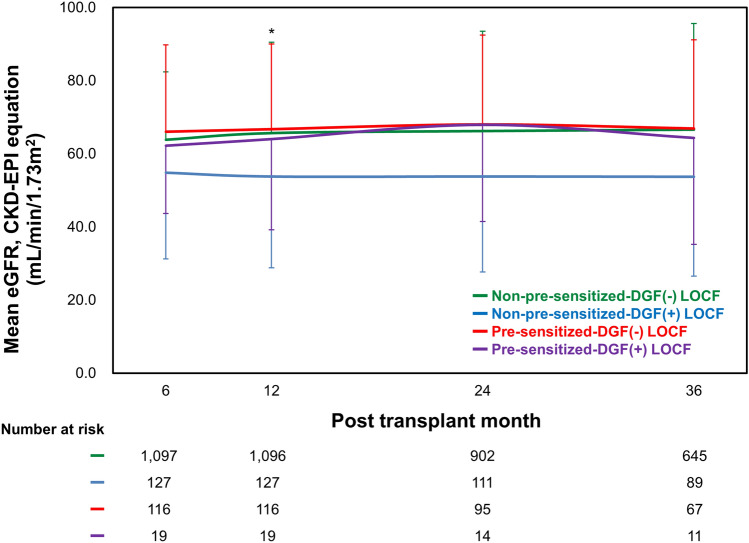
Comparison of the change in allograft function and death-censored allograft survival
Since information whether KT recipients were on dialysis at the time of discharge was unavailable, serum creatinine from 6-month after transplantation were used to compare allograft function across 4 subgroups. During 3-year follow-up, allograft function measured by eGFR using chronic kidney disease-epidemiology collaboration (CKD-EPI) equation declined in non-pre-sensitized-DGF(+) subgroup. While the change in time-related allograft function at 12 months from the respective baseline of non-pre-sensitized-DGF(−) subgroup were significantly different from that of non-pre-sensitized-DGF(+) in linear mixed model (p = 0.007), other subgroups showed no significant difference. The change in time-related allograft function at other time points showed no significant difference across 4 subgroups (p = 0.435 at 24 months, p = 0.059 at 36 months) (Fig. 2).
Figure 2.
Comparison of the time-related changes in allograft function based on eGFR using CKD-EPI equation (mL/min/1.73 m2) according to DGF and pre-sensitization status. During 36 months, the non-pre-sensitized-DGF(+) subgroup showed the lowest allograft function compared with other subgroups. eGFR Estimated glomerular filtration rate, CKD-EPI chronic kidney disease-epidemiology collaboration, DGF delayed graft function. *p < 0.05 non-pre-sensitized-DGF(−) vs. non-pre-sensitized-DGF(+) subgroup.
Totally, 41 cases of allograft failure developed during the follow-up period. The median follow-up period of graft failure in each group showed no significant difference [non-pre-sensitized-DGF(−) 37.5 (interquartile range (IQR) 25.0–50.6], non-pre-sensitized-DGF(+) 36.8 (IQR 21.7–58.3), pre-sensitized-DGF(−) 37.7 (IQR 23.6–47.36), and pre-sensitized-DGF(+) 36.0 (IQR 17.7–44.1) months, p = 0.610). The main factor contributing to allograft loss was rejection (15/41, 36.6%). Of these, 5 had clinical rejection, and 10 had BPAR. Acute ABMR occurred in 6/15 (40%), of which 5 were in non-pre-sensitized-DGF(−) subgroup and 1 in pre-sensitized-DGF(−) subgroup. In non-pre-sensitized-DGF(−) subgroup, rejection was the main cause of allograft loss (11/30, 36.7%), followed by unknown (10/30, 33.3%). In non-pre-sensitized-DGF(+) subgroup, the main cause of allograft loss was rejection (3/8, 37.5%). In pre-sensitized-DGF(−) subgroup, both rejection (1/3, 33.3%) and postoperative complications (1/3, 33.3%) accounted for same proportion. In pre-sensitized-DGF(+) subgroup, no allograft loss was reported. The Kaplan–Meier curve showed no significant difference in death-censored allograft survival among 4 subgroups (log rank p = 0.114) (Fig. 3).
