Abstract
111In-leukocyte scintigraphy has generally been considered a sensitive diagnostic test for the evaluation of infectious or inflammatory processes in the abdomen due to a lack of normal physiologic bowel activity. Herein we present a case of a patient status post endovascular repair of an abdominal aortic aneurysm for which an 111In-leukocyte scan was ordered to assess for graft infection. Planar imaging revealed an abnormal focus of radiotracer activity in the right lower quadrant of the abdomen. A SPECT-CT obtained to further delineate the anatomic location of abnormal activity showed abnormal leukocyte activity localizing to the terminal ileum secondary to a micro-perforation from an ingested fishbone. This case underscores the principle that in the absence of known intra-abdominal pathology, 111In-leukocyte activity in the abdomen should always be considered abnormal, and that further evaluation with dedicated cross-sectional imaging should be performed to assist with the localization of abnormal activity.
Keywords: Indium-111, Leukocytes, White blood cells, Fish bone, Perforation, SPECT/CT
Introduction
111In-leukocyte scintigraphy has generally been considered a sensitive diagnostic test for the evaluation of infectious or inflammatory processes in the abdomen due to a lack of normal physiologic bowel activity. Protocols vary, but the most common method involves performing in vitro labeling of the patient's leukocytes before injecting the labeled cells intravenously. Subsequently, gamma camera whole-body planar imaging is acquired. Additional spot views can be obtained as necessary, and single-photon emission computed tomography (SPECT) combined with computed tomography (CT) of the same body region is often utilized to further localize any abnormal activity seen on planar imaging. As with many nuclear medicine imaging agents, 111In-leukocyte scintigraphy offers the advantage of imaging a physiologic process with the ability to relate these findings to patient anatomy.
Case report
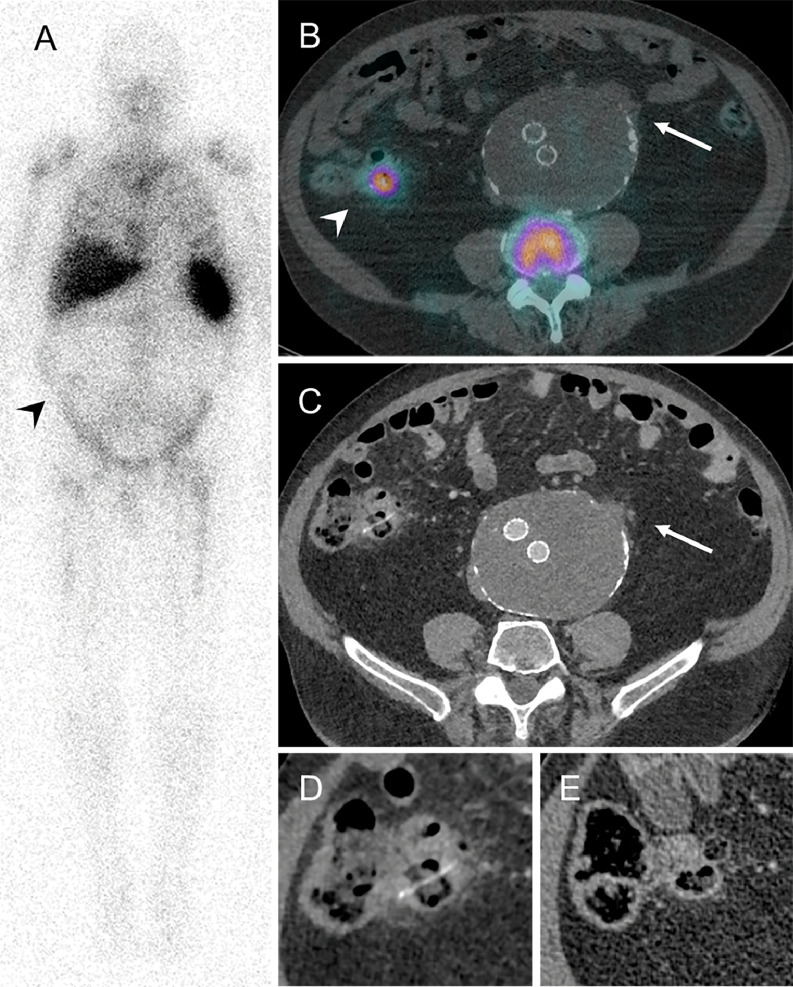
A 77-year-old with a history of an 11 cm abdominal aortic aneurysm status post endovascular repair was found to have an enlarging aneurysmal sac on a routine surveillance CT angiogram. No obvious endoleak was identified; however, there was a new irregular soft tissue density with adjacent fat stranding along the wall of the excluded aneurysmal sac that was concerning for impending rupture. Although the patient was asymptomatic and laboratory values were normal at the time, they were referred for an 111In-leukocyte scan to exclude infection as the source of this abnormality. An anterior whole body planar 111In-leukocyte emission scan showed no abnormal activity in the central abdomen to suggest a graft or focal aortic infection. However, there was a subtle focus of increased radiotracer activity within the right lower quadrant of the abdomen, as well as subtle activity extending along the course of colon (Fig. 1A). A SPECT/CT of the abdomen and pelvis was subsequently acquired to better evaluate the source of this activity. An axial fused SPECT/CT image showed a focus of increased 111In-leukocyte activity in the terminal ileum that corresponded to the abnormality seen on the planar image. No activity was associated with the region of soft tissue thickening and adjacent retroperitoneal fat stranding along the left anterolateral aspect of the excluded aneurysmal sac (Fig. 1B). Dedicated axial CT images of the terminal ileum showed a linear hyperdensity within the bowel with associated wall thickening, inflammatory fat stranding, and multiple adjacent locules of extra-luminal gas (Fig. 1C-1D). Given the constellation of findings, the patient was diagnosed with an ileal micro-perforation from an ingested fish bone. Fortunately, the patient remained asymptomatic and could be managed conservatively. A magnified axial CT image of the terminal ileum acquired at follow-up 3 months later showed resolution of the ileal inflammation, two contained micro-perforations, and an absence of the previously visualized fish bone (Fig. 1E).
