Abstract
Brodie's abscess is a relatively rare subacute form of osteomyelitis. Early diagnosis is challenging because of its insidious onset and vague symptoms. Magnetic resonance imaging is helpful in the diagnosis of Brodie's abscess; however, to date, no study has described the imaging findings of this disease in the early stage. Here, we present the case of a 14 year-old boy with Brodie's abscess in the proximal tibia. The lesion initially presented as a bone marrow edema in the proximal metaphysis of the left tibia on MRI and was misinterpreted as a bone bruise. Further radiological examination was performed 1 month later; this revealed the formation of an abscess cavity, which suggested Brodie's abscess. The patient was referred to our hospital and underwent curettage and debridement, which led to the definitive diagnosis of Brodie's abscess on histopathological findings and bacterial culture. On careful retrospective evaluation, the initial radiological findings suggested a microabscess on the metaphyseal side of the growth plate and bone marrow edema spreading from the lesion to the epiphysis. These radiological changes could be reliable evidence proving that the metaphyseal side of the growth plate is the origin of Brodie's abscess. Moreover, bone marrow edema with suspected microabscess in the metaphysis of the long bones can be the initial stage of the formation of Brodie's abscess and should be carefully followed up.
Keywords: Brodie's abscess, Bone bruise, Bone marrow edema, Growth plate
Case report
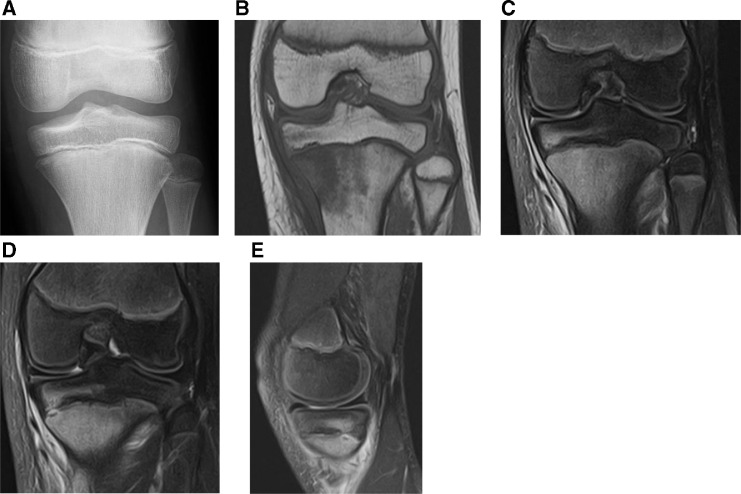
Our patient was a 14 year-old male baseball catcher without any notable medical history who presented to a nearby orthopedic clinic with a complaint of pain in the left knee without any inciting injury. Because plain radiography at initial presentation did not show any significant findings (Fig. 1A), the patient was diagnosed with overuse and advised to take some rest, which did not resolve the left knee pain. The first MRI showed a poorly defined edematous lesion on the medial side of the proximal tibia as well as around the pes anserinus and the distal part of the medial collateral ligaments with low signal intensity on T1-weighted images and high signal intensity on T2-weighted images (Fig. 1B-E). Despite no clear inciting injuries, his high activity as a baseball player and the MRI findings led to the misdiagnosis of a bone bruise. Although the patient was advised to take some rest, the symptom did not improve after a month, which resulted in his referral to our hospital.
Fig. 1.
Initial imaging examination. (A) Anteroposterior plain radiograph of the left knee shows no significant signs of abnormalities. (B, C) Magnetic resonance imaging of the left knee. Coronal view of T1-weighted and fat-suppressed T2-weighted images. Bone marrow edema around the pes anserinus and fluid accumulation below the medial collateral ligament are observed. (D, E) Another imaging slice of coronal and sagittal view of fat-suppressed T2-weighted images. There was a space occupied lesion at the metaphyseal growth plate and it was considered a microabscess retrospectively.
On physical examination, the patient had tenderness at the slightly swollen point on the medial side of the left knee without typical local signs of infection, such as erythema and warmth. No restriction in knee motion was observed. The patient was subjected to routine biochemical and radiological investigations. The leukocyte count was 3,800/μL and C-reactive protein level was 0.86 mg/dL, which suggested a mild increase in inflammatory response.