Figure 3.
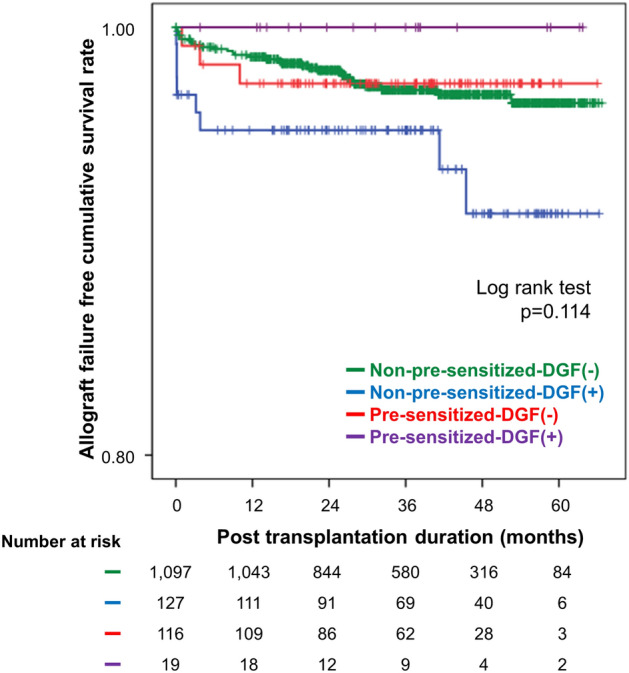
Kaplan–Meier estimates of death-censored allograft survival according to DGF and pre-sensitization status. The numbers below the figures denote the number of KTRs at risk in each subgroup. DGF delayed graft function, KTR kidney transplantation recipient.
Comparison of patient survival and post-transplant complications
A total of 55 (4.0%) patients died in our cohort due to cardiovascular disease in 9 cases, infection in 26, malignancy in 4, others (liver disease, cerebral infarction, acute CNI toxicity, gastrointestinal bleeding, and acute rejection etc.) in 11, and unknown etiology in 5 cases. In each subgroup, 37 (3.4%) died in the non-pre-sensitized-DGF(−) subgroup, 14 (11.0%) in the pre-sensitized-DGF(+) subgroup, 4 (3.4%) in the pre-sensitized-DGF(−) subgroup, and none (0.0%) in the pre-sensitized-DGF(+) subgroup. The total death rate was the highest in the non-pre-sensitized-DGF(+) subgroup (p = 0.001) (Table 4a).
Table 4.
(a) Causes of death and (b) clinical outcomes among the 4 subgroups according to DGF and pre-sensitization status.
| Non-pre-sensitized (n = 1224) | Pre-sensitized (n = 135) | p-value | ||||
|---|---|---|---|---|---|---|
| DGF(−) (n = 1097) | DGF(+) (n = 127) | DGF(−) (n = 116) | DGF(+) (n = 19) | |||
| (a) | ||||||
| Total (n, %) | 37 (3.4%) | 14 (11.0%) | 4 (3.4%) | 0 (0.0%) | 0.001 | |
| Cardiovascular disease (n, %) | 7 (18.9%) | 1 (6.4%) | 1 (25.0%) | 0 (0.0%) | ||
| Infection (n, %) | 20 (54.1%) | 4 (31.3%) | 2 (50.0%) | 0 (0.0%) | ||
| Malignancy (n, %) | 1 (2.7%) | 2 (12.5%) | 1 (25.0%) | 0 (0.0%) | ||
| Others (n, %) | 8 (21.6%) | 3 (25.0%) | 0 (0.0%) | 0 (0.0%) | ||
| Unknown (n, %) | 1 (2.7%) | 4 (25.0%) | 0 (0.0%) | 0 (0.0%) | ||
| (b) | ||||||
| BKVAN (n, %) | 32 (2.9%) | 4 (3.1%) | 5 (4.3%) | 0 (0.0%) | 0.729 | |
| Cardiovascular disease (n, %) | 141 (12.9%) | 24 (18.9%) | 14 (12.1%) | 0 (0.0%)† | 0.081 | |
| Cerebrovascular disease (n, %) | 10 (0.9%) | 1 (0.8%) | 0 (0.0%) | 0 (0.0%) | 0.740 | |
| Infection | ||||||
| Overall (n, %) | 273 (32.9%) | 37 (39.4%) | 37 (42.0%) | 3 (23.1%) | 0.185 | |
| CMV infection (n, %) | 49 (5.9%) | 4 (4.3%) | 1 (1.1%) | 0 (0.0%) | 0.203 | |
| PJP infection (n, %) | 5 (0.6%) | 1 (1.1%) | 1 (1.1%) | 0 (0.0%) | 0.889 | |
| Malignancy (n, %) | 77 (7.0%) | 11 (8.7%) | 9 (7.8%) | 2 (10.5%) | 0.848 | |
Continuous variables are shown as mean ± standard deviation or median with interquartile range. Categorical variables are shown as number (proportions).