Fig. 1.
111In-leukocyte whole-body planar image (A) showing a subtle focus of abnormal radiotracer activity in the right lower quadrant of the abdomen (arrowhead). Axial SPECT-CT (B) and axial CTA (C) images show an absence of radiotracer activity at the region of concern identified on recent CT angiogram (arrow); however, there is abnormal radiotracer activity localizing to the terminal ileum (arrowhead). Magnified axial CT image of the terminal ileum (D) shows a linear hyperdensity representing a fishbone with associated inflammation and locules of extraluminal gas. Magnified axial CT at follow-up 3 months after initial imaging (E) shows absence of the previously identified fishbone with resolution of the inflammation and locules of extraluminal gas.
Discussion
Although intestinal perforation is a rare complication of foreign body ingestion, fish bones are the most common cause when it does occur [1], [2], [3]. Once a bone passes through the stomach, perforation can occur anywhere along length of the bowel, but typically occurs in areas of acute angulation such as the ileocecal or rectosigmoid junctions [1,4]. Bowel perforation leading to acute abdomen results in significant morbidity and mortality both in the acute and chronic settings, and therefore timing of early detection and prompt management is crucial as it relates to patient outcomes. Computed tomography (CT) is the preferred modality to evaluate these patients with suspected complications of foreign body ingestion [5]. CT findings can be very subtle, and in the absence of obvious secondary signs of inflammation, the physiologic significance of foreign body ingestion can be unclear. As such, this case illustrates an exceedingly rare diagnosis made via 111In-leukocyte scintigraphy, which is even rarer in an asymptomatic individual, and showed evidence of active inflammation on scintigraphy despite no obvious secondary signs of inflammation on CT alone. When the diagnosis is unclear or when there is uncertainty about the significance of focal abdominal activity on scintigraphy, SPECT/CT should be utilized to localize the source of abnormal activity [6]. Furthermore, this case highlights the importance of recognizing that 111In-leukocyte activity within the abdomen, no matter how subtle, is abnormal, and may represent a potential source of patient morbidity [7], [8], [9].
Declarations of interest
No conflicts of interest.
Patient consent
Per the “Non-identifiable images” section of Elsevier Policy, written consent was not obtained, as only non-identifiable images were used.
References
- 1.Venkatesh SH, Kumar N, Karaddi V. CT findings of accidental fish bone ingestion and its complications. Diagnostic Interv Radiol. 2016;22:156–160. doi: 10.5152/dir.2015.15187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Goh K.P.B, Tan Y-M, Lin S-E. CT in the Preoperative Diagnosis of Fish Bone Perforation of the. Am J Roentgenol. 2006;187:710–714. doi: 10.2214/AJR.05.0178. [DOI] [PubMed] [Google Scholar]
- 3.Bathla G, Teo LL, Dhanda S. Pictorial essay: Complications of a swallowed fish bone. Indian J Radiol Imaging. 2011;21:63–68. doi: 10.4103/0971-3026.76061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ward E, Killeen R, Campbell N, Torreggiani WC. Abdominal CT findings in small bowel perforation. Br J Radiol. 2009;82:522–523. doi: 10.1259/bjr/13739225. [DOI] [PubMed] [Google Scholar]
- 5.Coulier B, Tancredi MH, Ramboux A. Spiral CT and multidetector-row CT diagnosis of perforation of the small intestine caused by ingested foreign bodies. Eur Radiol. 2004;14:1918–1925. doi: 10.1007/s00330-004-2430-1. [DOI] [PubMed] [Google Scholar]
- 6.Erba PA, Israel O. SPECT/CT in infection and inflammation. Clin Transl Imaging. 2014;2:519–535. doi: 10.1007/s40336-014-0092-9. [DOI] [Google Scholar]
- 7.Carrier L, Picard D, Chartrand R, Dionne D. Abdominal patterns of indium-111 labeled leukocyte imaging. Clin Nucl Med. 1986;11:153–157. doi: 10.1097/00003072-198603000-00003. [DOI] [PubMed] [Google Scholar]
- 8.Baba AA, McKillop JH, Cuthbert GF, Neilson W, Gray HW, Anderson JR. Indium 111 leucocyte scintigraphy in abdominal sepsis. Do the results affect management? Eur J Nucl Med. 1990;16:307–309. doi: 10.1007/BF00842785. [DOI] [PubMed] [Google Scholar]
- 9.Lewis SS, Cox GM, Stout JE. Clinical utility of indium 111-labeled white blood cell scintigraphy for evaluation of suspected infection. Open Forum Infect Dis. 2014;1:ofu089. doi: 10.1093/ofid/ofu089. [DOI] [PMC free article] [PubMed] [Google Scholar]