Subsequent plain radiography and MRI revealed a well-defined intramedullary cystic lesion at the edge of the proximal tibial metaphysis (Fig. 2 A–C). On T1-weighted images, the central part of the lesion showed low signal intensity, the thin layer around this central part was isointense to the muscle, and the discrete peripheral zone showed low signal intensity. Therefore, based on these radiological features and clinical course, we suspected the formation of Brodie's abscess.
Fig. 2.
Second imaging examination 1 month after the initial examination. (A) Anteroposterior plain radiograph of the left knee shows the osteolytic lesion on the medial side of the tibial metaphysis. (B, C) Magnetic resonance imaging of the left knee. Coronal view of T1-weighted and fat-suppressed T2-weighted images. An osteolytic lesion is detected. The central part of the lesion has a low signal intensity on T1-weighted images and high signal intensity on fat-suppressed T2-weighted images, which suggested pus accumulation.
Curettage and debridement were performed to determine and treat the pathological diagnosis. The operation was carefully performed to avoid damaging the adjacent growth plate (Fig. 3A). Intraoperative findings confirmed that the dark red pus spilled after fenestration of the bone, which was subjected to culture examination. The histopathological findings revealed proliferation of the granulation tissue and infiltration of the inflammatory cells, including neutrophils and plasma cells (Fig. 3B). Because Methicillin-sensitive Staphylococcus aureus grew on a culture specimen obtained during surgery, intravenous administration of cefazolin for 2 weeks and oral cefalexin for 3 months were performed. The pain resolved shortly after the surgery. At the 18-month follow-up, there were no significant changes in the growth plate (Fig. 4A) nor clear signs of reactivation on MRI (Fig. 4B and C). The patient had no complaints of pain in the left knee and resumed playing baseball.
Fig. 3.
Intraoperative and pathological findings. (A) Curettage was performed through the thinning area of the cortical bone, preventing damage to the growth plate. (B) Hematoxylin and eosin staining (100 × magnification). No atypical cells were detected. Inflammatory cell infiltration and granulation tissue proliferation were observed, some of which invade the cancellous bone.
Fig. 4.
Postoperative findings 18 months after surgery. (A) Anteroposterior plain radiograph of the left knee shows no significant change in the growth plate. (B, C) Magnetic resonance imaging of the left knee. Coronal view of T1-weighted and fat-suppressed T2-weighted images. The lesion is replaced by native tissue with postoperative inflammatory change.
Discussion
Brodie's abscess is a subacute form of osteomyelitis that presents as an accumulation of pus in bones [1]. In 1832, Sir Benjamin Brodie first described a localized abscess in the tibia without systemic symptoms of infection. He examined a case resulting in amputation and demonstrated the efficacy of perforating the bone using a trephine [2]. Since then, numerous studies have described different clinical and treatment aspects. Considering its epidemiology, Brodie's abscess is more likely to occur in young males. The most commonly affected sites are the metaphyseal parts of the long bones, particularly the femur and tibia [3], [4], [5]. The most common pathogen is Staphylococcus aureus, although Pseudomonas, Kingella kingae, and Streptococcus pyogenes have also been reported to be causative organisms [6,7]. The symptoms are commonly confined to the affected sites; systemic symptoms of infection, including fever, are rarely noted. Therefore, the diagnosis of Brodie's abscess can be difficult and requires a considerable amount of time.