Others: liver disease, cerebral infarction, acute CNI toxicity, gastrointestinal bleeding, intestinal obstruction, acute rejection etc.
DGF delayed graft function, CNI calcineurin inhibitor, BKVAN BK virus associated nephropathy, CMV cytomegalovirus, PJP Pneumocystis jirovecii pneumonia.
There was no significant difference in development of BK virus-associated nephropathy (BKVAN), cerebrovascular disease, infectious complications and malignancy across the 4 subgroups (Table 4b).
Discussion
Pre-sensitization to HLA is a well-known pre-transplant factor, which can increase the risk for allograft rejection and allograft failure. Meanwhile, DGF is a well-known post-transplant factor, which also induces adverse allograft outcomes. This study demonstrated that the combination of post-transplant factor (DGF) and pre-transplant risk factor (pre-sensitization) had a synergistic adverse effect on allograft outcomes, especially higher incidence of allograft rejection.
First, we compared baseline characteristics of donors and recipients across 4 clinical subgroups. In terms of donor factors, baseline renal function was significantly lower in patients who showed DGF, which was consistent with previous studies, which reported that low baseline kidney function is a risk factor for DGF13. In contrast, there was no significant difference in the frequency of DGF between pre-sensitized and non-pre-sensitized subgroups, which suggests that pre-sensitization may not have a significant effect on the development of DGF. Among recipient factors, the dialysis was significantly prolonged in pre-sensitized subgroups, which suggested that sensitized subjects need longer wait time for DDKT allocation14–16. As expected, the proportion of female recipients was higher in both pre-sensitized subgroups15 and the proportion of recipients with previous KT history was higher and tended to be high in both pre-sensitized subgroups than in non-pre-sensitized subgroups. In addition, although a majority of patients received primary maintenance immunosuppression with tacrolimus, a higher number of patients tended to receive sirolimus in the non-pre-sensitized-DGF(+) subgroup. This finding suggested that physicians decided a switch from CNI to mammalian target of rapamycin (mTOR) inhibitor, given that CNI may contribute to delayed recovery of allograft function17.
Second, we compared the incidence of overall BPAR according to pre-sensitization or the development of DGF. As a result, the incidence of overall BPAR showed a tendency to be higher in the pre-sensitized-DGF(+) subgroup, and that of acute ABMR was the highest in the pre-sensitized-DGF(+) subgroup. Interestingly, pre-sensitization and DGF showed significant interaction with each other, which suggests their synergistic impact on the development of overall BPAR and acute ABMR. This finding can be explained by two factors. First, DGF per se can increase the immunogenicity of allograft, and thereby increase the vulnerability to immune reaction of pre-formed HLA-DSA. Indeed, IRI in DGF can up-regulate the major histocompatibility complex (MHC) class I and II antigens, and enhance the expression of adhesion and costimulatory molecules of allograft tissue18–21. Moreover, the IRI induces ligands of toll-like receptors (TLRs) and activate cells of the innate immune system, inducing activation and maturation of dendritic cells, followed by adaptive immune response21. Indeed, the previous studies demonstrated that DGF is associated with an increased risk of allograft loss and acute rejection22,23. Second, the conversion of CNI to mTOR inhibitor was more frequently detected in patients who suffered from DGF in this study, perhaps because CNI might be considered as a contributor to DGF. Lower suppressive potency of mTOR inhibitor for humoral immunity in comparison with tacrolimus is another possible cause of higher rate of acute ABMR in pre-sensitized-DGF(+) subgroup24.