Subacute osteomyelitis has not been strictly defined, but generally it is recognized as any infection in the bony tissue that persists for >2 weeks without any symptoms of acute illness [8,9]. The infection can persist without marked symptoms for weeks because of the low virulence of the causative organism, good host resistance, or inappropriate use of antibiotics. The prevalence of acute primary hematogenous osteomyelitis in children is estimated to be between 1 and 13 per 100,000 [10], whereas that of subacute osteomyelitis is generally lower [11]. The formation of Brodie's abscess is even rarer, accounting for only 2.4% of the total number of cases of osteomyelitis [3]. In this report, the rarity of Brodie's abscess led to the misinterpretation of the initial bone marrow edema on MRI as a bone bruise, a more common condition. Brodie's abscess is seen predominantly in young males with an unfused epiphyseal growth plate, typically presenting during the second decade of life. It is commonly found in the metaphysis of long bones, such as the tibia and femur [3], [4], [5]. The main symptoms are localized bone pain and swelling. Owing to the lack of systemic illness and frequently normal laboratory findings, clinically diagnosing Brodie's abscess can be challenging. In this case report, although it occurred at a common site at a common age, only localized pain and a mild increase in C-reactive protein levels were noted. Furthermore, because of the high activity of the patient as a baseball player, the condition was misdiagnosed as a bone bruise.
The radiological findings of Brodie's abscess are similar to those of other benign and malignant bone lesions causing inflammation in the surrounding area, including osteoid osteoma, Langerhans cell histiocytosis chondrosarcoma, Ewing's sarcoma, and traumatic lesions [5,[12], [13], [14]]. Plain radiography of Brodie's abscess shows a lytic lesion with peripheral sclerotic rim fading [13]. The features of MRI are helpful for the diagnosis of Brodies’ abscess. Marti-Bonmati et al. first described the “target” appearance on MRI, comprising four separate layers: (1) a center, (2) two rings, and (3) a peripheral halo [15]. The central region represents the abscess cavity. The inner ring corresponds to the granulation layer, and the outer ring corresponds to reactive sclerosis. The peripheral halo represents the imaging equivalent of bone marrow edema. Additionally, Grey et al. and McGuinness et al. described the importance of the “penumbra sign,” referring to a transition zone with relatively high signal intensity on T1-weighted images between the abscess and reactive sclerosis [16,17]. In this case report, the patient demonstrated both the “target” appearance and “penumbra sign” on the second MRI (Fig. 2 A–C). However, to date, no study has demonstrated the imaging features in the early stage of the disease.
Bone marrow edema, particularly that occurring at the knee, has a wide differential diagnosis, which includes ischemic, mechanical, and reactive causes of bone marrow edema [18]. Additionally, the focal periphyseal edema zone on MRI that was first described by Zbojniewicz et al. may be helpful in characterizing bone marrow edema, particularly in the case of adolescents [19]. The focal periphyseal edema zone is probably related to the early stage of physiological closure of the growth plate. Although it causes pain, there is little need for invasive measures and no need for follow-up MRI; moreover, conservative treatment shows good outcomes. In our patient, the metaphyseal side of the growth plate appeared to be slightly separated on initial MRI. On careful retrospective evaluation, inferring a microabscess was possible (Fig. 1 D and E). The bone marrow edema in our patient spread around the microabscess even in the epiphysis, which indicates that the microabscess was the center of the diffuse inflammation.
Several etiologies are associated with osteomyelitis. Kremers HM et al. reported that hematogenous infections and trauma-related contiguous infections cause of most cases of pediatric osteomyelitis [20]. Particularly, the metaphysis is the primary site of infection in children owing to its abundant vascularity [21]. The reduced rate of blood flow in the capillary loops at the metaphysis renders this site more susceptible to hematogenous seeding of infection, furnishing a breeding ground for septic emboli [22], [23], [24]. We believe that the radiological changes in our patient observed on sequential MRI suggest that the infection occurred from the metaphyseal side of the growth plate.
Treatment options for Brodie's abscess vary. It has been reported that treatment with the combination of antibiotics and immobilization without operation is successful in some cases [25]. Currently, the trend toward the use of medication alone for pediatric osteomyelitis is increasing, but no prospective studies support this [26]. Early biopsy and curettage combined with antibiotics are considered the standard procedure for not only treatment but also histopathological diagnosis of Brodie's abscess [4,5]. The duration of antibiotic treatment has also been a subject of debate; however, chronic infections require antibiotic therapy lasting for 3 to 6 months after surgery [27]. In our patient, antibiotics were administered for 3 months postoperatively, and no recurrence was observed.