Surprisingly, pre-sensitization or DGF per se had no significant effect on the development of overall BPAR. The reason is unclear, but it may be attributed to the limited definition of both pre-sensitization and DGF in the study using a nationwide cohort, retrospectively. In case of pre-sensitization, since data of DSA were collected from 2017, the results of HLA-DSA were not available in some recipients. Therefore, in such recipients, we defined sensitization to HLA by the presence of panel reactive antibodies (PRA), together with positive crossmatch test results. Even though this definition is used for “pre-sensitization”, we cannot assess the degree of sensitization clearly. In case of DGF, the definition of DGF is varies among previous studies25. Indeed, the definition of DGF merely depends on the performance of dialysis after KT, and the decision whether or not to perform dialysis can differ according to the transplant centers. In addition, due to the absence of detail data, individualized immunosuppression regimen according to immunologic risk stratification and the serum level of immunosuppressant in each recipient did not be considered in our analysis. Therefore, the aforementioned factors can induce bias that can affect the result of this study.
Interestingly, non-pre-sensitized-DGF(+) group showed worst allograft function at 36 months post-transplant follow-up. One of the possible reasons is the baseline status of the corresponding donor kidney (Supplementary Table 1). The donor of this group showed relatively lower renal function at baseline, longer cold ischemic time, and a higher kidney donor profile index (KDPI) score, even though statistically insignificant. All of the foregoing findings suggest that the baseline status of donor kidney was the worst in this group, which may result in sustained low allograft function. In regard to allograft function, the impact of the baseline kidney function can be more significant than allograft rejection during the limited follow-up duration. Hence, the allograft survival was not different across 4 subgroups.
Lastly, we compared the post-transplant complications among the 4 subgroups. Non-pre-sensitized-DGF(+) subgroup showed the higher patient death rate. However, only 55 cases out of 1359 KTRs were found and there was no patient death in the pre-sensitized-DGF(+) subgroup. Therefore, longer observations may be required to arrive at any conclusion. Compared with post-transplant complications, no difference was detected across 4 subgroups in the development of BKVAN, cardiovascular disease, cerebrovascular disease, infection, and malignancy. However, further investigation may be required to clarify this issue26.
This study has some limitations. First, this nationwide registry analysis reflects similar limitations found in similar large registry analyses as shown in our previous studies27. While patient numbers are enhanced, important details for the endpoints are missing, thereby reducing the clinical utility of the findings. For example, the HLA-DSA was not available for analysis in some patients (22.6%). Additionally, MFI cut-off to define positive at respective centers was not available, and we cannot use the class and the strength of DSA in the analysis, which has been reported as an important risk factor for allograft rejection and failure6,10,28–30. Second, the follow-up duration of this registry is limited as mentioned previously. Therefore, traditional risk factors for allograft failure such as DGF and pre-sensitization did not significantly affect allograft outcome. Third, we could not determine the specified protocols at each center in DDKT for highly sensitized recipients, such as desensitization and surveillance biopsy protocols. Despite pre-transplant desensitization was performed in 35 recipients, including those whom with positive B-cell crossmatch, no data were available on the protocol. Some centers used rituximab to treat such patients, and others did not, but unfortunately, it was not considered in this analysis. Nevertheless, our study is the first multi-centered cohort study to investigate the association of DGF and pre-sensitization in allograft outcomes.
In conclusion, we have shown that combination of DGF and pre-sensitization to HLA had a detrimental impact on allograft outcome in terms of rejection. Therefore, we suggest that more careful monitoring or surveillance of allograft rejection is required. Further, we need to use more intensified immunosuppression protocol to prevent allograft rejection when DGF occurred in DDKT with pre-sensitization.