In conclusion, the initial MRI findings of the present case proved the concept of infectious origin of Brodie's abscess on the metaphyseal side of the growth plate. Bone marrow edema associated with a space-occupying lesion suggestive of a microabscess at the metaphysis growth plate without any traumatic history could be the initial stage of Brodie's abscess and should be carefully followed up.
Patient consent
Informed consent was obtained from the participant included in the study.
Footnotes
Acknowledgments: We would like to thank to Ms. Makana Suzuki for her administrative support.
Competing Interests: The authors declare that they have no conflicts of interest.
Ethical approval: All procedures performed in our study involving the human participant were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
References
- 1.Harris NH, Kirkaldy-Willis WH. Primary subacute pyogenic osteomyelitis. J Bone Joint Surg Br. 1965;47:526–532. [PubMed] [Google Scholar]
- 2.Brodie BC. An account of some cases of chronic abscess of the tibia. Med Chir Trans. 1832;17:239–249. doi: 10.1177/095952873201700111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Olasinde AA, Oluwadiya KS, Adegbehingbe OO. Treatment of brodie's abscess: excellent results from curettage, bone grafting and antibiotics. Singapore Med J. 2011;52(6):436–439. [PubMed] [Google Scholar]
- 4.Stephens MM, MacAuley P. Brodie's abscess. a long-term review. Clin Orthop Relat Res. 1988;234:211–216. [PubMed] [Google Scholar]
- 5.van der Naald N, Smeeing DPJ, Houwert RM, Hietbrink F, Govaert GAM, van der Velde D. Brodie's abscess: a systematic review of reported cases. J Bone Jt Infect. 2019;4(1):33–39. doi: 10.7150/jbji.31843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Amit P, Maharajan K, Varma B. Streptococcus pyogenes associated post-traumatic brodie's abscess of cuboid: a case report and review of literature. J Orthop Case Rep. 2015;5(3):84–86. doi: 10.13107/jocr.2250-0685.318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ruttan TK, Higginbotham E, Higginbotham N, Allen CH, Hauger S. Invasive kingella kingae resulting in a brodie abscess. J Pediatric Infect Dis Soc. 2015;4(2):e14–e16. doi: 10.1093/jpids/piu046. [DOI] [PubMed] [Google Scholar]
- 8.Agrawal P, Sobti A. A brodie's abscess of femoral neck mimicking osteoid osteoma: diagnostic approach and management strategy. Ethiop J Health Sci. 2016;26(1):81–84. doi: 10.4314/ejhs.v26i1.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mandell JC, Khurana B, Smith JT, Czuczman GJ, Ghazikhanian V, Smith SE. Osteomyelitis of the lower extremity: pathophysiology, imaging, and classification, with an emphasis on diabetic foot infection. Emerg Radiol. 2018;25(2):175–188. doi: 10.1007/s10140-017-1564-9. [DOI] [PubMed] [Google Scholar]
- 10.Yeo A, Ramachandran M. Acute haematogenous osteomyelitis in children. BMJ. 2014;348:g66. doi: 10.1136/bmj.g66. [DOI] [PubMed] [Google Scholar]
- 11.Riise OR, Kirkhus E, Handeland KS, Flato B, Reiseter T, Cvancarova M. Childhood osteomyelitis-incidence and differentiation from other acute onset musculoskeletal features in a population-based study. BMC Pediatr. 2008;8:45. doi: 10.1186/1471-2431-8-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nicolajsen K, Jorgensen PS, Torholm C. [Brodie abscess. Primarily misinterpreted as traumatic lesion] Ugeskr Laeger. 1996;158(2):171–172. [PubMed] [Google Scholar]