Methods
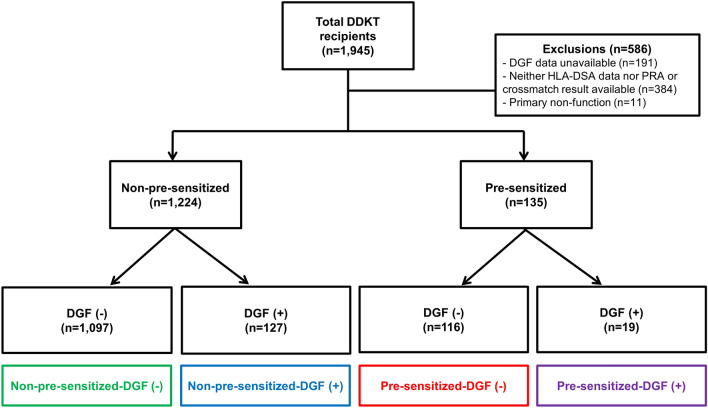
Study population
We analysed KOTRY data from the Korean Society for Transplantation31, compiling data from 30 kidney transplantation centers in Korea32. The KOTRY data includes 1945 DDKT cases between May 2014 and June 2019, from which we excluded 586 DDKT recipients with unavailable data regarding PRA, HLA-DSA, crossmatch tests or DGF development, and with primary non-function of the kidney allograft. Therefore, we included 1359 DDKT recipients in the present investigation and classified the patients into four subgroups according to the pre-sensitization and the development of DGF post-transplant: non-pre-sensitized-DGF(−) (n = 1097), non-pre-sensitized-DGF(+) (n = 127), pre-sensitized-DGF(−) (n = 116), pre-sensitized-DGF(+) (n = 19) (Fig. 4). The median follow-up period of this study was 38.1 (IQR 25.2–50.8) months.
Figure 4.
Distribution of the patient population according to DGF or pre-sensitization to HLA. DGF delayed graft function, HLA human leukocyte antigen, DDKT deceased donor kidney transplantation, DSA donor-specific antibody.
We defined pre-sensitization to HLA by the presence of (i) HLA-DSA (by Luminex single antigen assay) or (ii) PRA (by solid-phase HLA antibody screening), combined with positive crossmatch test results. HLA-DSA data were available in 1052 recipients (77.4%). Therefore, the sensitization to HLA was defined by the detection of HLA-DSA in those patients. In another 307 (22.6%) DDKT recipients for whom HLA-DSA data were not available, we defined sensitization to HLA based on the positive results of PRA and crossmatch test, regardless of whether complement-dependent cytotoxicity or flow cytometry. DGF was defined as the need for dialysis within 1 week of transplantation. The medical records were reviewed after receiving informed consent32. This study was performed in accordance with the Declaration of Helsinki and the Declaration of Istanbul. The study was approved by the Institutional Review Board of Seoul St. Mary’s Hospital (KC14ONMI0460).
Definition of clinical outcomes
The clinical outcomes investigated in this study included the incidence of overall BPAR, acute ABMR, time-related changes in allograft function measured as eGFR, death-censored allograft survival rates, and post-transplant complications such as BKVAN, cardiovascular disease, cerebrovascular disease, infection and malignancy. BPAR was diagnosed according to the Banff 2013 classification33. Rejection-free allograft survival was defined as the time elapsed from transplantation to the first episode of BPAR. Serum creatinine levels were collected at six months and later at one-year intervals post-transplant. The eGFR for each concordant time was assessed using the CKD-EPI equation34. Allograft survival was defined as the time from transplantation to initiation with alternative renal replacement therapy. Cardiovascular disease is defined as cardiovascular death, myocardial infarction, ischemic heart disease with relevant clinical evidence (accompanied by therapeutic intervention or objective findings), new-onset congestive heart failure requiring hospitalization, and arrhythmia. Cerebrovascular disease included non-traumatic hemorrhagic or ischemic brain disease confirmed by computed tomography or magnetic resonance imaging32. BKVAN was diagnosed by allograft biopsy. All clinical parameters were compared across the four patient subgroups.