- 13.Gould CF, Ly JQ, Lattin GE, Jr., Beall DP, Sutcliffe JB., 3rd Bone tumor mimics: avoiding misdiagnosis. Curr Probl Diagn Radiol. 2007;36(3):124–141. doi: 10.1067/j.cpradiol.2007.01.001. [DOI] [PubMed] [Google Scholar]
- 14.Moser T, Ehlinger M, Chelli Bouaziz M, Fethi Ladeb M, Durckel J, Dosch JC. Pitfalls in osteoarticular imaging: how to distinguish bone infection from tumour? Diagn Interv Imaging. 2012;93(5):351–359. doi: 10.1016/j.diii.2012.01.021. [DOI] [PubMed] [Google Scholar]
- 15.Marti-Bonmati L, Aparisi F, Poyatos C, Vilar J. Brodie abscess: MR imaging appearance in 10 patients. J Magn Reson Imaging. 1993;3(3):543–546. doi: 10.1002/jmri.1880030318. [DOI] [PubMed] [Google Scholar]
- 16.McGuinness B, Wilson N, The Doyle AJ. "penumbra sign" on T1-weighted MRI for differentiating musculoskeletal infection from tumour. Skeletal Radiol. 2007;36(5):417–421. doi: 10.1007/s00256-006-0267-1. [DOI] [PubMed] [Google Scholar]
- 17.Grey AC, Davies AM, Mangham DC, Grimer RJ, Ritchie DA. The 'penumbra sign' on T1-weighted MR imaging in subacute osteomyelitis: frequency, cause and significance. Clin Radiol. 1998;53(8):587–592. doi: 10.1016/s0009-9260(98)80150-5. [DOI] [PubMed] [Google Scholar]
- 18.Hofmann S, Kramer J, Vakil-Adli A, Aigner N, Breitenseher M. Painful bone marrow edema of the knee: differential diagnosis and therapeutic concepts. Orthop Clin North Am. 2004;35(3):321–333. doi: 10.1016/j.ocl.2004.04.005. ix. [DOI] [PubMed] [Google Scholar]
- 19.Zbojniewicz AM, Laor T. Focal Periphyseal Edema (FOPE) zone on MRI of the adolescent knee: a potentially painful manifestation of physiologic physeal fusion? AJR Am J Roentgenol. 2011;197(4):998–1004. doi: 10.2214/AJR.10.6243. [DOI] [PubMed] [Google Scholar]
- 20.Kremers HM, Nwojo ME, Ransom JE, Wood-Wentz CM, Melton LJ, 3rd, Huddleston PM., 3rd Trends in the epidemiology of osteomyelitis: a population-based study, 1969 to 2009. J Bone Joint Surg Am. 2015;97(10):837–845. doi: 10.2106/JBJS.N.01350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jaramillo D, Dormans JP, Delgado J, Laor T, St Geme JW., 3rd Hematogenous osteomyelitis in infants and children: imaging of a changing disease. Radiology. 2017;283(3):629–643. doi: 10.1148/radiol.2017151929. [DOI] [PubMed] [Google Scholar]
- 22.Offiah AC. Acute osteomyelitis, septic arthritis and discitis: differences between neonates and older children. Eur J Radiol. 2006;60(2):221–232. doi: 10.1016/j.ejrad.2006.07.016. [DOI] [PubMed] [Google Scholar]
- 23.Green NE, Edwards K. Bone and joint infections in children. Orthop Clin North Am. 1987;18(4):555–576. [PubMed] [Google Scholar]
- 24.Fathinul F, Nordin A. F-FDG PET/CT as a potential valuable adjunct to MRI in characterising the Brodie's abscess. Biomed Imaging Interv J. 2010;6(3):e26. doi: 10.2349/biij.6.3.e26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ross ER, Cole WG. Treatment of subacute osteomyelitis in childhood. J Bone Joint Surg Br. 1985;67(3):443–448. doi: 10.1302/0301-620X.67B3.3997957. [DOI] [PubMed] [Google Scholar]
- 26.Dartnell J, Ramachandran M, Katchburian M. Haematogenous acute and subacute paediatric osteomyelitis: a systematic review of the literature. J Bone Joint Surg Br. 2012;94(5):584–595. doi: 10.1302/0301-620X.94B5.28523. [DOI] [PubMed] [Google Scholar]
- 27.Lima AL, Oliveira PR, Carvalho VC, Cimerman S, Savio E. Diretrizes Panamericanas para el Tratamiento de las Osteomielitis e Infecciones de Tejidos Blandos G. Recommendations for the treatment of osteomyelitis. Braz J Infect Dis. 2014;18(5):526–534. doi: 10.1016/j.bjid.2013.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]