Statistical method
All continuous variables were expressed as mean ± standard deviation. If the variables followed the normal distribution, an analysis of variance (ANOVA) was performed. If the variables showed non-normal distribution, a Kruskal–Wallis test was performed. Tukey’s method or Mann–Whitney test was performed as a post-hoc analysis. All categorical variables were compared using the chi-square test or Fisher's exact test and expressed as proportions. Withdrawal-censored allograft rejection rate and death-censored allograft survival rate were evaluated by using the Kaplan–Meier survival analysis and were compared using the log-rank test. The effects of DGF and pre-sensitization, and the interaction between DGF and pre-sensitization on overall BPAR or acute ABMR were analyzed via Cox proportional-hazards regression analysis. Baseline clinical and laboratory parameters showing significant differences (p value < 0.05) in univariable analysis or known to affect allograft rejection were fitted into the multivariable model. We selected donor factors (cold ischemic time, KDPI) and recipient factors (BMI, dialysis duration, mismatch number, previous KT history, PRA > 50%) as confounders. Time-related allograft function between subgroups were compared using a linear mixed model. The last observation carried forward (LOCF) analysis was used for missing eGFR values. All missing data were censored from the last follow-up date. p values < 0.05 were statistically significant. All statistical analyses were performed using the SPSS® software, version 24 (IBM Corporation, Armonk, NY, USA) and Microsoft Excel 2016.
Supplementary Information
Acknowledgements
This research was supported by a fund (2014-ER6301-00, 2014-ER6301-01, 2014-ER6301-02, 2017-ER6301-00, 2017-ER6301-01, 2017-ER6301-02) by Research of Korea Centers for Disease Control and Prevention and Research Fund of Seoul St. Mary’s Hospital, The Catholic University of Korea and also supported by a grant from the Korean Health Technology R&D Project, Ministry of Health & Welfare, Republic of Korea (HI20C0317).
Author contributions
H.L.: participated in designing study, analyzing and interpreting the data, and writing the paper. Y.P.: participated in analyzing the data, and writing the paper. T.H.B.: participated in collecting data. S.H.S.: participated in collecting data. S.H.S.: participated in collecting data. J.Y.: participated in collecting data. C.A.: participated in collecting data. C.W.Y.: participated in collecting data. B.H.C.: participated in designing study, analyzing and interpreting the data, and revising the paper. KOTRY study group: participated in collecting data.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Hanbi Lee and Yohan Park.
A list of authors and their affiliations appears at the end of the paper.
Contributor Information
Byung Ha Chung, Email: chungbh@catholic.ac.kr.
The Korean Organ Transplantation Registry Study Group:
Jin Min Kong, Oh Jung Kwon, Deok Gie Kim, Cheol-Woong Jung, Yeong Hoon Kim, Joong Kyung Kim, Chan-Duck Kim, Ji Won Min, Sung Kwang Park, Yeon Ho Park, Park Jae Berm, Jung Hwan Park, Jong-Won Park, Ho Sik Shin, Hye Eun Yoon, Kang Wook Lee, Dong Ryeol Lee, Dong Won Lee, Sam Yeol Lee, Sang-Ho Lee, Su Hyung Lee, Jung Jun Lee, Lee Jung Pyo, Jeong-Hoon Lee, Jin Seok Jeon, Heungman Jun, Kyunghwan Jeong, Ku Yong Chung, Hong Rae Cho, Ju Man Ki, Dong-Wan Chae, Soo Jin Na Choi, Duck Jong Han, Seungyeup Han, and Kyu Ha Huh
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-021-95327-6.
References
- 1.Agarwal A, Murdock P, Fridell JA. Comparison of histidine-tryptophan ketoglutarate solution and University of Wisconsin solution in prolonged cold preservation of kidney allografts. Transplantation. 2006;81:480–482. doi: 10.1097/01.tp.0000196724.89757.79. [DOI] [PubMed] [Google Scholar]
- 2.Roels L, et al. Inferior outcome of cadaveric kidneys preserved for more than 24 hr in histidine-tryptophan-ketoglutarate solution. Leuven Collaborative Group for Transplantation. Transplantation. 1998;66:1660–1664. doi: 10.1097/00007890-199812270-00015. [DOI] [PubMed] [Google Scholar]
- 3.Yarlagadda SG, et al. Marked variation in the definition and diagnosis of delayed graft function: A systematic review. Nephrol. Dial. Transplant. 2008;23:2995–3003. doi: 10.1093/ndt/gfn158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schroppel B, Legendre C. Delayed kidney graft function: from mechanism to translation. Kidney Int. 2014;86:251–258. doi: 10.1038/ki.2014.18. [DOI] [PubMed] [Google Scholar]
- 5.Sethi S, et al. Desensitization: Overcoming the immunologic barriers to transplantation. J. Immunol. Res. 2017 doi: 10.1155/2017/6804678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chung BH, et al. Clinical impact of the baseline donor-specific anti-human leukocyte antigen antibody measured by Luminex single antigen assay in living donor kidney transplant recipients after desensitization therapy. Transpl. Int. 2014;27:49–59. doi: 10.1111/tri.12199. [DOI] [PubMed] [Google Scholar]
- 7.Haririan A, et al. Positive cross-match living donor kidney transplantation: Longer-term outcomes editorial comment. J. Urol. 2009;182:1138–1138. doi: 10.1016/j.juro.2009.05.115. [DOI] [PubMed] [Google Scholar]
- 8.Marfo K, Lu A, Ling M, Akalin E. Desensitization protocols and their outcome. Clin. J. Am. Soc. Nephrol. 2011;6:922–936. doi: 10.2215/Cjn.08140910. [DOI] [PubMed] [Google Scholar]
- 9.Caro-Oleas JL, et al. Clinical relevance of HLA donor-specific antibodies detected by single antigen assay in kidney transplantation. Nephrol. Dial. Transpl. 2012;27:1231–1238. doi: 10.1093/ndt/gfr429. [DOI] [PubMed] [Google Scholar]
- 10.Lefaucheur C, et al. Preexisting donor-specific HLA antibodies predict outcome in kidney transplantation. J. Am. Soc. Nephrol. 2010;21:1398–1406. doi: 10.1681/ASN.2009101065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mohan S, et al. Donor-specific antibodies adversely affect kidney allograft outcomes. J. Am. Soc. Nephrol. 2012;23:2061–2071. doi: 10.1681/ASN.2012070664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Haller J, et al. Differential impact of delayed graft function in deceased donor renal transplant recipients with and without donor-specific HLA-antibodies. Transplantation. 2019;103:e273–e280. doi: 10.1097/TP.0000000000002802. [DOI] [PubMed] [Google Scholar]
- 13.Mannon RB. Delayed graft function: The AKI of kidney transplantation. Nephron. 2018;140:94–98. doi: 10.1159/000491558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Keith DS, Vranic GM. Approach to the highly sensitized kidney transplant candidate. Clin. J. Am. Soc. Nephrol. 2016;11:684–693. doi: 10.2215/CJN.05930615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bostock IC, et al. Probability of deceased donor kidney transplantation based on % PRA. Transpl. Immunol. 2013;28:154–158. doi: 10.1016/j.trim.2013.05.002. [DOI] [PubMed] [Google Scholar]
- 16.Jeon HJ, et al. Outcomes of end-stage renal disease patients on the waiting list for deceased donor kidney transplantation: A single-center study. Kidney Res. Clin. Pract. 2019;38:116–123. doi: 10.23876/j.krcp.18.0068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Diekmann F, et al. Sequential quadruple immunosuppression including sirolimus in extended criteria and nonheartbeating donor kidney transplantation. Transplantation. 2007;84:429–432. doi: 10.1097/01.tp.0000269610.13590.52. [DOI] [PubMed] [Google Scholar]
- 18.de Sandes-Freitas TV, et al. Prolonged delayed graft function is associated with inferior patient and kidney allograft survivals. PLoS ONE. 2015;10:e0144188. doi: 10.1371/journal.pone.0144188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shoskes DA, Parfrey NA, Halloran PF. Increased major histocompatibility complex antigen expression in unilateral ischemic acute tubular necrosis in the mouse. Transplantation. 1990;49:201–207. doi: 10.1097/00007890-199001000-00045. [DOI] [PubMed] [Google Scholar]
- 20.Doshi MD, Garg N, Reese PP, Parikh CR. Recipient risk factors associated with delayed graft function: A paired kidney analysis. Transplantation. 2011;91:666–671. doi: 10.1097/TP.0b013e318209f22b. [DOI] [PubMed] [Google Scholar]
- 21.Land WG. The role of postischemic reperfusion injury and other nonantigen-dependent inflammatory pathways in transplantation. Transplantation. 2005;79:505–514. doi: 10.1097/01.tp.0000153160.82975.86. [DOI] [PubMed] [Google Scholar]
- 22.Yarlagadda SG, Coca SG, Formica RN, Jr, Poggio ED, Parikh CR. Association between delayed graft function and allograft and patient survival: A systematic review and meta-analysis. Nephrol. Dial. Transplant. 2009;24:1039–1047. doi: 10.1093/ndt/gfn667. [DOI] [PubMed] [Google Scholar]
- 23.Butala NM, Reese PP, Doshi MD, Parikh CR. Is delayed graft function causally associated with long-term outcomes after kidney transplantation? Instrumental variable analysis. Transplantation. 2013;95:1008–1014. doi: 10.1097/TP.0b013e3182855544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Croze LE, et al. Conversion to mammalian target of rapamycin inhibitors increases risk of de novo donor-specific antibodies. Transpl. Int. 2014;27:775–783. doi: 10.1111/tri.12330. [DOI] [PubMed] [Google Scholar]
- 25.Mallon DH, Summers DM, Bradley JA, Pettigrew GJ. Defining delayed graft function after renal transplantation: Simplest is best. Transplantation. 2013;96:885–889. doi: 10.1097/TP.0b013e3182a19348. [DOI] [PubMed] [Google Scholar]
- 26.Lee SH, et al. Risk factors for Pneumocystis jirovecii pneumonia (PJP) in kidney transplantation recipients. Sci. Rep. 2017;7:1571. doi: 10.1038/s41598-017-01818-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ko EJ, Yu JH, Yang CW, Chung BH, Korean Organ Transplantation Registry Study Group Clinical outcomes of ABO- and HLA-incompatible kidney transplantation: a nationwide cohort study. Transpl. Int. 2017;30:1215–1225. doi: 10.1111/tri.12979. [DOI] [PubMed] [Google Scholar]
- 28.Riethmuller S, et al. Donor-specific antibody levels and three generations of crossmatches to predict antibody-mediated rejection in kidney transplantation. Transplantation. 2010;90:160–167. doi: 10.1097/TP.0b013e3181e36e08. [DOI] [PubMed] [Google Scholar]
- 29.Chung BH, et al. Impact of the Baseline anti-A/B antibody titer on the clinical outcome in ABO-incompatible kidney transplantation. Nephron Clin. Pract. 2013;124:79–88. doi: 10.1159/000355855. [DOI] [PubMed] [Google Scholar]
- 30.Toki D, et al. Acute antibody-mediated rejection in living ABO-incompatible kidney transplantation: Long-term impact and risk factors. Am. J. Transplant. 2009;9:567–577. doi: 10.1111/j.1600-6143.2008.02538.x. [DOI] [PubMed] [Google Scholar]
- 31.Ahn C, et al. Initial report of the Korean Organ Transplant Registry: The first report of national kidney transplantation data. Transplant. Proc. 2014;46:425–430. doi: 10.1016/j.transproceed.2013.11.083. [DOI] [PubMed] [Google Scholar]
- 32.Yang J, et al. Design and methods of the Korean Organ Transplantation Registry. Transplant. Direct. 2017;3:e191. doi: 10.1097/TXD.0000000000000678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Haas M, et al. Banff 2013 meeting report: Inclusion of c4d-negative antibody-mediated rejection and antibody-associated arterial lesions. Am. J. Transplant. 2014;14:272–283. doi: 10.1111/ajt.12590. [DOI] [PubMed] [Google Scholar]
- 34.Levey AS, et al. A new equation to estimate glomerular filtration rate. Ann. Intern. Med. 2009;150:604–612. doi: 10.7326/0003-4819-150-9-200905050-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.